Abstract
Unicystic ameloblastoma is a rare, benign, locally invasive odontogenic neoplasm of young age that show clinical, radiographic, or gross features of an odontogenic cyst, but histologically shows typical ameloblastomatous epithelium lining part of the cyst cavity, with or without luminal and/or mural tumor growth. The article presents atypical cases of a large, asymptomatic unicystic ameloblastoma of posterior maxilla and mandibular molar-ramus regions which were treated by surgical enucleation and application of Carnoy's solution for 3 min. The article also describes the importance and complexity of differential diagnosis of an odontogenic lesion sharing common clinical and radiographical features.
Keywords: Carnoy's solution, dentigerous cyst, maxillary posterior region, recurrence, surgical enucleation, unicystic ameloblastoma
Introduction
Unicystic ameloblastoma (UA) variant of ameloblastoma was first described by Robinson and Martinez[1] in 1977 as a special type of ameloblastoma. According to WHO 1992 definition, ameloblastoma is a benign locally invasive polymorphic neoplasm consisting of proliferating odontogenic epithelium which usually has a follicular or a plexiform pattern lying in a fibrous stroma. It usuallyoriginate in the mandibular molar-ramus area and appears very similar to a non-neoplastic odontogenic cyst and is frequently misdiagnosed as a dentigerous cyst and a odontogenic keratocyst; hence histological confirmation is mandatory.[2] Ackermann et al,[3] classified UA in three histologic subtypes: (1) lumenal (type 1), (2) intralumenal (type 2) in which tumor is confined to the epithelium of the cyst and may be treated conservatively by enucleation. (3) Mural pattern (type 3) in which tumor is present in the connective tissue wall of the cyst should be treated aggressively in exactly the same manner as multicystic ameloblastoma.
The pathogenesis of UA and cystic degeneration are not yet clear. It has been suggested that epithelial dysadhesion (e.g. defective desmosomes) or intrinsic production of proteinases (e.g. metalloproteinases, serine proteinases); enzymes that normally degrade the central zone of the enamel organ after tooth development may contribute to cystic degeneration of neoplasm.[4] Recently, Kahn[5] pointed out the possibility of human papilloma virus contributing to the development of unicystic ameloblastoma. The purpose of this article is to present two young cases of UA involving the maxillary right posterior region and the mandibular right molar-ramus region.
Case Reports
Case 1
A 9-year-old male patient with non-contributory medical history sought dental evaluation due to carious teeth and painless swelling on the maxillary right posterior region. The patient described initial observation of the swelling approximately 2 months prior to presentation. Clinical examination revealed painless swelling associated with carious primary maxillary right canine, first and second molar [Figure 1]. Panoramic radiograph disclosed a well-corticated unilocular radiolucent lesion (approximately 4 cm × 3 cm) in relation to primary maxillary right first molar. The unilocular radiolucency extended from the distal surface of the permanent maxillary right lateral incisor to the mesial surface of permanent maxillary second premolar [Figure 2]. On aspiration of cyst cavity, golden yellow colored fluid was noticed. On the basis of age, location, clinical, and radiographical features, preoperative diagnosis of an inflammatory dentigerous cyst and UA was made. Patient's parents were informed regarding the complexity of diagnosis, different treatment options, and recurrence. Taking into consideration the age and complexity of diagnosis, surgical enucleation followed by Carnoy's solution application and extraction of closely related teeth was planned under local anesthesia (Lox 2%, Mumbai). Primary maxillary right first and second molar and canine were extracted. The cystic cavity was punctured for drainage of fluid in order to reduce the size of the lesion. From the same extraction socket, the lesion was enucleation along with impacted permanent maxillary right first premolar [Figures 3 and 4]. Copious irrigation of bony cavity was done with a betadine solution (Win-Medicare, New Delhi) and normal saline. Carnoy's solution was applied in the bone cavity for 3 min with cotton applicators. Bony cavity was rinsed with normal saline and packed with glycerin and betadine-soaked ribbon gauze. Then horizontal matrix sutures with mersilk (Ethicon, Johnson & Johnson) were given. The excised lesion was sent for histopathological examination and gauze pack was removed 2 days postoperatively. Histological analysis of surgical specimen showed a cystic lesion surrounded by a fibrous tissue capsule lined by odontogenic epithelium of variable thickness proliferating into the lumen in a plexiform pattern. The lesion was diagnosed as unicystic ameloblastoma with intralumenal proliferations [Figure 5]. In the subsequent visit removable partial denture was given as functional space maintainer. The patient was advised to undergo treatment of the other carious teeth. Thereafter, the patient did not report for 6 months. Intraoral examination after 6 months revealed erupting permanent maxillary right lateral incisor and second premolar. The modified space maintainer was given to the patient in order to preserve the mseio-distal width. No parasthesia of lip or cheek was observed. As the diagnosis carries a risk of recurrence, a long term follow-up period was planned.
Figure 1.

Intraoral view showing an expansible lesion in the right maxillary posterior region
Figure 2.
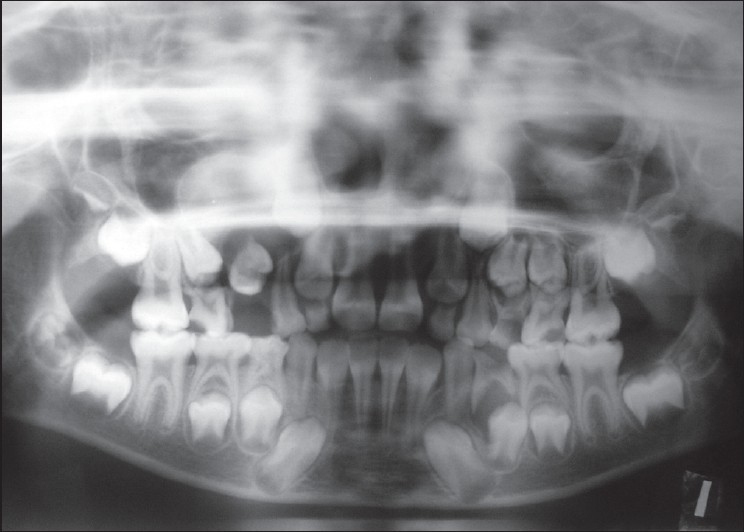
Preoperative panoramic radiograph
Figure 3.
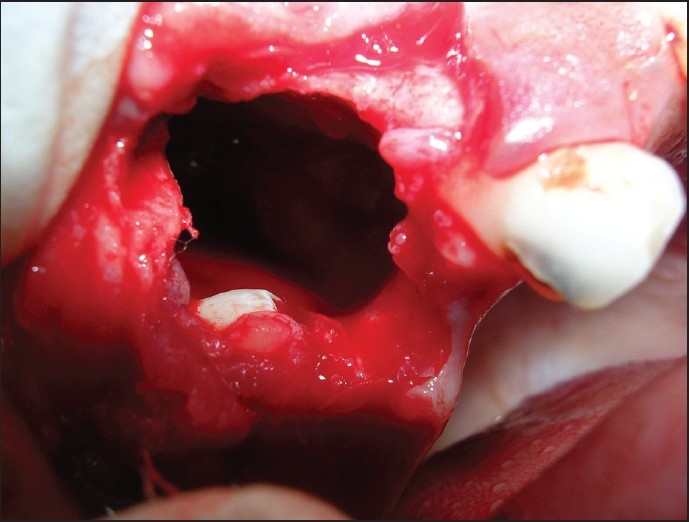
Surgical area after enucleation of a lesion
Figure 4.
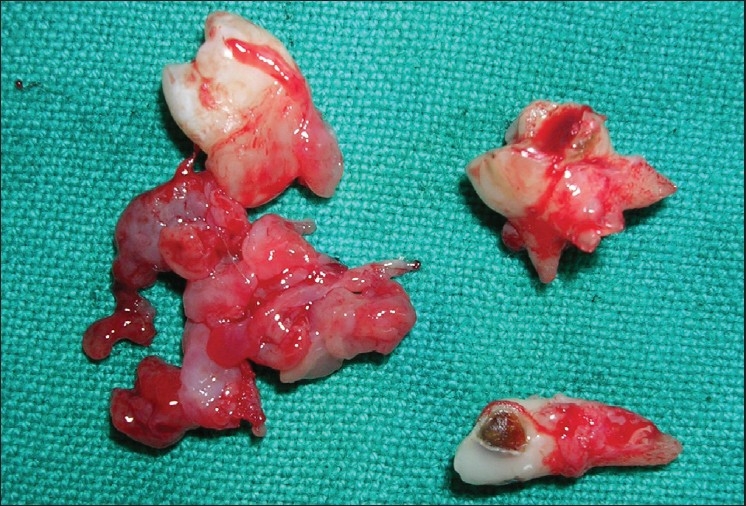
The excised lesion along with removed permanent teeth
Figure 5.
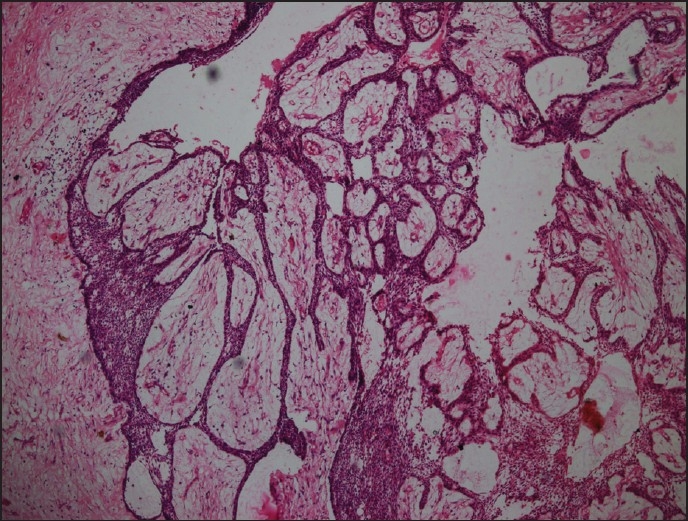
Cystic lesion surrounded by fibrous tissue capsule lined by odontogenic epithelium of variable thickness proliferating into the lumen in a plexiform pattern
Case 2
A 12-year-old female patient with non-contributory medical history sought dental evaluation due to painless swelling on the right mandibular molar-ramus region. The patient described initial observation of the swelling approximately 2 months prior to presentation. Clinical examination revealed an expansible lesion in the right mandibular third molar region and blue colored swelling distal to first molar [Figure 6]. Panoramic radiograph disclosed a unilocular radiolucent lesion (approximately 7 cm × 4 cm) with well-corticated borders involving right body, angle, and ramus of mandible. The impacted second and third molar was displaced up to the inferior border of the body and the coronoid process of mandible, respectively [Figure 7]. On aspiration of cyst cavity, golden yellow colored fluid was noticed. The CT scan confirmed the buccal and lingual cortical expansion with perforation of lingual cortex of the mandible. The lesion was difficult to diagnose on the basis of clinical and radiographic findings. Therefore, UA, dentigerous cyst, odontogenic keratocyst were considered in the differential diagnosis. Patient's parents were informed regarding the complexity of diagnosis, different treatment options, and recurrence. Taking into consideration the age and complexity of diagnosis surgical enucleation followed by Carnoy's solution application and extraction of closely related teeth was planned. Under local anesthesia (Lox 2%, Mumbai), crevicular incision was given from permanent mandibular right canine to permanent mandibular first molar. The incision extended distally over anterior border of ramus of mandible followed by mesial releasing incision from permanent mandibular right canine. Mucoperiosteal flap was reflected and underlying bone was exposed followed by decortication of the buccal cortex with bone rongeur [Figure 8]. The lesion was enucleated along with impacted teeth and erupted first permanent mandibular molar [Figure 9]. Copious irrigation of bony cavity was done with betadine solution and normal saline. Carnoy's solution was applied in the bone cavity for 3 min with cotton applicators. The bony cavity was rinsed with normal saline and packed with glycerin and betadine-soaked ribbon gauze. Then horizontal matrix sutures with mersilk (Ethicon, Johnson & Johnson) were given. The excised lesion was sent for histopathological examination and gauze pack was removed 2 days postoperatively. Histological analysis of surgical specimen showed a cystic lesion surrounded by a fibrous tissue capsule lined by odontogenic epithelium of variable thickness proliferating into the lumen in a plexiform pattern. The lesion was diagnosed as unicystic ameloblastoma with intralumenal proliferations. In the post-operative days, the patient was assessed for parasthesia of lip or cheek. As the diagnosis carries a risk of recurrence, a long term follow-up period was planned.
Figure 6.

Intraoral view showing an expansible lesion in the right mandibular third molar region and blue colored swelling distal to first molar
Figure 7.
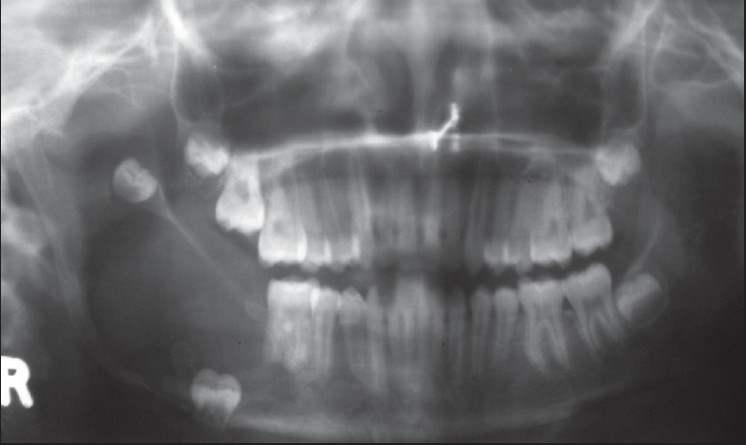
Preoperative panoramic radiograph of the mandibular molar-ramus region
Figure 8.

Intraoral view showing decortication of the buccal cortex
Figure 9.

The excised lesion along with extracted permanent and primary teeth
Discussion
Unicystic ameloblastoma is a tumor of young age group (second decade), typically unilocular radiographic appearance, macroscopically cystic nature and most important, its relatively better response to conservative treatment make it a distinguishable entity. It accounts for 10% to 15% of all intra-osseous ameloblastoma.[3] Although most commonly found in association with the crowns of impacted teeth, it may be found in interradicular, periapical, or edentulous region.[2] Commonly associated manifestations include painless swelling, facial asymmetry, unilocular lesion with defined sclerotic borders, tooth impaction, displacement, mobility, root resorption, root divergence, occlusal interference, and extrusion of tooth.[6] This distinct prognostic entity is predominantly observed in the mandibular molar-ramus region. The posterior region of maxilla is considered to be rare and atypical. The ratio of mandibular to maxillary unicystic ameloblastoma has been reported to be 13:1.[7] The present case report describes the UA of maxillary posterior and mandibular molar-ramus regions mimicking an inflammatory dentigerous cyst.
Unicystic ameloblastoma shares common clinical and radiographical manifestations with other odontogenic lesions making diagnosis difficult. Dentigerous cyst, odontogenic keratocyst, residual cyst, adenomatoid odontogenic tumor, giant cell lesion, and sometimes solid ameloblastoma can be the possible differential diagnosis for UA. Keratocyst usually spread anterio-posteriorly and seldom shows cortical expansion. On aspiration, keratocyst shows a large amount of keratin.[8] Residual cysts are associated with missing teeth that have been extracted.[9] Adenomatoid odontogenic tumors have a predilection for anterior maxilla, whereas a central giant lesion often arises anterior to first mandibular molar.[9] Solid ameloblastoma is multilocular and is seen uncommonly in patients less than 30 years of age.[5] Great difficulty exists in differentiating dentigerous cyst from UA. However, following manifestations favors UA. Defect in the wall of a cyst, unilocular cystic lesion extending into the ramus, expansion of both the buccal and lingual cortex (tumor usually grows buccally and lingually, whereas the cyst grows toward most dependent part, i.e. buccally),[6] presence of erythematous and granulomatous tissue at the marginal gingival (mucosal ulceration) with the absence of the bony cortex, and associated healthy primary dentition.[8] However, in the present case report 1, posterior maxilla (a rare site for UA) was involved and associated primary dentition was carious favoring an inflammatory dentigerous cyst. Even the surgical findings in both the cases were not conclusive for a cyst or tumor.
Various treatment modalities for UA have been used such as segmental or marginal resection, more conservative treatment such as enucleation and curettage, marsupilization to reduce the size of the lesion, followed by second stage surgery.[1,10] These treatments can be followed by adjunctive therapy including cryotherapy, thermal or chemical cauterization, and even radiotherapy or chemotherapy.[11,12] The reported recurrence rate after treatment for unicystic ameloblastoma ranges from 10% to 25%.[1] There is no adequate evidence to prove which treatment modality is more effective.
Resection of UA results in the lowest recurrence rate (3.6%) if adequate bone margins are removed. Despite high success rate for resection of UA more conservative treatment in order to optimize quality of life is generally favored.[13] Marsupialization together with other treatment resulted in an 18% recurrence. The aim of Marsupialization is to reduce the size of UA so that less extensive surgery is required. The treatment modality is not so popular method, but most benefit is expected in severely ill patients or those with a huge lesion.[10,13]
Enucleation alone yielded the highest recurrence rate among all treatment (30.5%). Two possible explanations: firstly, cystic lining of the tumor is inadequately removed; secondly, ameloblastic tumor cells can invade the cancelleous bone to a certain extent.[13] Enucleation followed by application of Carnoy's solution has resulted in a recurrence rate of 16.0% which is the best except for resection. The recurrence rate could even lower than reported, if the closely related teeth with tumor are extracted. Because in an attempt to preserve the tooth without damage, tumor remnants may be left around the tooth apex or root and these may lead to recurrence.[12,13] In the present case reports, teeth in close relation of tumor were extracted. Carnoy's solutions a powerful fixative penetrates the cancellous spaces and thus fixes the remaining tumor cells. Usually, Carnoy's solutions are applied for 3-5 min. However, Frerich et al,[14] suggested that the application of Carnoy's solutions should not exceed by 3 min and should not be directly applied over the nerve as it could lead to nerve impairment.
It has been suggested that for all unilocular lesions, an excisional biopsy by enucleation should be carried out. If the histopathological diagnosis shows Ackerman[3] type 1 or type 2 unicystic ameloblastoma, then follow-up and a wait and see policy is advocated till recurrence is noted. However, for a pathological diagnosis of Ackerman[3] type 3 unicystic ameloblastoma, resection in the forms of partial maxillectomy, marginal, or segmental resection of mandible is recommended. The rationale for treatment without an incisional biopsy is that a small tissue may not reflect all types of Ackerman unicystic ameloblastoma; thus, the chance of under diagnosis is high.[3] Therefore, we support the concept Carnoy's solutions application for 3 min following enucleation and extraction of closely related teeth.
Conclusion
Oral health care providers should be aware of the unilocular radiolucencies of the jaws as this lesion could be UA. Timely intervention and conservative surgical treatment followed by application of Carnoy's solution and the extraction of closely related teethmay improve treatment outcome and potential complications associated with larger resection.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Robinson L, Martinez MG. Unicystic Ameloblastoma: A Prognostic Distinct Entity. Cancer. 1977;40:2278–85. doi: 10.1002/1097-0142(197711)40:5<2278::aid-cncr2820400539>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 2.Isacsson G, Andersson L, Forsslund H, Bodin I, Thomsson M. Diagnosis and treatment planning of unicystic ameloblastoma. Int J Oral Maxillfac Surg. 1986;15:759–64. doi: 10.1016/s0300-9785(86)80119-3. [DOI] [PubMed] [Google Scholar]
- 3.Ackermann GL, Altini M, Shear M. The unicystic ameloblastoma: A clinicopathological study of 57 cases. J Oral Pathol. 1988;17:541–6. doi: 10.1111/j.1600-0714.1988.tb01331.x. [DOI] [PubMed] [Google Scholar]
- 4.Rosenstein T, Pogrel MA, Smith RA, Regezi JA. Cystic ameloblastoma- Behaviour and treatment of 21 cases. J Oral Maxillofac Surg. 2001;59:1311–6. doi: 10.1053/joms.2001.27522. [DOI] [PubMed] [Google Scholar]
- 5.Kahn MA. Ameloblastoma in young persons: A clinicopathologic analysis and etiologic investigation. Oral Surg. 1989;67:706. doi: 10.1016/0030-4220(89)90013-3. [DOI] [PubMed] [Google Scholar]
- 6.Worth HM. Benign tumors of jaw. 1st ed. Chicago: Year Book Medical Publisher; 1963. Principles and practice of oral radiologic interpretations; pp. 476–546. [Google Scholar]
- 7.Philipsen HP, Reichart PA. Unicystic ameloblastoma.A review of 193 cases from the literature. Oral Oncol. 1998;34:317–25. doi: 10.1016/s1368-8375(98)00012-8. [DOI] [PubMed] [Google Scholar]
- 8.Navarro CM, Principi SM, Massucato EM, Sposto MR. Maxillary unicystic ameloblastoma. Dentomaxillofac Radiol. 2004;331:60–2. doi: 10.1259/dmfr/32974609. [DOI] [PubMed] [Google Scholar]
- 9.Ghom A. Textbook of oral medicine and oral radiology. 1st ed. Amsterdam: Elsevier Publishing; 2005. Odontogenic tumors; p. 239. [Google Scholar]
- 10.Nakamura N, Higuchi Y, Mitsuyasu T, Sandra F, Ohishi M. Comparison of long term result between different approaches of ameloblastoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:13–20. doi: 10.1067/moe.2002.119517. [DOI] [PubMed] [Google Scholar]
- 11.Holland PS, Mellor WC. The conservative treatment of ameloblastoma using diathermy or cryosurgery. A 29 year review. Int J Oral Surg. 1981;10:32–6. [PubMed] [Google Scholar]
- 12.Lee PK, Samman N, Ng IO. Unicystic ameloblastoma- Use of Carnoy's solution after enucleation. Int J Oral Maxillofac Surg. 2004;33:263–7. doi: 10.1006/ijom.2003.0496. [DOI] [PubMed] [Google Scholar]
- 13.Recurrence related to treatment modalities of unicystic ameloblastoma: A systematic review. Int J Oral Maxillofac Surg. 2006;35:681–90. doi: 10.1016/j.ijom.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 14.Frerich B, Cornilious CP, Wietholter H. Critical time of exposure of rabbit inferior alveolar nerve to Carnoy's solution. Int J Oral Maxillofac Surg. 1994;52:599–606. doi: 10.1016/0278-2391(94)90098-1. [DOI] [PubMed] [Google Scholar]


