Abstract
Herein we report treatment for a 19-year-old female patient with severe osteoarthritis of the temporomandibular joint. The patient had severe open bite with a Class II molar relationship. She had limited mouth opening and pain. Clinical examination and magnetic resonance imaging revealed that she had anterior disc displacement without reduction. By splint therapy, limited mouth opening and pain was eliminated, but an anterior open bite developed after the treatment. By orthodontic treatment, an acceptable occlusion was achieved with a Class I molar relationship.
Keywords: Anterior open bite, disc displacement without reduction, orthodontic treatment, splint therapy, temporomandibular disorders
Introduction
Arthritis means inflammation of the articular surfaces of the joint. Several types of arthritides can affect the temporomandibular joint (TMJ). The most common causative factor of arthritis is generally thought to be the mechanical overloading of the articular structures of the joint. When the precise cause of osteoarthritis can be defined, the condition is referred to as secondary osteoarthritis. When the cause of the arthritic condition cannot be determined, it is referred to as primary osteoarthritis.[1] A strong association between disc displacements, in particular, without reduction and osteoarthritis has been demonstrated both in autopsy studies and clinical studies. Therefore, it is widely assumed that disc displacement can lead to osteoarthritis.[2] The patient usually reports joint pain aggravated by mandibular movement. Limited mandibular opening is characteristic because of the joint pain. Crepitation can typically be felt. Lateral and posterior palpation of the condyle increases the pain. The diagnosis is usually confirmed by TMJ radiographs. As mechanical overloading is the causative factor, treatment should attempt to decrease this loading. Using occlusal appliances (anterior positioning or stabilization) is indicated to decrease the loading force. Sometimes after the symptoms have resolved, the sequela of the disorder may need to be treated. If significant amounts of the bony structure have been lost, the posterior teeth begin to contact heavily. These teeth act as fulcrums by which the mandible rotates, collapsing posteriorly and opening anteriorly. The result is an anterior open bite.
This case report describes the multidisciplinary treatment of a temporomandibular disorder (TMD) patient with anterior open bite.
Case Report
A 19-year-old female patient presented to our clinic with a chief complaint of limited mouth opening and severe pain in TMJ area. The complaints of the patient started 2 years before with the luxation of the mandible for 5 minutes, while eating a sandwich. Then, a soft appliance was fabricated by her dentist. As the pain gradually increased, the patient needed to use analgesics. Then, the patient was referred to University Clinics for limitation during mouth opening. She was clinically evaluated by using research diagnostic criteria for temporomandibular disorders (RDC/TMD).[3] She had a dysfunctional pain score, and the pain was aggravated by chewing, eating and yawning. Maximum mouth opening was 30 mm with pain in both TMJs. Lateral movement was 6 mm and protrusive movement was 5 mm. The palpation of the extraoral and intraoral muscles showed moderate to severe pain for 10 pairs of muscles. Severe pain was determined by palpation of the joints.
Splint therapy
Because of the limited mouth opening, the impression of the teeth could not be taken in the first rendezvous. So, a nonsteroid anti-inflammatory agent and a muscle relaxant were prescribed for 10 days. Also, the patient was advised to have magnetic resonance imaging (MRI) of TMJs. Evaluation of the MRI showed that the patient had disc displacement without reduction and an increase of inflammation of both TMJs. Ten days later, as the pain decreased, the impressions could be taken. Then, a hard stabilization splint with 3 mm thickness was constructed for the patient. The recalls were good for 1, 7 and 15 days after the delivery of the splint, but in 30 days, the contacts of the mandibular anterior teeth disappeared. The gap was closed by adding acrylic resin. But the gap occurred gradually in all appointments and was closed by adding acrylic resin for 5 months.
Examination of the patient with RDC/TMD was repeated after 6 months and the pain was completely disappeared. Maximum mouth opening was 48 mm, lateral movement was 8 mm and protrusive movement was 7 mm without pain. But a fine crepitus with mandibular movements in both TMJs was determined. Palpation of extraoral and intraoral muscles showed no pain except for mild pain in the body of left masseter muscle. Also, no pain was shown by palpation of the joints. Besides these positive results, a negative result, that is, an anterior open bite developed after the treatment. After 6 months, the patient gave up using splint. The patient was followed up 6 months for any reversal. As there was no reversal, the patient was informed about the treatment for anterior open bite. She refused to have any surgical treatment and an orthodontic treatment was planned.
The clinical examination and diagnostic blood tests did not reveal rheumatoid arthritis. [The criteria such as morning stiffness, arthritis of three or more joint areas, hand joint involvement, symmetric arthritis and rheumatoid nodules were not present. Serum rheumatoid factor, anti-cyclic citrullinated peptide antibody (anti-CCP), antinuclear antibody (ANA) and anti-ds DNA were all negative. Sedimentation and C-reactive protein (CRP) were in normal range.
Orthodontic treatment
The patient had a severe open bite with a Class II molar and canine relationship at the time of the initial examination [Figures 1 and 2]. The vertical craniofacial morphology was mesofacial type with facial symmetry. Overjet and overbite were +6.2 mm and –3.8 mm, respectively. Orthodontic anamnesis revealed that she had occlusal contacts between all the upper and lower teeth before TMD. Cephalometric analysis indicated a tendency for skeletal Class II malocclusion with a slightly retruded mandible. Labio-lingual inclinations of the maxillary and mandibular incisors were almost normal. After the splint therapy, occlusal reconstruction by use of an upper and lower multibracket appliance was begun. Orthodontic treatment was started using 0.018 × 0.025 inch slot Time 2 straightwire brackets, and very light and continuous forces were applied with 0.014 inch NiTi archwires during the initial leveling to minimize mechanical loading on the TMJ as much as possible [Figures 3 and 4]. After leveling, 0.016 × 0.022 inch NiTi and stainless steel archwires were placed for alignment. After leveling and aligning of both dentitions, 0.016 × 0.022 inch Reverse curve NiTi and 0.016 × 0.022 inch Reverse curve stainless steel upper and lower archwires were used for the upper and lower dentitions, respectively, with the use of short Class II up and down elastics at the anterior part to prevent anterior intrusion and flaring and to control the occlusal plane. Detailing was done with 0.016 × 0.016 inch stainless steel archwires and up and down elastics and Class II type zigzag elastics for 24 hours to settle the occlusion until debonding. After 16 months of treatment, an acceptable occlusion was achieved without any TMD symptoms [Figures 5 and 6]. Overjet and overbite improved to +2.1 mm and +2.5 mm, respectively [Figures 7–9]. Cephalometric analyses indicated a counterclockwise rotation of the mandible. The retention phase was accomplished using upper and lower fixed lingual retainers. After 2 years of retention, acceptable occlusion was maintained without any relapse and recurrence of any TMD symptoms, indicating a long-term stability of occlusion and TMJ components [Figure 10].
Figure 1.

Frontal view of malocclusion from severe condylar bone loss
Figure 2.

Lateral view of malocclusion from severe condylar bone loss
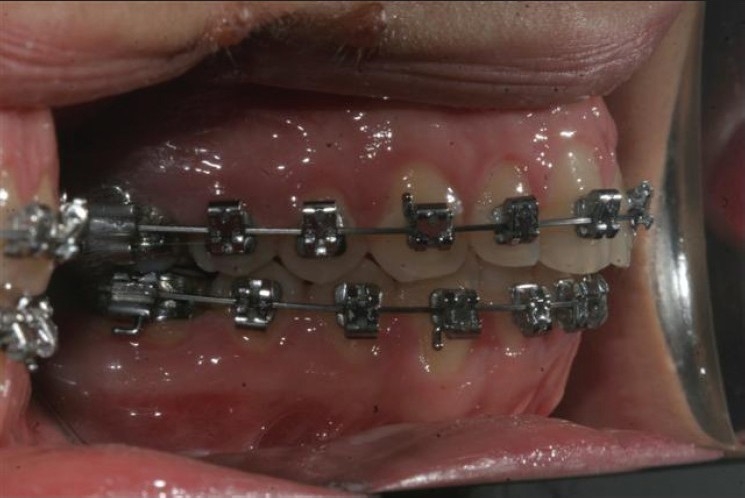
Figure 3.

Frontal view of orthodontic brackets and wires before treatment
Figure 4.

Lateral view of orthodontic brackets and wires before treatment
Figure 5.
Frontal view of finished leveling of the dentition
Figure 6.

Finished leveling of the dentition
Figure 7.

Frontal view of achived occlusion after treatment
Figure 9.

Lateral view of achived occlusion after treatment (right)
Figure 10.

Intraoral view after 2 years
Figure 8.

Lateral view of achived occlusion after treatment (left)
Discussion
The patient had severe deformation of the mandibular condyle and an increase of inflammation of both TMJs with a diagnosis of disc displacement without reduction before treatment. For the treatment of disc displacement without reduction, splint therapy and surgical procedures such as arthrocentesis or disc repositioning by open surgery are the choices. As our patient refused all surgical procedures, either invasive or noninvasive, we planned non-surgical treatment modalities.
Stabilization splints are preferred for decreasing the loading force to the condyle and to protect from resorption. They have no effect to reposition the disc on condyle, but allow the retrodiscal tissue to produce a pseudodisc where the condyle can function without any limitation and pain. As the chief complaint of the patient was pain and limitation during mouth opening, we first attempted to solve these problems. After initial medical and splint therapy, the complaints disappeared, but the patient had an anterior open bite as a new complaint. Remodeling of the condyle sometimes causes an open bite because of the subsequent decrease in ramus height.[4,5] Open bite related to condylar resorption almost exclusively affects women. Its exact etiology and pathogenesis remain unclear. It has been associated with rheumatoid arthritis, TMJ internal derangement, condylar fractures, connective tissue or autoimmune diseases, orthodontic treatment, and orthognathic surgery. In most cases, however, there is no identifiable precipitating event; hence, the term “idiopathic condylar resorption” is used for this condition. The female predisposition to this condition may be attributed to the influence of estrogen and prolactin on the bone response.[6] Treatment of this problem is controversial. Condylectomy and reconstruction with costochondral graft offer definitive management of active idiopathic condylar resorption.[6–9]
After initial medical and splint therapy, orthodontic treatment was the choice of our patient. An acceptable occlusion was maintained without recurrence of any TMD symptoms, indicating a long-term stability of occlusion and TMJ components. Tanaka et al.[10] used a multibracket appliance for a similiar case and concluded that their method could be a new therapeutic approach to TMD patients.
Conclusion
In conclusion, a patient with severe TMD symptoms and a progressive condyle resorption can be treated with a multidisciplinary approach and noninvasively.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Okeson JP. St. Louis: Elsevier Inc; 2008. Management of temporomandibular disorders and occlusion. [Google Scholar]
- 2.Laskin DM. Chicago: Quintessence Publishing Co Inc; 2006. Temporomandibular disorders an evidence-based approach to diagnosis and treatment. [Google Scholar]
- 3.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and spesifications, critique. J Craniomandib Disord Facial Oral Pain. 1992;6:301–55. [PubMed] [Google Scholar]
- 4.Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption: Part I. Am J Orthod Dentofacial Orthop. 1996;110:8–15. doi: 10.1016/s0889-5406(96)70081-1. [DOI] [PubMed] [Google Scholar]
- 5.Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption: Part II. Am J Orthod Dentofacial Orthop. 1996;110:117–27. doi: 10.1016/s0889-5406(96)70099-9. [DOI] [PubMed] [Google Scholar]
- 6.Papadaki ME, Tayebaty F, Kaban LB, Troulis MJ. Condylar resorption. Oral Maxillofac Surg Clin North Am. 2007;19:223–34. doi: 10.1016/j.coms.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Huang YL, Pogrel MA, Kaban LB. Diagnosis and management of condylar resorption. J Oral Maxillofac Surg. 1997;55:114–9. doi: 10.1016/s0278-2391(97)90222-6. [DOI] [PubMed] [Google Scholar]
- 8.Bilodeau JE. Retreatment of a patient who presented with condylar resorption. Am J Orthod Dentofacial Orthop. 2007;131:89–97. doi: 10.1016/j.ajodo.2004.11.040. [DOI] [PubMed] [Google Scholar]
- 9.Wolford LM, Cardenas L. Idiopathic condylar resorption: Diagnosis, treatment protocol, and outcomes. Am J Orthod Dentofacial Orthop. 1999;116:667–77. doi: 10.1016/s0889-5406(99)70203-9. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka E, Kikuchi K, Sasaki A, Tanne K. An adult case of TMJ osteoarthrosis treated with splint therapy and the subsequent orthodontic occlusal reconstruction: Adaptive change of the condyle during the treatment. Am J Orthod Dentofacial Orthop. 2000;118:566–71. doi: 10.1067/mod.2000.93966. [DOI] [PubMed] [Google Scholar]


