Abstract
Background:
Hidradenitis suppurativa is a chronic skin condition involving the apocrine glandular zones. Affected patients may present with acute abscesses, but the condition often progresses to a chronic state with persistent pain, sepsis, sinus tract, fistula formation, purulent discharge, and dermal scarring. The treatment of patients with severe disease can be difficult and may require complex surgical intervention.
Materials and Methods:
For this study, we selected 30 patients from the outpatient department. The patients were divided into two groups of 15 patients each. In patients of group I, oral acitretin 0.5 mg/kg body weight was given alone. Oral acitretin was given for a period of 12 weeks, and follow-up of the patients was done every 4 weeks for a period of 6 months. In patients of group II, oral acitretin 0.5 mg/kg was given plus a wide surgical excision was done.
Results and Discussion:
In our study, the commonest site of involvement of hidradenitis suppurativa was axilla in 83.3% patients, perineum was involved in 13.3% patients, and periumbilical involvement was seen in 3.3% patients. The commonest clinical feature was nodules seen in 90% patients; pain was seen in 60% patients, dermal scarring in 73.3% patients, malodorous discharge in 33.3% patients, abscess in 30% patients, and fistulous tracts were seen in 20% patients. The recurrence rate was low (20%) in group II patients in whom oral acitretin was given plus surgical excision was done as compared with group I (40%) in whom oral acitretin was given alone.
Keywords: Abscess, hidradenitis suppurativa, recurrent, scarring, sinus tract, surgical excision
Introduction
Hidradenitis suppurativa is a chronic recurrent inflammatory process involving apocrine sweat glands and adjacent connective tissue.[1] If diagnosed and treated early, hidradenitis suppurativa can be managed by medical measures. In more severe cases, surgical intervention is the only treatment that has any significant effect on the course of the condition.[2]
Materials and Methods
For this study, we selected 30 patients from the outpatient department. The patients were divided into two groups of 15 patients each. In patients of group I, oral acitretin 0.5 mg/kg body weight was given alone. Oral acitretin was given for a period of 12 weeks, and follow-up of the patients was done every 4 weeks for a period of 6 months. In patients of group II, oral acitretin 0.5 mg/kg was given plus a wide surgical excision was done. Regarding the surgical management, local excision of the sinus tracts with direct primary suture was done. Informed consent was obtained from all patients and a prior approval of the hospital's ethical committee was taken for the study. Routine investigations were performed, including complete blood profile, fasting blood sugar, erythrocyte sedimentation rate, urine complete examination, and liver and kidney function tests.
Results
The data were collected [Tables 1 and 2] and the results were analyzed.
Table 1.
Clinical features of hidradenitis suppurativa
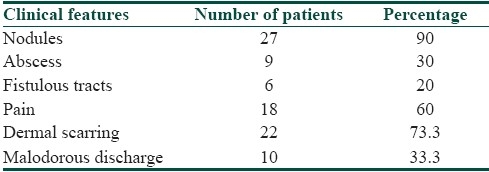
Table 2.
Recurrence rates in the two groups

Discussion
The commonest age group involved was 11-20 years (46.6%), followed by 30% patients in the age group of 11-20 years, 16.6% patients between 31 and 40 years, and 3.3% patients between 41 and 50 years. Females outnumbered males, and the female/male ratio was 2.3:1. A positive family history was seen in 30% patients. The duration of the disease was less than 6 months in 10% patients, between 6 and 12 months in 36.6% patients, between 13 and 24 months in 40% patients, and more than 24 months in 13.3% patients. The commonest site of involvement of hidradenitis suppurativa was axilla in 83.3% patients, perineum was involved in 13.3% patients, and periumbilical involvement was seen in 3.3% patients. The commonest clinical feature [Table 1] was nodules seen in 90% patients, pain in 60% patients, dermal scarring in 73.3% patients, malodorous discharge [Figure 1] in 33.3% patients, abscess in 30% patients, and fistulous tracts [Figure 2] were seen in 20% patients. The recurrence rate was low (20%) in group II patients in whom oral acitretin was given plus surgical excision was done as compared with group I (40%) in whom oral acitretin was given alone [Table 2].
Figure 1.

Multiple discharging sinuses from the axilla in a 36-year-old female
Figure 2.

Contractures, scarring, and sinus tract formation in a 50-year-old male
Treatment options include systemic tetracyclines or macrolide antibiotics in doses similar to those given for acne.[3] Acitretin has been shown to lead to sometimes dramatic responses in a number of patients. When medical treatments fail, surgery is the only alternative. Local excision of sinus tracts, when used as an alternative to wide ablative en bloc excision, is associated with a higher recurrence rate but a lower morbidity rate.[4,5] When the disease has become chronic and extensive, most authors agree that removal of the affected area and the adjacent apocrine glandular zone for a distance of 2 cm beyond the diseased portion is the best option if the likelihood of recurrence is to be minimized.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Jemec GB, heidenheim M, Nielsen NH. The prevalence of hidradenitis suppurativa and its potential precursor lesions. J Am Acad Dermatol. 1996;35:191–4. doi: 10.1016/s0190-9622(96)90321-7. [DOI] [PubMed] [Google Scholar]
- 2.Parks RW, Parks TG. Pathogenesis, clinical features and management of hidradenitis suppurativa. Ann R Coll Surg Engl. 1997;79:83–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Slade DE, Powell BW, Mortimer PS. Hidradenitis suppurativa: Pathogenesis and management. Br J Plast Surg. 2003;56:451–61. doi: 10.1016/s0007-1226(03)00177-2. [DOI] [PubMed] [Google Scholar]
- 4.Hogan DJ, Light MJ. Successful treatment of hidradenitis suppurativa with acitretin. J Am Acad Dermatol. 1988;19:355–6. doi: 10.1016/s0190-9622(88)80251-2. [DOI] [PubMed] [Google Scholar]
- 5.Rhode JM, Burke WM, Cederna PS, Haefner HK. Outcomes of surgical management of stage iii vulvar hidradenitis suppurativa. J Reprod Med. 2008;53:420–8. [PubMed] [Google Scholar]


