Abstract
To emphasize that solitary hydatid cyst can be localized in the soft tissue and present as a soft tissue mass even in an unusual site like face, we report the case of a 42-year-old male patient presenting with a slowly growing mass in right temporal region. Computed tomography (CT) scan showed an encapsulated mass with multiple cysts. Histopathological examination revealed the characteristic findings, which were consistent with soft-tissue hydatid disease. In the absence of visceral organ involvement, this is the first reported case of a primary subcutaneous hydatid cyst in the skin of face in India. In the English literature, only one case of this kind has been reported till date. When imaging methods confirm cystic nature of a swelling, even in unusual sites, one should always keep a possibility of hydatid cyst and manage accordingly during surgery to avoid precipitation of acute anaphylaxis.
Keywords: Cyst, face, hydatid, solitary, subcutaneous
Introduction
Echinococcus granulosus, a cestode, is the causative parasite of the cyclozoonotic infection, hydatid disease. Echinococcus require two mammalian hosts for completion of its life cycle. Dog is the primary host. Intermediate hosts are sheep, cattle, horses and occasionally man. The endemic regions of human cystic hydatid disease are the cattle and sheep raising areas of the southern parts of South America, the Mediterranean region, the Middle East, many parts of Africa, southern and central Russia, Central Asia and many regions of China.[1,2]
E. granulosus has a definitive host that harbors the adult worm in its intestinal tract, whereas the intermediate host carries the larval stage in its internal organs. Humans acquire the infection by ingesting eggs of E. granulosus in contaminated food as a result of close contact with dogs and sheep. The eggs hatch in the intestinal mucosa and the larvae penetrate the mucosa, reaching the liver through the portal vein. The larvae are then trapped in the sinusoids, where they develop into one or several unilocular cysts. The most frequently involved organs are the liver (70%) and lung (20%). Besides systemic dissemination through the portal vein, the larvae also can disseminate through lymphatic channels. Other organs, muscle (5%), spleen (1%), bones (3%), kidneys (2%), heart (1%), pancreas (1%) and central nervous system (1%) are involved only rarely.[3,4]
Even in the countries where Echinococcus infestation is endemic, occurrence of hydatid cyst in the face is very rare. In the head and neck region, few case reports of hydatid cysts involving the parotid gland, parapharyngeal space, infratemporal fossa, maxillary sinus and pterygopalatine fossa have been reported in the literature.[5] Till date, only one case of hydatid cyst has been reported involving the subcutaneous tissue of the face primarily without any other site involvement.[6]
We present the first case in India with hydatid cyst manifesting in temporal region. This case reminds our clinicians to consider this disease in the differential diagnosis even in the absence of visceral involvement and any indicator of hydatid disease, when dealing with the cysts of the head and neck region.
Case Report
A 45-year-old man working in navy presented to our institute with the complaint of painless, gradually increasing swelling in the right temporal region for the last two years. Clinical examination revealed swelling to be cystic and fluctuant on palpation. It was a 6.2×3.5 cm subcutaneous swelling not adherent to the underlying bone [Figure 1]. The medical and medication history was noncontributory. No other family member had any such complaints.
Figure 1.

Photograph showing swelling in right temporal region on face
Computed tomography demonstrated an extracranial, oval complex cystic lesion in right temporal and infratemporal region. The lesion showed mild enhancement of its walls and was extending along the right temporalis muscle [Figure 2]. Based on these findings, possibility of dermoid cyst was considered. Fine needle aspiration biopsy (FNAB) was performed. Smears were paucicellular with proteinaceous background. A diagnosis of benign cystic lesion was rendered on FNAB. Other routine hematological investigations and plain chest radiograph were normal. Surgery was done under general anesthesia; circular incision was given around the margin of the cyst over the scalp. The mass was dissected from the surrounding structures and excised totally. Fortunately, the integrity of the capsule was maintained and there was no spillage of cyst fluid into the surrounding structures.
Figure 2.
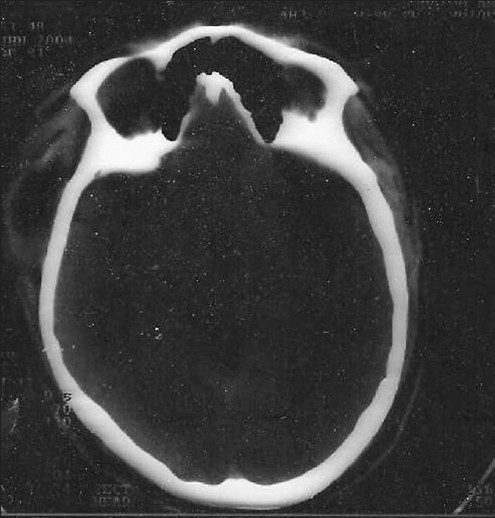
CT scan showing cystic lesion with septations in right temporal region
The mass was examined histopathologically. Grossly, there were multiple cysts measuring from 1.5 to 3.0 cm in diameter. On cutting, all the cysts were unilocular, filled with clear fluid and had tiny vesicular projections on their inner surface.
On microscopic examination, a lamellated ectocyst with germinative endocyst conforming to morphology of hydatid cyst was demonstrated. The patient was subjected to ultrasonography of the abdomen with CT scan of the thorax, to exclude the possibility of invasion of any of the visceral organs. But, surprisingly, the investigations did not reveal any other organ involvement by the disease process. Patient was given medical treatment with albendazole (800 mg/d) for six weeks. After 22 months of surgery, the patient has no complaints and is disease free.
Discussion
Hydatid cysts in the head and neck region have been reported only infrequently even in endemic areas. Intestinal parasite infections of the maxillofacial region account for only about 2% of hydatid infections of the body.[2] Hydatid cysts are not usually considered in the differential diagnosis of head and neck cystic swellings, especially in non-endemic areas in the absence of hydatid disease elsewhere in the body. The rarity of the disease in this anatomical location presents a diagnostic difficulty for the physician if he or she is not familiar with the disease.
Echinococcal disease may affect humans. Man can serve as an intermediate host, who may acquire the infection either by direct contact with the definitive host like dog, or by ingestion of food or fluids contaminated with ova of E. granulosus from canine faeces.[7] Hence, a detailed questionnaire about patient's occupation, patients residence and family history may suggest a diagnosis of hydatid disease in the differential diagnosis. The ova enter and hatch as embryos in the human intestinal tract. Most larvae usually settle in the liver and lung but the embryos may escape the portal circulation and enter the systemic circulation or the lacteal duct to spread more generally throughout the body. As most of the larvae settle in liver and lung, patients with echinococcosis in any part of the body must undergo thorough systemic investigation. Multiorgan involvement is found to be as high as 20% to 30%. The liver is always involved in multiple organ infections in addition to other organs or tissues.[8] Our patient did not had any evidence of hydatid disease elsewhere in the body, neither at the time of presentation nor on postoperative diagnostic imaging. The solitary occurrence of hydatid cysts has been confirmed by other authors.[2,5,9]
Clinically, signs and symptoms of this disease depend on the anatomic location, size, and pressure caused by the enlarged cyst. But, this type of clinical presentation is also characteristic of any slowly growing benign tumor in the body. Due to these factors, the nature of the signs and symptoms produced by hydatid cysts are extremely variable and never pathognomic.[3,6] In the present case, cyst was located on face and the major worry of the patient was disfiguration of the face outline.
We performed FNAB as we had no clue of a possible diagnosis of a hydatid cyst. However, use of FNAB as a diagnostic tool has not been favored because of the potential to precipitate acute anaphylaxis or to spread daughter cysts.[7] Fortunately, there was no anaphylaxis in our case. FNAB smears made from aspirated cyst fluid may show scolices, hooklets, or remnants of laminated membrane.[4] However, we could not demonstrate any of these on FNAB results and with the possibility of benign cystic disease, the case was subjected to surgical excision.
Peripheral blood smear may show marked eosinophilia in 30% cases. Serological tests, including latex agglutination, indirect hemagglutination, and enzyme-lined immunosorbent assay, have been widely used to facilitate the diagnosis. However, diagnostic sensitivity and specificity of all serological tests is low. Importance of these tests is mainly in the follow up of patients on treatment.[2,8]
Imaging techniques remain more sensitive than serodiagnosis, the diagnosis of hydatid disease has been greatly facilitated with the use of USG, CT, and magnetic resonance imaging. These techniques can demonstrate the daughter cysts, vesicles and internal septae in these avascular cysts. Complexity or the presence of any solid component can also be visualized correctly.[3,4] Although CT scan was done in the present case, exact characterization could not be done and the report was suggestive of benign cyst. Hence, we performed FNAB in the involved site.
Treatment of choice for hydatid cyst is surgical removal. When the presurgical diagnosis of hydatid cyst is made, surgeon should take care of three things. (1) Inactivation of daughter cysts and scolices prior to surgery by injecting 20% hypertonic saline solution or 0.5% sliver nitrate into the cyst. (2) No spillage of cyst contents during surgery to avoid anaphylactoid reaction, recurrence and multiple hydatidosis. (3) Complete removal of the cyst including the innermost germinative layer, which can produce scolices, if left out.[5,9] There was complete cyst removal with no rupture and spillage of cyst contents in the present case. After 22 months of surgery, the patient has no evidence of recurrence and is completely disease and symptom free.
Drug therapy alone has been preferred in patients with poor general condition who cannot tolerate surgical procedure, multiple organ involvement or cyst located in inaccessible site.[2] We treated the present case with albendazole for six weeks post operatively.
In recent reports, percutaneous treatment of abdominal and pulmonary hydatid cyst has been reported as an alternative to surgery. Results have shown less recurrence and lower morbidity and mortality rates.[10] However, this technique has not been preferred and used widely for head and neck hydatid cysts.
The present case report reminds us (1) To bear in mind the differential diagnosis of hydatid cyst while dealing with the cysts of head and neck region. Although rare, hydatid cyst can present as a slowly growing cystic mass even on face. (2) Imaging techniques, though sensitive for the diagnosis of a cyst, sometimes cannot pin-point the exact etiology of cystic lesion (3) FNAB of a cyst located on face may cause anaphylactic reaction and one should always be prepared for the consequent emergency. (4) During surgical removal of cysts in which no definite etiology has been made preoperatively, great care must be taken to avoid spilling of the cystic contents.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev. 2004;17:107–35. doi: 10.1128/CMR.17.1.107-135.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eroğlu A, Atabekoğlu S, Kocaoğlu H. Primary hydatid cyst of the neck. Eur Arch Otorhinolaryngol. 1999;256:202–4. doi: 10.1007/s004050050140. [DOI] [PubMed] [Google Scholar]
- 3.Kireşi DA, Karabacakoğlu A, Odev K, Karaköse S. Uncommon locations of hydatid cysts. Acta Radiol. 2003;44:622–36. doi: 10.1080/02841850312331287749. [DOI] [PubMed] [Google Scholar]
- 4.Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A. Hydatid disease from head to toe. Radiographics. 2003;23:475–94. doi: 10.1148/rg.232025704. [DOI] [PubMed] [Google Scholar]
- 5.Gangopadhyay K, Abuzeid MO, Kfoury H. Hydatid cyst of the pterygopalatine-infratemporal fossa. J Laryngol Otol. 1996;110:978–80. doi: 10.1017/s0022215100135509. [DOI] [PubMed] [Google Scholar]
- 6.Ozturk, Serdar Hydatid cyst in the soft tissue of the face without any primary. Ann Plast Surg. 2001;46:170–3. doi: 10.1097/00000637-200102000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Sennaroglu L, Onerci M, Turan E, Sungur A. Infratemporal hydatid cyst: Unusual location of echinococcosis. J Laryngol Otol. 1994;108:601–3. doi: 10.1017/s0022215100127562. [DOI] [PubMed] [Google Scholar]
- 8.Aletras H, Symbas N. Hydatid disease of the lung. In: Shields TW, LoCicero J, Ponn RB, editors. General Thoracic Surgery. 5th ed. Philadelphia: Lippincott Williams and Wilkins; 2000. pp. 1113–22. [Google Scholar]
- 9.Akal M, Kara M. Primary hydatid cyst of the posterior cervical triangle. J Laryngol Otol. 2002;116:153–5. doi: 10.1258/0022215021909953. [DOI] [PubMed] [Google Scholar]
- 10.Akhan O, Ensari S, Ozmen M. Percutaneous treatment of a parotid gland hydatid cyst: A possible alternative to surgery. Eur Radiol. 2002;12:597–9. doi: 10.1007/s003300100972. [DOI] [PubMed] [Google Scholar]


