Abstract
Objectives:
The aim of this study is to evaluate the efficacy and tolerability of Sudarshan Kriya Yoga (SKY) course in generalized anxiety disorder (GAD) outpatients, who after eight weeks of an appropriate dose of traditional therapy had not yet achieved remission.
Subjects:
The adult participants (18-65 years) were outpatients with a primary diagnosis of GAD with or without comorbidities on the Mini-International Neuropsychiatric Interview (MINI). Participants had a minimum of eight weeks standard treatment with an appropriate dose of a standard prescription anxiolytic, a clinician global impression-severity (CGI-S) score of 5-7, a Hamilton anxiety scale (HAM-A) total score ≥20 including a score of >2 on the anxious mood and tension items.
Materials and Methods:
Forty-one patients were enrolled in an open-label trial of the SKY course as an adjunct to standard treatment of GAD at the START Clinic for Mood and Anxiety Disorders, a tertiary care mood and anxiety disorder clinic in Toronto. The SKY course was administered over five days (22 h total). Subjects were encouraged to practice the yoga breathing techniques at home for 20 min per day after the course and were offered group practice sessions for 2 h once a week led by certified yoga instructors. The primary outcome measure was the mean change from pre-treatment on the HAM-A scale. Psychological measures were obtained at baseline and four weeks after completing the intervention.
Results:
Thirty-one patients completed the program (mean age 42.6 ± 13.3 years). Among completers, significant reductions occurred in the pre- and post-intervention mean HAM-A total score (t=4.59; P<0.01) and psychic subscale (t=5.00; P≤0.01). The response rate was 73% and the remission rate 41% as measured on the HAM-A.
Conclusion:
The results of this small pilot trial suggest that the SKY course represents a potentially valuable adjunct to standard pharmacotherapy in patients with GAD or treatment-resistant GAD, and warrants further investigation. In particular, changes in worry and body symptoms showed significant improvements that may further our understanding of the mechanism of change in the tolerance of anxiety and worry.
Keywords: Anxiety, cognitive behavioral therapy, generalized anxiety disorder, mindfulness based stress reduction, post-traumatic stress disorder, yoga
INTRODUCTION
Anxiety disorders are among the most prevalent psychiatric conditions in the United States, as indicated by a lifetime prevalence of 28.8%[1] and a 12-month prevalence rate of 18.1%.[2] It is estimated that the cost of care for anxiety disorders was $42.3 billion US in 1990.[3] Direct costs of care include hospitalizations, emergency room visits, prescription drugs, and counseling, whereas indirect costs include absenteeism from work or school, reduced productivity, unemployment, substance abuse/addiction often as ‘self-medication,’ and even suicide.[4]
Generalized anxiety disorder (GAD), with a one-year prevalence of approximately 3% and a lifetime prevalence of 5%,[5] has the potential to cause serious interference with a person's daily living.[6] By definition, GAD is characterized by excessive anxiety and worry that lasts for at least six months and is associated with three or four or more of the following symptoms: restlessness, being easily fatigued, difficulty in concentrating, irritability, muscle tension, and sleep disturbance.[5] Excessive and uncontrollable worry is a core feature of GAD.[5] The content of worry is often about the individuals’ health, health of their significant others, personal finances and the future.[5]
The age of onset for GAD is often prior to age 20 and women are more likely to be diagnosed than men.[7] This disorder also exhibits a high degree of chronicity, and is often complicated by a high prevalence (45-91%) of comorbidity with other psychiatric and/or medical conditions including panic disorder, agoraphobia, social phobia, major depressive disorder, and dysthymia,[8,9] as well as a variety of cardiovascular, gastrointestinal and respiratory diseases.[7] Relapse rates are fairly high for people suffering with GAD with two thirds of patients suffering a recurrence within one-year.[10]
Current pharmacotherapeutic options for GAD include antidepressants such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRI) e.g., venlafaxine, O-desmethyl-venlafaxine, duloxetine, milnacipran, buspirone, hydroxyzine, benzodiazepines,[11] low-dose anti-psychotics, and pregabalin.[12] Nevertheless, all pharmacological treatments for GAD can cause troublesome side effects, including nausea, sexual dysfunction, and weight gain for the antidepressants[13,14] and anterograde memory impairment, sedation and the risk of dependence with benzodiazepines, which are, therefore, not recommended for long-term use.[15] Response to these treatments tends to be highly variable, ranging from 40% to 70%.[16–19] Furthermore, limits in terms of efficacy and tolerability often result in poor patient adherence to medication and thus, long-term remission is often difficult to achieve.[20] On average, only a third of GAD patients achieve remission within a year of follow-up, while patients who do achieve an initial response often relapse.[21]
A variety of nonpharmacological treatments are available, and a great deal of evidence supports the use of cognitive behavioral therapy (CBT) in GAD.[22] However, this form of treatment is limited by high drop-out rates and poor treatment adherence, as well as suboptimal remission rates.[23] Indeed, in two trials evaluating CBT in subjects with GAD, 16-17% had dropped out before the mid-point of treatment.[23]
Hatha yoga (in the US commonly called “yoga”) as it originated in ancient India, consists of a system of spiritual, moral and physical practices. Two central and common aspects of yoga practice today are physical postures (asanas) and breathing exercises (pranayamas). These breathing exercises aim to focus the mind, facilitate relaxation and enhance wellness. Evidence suggests that these practices result in physiological effects such as increased parasympathetic drive, calming of stress response systems, neuroendocrine release of hormones, and modulation of thalamic generators.[24] A review of the literature evaluating the different forms of yoga suggests potential beneficial effects on individuals with depressive disorders[25] as well as on anxiety, stress reduction and general well-being.[24,26–30] However, the results need to be interpreted cautiously, since the sample sizes of many of these published studies are relatively small and many are not rigorous, controlled trials.
Positive effects of yoga on stress reduction have been demonstrated with Sudarshan Kriya Yoga (SKY), also known as The Art of Living Course, sponsored by a non-profit organization, the Art of Living Foundation. SKY is a well-described yoga-based stress reduction program that has been reported to relieve severe major depression[31] and dysthymia.[32,33] In a randomized controlled study, Janakiramaiah and colleagues (2000)[31] found that the level of depression significantly decreased (68-73%) in subjects hospitalized for major clinical depression who were given one week of instruction in SKY, followed by 30 min of practice (mean of 4.5 days a week) for three weeks, and this intervention was as effective as imipramine 150 mg/day. The SKY course has also been used to treat substance abusing populations,[34] military veterans with post-traumatic stress disorder (PTSD),[35] non-military patients with PTSD,[27,36,37] and victims of war or mass disasters.[38–40] In a controlled trial of three comparison refugee groups, from the 2004 Southeast Asia tsunami, an 8-h yoga breath program with SK resulted in a 60% drop in mean scores on the post-traumatic stress checklist (PCL-17) and a 90% drop in mean scores on Beck depression inventory (BDI) in one week. Scores continued to improve at six-month follow-up.[38] Practitioners of this form of yoga are reported to have concurrent high activity of both alpha and beta waves as measured by electroencephalography (EEG), indicating simultaneous increased mental focus and relaxation.[40] A drop in blood lactate levels, with a concomitant increase in the antioxidant enzymes superoxide dismutase, catalase, and glutathione, suggests favorable effects on antioxidant status.[41]
The breathing techniques associated with SKY are all done in a sitting posture, either in a chair or on the floor with eyes and mouth kept closed while breathing through the nose. The breathing practices of the SKY program include:
-
a.
Three-Stage Pranayama with Ujjayi, also called Victory Breath or Ocean Breath
-
b.
Bhastrika or Bellow's Breath
-
c.
Sudarshan Kriya or the Rhythmic Breath Technique
-
d.
Alternate Nostril Breathing
Victory Breath (Ujjayi, Ocean Breath) uses a sound like one hears inside a seashell throughout inhalation and exhalation while breathing through the nose. The sound is created by a slight contraction of the laryngeal muscles and partial closure of the glottis. This creates airway resistance and enables control of the rate of air flow such that the breath cycle can be prolonged. Ujjayi is a slow, deep breathing technique at 4 to 6 breaths per minute. Three-Stage Pranayama with Ujjayi employs arm postures, a specific ratio for the duration of inhalation and exhalation phases, and breath-holds. During SKY, this is practiced for approximately 8 min. Ujjayi tends to be calming and to produce a sense of well-being.
Bellows breath (Bhastrika) involves forceful rapid deep breathing through the nose at a rate of 20 to 30 breaths per minute. Each set of 20 breaths is called a “Round.” Bhastrika is done in a seated position with the eyes and mouth closed. Three 1-min rounds of Bhastrika are each followed by 30 seconds of normal breathing. Arm movements are used to increase the force and depth of respiration. This breathing exercise lasts for approximately 5 min. The effects include increased ventilation, circulation, and alertness.
Rhythmic breath technique (Sudarshan Kriya or SK): The translation of Sudarshan Kriya from Sanskrit is ‘right vision through purifying action.’ SK involves rhythmic, cyclical forms of breathing in which there are no pauses between inhalation and exhalation. During the Art of Living Course, a tape recording of Sri Sri Ravi Shankar's voice is used during SK to time the breaths using the sound so-hum (‘so’ for inhale and ‘hum’ for exhale). This Long Kriya involves multiple rounds of slow (8-14 respiratory cycles per minute), medium (40-50 respiratory cycles per minute), and fast (60-100 cycles per minute) cycles with varying rhythms and intensities. The Long Kriya lasts about 30 min. The daily home practice is a Short Kriya with simpler patterns and takes approximately 10 min.
The purpose of this study is to investigate the SKY course as an adjunctive treatment for patients suffering from unremitted GAD, who were on medications and who had previously received a variety of treatments including CBT and mindfulness-based therapies (MBT). This study evaluated the addition of the SKY course to the standard treatments being given to patients suffering from GAD despite having received previous courses of standard treatments, including pharmacotherapy, CBT, MBT, and psychotherapy.
MATERIALS AND METHODS
Subjects
Subjects were enrolled in the study after being referred from practitioners at the START Clinic for Mood and Anxiety Disorders, a tertiary care clinic in Toronto. Subjects with a primary diagnosis of GAD (with or without comorbidities) as assessed using the mini-international neuropsychiatric interview (MINI) were eligible for enrollment in the study.
Patient inclusion/exclusion criteria
Patients were eligible for inclusion in the study if they were outpatients (aged 18-65 years) who provided informed consent, with a primary diagnosis of GAD according to the Diagnostic and Statistical Manual Fourth Edition Text Revision (DSM-IV-TR),[5] a minimum of eight weeks history of standard treatment with an appropriate dose of a traditional prescription anxiolytic, a clinical global impression-severity of illness (CGI-S) score of 5-7, and a Hamilton Anxiety Scale (HAM-A) total score ≥20 including a score of >2 on the anxious mood and tension items. Patients were excluded from the study if they met criteria for alcohol or drug abuse or dependence (currently or within the last six months), had mania or hypomania in the previous six months according to the MINI, a history of schizophrenia, bipolar disorder Type I, any other psychotic disorder (as defined in the DSM-IV-TR), any other serious medical condition, those having serious suicidal risk (investigator judgment), or had undertaken changes in their use of medication or therapy within two weeks of initial screening.
Study design
This was an open-label study to examine the efficacy and tolerability of the SKY course as an adjunctive therapy for GAD in outpatients who had not achieved remission (HAM-A ≤ 7) following at least eight weeks of an adequate and stable dose of conventional therapy.
Sudarshan Kriya Yoga procedure
The Sudarshan Kriya Yoga (SKY) course is a well-described, yoga-based stress reduction program usually taught over five or six consecutive days for a total of 22 h. This multi-component program includes yoga postures, advanced yoga breath techniques, brief guided meditation, self-reflection, and cognitive-based stress education and coping strategies. The instructor (RPB) is a physician and an experienced yoga teacher certified to teach the SKY course who has had more than five years experience in the presentation of similar programs internationally.
During the SKY course, Victory Breath and Bellows Breath were introduced on the first day over a 3-h training session. A 30-min balanced set of yoga stretches was learned and practiced on day 2 during a 6.5-h training session, and the Long Sudarshan Kriya practice was learned on day 3 and repeated on day 4 (10 h training over 2 days). All techniques were performed every day from day 3. The breath protocol was followed by a guided meditation, body scan, and rest. The home practice with Short Kriya was introduced on day 5. Discussion of cognitive coping and stressor evaluation strategies took place at different times throughout the course. Subjects were provided with a chart demonstrating the yoga postures to guide their home practice.
After completion of the SKY course, subjects were encouraged to practice the yoga breathing techniques at home for 20 min per day. In addition, they were offered group practice sessions for 2 h once a week led by other certified yoga instructors.
Assessments
Subjects were administered a variety of scales and test measures in the week prior and one month following the SKY course. The primary efficacy endpoint was the mean change from pre- to post- treatment on the HAM-A. The secondary efficacy endpoints were the mean changes from pre- to post- treatment in the Penn state worry questionnaire (PSWQ), anxiety sensitivity index (ASI), beck anxiety inventory (BAI), coping inventory for stressful situations (CISS; subscales for task oriented coping, emotion oriented coping, and avoidance oriented coping), beck depression inventory (BDI), intolerance of uncertainty (IUS), multidimensional perfectionism scale (MPS) subscales for self (MPSSelf), other (MPSOther), and social (MPSSocial), social phobia inventory (SPIN), and Liebowitz social anxiety scale-self report total (LSAS_SRTotal), as well as the fear and anxiety (LSAS_SRF and A) and avoidance (LSAS_SRAvoidance) subscales.
Instruments
Two of the investigators (MV and PLV) and two graduate students who were trained in the administration of the scales and instruments by MV administered the following scales and/or test instruments:
MINI: The MINI (clinician rated) (MINI CR) is a short, semi-structured diagnostic inventory for DSM-IV and International Classification of Diseases 10th Revision (ICD-10) used to explore seventeen Axis I psychiatric disorders. The MINI has good reliability and validity as compared to the Composite International Diagnostic Interview and the Structured Clinical Interview for DSM-IV (SCID), but has a much shorter format than the above mentioned and therefore, can be administered quickly and easily[42] and exhibits a high inter-rater reliability kappa of 0.98.[43]
HAM-A: The HAM-A is a 14-item test measuring overall anxiety, psychic anxiety (mental agitation, psychological distress, fears, feelings of tension, and difficulty concentrating) and somatic anxiety (physical complaints related to anxiety, for example, muscular pain, weakness, cardiovascular problems, and restlessness).[44] In anxiety studies, the definition of treatment response has been based upon a ≥50% drop in the HAM-A while the definition of remission has been based upon a score ≤7 on the HAM-A.[45]
ASI: The ASI is a self-report scale depicting the tendency to experience fear and anxiety-related symptoms.[46] It contains 16 items in response to which participants indicate how much each item applies to them using a 5-point Likert type scale ranging from 0 = ‘very little’ to 4 = ‘very much.’ The ASI has been shown to possess good reliability and validity.[47–49]
BAI: The BAI is a self-report scale designed to evaluate the severity of physical symptoms of anxiety during the previous week.[50,51] Participants rate the 21 items on a 4-point Likert type severity scale from 0 = ‘not at all’ to 3 = ‘severely, I could barely stand it.’ Total response scores range from 0 to 63, with higher scores indicating more severe anxiety. The BAI possesses adequate test-retest reliability and convergent validity.[52]
CISS: The CISS is a 48-item self-report measure that assesses how much an individual engages in various coping activities during stressful situations using a 5-point Likert scale ranging from 1 = ‘not at all’, to 5 = ‘very much.’ The CISS includes three 16-item scales that assess emotion-oriented coping (emotion scale), task-oriented coping (task scale), and avoidance (avoidance scale). The CISS has a test-retest reliability of between 0.6 and 0.7 over a period of six weeks.[53]
PSWQ: The PSWQ is a 16-item instrument that evaluates the trait of pathological worry by measuring generality, excessiveness and uncontrollability. Each item describes characteristics corresponding to an aspect of worry, and ratings are made on a 5-point Likert type scale from 1 = ‘not at all typical of me’ to 5 = ‘very typical of me.’ This self-report measure has demonstrated good internal consistency and good test-retest reliability.[54]
Beck depression inventory II (BDI II): The BDI-II is a 21-item self-report measure designed to assess the presence and severity of depression. Items are based on DSM-IV diagnostic criteria for MDD and are rated on a 4-point present-state severity scale.[55] Test items describe possible feelings within the past two weeks, and subjects are asked to rate how much these statements parallel their own feelings using a 4-point Likert scale (higher scores coinciding with a greater degree of depression). The scores range from 0 to 63, with scores of 0 to 13 indicating minimal depression, 14 to 19 mild depression, 20 to 28 moderate depression, and 29 to 63 severe depression. The BDI II has demonstrated excellent psychometric properties with good internal consistency (α = 0.91).[56]
IUS: The IUS assesses intolerance to uncertainty, and follows a four-factor structure representing the ideas that uncertainty i) is stressful and upsetting, ii) leads to the inability to act, iii) uncertain events are negative and should be avoided, and iv) being uncertain is unfair. This 27-item scale includes items such as “Uncertainty keeps me from living a full life” and “Unforeseen events upset me greatly.” Subjects rate each item on a 5-point Likert scale ranging from 1 = ‘not at all characteristic of me’, to 5 = ‘entirely characteristic of me.’ The IUS has demonstrated good test-retest reliability over five weeks (r=.78) and has excellent internal consistency (α =0.91).[57,58]
MPS: The MPS is a 45-item self-report questionnaire containing three subscales including self-oriented perfectionism, which entails being severely critical of one's own behaviors and setting demanding standards for oneself; other-oriented perfectionism, which refers to unreasonably high expectations of behavior for significant others; and socially prescribed perfectionism, based upon the perception that significant others have unrealistic standards for oneself, stringently evaluate one's behavior, and essentially pressure one to be perfect.[59] Ratings are made on a 7-point scale from 1 = strongly disagree to 7 = strongly agree. The MPS possesses good psychometric properties in clinical samples.[60]
SPIN: The SPIN is a 17-item self-report inventory used to assess fear, phobic avoidance, and physiological symptoms related to social anxiety disorder. Participants rate each item on a 5-point Likert-type scale ranging from 0 = ‘not at all’, to 4 = ‘extremely.’ Scores for the SPIN can range from 0 to 68, with higher scores indicating greater symptoms related to social anxiety. The SPIN has demonstrated good test-retest reliability, internal consistency, convergent and divergent validity.[61]
LSAS-SR: LSAS-SR is a 24-item self-report questionnaire used to assess fear or anxiety and avoidance in relation to social and performance situations. Each question is rated on a 4-point scale, from 0 to 3, with zero representing no fear or avoidance and 3 representing severe fear and unusual avoidance (67-100% of the time). The scale has been tested, and results indicate a high correlation with other measures of social anxiety along with high internal consistency.[62]
Statistical analysis
All analyses employed the last observation carried forward (LOCF) in the intent-to-treat (ITT) population, which included all individuals enrolled in the study (i.e., completers and non-completers). The results were also analyzed by a subgroup of completers and non-completers to show possible differences between these two groups. Results of primary and secondary efficacy outcome measures were analyzed using a 2-tailed Student's t-test at a 5% alpha level. Within-group comparisons were made from pre-treatment measures for efficacy. Because of the multiple comparisons, a Bonferroni correction was undertaken for all the within subject variables, with a P value of <0.025 for significance. This correction was undertaken using the formula of α/n, (where α = significance and n=number of within-subject variables), thus lowering the significance level and making it harder for any of the results to reach significance, and consequently lowering the number of false positives.[63]
RESULTS
Forty-one subjects enrolled in the study with 31 completers. The primary reason for drop out, given by nine of the 10 subjects, was difficulty in managing the time required for participation. The one other drop out felt that the spirituality presented in the study did not match his belief system. Mean baseline scores for all scales used for completers and non-completers are included in Table 1. Patient demographics and pre-treatment scores for all of the enrolled subjects (i.e., ITT population) as well as for the subsets of those who dropped out and who completed the study are presented in Table 2.
Table 1.
Baseline scores on scales for study completers and non-completers
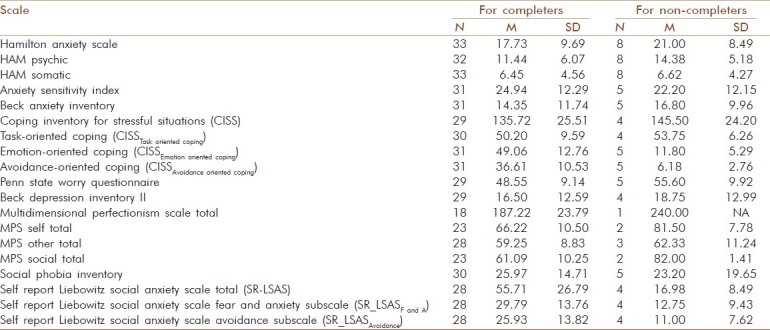
Table 2.
Comparison of mean baseline scores for completers and non completers
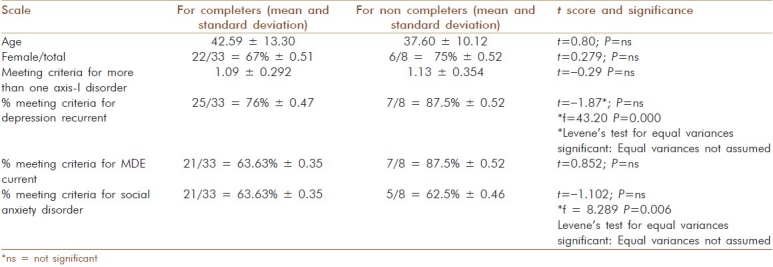
Table 3 highlights the changes four weeks after completing the SKY course for the ITT population. Significant changes were noted for the HAM-A total score (t=4.59; P<.01) and the psychic subscale (t=5.00; P<.01), as well as near significance (given the Bonferroni correction) of the somatic subscale (t=3.25; P<.01). Only 29 subjects completed the HAM-A. The response rate was 73% (21 out of 29 subjects, defined as a decrease ≥50% on the HAM-A) and remission rate of 41% (12 out of 29 subjects, defined as a HAM-A score ≤7).
Table 3.
List of measures assessed pre and post and significance assessment for the ITT population (completers and non-completers)
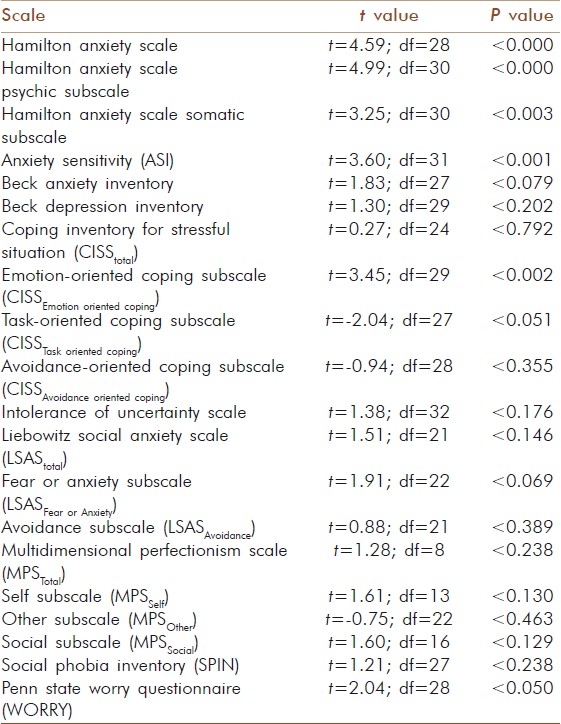
No significant differences were noted in the BDI II pre- and post-treatment (t=1.30; P=ns), but the difference between pre-and post treatment approached significance for the BAI (t=1.83; P<.08). Significant changes were also noted in the ASI (t=3.60; P<.01) and on the PSWQ (t=2.04; P<.05). This is in contrast to the lack of significant changes noted on the IUS (t=1.38; P=ns) as well as MPS subscales for self (t=1.61; P=ns), others (t=-0.75; P=ns), and for social interactions (t=1.60; P=ns). While no significant differences were noted in the SPIN (t=1.21; P=ns), total LSAS score (t=1.51; P=ns), or the avoidance subscale (t=0.88; P=ns), there was a near significant difference noted in the fear and anxiety subscale of the LSAS (t=1.91; P<.07). On measures of strategies of coping, no significant difference was noted in avoidance oriented coping and were found in task-oriented coping (t=–2.04; P<.05) and significant decreases were noted in emotion-oriented coping (t=–3.45; P<0.02).
DISCUSSION
Significant improvements were documented in patient anxiety four weeks after completing the SKY course, supporting the potential efficacy of this approach in people suffering from GAD. These findings are confirmed by the response rate (73%) and remission rate (41%) following the SKY course.
The lack of significant changes noted on the IUS and MPS subscales for self, others and social interactions suggests that the mechanisms that are targeted by these tests (intolerance of uncertainty and perfectionism) are not likely to account for the changes in anxiety associated with taking the SKY course. Conversely, data derived from measures of coping strategies approached significance on task-oriented coping and reached significance on emotion-oriented coping, which suggests that the changes in anxiety subsequent to attending the SKY course might have led to these improvements. This interpretation would be consistent with the lessons of the program that focus on improving acceptance of experiences and limiting catastrophization of terrifying thoughts or worries. Thus, the decrease in anxiety induced by the yoga practices may have been sufficient to increase task-oriented coping, an adaptive coping strategy. Similarly, from the improvement in emotion-oriented coping, it can be inferred that changes in less adaptive personality trait behaviors such as neuroticism which are associated with psychological distress are improved. The lack of differences noted in avoidance oriented coping, may have been a function of time, that is, the time to assessment may have been too short to detect the more long-term changes such as avoidance.
The near significant difference in the fear and anxiety subscale of the LSAS may be analogous to changes in other anxiety symptoms in that one would expect to detect improvements in fear and anxiety long before the appearance of changes in avoidance. Again, the time frame of this study may have been too short to allow for changes in avoidance to emerge.
Interestingly, significant differences were not noted on the BDI II scale, suggesting that depressive symptoms in patients diagnosed with GAD were not affected by the SKY course. However, BDI II levels were relatively low in subjects entering the trial with mean pre levels being 16.50 ± 12.59. Based upon the BDI II criteria for severity of depression, these subjects suffered from mild depression (defined as scores of 14 to 19),[56] indicating the possibility of a relative floor effect resulting in greater difficulty in detecting a change in their depression symptoms with the program.
The completion rate of about 76% compares favorably with other short-term psychotherapy studies in GAD[64,65] as well as pharmacotherapy studies.[66] This is particularly relevant given the severity of treatment resistance in this population of GAD patients. Response rates of 73% and remission rates of 41% also compare favorably with other studies of psychotherapy and pharmacotherapy.[67,68]
Several limitations are evident and, therefore, interpretations of this preliminary data must be cautious. Firstly, the data are open label and unblinded, such that demand characteristics may have played a role in the outcome. For example, it is possible that subjects felt pressured to score lower on the post-intervention anxiety scales. However, this concern is mitigated by the fact that test scores did not improve on all post-intervention measures. Furthermore, the absence of an active control group makes it impossible to control for the expectation effects of the intervention. Future studies could extend our preliminary data by providing an active control comparison group and blinding the assessors as to subject group assignment. Although patients were encouraged to continue practicing yoga at home for 20 min daily after the course, our study did not prospectively evaluate compliance to home practice and therefore its effects at the one-month follow-up are unknown. Finally, follow up beyond the first month after attending the SKY course would provide more information on long-term efficacy and the potential effects on symptoms, such as avoidance, that tend to improve later in the course of recovery.
Our data are preliminary in nature and thus, data for compliance and follow up symptoms were not recorded. Nevertheless, of those who completed the study, 100% attended all five sessions. Future studies of breathing programs and treatment of anxiety should evaluate longer term follow up and compliance with home practice.
CONCLUSION
In summary, this SKY course, a 22-h program delivered over five days, used as an adjunct to standard treatment in outpatients referred to a tertiary care center, was shown to be effective in significantly reducing anxiety in patients meeting criteria for GAD who had failed to achieve remission despite previous treatments with CBT and/or Mindfulness Based Stress Reduction (MSBR) and who were taking stable doses of psychotropic medications at the time of the study. The integration of Eastern mind-body practices and Western medicine bodes well for alleviating anxiety symptoms in those suffering from serious remission-resistant GAD. Future studies should explore the potential benefits of yoga interventions such as the SKY course within a longer time frame using a randomized controlled design with blinded assessment.
ACKNOWLEDGEMENTS
We wish to thank the Art of Living Foundation for assigning instructors to assist in teaching the Sudarshan Kriya Yoga course and the follow-up sessions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005b;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greenberg PE, Sisitky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JR, et al. The economic burden of anxiety disorders n the 1990s. J Clin Psychiatry. 1999;60:427–35. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- 4.Statistics Canada. The Daily-Canadian Community Health Survey: Mental health and well-being (Canada Catalogue no. 11-001-XIE) [Retrieved October 19, 2006, Last cited on 2003, Sept. 3]. from: http://www.statcan.ca/Daily/English/030903/d030903.pdf .
- 5.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington: American Psychiatric Association; 2001. American Psychiatric Association. DSM-IV-TR. [Google Scholar]
- 6.Wittchen HU. Generalized Anxiety Disorder: Prevalence Burden, and Cost to Society. Depress Anxiety. 2002;16:162–71. doi: 10.1002/da.10065. [DOI] [PubMed] [Google Scholar]
- 7.Wittchen HU, Zhao S, Kessler RC, Eaton WW. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:355–64. doi: 10.1001/archpsyc.1994.03950050015002. [DOI] [PubMed] [Google Scholar]
- 8.Massion AO, Warshaw MG, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. Am J Psychiatry. 1993;150:600–7. doi: 10.1176/ajp.150.4.600. [DOI] [PubMed] [Google Scholar]
- 9.Olfson M, Fireman B, Weissman MM, Leon AC, Sheehan DV, Kathol RG, et al. Mental disorders and disability among patients in a primary care group practice. Am J Psychiatry. 1997;154:1734–40. doi: 10.1176/ajp.154.12.1734. [DOI] [PubMed] [Google Scholar]
- 10.Brawman-Mintzer O, Lydiard RB. Generalized anxiety disorder: Issues in epidemiology. J Clin Psychiatry. 1996;57(Suppl 7):3–8. [PubMed] [Google Scholar]
- 11.Ballenger JC. Update on anxiety disorders. Arch Intern Med. 1991;151:857–9. [PubMed] [Google Scholar]
- 12.Montgomery SA. Pregabalin for the treatment of generalised anxiety disorder. Expert Opin Pharmacother. 2006;7:2139–54. doi: 10.1517/14656566.7.15.2139. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy SH, Eisfeld BS, Cooke RG. Quality of life: An important dimension in assessing the treatment of depression. J Psychiatry Neurosci. 2001;26(Suppl):S23–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Kennedy SH, Dickens SE, Eisfeld BS, Bagby RM. Sexual dysfunction before antidepressant therapy in major depression. J Affect Disord. 1999;56:201–8. doi: 10.1016/s0165-0327(99)00050-6. [DOI] [PubMed] [Google Scholar]
- 15.Michelini S, Cassano GB, Frare F, Perugi G. Long-term use of benzodiazepines: Tolerance, dependence and clinical problems in anxiety and mood disorders. Pharmacopsychiatry. 1996;29:127–34. doi: 10.1055/s-2007-979558. [DOI] [PubMed] [Google Scholar]
- 16.Baldwin DS, Nair RV. Escitalopram in the treatment of generalized anxiety disorder. Expert Rev Neurother. 2005;5:443–9. doi: 10.1586/14737175.5.4.443. [DOI] [PubMed] [Google Scholar]
- 17.Gelenberg AJ, Lydiard RB, Rudolph RL, Aguiar L, Haskins JT, Salinas E. Efficacy of venlafaxine extended-release capsules in nondepressed outpatients with generalized anxiety disorder: A 6-month randomized controlled trial. JAMA. 2000;283:3082–8. doi: 10.1001/jama.283.23.3082. [DOI] [PubMed] [Google Scholar]
- 18.Pollack MH, Zaninelli R, Goddard A, McCafferty JP, Bellew KM, Burnham DB, et al. Paroxetine in the treatment of generalized anxiety disorder: Results of a placebo-controlled, flexible-dosage trial. J Clin Psychiatry. 2001;62:350–7. doi: 10.4088/jcp.v62n0508. [DOI] [PubMed] [Google Scholar]
- 19.Rickels K, Downing R, Schweizer E, Hassman H. Antidepressants for the treatment of generalized anxiety disorder.A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry. 1993;50:884–95. doi: 10.1001/archpsyc.1993.01820230054005. [DOI] [PubMed] [Google Scholar]
- 20.Katzman MA, Vermani M, Jacobs L, Marcus M, Kong B, Lessard S, et al. Quetiapine as an adjunctive pharmacotherapy for the treatment of non-remitting generalized anxiety disorder: A flexible-dose, open-label pilot trial. J Anxiety Disord. 2008;22:1480–6. doi: 10.1016/j.janxdis.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Andrews G, Sanderson K, Slade T, Issakidis C. Why does the burden of disease persist.Relating the burden of anxiety and depression to effectiveness of treatment? Bull World Health Organ. 2000;78:446–54. [PMC free article] [PubMed] [Google Scholar]
- 22.Covin R, Ouirret AJ, Seeds PM, Dozois DJ. A meta-analysis of CBT for pathological worry among clients with GAD. J Anxiety Disord. 2008;22:108–16. doi: 10.1016/j.janxdis.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 23.Durham RC, Chambers JA, MacDonald RR, Power KG, Major K. Does cognitive-behavioural therapy influence the long-term outcome of GAD.An 8-14 year follow-up of two clinical trials? Psychol Med. 2003;33:499–509. doi: 10.1017/s0033291702007079. [DOI] [PubMed] [Google Scholar]
- 24.Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: Part I-neurophysiologic model. J Altern Complement Med. 2005;11:189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 25.Pilkington K, Kirkwood G, Rampes H, Richardson J. Yoga for depression: The research evidence. J Affect Disord. 2005;89:13–24. doi: 10.1016/j.jad.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 26.Brown RP, Gerbarg PL. Sudarshan kriya yogic breathing in the treatment of stress, anxiety, and depression: Part II-Clinical applications and guidelines. J Comp and Alt Med. 2005;11:711–7. doi: 10.1089/acm.2005.11.711. [DOI] [PubMed] [Google Scholar]
- 27.Brown RP, Gerbarg PL, Muskin PR. How to use Herbs, Nutrients, and Yoga in Mental Health Care. New york: W.W. Norton; 2009. pp. 71–106. [Google Scholar]
- 28.Lavey R, Sherman T, Mueser KT, Osborne DD, Currier M, Wolfe R. The effects of yoga on mood in psychiatric inpatients. Psychiatr Rehabil J. 2005;28:399–402. doi: 10.2975/28.2005.399.402. [DOI] [PubMed] [Google Scholar]
- 29.Ray US, Mukhopadhyaya S, Purkayastha SS, Asnani V, Tomer OS, Prashad R, et al. Effect of yogic exercises on physical and mental health of young fellowship course trainees. Indian J Physiol Pharmacol. 2001;45:37–53. [PubMed] [Google Scholar]
- 30.Malathi A, Damodaran A. Stress due to exams in medical students--role of yoga. Indian J Physiol Pharmacol. 1999;43:218–24. [PubMed] [Google Scholar]
- 31.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255–9. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 32.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Shetty TK, Subbakrishna DK, et al. Therapeutic efficacy of Sudarshan Kriya Yoga (SKY) in dysthymic disorder. NIMHANS J. 1998;16:21–8. [Google Scholar]
- 33.Naga Venkatesha Murthy PJ, Janakiramaiah N, Gangadhar BN, Subbakrishna DK. P300 amplitude and antidepressant response to Sudarshan Kriya Yoga (SKY) J Affect Disord. 1998;50:45–8. doi: 10.1016/s0165-0327(98)00029-9. [DOI] [PubMed] [Google Scholar]
- 34.Vedamurthachar A, Janakiramaiah N, Hegde JM, Shetty TK, Subbakrishna DK, Sureshbabu SV, et al. Antidepressant efficacy and hormonal effects of Sudarshan Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord. 2006;94:249–53. doi: 10.1016/j.jad.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 35.Carter JJ, Byrne GG, Brown RP, Gerbarg PL. Los Angeles, CA: Symposium on Yoga Therapy and Research; 2009. Multi-component Yoga Breath Based Program Reduces PTSD in Australian Vietnam War Veterans: A Randomized Controlled Trial. [Google Scholar]
- 36.Gerbarg PL. Yoga and Neuro-psychoanalysis. In: Anderson FS, editor. Bodies in Treatment: The Unspoken Dimension. Hillsdale NJ: The Analytic Press Inc; 2007. pp. 132–3. [Google Scholar]
- 37.Sageman S. Breaking through the despair: Spiritually oriented group therapy as a means of healing women with severe mental illness. J Am Acad Psychoanal Dyn Psychiatry. 2004;32:125–41. doi: 10.1521/jaap.32.1.125.28329. [DOI] [PubMed] [Google Scholar]
- 38.Descilo T, Vedamurtachar A, Gerbarg PL, Nagaraja D, Gangadhar BN, Damodaran B, et al. Effects of a yoga-breath intervention alone and in combinations with an exposure therapy for PTSD and depression in survivors of the 2004 Southeast Asian tsunami. Acta Psychiatr Scand. 2010;12:289–300. doi: 10.1111/j.1600-0447.2009.01466.x. [DOI] [PubMed] [Google Scholar]
- 39.Gerbarg PL, Brown RP. Yoga: A breath of relief for Hurricane Katrina refugees. Curr Psychiatry. 2005;4:55–67. [Google Scholar]
- 40.Bhatia M, Kumar A, Kumar N, Pandey RM, Kochupillai V. Electrophysiologic evaluation of Sudarshan Kriya: An EEG, BAER, P300 study. Indian J Physiol Pharmacol. 2003;47:157–63. [PubMed] [Google Scholar]
- 41.Sharma H, Sen S, Singh A, Bhardwaj NK, Kochupillai V, Singh N. Sudarshan Kriya practitioners exhibit better antioxidant status and lower blood lactate levels. Biol Psychol. 2003;63:281–91. doi: 10.1016/s0301-0511(03)00071-1. [DOI] [PubMed] [Google Scholar]
- 42.Pinninti NR, Madison H, Musser E, Rissmiller D. MINI International Neuropsychiatric Schedule: Clinical utility and patient acceptance. Eur Psychiatry. 2003;18:361–4. doi: 10.1016/j.eurpsy.2003.03.004. [DOI] [PubMed] [Google Scholar]
- 43.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(suppl 20):22–33. [PubMed] [Google Scholar]
- 44.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 45.Pollack MH, Simon NM, Zalta AK, Worthington JJ, Hoge EA, Mick E, et al. Olanzapine augmentation of fluoxetine for refractory generalized anxiety disorder: A placebo controlled study. Biol Psychiatry. 2006;59:211–21. doi: 10.1016/j.biopsych.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 46.Reiss S, McNally RJ. The expectancy model of fear. In: Reiss S, McNally RJ, editors. Theoretical issues in behavior therapy. New York: Academic Press; 1985. pp. 107–21. [Google Scholar]
- 47.Peterson RA, Plehn K. Measuring anxiety sensitivity. In: Taylor S, editor. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Mahwah, NJ: Lawrence Erlbaum; 1999. pp. 61–82. [Google Scholar]
- 48.Peterson RA, Reiss S. Test Manual for the Anxiety Sensitivity Index. Orland Park, IL: International Diagnostic Systems; 1987. [Google Scholar]
- 49.Peterson RA, Reiss S. Anxiety Sensitivity Index Manual. 2nd ed. Worthington, OH: International Diagnostic Services; 1992. [Google Scholar]
- 50.Beck AT, Epstein N, Brown G, Steer RA. An inventor for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. 1988;56:893–7. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 51.Beck AT, Steer RA. Beck Anxiety Inventory Manual. San Antonio: The Psychological Corporation Harcourt Brace Jovanovich, Inc; 1990. [Google Scholar]
- 52.Osman A, Kopper BA, Barrios FX, Osman JR, Wade T. The Beck Anxiety Inventory: Reexamination of factor structure and psychometric properties. J Clin Psychol. 1997;53:7–14. doi: 10.1002/(sici)1097-4679(199701)53:1<7::aid-jclp2>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 53.Endler NS, Parker JD. Assessment of multidimensional coping: Task, emotion, and avoidance strategies. Psychol Assess. 1994;6:50–60. [Google Scholar]
- 54.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28:487–95. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 55.Arnau RC, Meagher MW, Norris MP, Bramson R. Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychol. 2001;20:112–9. doi: 10.1037//0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- 56.Beck AT, Steer RA, Brown GK. 2nd Ed. San Antonio, TX: Psychological Corporation; 1996. Beck Depression Inventory manual. [Google Scholar]
- 57.Buhr K, Dugas MJ. The intolerance of uncertainty scale: Psychometric properties of the English version. Behav Res Ther. 2002;40:931–45. doi: 10.1016/s0005-7967(01)00092-4. [DOI] [PubMed] [Google Scholar]
- 58.Buhr K, Dugas MJ. Investigating the construct validity of intolerance of uncertainty and its unique relationship with worry. J Anxiety Disord. 2006;20:222–36. doi: 10.1016/j.janxdis.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 59.Hewitt PL, Flett GL. Perfectionism in the self and social contexts: Conceptualization, assessment, and association with psychopathology. J Pers Soc Psychol. 1991;60:456–70. doi: 10.1037//0022-3514.60.3.456. [DOI] [PubMed] [Google Scholar]
- 60.Hewitt PL, Flett GL, Turnbull-Donovan W, Mikail SF. The multidimensional perfectionism scale: Reliability, validity, and psychometric properties in psychiatric samples. J Consult Clin Psychol. 1991;3:464–8. [Google Scholar]
- 61.Connor KM, Davidson JR, Churchill LE, Sherwood A, Foa E, Weisler RH. Psychometric properties of the Social Phobia Inventory (SPIN): New self rating scale. Br J Psychiatry. 2000;176:379–86. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- 62.Rytwinski NR, Fresco DM, Heimberg RG, Coles ME, Liebowitz MR, Cissell S, et al. Screening for social anxiety disorder with the Self Report Version of the Liebowitz Social Anxiety Scale. Depress Anxiety. 2009;26:34–8. doi: 10.1002/da.20503. [DOI] [PubMed] [Google Scholar]
- 63.Weisstein, Eric W. “Bonferroni Correction”. From MathWorld--A Wolfram Web Resource. [Last cited on 2011 Aug, 8]. Available from: http://mathworld.wolfram.com/BonferroniCorrection.html .
- 64.Stanley MA, Wilson NL, Nony DM, Rhoades HM, Wagener PD, Greisinger AJ, et al. Cognitive behavioural therapy for generalized anxiety disorder among older adults in primary care: A randomized clinical trial. JAMA. 2009;301:1460–7. doi: 10.1001/jama.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D. Mindfulness-based cognitive therapy for generalized anxiety disorder. J Anxiety Disord. 2008;22:716–21. doi: 10.1016/j.janxdis.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 66.Stein DJ, Ahokas AA, Bodinat C. Efficacy of agomeltine in generalized anxiety disorder: A randomized, double-blind, placebo-controlled study. J Clin Psychopharmacol. 2008;28:561–6. doi: 10.1097/JCP.0b013e318184ff5b. [DOI] [PubMed] [Google Scholar]
- 67.Ferrero A, Piero A, Fassina S, Massola T, Lanteri A, Daga GA, et al. A 12-month comparison of brief psychodynamic psychotherapy and pharmacotherapy treatment in subjects with generalized anxiety disorders in a community setting. Eur Psychiatry. 2007;22:530–9. doi: 10.1016/j.eurpsy.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 68.Nimatoudis I, Zissis NP, Kogeorgos J, Theodoropoulou S, Vidalis A, Kaprinis G. Remission rates with venlafaxine extended release in Greek outpatients with generalized anxiety disorder. A double-blind, randomized, placebo controlled study. Int Clin Psychopharmacol. 2004;19:331–6. doi: 10.1097/00004850-200411000-00003. [DOI] [PubMed] [Google Scholar]


