Abstract
Background:
Long-term alternate nostril breathing (ANB) has been shown to enhance autonomic control of the heart by increasing parasympathetic modulation. However, there is no information on the immediate effects of ANB on autonomic control compared to paced breathing (PB) at the same rate in individuals who are inexperienced with yogic breathing.
Aim:
To examine cardiac autonomic modulation following ANB in comparison to that following PB in individuals who were inexperienced in ANB.
Materials and Methods:
Twenty healthy individuals (22.3 ± 2.9 years) with no prior experience with ANB engaged in
Results:
Analysis of covariance revealed lnTP, lnLF and lnHF were greater during both post-ANB and post-PB compared to PRE (P<0.05). MAP and lnLF/lnHF did not significantly differ between conditions.
Conclusions:
These data suggest that there was an immediate increase in cardiac autonomic modulation following ANB and PB without a shift in autonomic balance in individuals inexperienced with yogic breathing. To our knowledge, this is the first investigation to investigate the autonomic effects of ANB in this population and also to compare the effects of ANB and PB at the same respiratory rate.
Keywords: Parasympathetic, sympathetic, yogic breathing
INTRODUCTION
Pranayama is one of the eight limbs of Asthanga Yoga and includes different respiratory techniques which aim to treat various physical and psychological ailments.[1] Anulom-Vilom, or alternate-nostril breathing (ANB), is a type of pranayama that involves left nostril inhalation followed by right nostril exhalation and then right nostril inhalation followed by left nostril exhalation. Several investigations have been conducted to determine the long-term effects of this technique on the cardiovascular and autonomic nervous systems in healthy and clinical populations and many of these studies have suggested that ANB leads to a shift in sympathovagal balance toward parasympathetic dominance.[2–5] For example, Pal et al.[2] found a reduced basal heart rate and a reduced heart rate response to standing, suggesting enhanced parasympathetic outflow in response to a three-month ANB intervention. Thereafter, Upadhyay Dhungel et al.[4] found that a four-week ANB intervention led to reduced heart rate and blood pressure, whereas Mourya et al.[5] reported reduced blood pressure and improved autonomic reactivity to a series of autonomic tests following a three-month ANB intervention in individuals with stage-1 hypertension.
On the other hand, there is less information on autonomic nervous system function in the time period immediately following a session of yogic breathing. By using heart rate variability (HRV), a noninvasive index of cardiac autonomic modulation, Raghuraj et al.[6] found no changes in autonomic control following 30 min of ANB in regular practitioners of yogic breathing. However, these authors did report increases in heart rate and skin conductance. On the other hand, Srivastava et al.[3] reported a reduction in heart rate, but no change in blood pressure or galvanic skin resistance following 15 min of ANB. These different findings may be partly explained by the participant populations as Raghuraj et al's subjects had at least three months experience with ANB, whereas it appears Srivastava et al. used individuals who were not regular practitioners of yogic breathing. Nevertheless, an important consideration that seems to have been overlooked in previous work is the influence that respiratory rate has on autonomic control of the heart. Since it has been well documented that breathing rate can influence autonomic control of heart[7] and ANB is generally performed at a relatively slow rate, it is possible that alterations in respiratory rate alone are responsible for any autonomic changes. Thus, it would be advantageous to compare the immediate effects of ANB to that of a controlled breathing condition at the same respiratory rate.
Therefore, the purpose of this investigation is to examine cardiac autonomic modulation, as assessed by HRV, immediately following both ANB and paced breathing (PB) at the same respiratory rate. In order to eliminate the influence of any chronic adaptations to breathing exercise, our study population included only those individuals with no previous experience with yogic breathing.
MATERIALS AND METHODS
Participants
Twenty healthy individuals (8 males, 12 females; age range: 19 – 29 years) participated in this study. None of the participants had previous experience with ANB and all participants made two visits to the laboratory for testing. All participants gave written informed consent and all procedures were approved by the Committee for the Protection of Human Subjects at San Francisco State University in San Francisco, CA, USA.
Experimental design
Participants were instructed not to eat or have caffeine within 3 h of arriving at the laboratory. During their first visit, participants gave written informed consent, completed a pre-participation questionnaire, had their height and weight measured, and their body mass index (BMI) was calculated. Additionally, participants engaged in a practice session of two breathing exercises [ANB and paced breathing (PB) at a rate of 5breaths/min-1]. An investigator provided a demonstration and instructions regarding the performance of these two breathing exercises. During their second visit, the participants performed ANB and PB in a random order for 30 min. ANB and PB were preceded and followed by 5 min of seated rest during which the participants breathed normally (PRE, post-ANB, and post-PB, respectively). An EKG was continuously collected at a sampling rate of 500 Hz during the entire session via a Biopac MP100 Data Acquisition System (Goleta, CA) for analysis of HRV. Blood pressure was also recorded via a sphygmomanometer and stethoscope during PRE, post-ANB, and post-PB.
Description of breathing techniques
Alternate nostril breathing: While sitting in a crossed leg position, participants inhaled through the left nostril, held the breath for a moment while keeping both nostrils closed, then exhaled from the right nostril keeping the left nostril closed. This was followed by inhalation through the right nostril and exhalation through left nostril in the same manner. The participants repeated this cycle at a breathing rate of 5breaths/min-1 for 30 min. Paced Breathing: The participants were instructed to breathe normally while maintaining a breathing rate of 5breaths/min-1 for 30 min. An investigator provided verbal cues to ensure that the appropriate breathing rate was maintained.
Data analysis
The EKGs collected during PRE, post-ANB, and post-PB were analyzed for the mean R wave to R wave (mean RR) interval and HRV parameters. Spectral analysis via fast Fourier transformation was performed on the EKG using Kubios software (Kuopio, Finland). From the power spectrum, the following spectral indices were obtained: total power (TP; 0.0-0.4 Hz), low-frequency power (LF; 0.04-0.15 Hz), and high-frequency power (HF; 0.15-0.40 Hz). Briefly, LF reflects a combination of sympathetic and parasympathetic cardiac modulation, HF reflects parasympathetic (vagal) cardiac modulation, and TP reflects the total variance in heart rate fluctuations.[8] The ratio of LF to HF was also calculated to quantify sympathovagal balance.[8] Both systolic (SBP) and diastolic (DBP) blood pressure were recorded and reported and further reported as mean arterial pressure (MAP) using the following equation: MAP=DBP + 0.333 * (SBP - DBP).
Statistical analysis
The Shapiro-Wilk test[9] was used to assess the normality of all data and data that were not normally distributed were transformed using the natural log (ln) algorithm. Independent t-tests were used to examine between-sex differences in descriptive and resting variables. Repeated measures analysis of covariance (ANCOVA) using sex as a covariate was used to examine differences in variables between the different conditions. When significance was found, post-hoc pairwise comparisons were performed with the Bonferroni correction. All tests were considered significant at the 0.05 level.
RESULTS
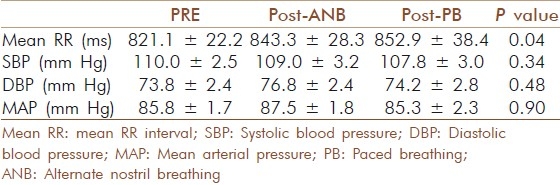
Descriptive statistics, resting mean RR interval, and MAP can be seen in Table 1. Males had a significantly greater body mass, height, BMI, and resting SBP, DBP, and MAP compared to females. However, there were no significant between-sex differences in age, resting mean RR interval, or any of the HRV parameters. The response of the mean RR interval and MAP to the conditions can be seen in Table 2. The ANCOVA revealed that there were significant differences in the mean RR interval between conditions (F=4.0; P<0.05), although the post-hoc tests were not significant. SBP (F=1.2; P=0.34), DBP (F=0.76; P=0.48), and MAP (F=0.10; P=0.90) did not differ between the conditions.
Table 1.
Descriptive statistics for the participants (mean ± SD)
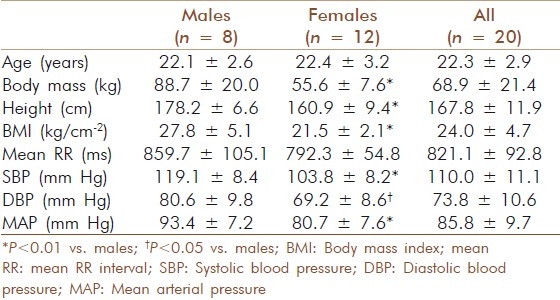
Table 2.
Mean RR interval and arterial blood pressure during the different conditions (mean ± SEM)
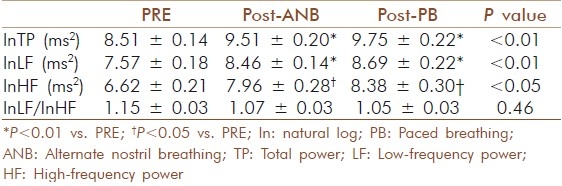
HRV indices during the different conditions are presented in Table 3. The ANCOVA revealed that there were differences in lnTP (F=7.3; P<0.01), lnLF (F=7.0; P<0.01), and lnHF (F=4.7; P<0.05) between conditions. Post-hoc analysis found that all of these variables were greater during post-ANB and post-PB compared to PRE. lnLF/lnHF did not statistically differ between conditions (F=0.83; P=0.46).
Table 3.
Heart rate variability indices during the different conditions (mean ± SEM)
DISCUSSION
The results of this investigation suggest that the period immediately following both ANB and PB is marked by elevated autonomic modulation of the heart. Furthermore, this occurs without a significant shift in sympathovagal balance. To our knowledge, this is the first study to compare ANB to a controlled breathing condition at the same breathing rate and suggests that autonomic changes occurring in response to ANB are primarily mediated by breathing rate in individuals without prior experience with yogic breathing.
Previous researchers have reported that long-term practice of ANB is associated with improvement in autonomic regulation of cardiac function in both healthy and diseased populations, reflected by a shift toward parasympathetic dominance.[2–5] On the other hand, results from studies examining autonomic control immediately after ANB have provided mixed results. In two separate studies, Raghuraj et al.[6,10] found no differences in measures of HRV measures following ANB. However, in the latter study, Raghuraj et al.[6] found a significant increase in heart rate immediately following 30 min of ANB, whereas Srivastava et al.[3] found a reduced heart rate immediately following 15 min of ANB. Although these mixed findings could be the result of the participant populations examined (i.e., experienced vs. inexperienced practitioners), these studies did not account for the influence that respiratory rate has on autonomic control.[7] Specifically, the lack of a comparison of the effects of ANB to a control condition matched for breathing rate makes it difficult to determine if the autonomic changes are due to the ANB technique itself, or simply due to changes in breathing rate.
Thus we sought to examine cardiac autonomic modulation immediately following ANB and also following a paced breathing condition at the same respiratory rate. By using individuals who were inexperienced with yogic breathing, we hoped to eliminate any influence that chronic ANB practice may have on the results. Our findings of an increase in lnTP, lnLF, and lnHF following both ANB and PB suggest that both conditions increased cardiac autonomic modulation. Since it has been documented that HF power of the HRV power spectrum primarily represents parasympathetic modulation of the heart, LF power reflects a combination of sympathetic and parasympathetic outflow, and[8] our data suggests that both ANB and PB increase autonomic modulation without causing a significant shift in sympathovagal balance. This is also supported by our finding that lnLF/lnHF was not significantly altered after either condition.
Although the statistical post-hoc tests did not find differences in the mean RR interval between conditions, the ANCOVA was significant suggesting that it was not the same during all conditions. Closer examination of our data reveals that calculated heart rates were approximately 73, 71, and 70 bpm for PRE, post-ANB, and post-PB, respectively. Thus, it appears that the breathing conditions had a modest influence on heart rate. This is consistent with the work of Hayano et al.[7] who reported that changes in breathing rate can alter cardiac parasympathetic autonomic modulation without significantly altering heart rate. Thus it appears that respiratory-related changes in autonomic modulation may be independent of mean vagal tone. Additionally, the autonomic changes did not appear to appreciably alter SBP, DBP, or MAP.
The results of this study may have implications related to the use and prescription of yogic breathing. Since both ANB and PB had similar effects on the autonomic nervous system, at least at a rate of 5breaths/min-1, PB may be just as beneficial as ANB for beginning yoga practitioners. Beginners may find slow breathing, without manipulation of the nostrils, easier to perform and thus it may enhance adherence to their practice. As one becomes more comfortable with controlled breathing techniques, participation in other breathing manipulation techniques (e.g., ANB) may provide further benefits. Furthermore, since low HRV measures have been associated with negative health consequences,[11] it seems that both ANB and PB are valid techniques to improve health and reduce the risk of cardiovascular events.
There are a few limitations of this investigation that warrant discussion. Firstly, our participants were instructed to breathe at a rate of 5breaths/min-1 during both conditions in order to control for the effects of breathing rate on autonomic modulation. However, during regular practice of ANB, breathing rate does not have to be as tightly controlled. Thus, it is possible to find different results if different breathing rates are utilized. Additionally, since HRV is an index of cardiac autonomic modulation, it may not reflect autonomic outflow to other tissues of the body. Thus confirmation of these findings using other autonomic measures (e.g., microneurography, galvanic skin response) is necessary to better represent autonomic activity throughout the body. Furthermore, if ANB has a more selective stimulatory effect on the olfactory neural pathways and the central autonomic network (e.g., hypothalamus, limbic system), measurement of these pathways may allow researchers to provide evidence for different and specific effects of ANB compared to PB. Nevertheless, HRV is a validated index of cardiac autonomic modulation[8] and we believe that our findings are representative of autonomic outflow to the heart.
In conclusion, we found that both ANB and PB result in enhanced autonomic modulation of the heart without a shift in autonomic balance. Our data suggests that autonomic changes occurring in response to ANB are primarily mediated by breathing rate in individuals without prior experience with yogic breathing. Future research should aim to determine the mechanisms responsible for these changes, possibly by quantifying the neural circuits involved, and potentially examine the time course of autonomic changes in response to chronic ANB practice.
ACKNOWLEDGEMENTS
We would like to acknowledge the support of the Chair of the Department of Kinesiology, Dr. Marialice Kern, Ph.D., and further thank all of the study participants for their time and effort in this project.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Stiles M. Newburyport (MA): Red Wheel/Weiser; 2001. Yoga sutras of Patanjali. [Google Scholar]
- 2.Pal GK, Velkumary S, Madanmohan T. Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120:115–21. [PubMed] [Google Scholar]
- 3.Srivastava RD, Jain N, Singhal A. Influence of alternate nostril breathing on cardiorespiratory and autonomic functions in healthy young adults. Indian J Physiol Pharmacol. 2005;49:475–83. [PubMed] [Google Scholar]
- 4.Upadhyay Dhungel K, Malhotra V, Sarkar D, Prajapati R. Effect of alternate nostril breathing exercise on cardiorespiratory functions. Nepal Med Coll J. 2008;10:25–7. [PubMed] [Google Scholar]
- 5.Mourya M, Mahajan AS, Singh NP, Jain AK. Effect of slow-and fast-breathing exercises on autonomic functions in patients with essential hypertension. J Altern Complement Med. 2009;15:711–7. doi: 10.1089/acm.2008.0609. [DOI] [PubMed] [Google Scholar]
- 6.Raghuraj P, Telles S. Immediate effect of specific nostril manipulating yoga breathing practices on autonomic and respiratory variables. Appl Psychophysiol Biofeedback. 2008;33:65–75. doi: 10.1007/s10484-008-9055-0. [DOI] [PubMed] [Google Scholar]
- 7.Hayano J, Mukai S, Sakakibara M, Okada A, Takata K, Fujinami T. Effects of respiratory interval on vagal modulation of heart rate. Am J Physiol. 1994;267:H33–40. doi: 10.1152/ajpheart.1994.267.1.H33. [DOI] [PubMed] [Google Scholar]
- 8.Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North AmericanSociety of Pacing and Electrophysiology. Circulation. 1996;93:1043–65. [PubMed] [Google Scholar]
- 9.Shapiro SS, Wilk MB. An analysis of variance test for normality. Biometrika. 1965;52:591–9. [Google Scholar]
- 10.Raghuraj P, Ramakrishnan AG, Nagendra HR, Telles S. Effect of two selected yogic breathing techniques on heart rate variability. Indian J Physiol Pharmacol. 1998;42:467–72. [PubMed] [Google Scholar]
- 11.Tsuji H, Larson MG, Venditti FJ, Jr, Manders ES, Evans JC, Feldman CL, et al. Impact of reduced heart rate variability on risk for cardiac events.The Framingham Heart Study. Circulation. 1996;94:2850–5. doi: 10.1161/01.cir.94.11.2850. [DOI] [PubMed] [Google Scholar]


