Abstract
Umbilical endometriosis is rare and challenging in both diagnosis and treatment. We report a case of an umbilical scar endometriotic nodule in a 39-year-old lady following laparoscopy-assisted vaginal hysterectomy. The wide local excision of the nodule and histopathological examination confirmed the diagnosis. We discuss the pathogenesis, diagnosis, differential diagnosis, and treatment options for the patient.
KEY WORDS: Cyclical pain, extrapelvic endometriosis, umbilical nodule
INTRODUCTION
Endometriosis is characterized by the presence of endometrial glands and stroma outside the uterus.[1] The most common sites are ovary, pouch of Douglas, and uterosacral ligaments in the pelvis. Extrapelvic endometriosis is uncommon accounting only for 1% of total cases.[2] The most common sites for extrapelvic endometriosis are bowel, bladder, lungs, umbilicus, and surgical scars. Pelvic endometriosis presents as dysmenorrhea, menorrhagia, infertility, and chronic pelvic pain. But extrapelvic endometriosis has varied signs and symptoms.
Umbilical endometriosis accounts for 0.5–1% of all extrapelvic endometriosis.[3] It is usually secondary to laparoscopic surgical procedures involving the umbilicus. Spontaneous primary nodules are very rare but few case reports have been reported. We report a case of umbilical scar endometriosis secondary to laparoscopic surgery.
CASE REPORT
A 39-year-old parous woman presented to us with an umbilical nodule since 6 months. She had cyclical pain and bleeding from the site. She had undergone laparoscopy-assisted vaginal hysterectomy 3 years ago for a symptomatic fibroid uterus. Although we did not get operative notes, she was not told to have endometriosis. Both ovaries were left behind.
At the time of presentation to us, she had a 2 × 2 cm purplish nodule at the umbilicus [Figures 1 and 2]. It was nontender and there were no signs of infection. There was no history of bleeding from the site. Characteristically, the patient had a history of cyclical pain every month. Transvaginal sonography was normal with no evidence of ovarian endometriosis. A wide local excision of the umbilical nodule [Figure 3] was done and histopathology confirmed the diagnosis as endometriosis at the umbilicus.
Figure 1.

Umbilical nodule
Figure 2.

Evidence of endometriosis at surgery
Figure 3.

Umbilicus after wide excision
The decidualization of umbilical endometriosis can be confused with malignant changes. However, umbilical endometriosis has low malignant potential.[4] Histopathology showed epidermis overlying the dermis containing endometrial glands, surrounded by edematous endometrial stroma with intravasated RBCs, congested blood vessels, lymphoplasmocytic infiltrate, and hemosiderin-laden hemorrhages confirming the diagnosis of scar endometriosis [Figure 4].
Figure 4.
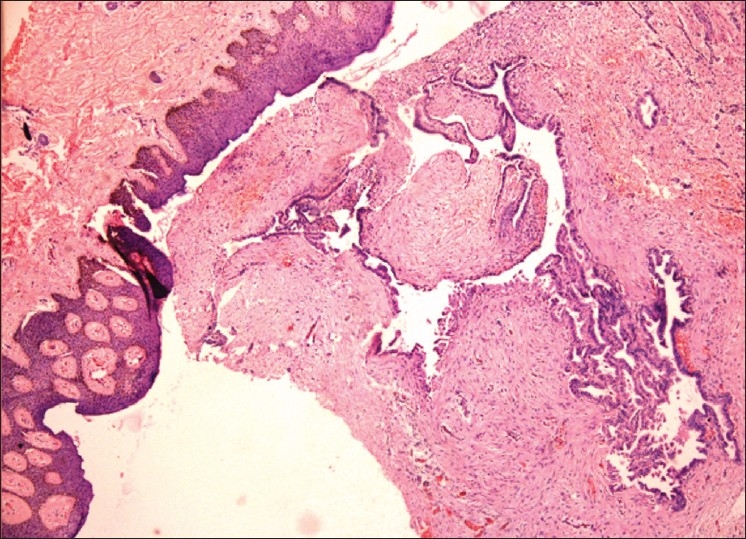
Histopathology showing dermis and endometriotic glands
DISCUSSION
Extrapelvic endometriosis is an uncommon gynecological problem. Umbilical endometriosis at the site of the laparoscopic entry is one of the common sites. Villar in 1886 reported the first case of umbilical endometriosis. Hence, this condition is also called Villar's nodule.[4] Surgical scar endometriosis is one of the sites. In our case, possibly the previous laparoscopic port site was the site for endometriosis. Although GnRH analogs can also be offered to these patients, our patient insisted on excision.
Many theories have been put forward to explain pathogenesis. The hypothesis of migration theory by Sampson explains ovarian endometriosis. While coelomic induction theory explains peritoneal endometriosis. Diminished natural killer cell immunity lessens the clearance of endometrial cells from peritoneum.[5–7]
Scar endometriosis is explained by the migratory pathogenesis theory wherein the endometrial tissue is dispersed by vascular and lymphatic channels due to surgical manipulation.[8] Other theories are mainly based on mullerian remnants undergoing metaplasia to endometriosis. Umbilical endometriosis in pregnancy is reported to require surgical excision.[4]
Clinical diagnosis is sometimes difficult with varying features such as flesh colored nodule, black nodule, flesh colored, bluish, and also in size up to several centimeters. Hence, malignant melanoma should be considered.
Surgical excision is the treatment of choice. If a wide excision and complete removal of the umbilicus is anticipated, it should be discussed with the patient, and reconstruction of the umbilicus can be offered.[9]
There is always a chance of the coexistence of pelvic endometriosis causing pelvic pain. There are no recommendations or guidelines to perform simultaneous laparoscopy to diagnose coexisting pelvic endometriosis while performing a local excision. Asymptomatic patients do not need laparoscopy anyway. Recurrence is always anticipated in all cases of endometriosis and hence patients should be explained before they undergo surgery.
Differential diagnosis are granuloma, primary or metastatic adenocarcinoma (Sister Joseph nodule), nodular melanoma, and cutaneous endosalpingosis.[10]
In our case, cyclical pain with a classical purplish nodule clinched the diagnosis. Since the excision was complete, neither hormones nor GnRH analogs were administered. Hence, to summarize endometriosis is considered in umbilical nodules and surgical excision and histopathology is done to rule out malignancy.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Sampson JA. Perforating hemorrhagic (chocolate) cysts of the ovary: Their importance and especially their relation to pelvic adenomas of the endometrial type. Arch Surg. 1921;3:245. [Google Scholar]
- 2.Markham SM, Carpenter SE, Rock JA. Extrapelvic endometriosis. Obstet Gynecol Clin North Am. 1989;16:193–219. [PubMed] [Google Scholar]
- 3.Latcher JW. Endometriosis of the umbilicus. Am J Obstet Gynecol. 1953;66:161–8. doi: 10.1016/0002-9378(53)90298-1. [DOI] [PubMed] [Google Scholar]
- 4.Skidmore RA, Woosley JT, Katz VL. Decidualized umbilical endometriosis. Int J Gynaecol Obstet. 1996;52:269–73. doi: 10.1016/0020-7292(95)02612-6. [DOI] [PubMed] [Google Scholar]
- 5.Liu DT, Hitchcock A. Endometriosis: Its association with retrograde menstruation, dysmenorrhoea and tubal pathology. Br J Obstet Gynaecol. 1986;93:859–62. doi: 10.1111/j.1471-0528.1986.tb07995.x. [DOI] [PubMed] [Google Scholar]
- 6.Matsuura K, Ohtake H, Katabuchi H, Okamura H. Coelomic metaplasia theory of endometriosis: Evidence from in vivo studies and an in vitro experimental model. Gynecol Obstet Invest. 1999;47(suppl 1):18–22. doi: 10.1159/000052855. [DOI] [PubMed] [Google Scholar]
- 7.Mathur S, Peress MR, Williamson HO, Youmans CD, Maney SA, Garvin AJ, et al. Autoimmunity to endometrium and ovary in endometriosis. Clin Exp Immunol. 1982;50:259–66. [PMC free article] [PubMed] [Google Scholar]
- 8.Schachter LR, Tash J, Olgac S, Bochner BH. Umbilical endometriosis. J Urol. 2003;170:2388–9. doi: 10.1097/01.ju.0000095784.41023.b7. [DOI] [PubMed] [Google Scholar]
- 9.Pfulg M, Van de Sijpe K, Blondeel P. A simple new technique for neo-umbilicoplasty. Br J Plast Surg. 2005;58:688–91. doi: 10.1016/j.bjps.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 10.Bagade P, Guirgus MM. Menstruating from the umbilicus as a rare case of primary umbilical endometriosis: A case report. J Med Case Reports. 2009;3:9326. doi: 10.1186/1752-1947-3-9326. [DOI] [PMC free article] [PubMed] [Google Scholar]


