Abstract
Purpose:
To compare the outcomes of pediatric cataract surgery with intraocular lens (IOL) implantation in an eye camp setting and tertiary care center.
Materials and Methods:
Children aged 5-16 years with visually significant cataract underwent phacoaspiration with IOL implantation in an eye camp (eye camp group) or tertiary care center (TCC group). All surgeries incorporated contemporary microsurgical techniques with implantation of polymethyl-methacrylate (PMMA) IOL. Major postoperative complications were managed at a tertiary care center. Postoperative complications, visual acuity and compliance were evaluated using the Chi-square test. A P value less then 0.05 was considered as statistically significant.
Results:
The cohort comprised 59 children in the eye camp group and 48 children in the TCC group. Thirty two of fifty nine (54.23%) eyes in the eye camp group and 30/48 (62.5%) eyes in the TCC group achieved 20/40 or better best corrected visual acuity (BCVA) postoperatively. Postoperatively, 36 (61%) eyes in the eye camp group and 22 (45.83%) eyes in the TCC group required Nd: YAG laser capsulotomy or a pars plana membranectomy. (P> 0.05) The most striking feature was loss to follow up. In the eye camp group, loss to follow was 20% at one year, 49% at two years, 62% at 3 years and 67% at 4 years compared to 12.5, 21, 27 and 33% respectively in the TCC group (P<0.05, all cases).
Conclusions:
The outcomes of camp and tertiary care center (hospital) based pediatric cataract surgery were similar. However, the major drawback of camp based surgery was loss to follow up which eventually affected the management of amblyopia and postoperative complications.
Keywords: Eye Camp, Intraocular Lens, Pediatric Cataract
INTRODUCTION
The World Health Organization (WHO) estimates that out of 1.5 million blind children, 1.3 million live in the developing countries (Global Initiative for the Elimination of Avoidable Blindness (WHO/PBL/97.61), 1997). It is estimated that childhood blindness secondary to cataract is responsible for 75 million blind years - an unfortunate occurrence. The prevalence of childhood cataract has been reported as 1 to 15 cases in 10,000 children with an estimated 130,000 to 200,000 children blind from bilateral cataract worldwide.1 Poor socioeconomic status, lack of awareness, lack of accessibility and lack of quality cataract surgery are major hurdles in the visual rehabilitation of age-related cataract in many parts of the developing world.2
In India and Nepal, surgical eye camps in the rural areas provide cheap and accessible services for the majority of people suffering from age-related cataract.3–8 However, poor outcomes from these camps have been reported due to poorly designed camps for adult cataract surgery.9–11 The question remains whether eye camp based pediatric cataract surgery can generate outcomes comparable to hospital based surgery.
Of clinical importance is the timing of surgical intervention in children which affects the visual outcomes to a much greater extent than the surgical modality or the postoperative optical correction.12–18 Early cataract surgery combined with suitable measures to address amblyopia is imperative for successful visual rehabilitation of a child with cataract. In developing countries, many parents delay proper evaluation and management of children with cataract and at times, camps held in the rural setting are the best means of diagnosing and providing these children with the necessary surgical facilities.
In this study, we report our experience of phacoaspiration with posterior chamber (PC) intraocular lens (IOL) implantation in children attending a well-equipped annual eye camp in North India compared to hospital based surgery.
MATERIALS AND METHODS
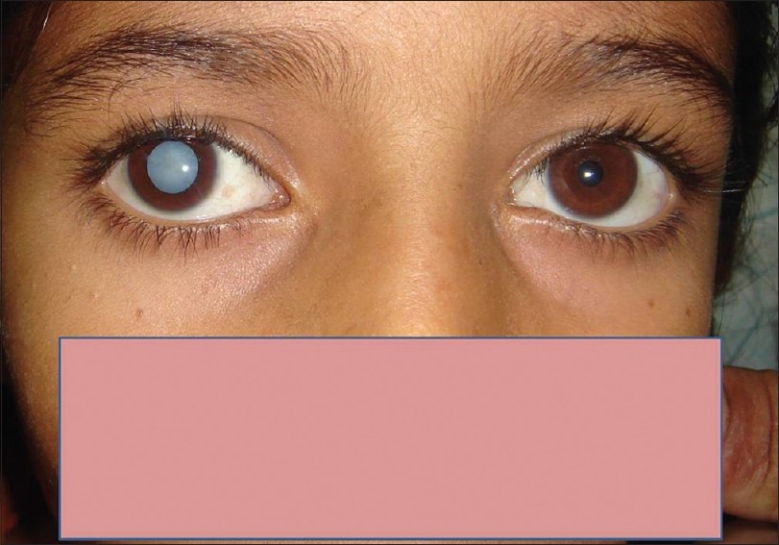
Of the 7200 patients undergoing cataract extraction at an annual eye camp organized by a charitable organization in rural Punjab, North India for one year (2001–2002), children aged 5 to 16 years with visually significant cataract were considered for inclusion in the study [Figure 1]. An approximately equal number of children were enrolled in a tertiary care hospital. Consecutive cases were included; however, surgery was performed at different times. Children with traumatic cataract, any associated ocular pathology such as uveitis, glaucoma, microcornea, ocular hypotony, retinal detachment, or vitreous hemorrhage and children with major cardio-respiratory or any other systemic disorders where the attending anesthetist found them unsuitable for anesthesia were excluded from the study.
Figure 1.

A group of children with visually significant cataract. Children are usually brought late for management of cataract particularly in the rural area
This study adhered to the guidelines of the declaration of Helsinki. The study was approved by the institute ethics committee (no NKG676). A detailed family history, history of trauma, education level child and socioeconomic status of the family were collected. Pediatric specialists carried out a thorough general physical examination. Preoperatively, a detailed ocular examination was performed on all children including best-corrected visual acuity (BCVA), slit lamp biomicroscopy after pupillary dilatation to document the type of cataract and the status of the anterior segment, intraocular pressure (IOP) with Goldman applanation tonometry or non-contact tonometry. The posterior segment was examined with ophthalmoscopy in eyes with relatively clear media. B-scan ultrasonography was performed in patients as clinically warranted,
IOL power was calculated using the Sanders-Retzlaff-Kraff (SRK II) formula18 with all eyes target for emmetropia in children between 8 and 16 years of age. The IOL calculations were undercorrected by 5% for children aged 5-7 years. Standard surgical guidelines were followed for surgery. The surgical technique for posterior capsule management in the primary surgery was similar in the two settings irrespective of age. Children who underwent surgery at the eye camp were from poor socioeconomic status and the procedure was provided free of cost.
Phacoaspiration was performed after continuous curvilinear capsulorhexis of 5-5.5 mm. The IOL was implanted in the capsular bag where possible. In cases that precluded capsular bag implantation, ciliary sulcus fixation of a PC IOL was performed. In all cases, polymethyl methacrylate (PMMA) IOL with optic diameter of 6 mm and overall length 12 mm (Auroab SQ3602, Aravind Hospital, Madurai, India) were implanted. Primary posterior capsulotomy (PPC) with anterior vitrectomy was performed in children with posterior polar or membranous cataract, or a posterior capsular plaque involving visual axis. Primary posterior capsulotomy (PPC) was performed using a vitrectomy cutter and the size of capsulotomy was kept between 3 and 3.5mm. All children under 8 years old underwent PPC and anterior vitrectomy. On the first postoperative day, all children received betamethasone 0.1%, 8-12 times a day for one week which was tapered over a period of next six weeks along with topical antibiotics (ciprofloxacin 0.3%) and homatropine 2% twice a day.
Follow up visits occurred at six weeks, six months and one year at eye camp or a hospital to record visual acuity, refraction, IOP and detailed slit lamp biomicroscopy. Management of posterior capsular opacification (PCO), amblyopia and other complications was performed at the tertiary care hospital. Occlusion therapy depending on the age of the child was full time during waking hours (6:1= six days of occlusion of the normal or pseudophakic eye and one day of occlusion of the postoperative eye) along with appropriate refractive correction within two-three weeks postoperatively.
Postoperative complications, visual results and follow up compliance were analyzed statistically using the Chi-square test. A P value less than 0.05 was considered significant.
RESULTS
In the eye camp, 96 children had pediatric cataract. Of these, 31 children with traumatic cataract and 6 children with developmental cataracts were not included in the study based on anesthesiology assessment. Hence, the eye camp group was comprised of 59 children with developmental cataract who met the inclusion criteria. In the TCC group, 48 of 64 children with visually significant cataract were included and 16 children with traumatic cataract were excluded.
All the children in the eye camp group belonged to a low socioeconomic status family with a rural background. Twenty one (35.60%) children had no formal education and 38 (64.40%) children were performing poorly at school. Cataract was hereditary in 15 of the 59 (25.42%) children.
In the TCC group, 22 of 48 (45.83%) children were from poor socioeconomic status. Twenty (41.67%) children in the TCC group were from a rural area and 28 (58.33%) from an urban area. Nine (18.75%) children had no formal education and 39 (81.25%) were performing poorly in school.
All children had visually significant cataract (central cataract 3mm or more) and visual acuity ranging from light perception to 20/400 preoperatively.
In the eye camp group, 32 (54.23%) children had zonular cataract, 12 (20.34%) had membranous cataract, 10 (16.94%) had total cataract, 4 (6.78%) had posterior polar and 1 (1.69%) child a unilateral anterior polar cataract. Associated findings were strabismus in 7 (11.86%) children and nystagmus in 6 (10.16%) children. The fellow eye was normal in 13 (22%) children [Figure 2].
Figure 2.
Right eye of a six-year-old child with unilateral cataract. Children with unilateral cataract are most susceptible to development of amblyopia if the cataract is not removed in a timely fashion. Occlusion therapy is a successful modality postoperatively
In the TCC group, 28 (58.33%) eyes had zonular cataract, 9 (18.75%) eyes had diffuse or total cataract, 6 (12.5%) eyes had posterior polar cataract, 3 (6.25%) eyes had membranous cataract and 2 (4.16%) eyes had posterior lenticonus. The fellow eye was normal in 8 (16.66%) eyes, pseudophakic in 28 (58.33%) eyes and cataractous in 12 (25%) eyes.
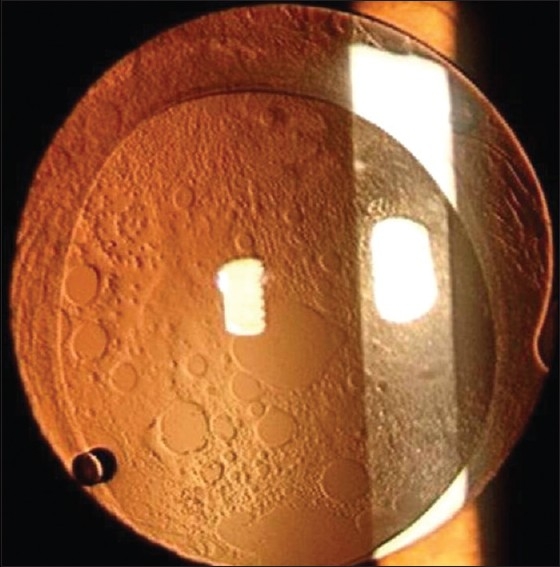
In the eye camp group, 40 (67.79%) eyes underwent phacoaspiration with intact posterior capsule and 19 (32.20%) eyes underwent PPC with anterior vitrectomy [Figure 3]. In the TCC group, 37 (77.08%) eyes underwent phacoaspiration with intact posterior capsule and 11 (22.92%) eyes underwent PPC with anterior vitrectomy. PPC with anterior vitrectomy was performed in children with posterior polar or membranous cataract or cataract with posterior capsule plaque impinging on the visual axis.
Figure 3.
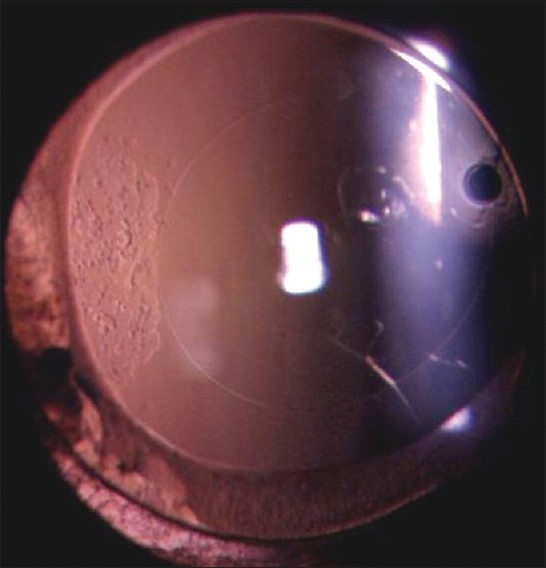
The same child as in Figure 2 after implantation with a polymethyl-methacrylate intraocular lens in the capsular bag after primary posterior capsulotomy and anterior vitrectomy. This child achieved 20/80 best corrected visual acuity in the right eye after surgery and underwent full time occlusion of the left eye (normal eye). After 12 months of follow up, right eye achieved best corrected visual acuity of 20/40
At last postoperative visit, 32 (54.23%) children in the eye camp group and 30 (62.5%) in the TCC group achieved BCVA of 20/40 [Table 1]. The difference in postoperative visual acuity was not statistically significant (P>0.05). In the eye camp group, the most common postoperative complications were visually significant PCO (61%) and uveitis (44.06%) [Table 2]. Visually significant PCO was managed with YAG laser capsulotomy / pars plana membranectomy with anterior vitrectomy [Figure 4]. In one case, pupillary capture was released with centration of the IOL. In the TCC group, 45.83% of eyes had PCO and 41.66% eyes had postoperative uveitis. PCO was managed surgically or with Nd: YAG laser capsulotomy [Table 2].
Table 1.
Visual outcome in pediatric cataract surgery in an eye camp verus a tertiary care center (hospital) setting
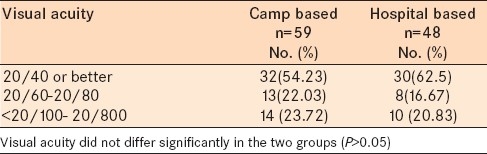
Table 2.
Postoperative complications in children undergoing pediatric cataract surgery in an eye camp versus a tertiary care center (hospital) setting
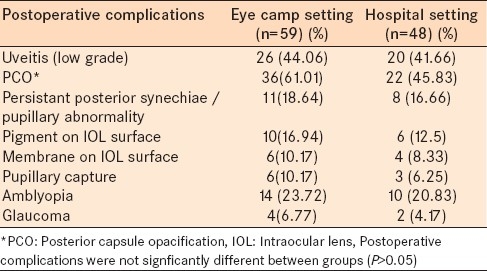
Figure 4.
Eye of a nine-years-old child implanted with all polymethyl-methacrylate intraocular lens in the capsular bag. Note visually significant posterior capsule opacification 15 months postoperatively. This child was treated with Nd: YAG laser capsulotomy to clear the visual axis
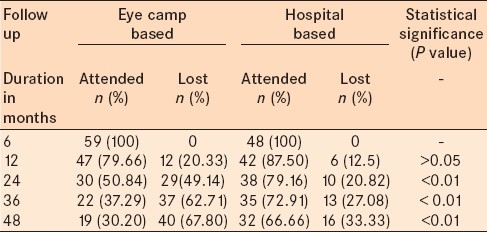
In the eye camp group, loss to follow up was 20% at 1 year, 49% at 2 years, 62% at 3 years and 67% at 4 years compared to 12.5, 21, 27 and 33% respectively in the TCC group [Table 3].
Table 3.
Follow up compliance of children in a tertiary care center (hospital) setting versus camp based surgery
DISCUSSION
Pediatric cataract surgery is highly refined due to well-developed microsurgical techniques.19–28 The decision to perform surgery and optimal timing are the most crucial factors for successful outcomes. Early surgery is recommended for unilateral cataract and bilateral visually significant cataracts.12–18 Visual rehabilitation of a child with congenital or developmental cataract requires a great degree of commitment and effort from the treating ophthalmologist, pediatrician as well as the parents. This is a time consuming, expensive and at times a frustrating exercise.
To achieve contemporary outcomes in pediatric cataract surgery, the ophthalmologist need to incorporate microsurgical techniques along with accurate selection of viscoelastic devices and intraocular lenses. In developing countries, very few centers have the skill, facility or equipment for performing pediatric cataract surgery with IOL implantation. Most of these centers are either tertiary care centers or private clinics which are located in the urban areas. The majority of the rural population is unable to access specialist care due to illiteracy, poor socio-economic status and lack of local surgical facilities. Favorable results have been reported after camp based IOL implantation for age-related-cataract3–8 but whether similar results are possible in the pediatric age group remains largely unaddressed.
Control of childhood blindness is one of the priorities identified for achieving the goals of Vision 2020. This is considered a priority because blind-years (number of years that a blind person lives after going blind) due to childhood blindness are second only to cataract and half of childhood blindness is avoidable (treatable/preventable). We utilized the services of an annual eye camp geared at adult cataract surgery which reduced the cost of management in children. Additionally, follow up and further surgical intervention was performed at a public sector tertiary care center to avoid any cost to the patient. All the surgical procedures and interventions in this study were performed free of cost to the patient.
The needs of children with cataract are different from that of adults. For example, management of the posterior capsule and aggressive amblyopia therapy are major factors governing the outcome of pediatric cataract surgery. Opacification of the posterior capsule occurs frequently and rapidly following cataract extraction in children.29–35 Obstruction of the visual axis occurs at a critical period of visual development and the major concern is amblyopia, especially in children with monocular cataracts. Strategies to maintain a clear visual axis coupled with amblyopia therapy are necessary to achieve visual rehabilitation.29–35 Although YAG laser capsulotomy is a simple and relatively safe procedure, its use is limited to older, more co-operative patients and the cost of equipment precludes widespread use in developing countries. In younger children, primary posterior capsulotomy and anterior vitrectomy have been advocated to avoid a second surgical intervention and to maintain a clear visual axis.21,29–34 Thirty eyes (19 eyes in the eye camp group and 11 eyes in the TCC group) had a primary posterior capsulectomy with anterior vitrectomy and all these eyes maintained a clear visual axis at six months postoperatively. Visually significant PCO was 16% higher in the eye camp group. However, this difference was not statistically significant. The frequency of complications such as postoperative uveitis, pupillary abnormality, IOL optic capture etc was similar between groups [Table 2].
After IOL implantation, the most important step is aggressive amblyopia management and spectacle correction. Most children with unilateral cataract who are in the visually immature stage will have varying density of amblyopia based on the timing of surgical intervention. Aphakia is an equivalent amblyogenic stimulus to the cataract itself. Alternately, an IOL provides a stable retinal image, ensures compliance and induces minimal aniseikonia.12–21 In this study, we instituted full-time occlusion therapy along with appropriate refractive correction within two to three weeks after surgery for children between 5 and 14 years. Compliance with amblyopia therapy was poor in the eye camp settings compared to the hospital setting.
In developing countries, many parents are unable to provide adequate care due to low socioeconomic status, lack of awareness regarding optimal management and poor accessibility to quality medical care. The majority of the children in this study were from a poor socioeconomic background and there was significant delay in seeking medical care.
Simultaneous bilateral cataract surgery in children has recently been reported by some authors.35,36 Simultaneous surgery may be a reasonable option for children from a poor socio-economic status as it reduces the cost of two surgical procedures and risk of anesthesia. We did not perform simultaneous bilateral cataract surgery in the eye camp setting due to the risk of infection. None of the children in the eye camp group had an infection postoperatively. Bourne et al., have reported much lower success in the eye camp setting due to lack of adequate postoperative rehabilitation of patients in eye camps.37 A study from Rajasthan, India reported poor postoperative outcomes attributable to a predominance of eye camp surgeries.38
The total cost of surgery including IOL and medicines per child in this series was borne by the Charitable Institution. The major expenses were the intraocular lens, and cost for use of A-scan, operating microscope, a vitrector and Nd: YAG laser system. The cost per case was offset by using equipment that is routinely used for adult camp based surgery (operating microscope, A-scan and biometer). The Nd: YAG laser system used was also in routine use at the government run tertiary care hospital where the operating surgeon works for the rest of the year. Nevertheless, it should to be emphasized that quality of surgery should not be sacrificed to save expenses.
Postoperative BCVA was similar between groups indicating eye camp surgery was safe, and had comparable results to a tertiary care center. The outcome in terms of visual axis clarity and final visual outcome was similar in the two settings for children who presented for follow up in a rural setting. More aggressive posterior capsule management may be appropriate for some children undergoing surgery at an eye camp (PPC) because of the low likelihood of follow up. Primary posterior capsulotomy and anterior vitrectomy was performed in all children below 8 years. We believe the surgeon may modify the criteria for PPC based on the child, the family, and the location of the surgery. However, further studies are warranted to evaluate this possibility.
The results of this study suggest that pediatric cataract surgery with PCIOL implantation in children in an eye camp setting is a viable method in developing countries for older children with poor socioeconomic status. These children should be carefully selected, and undergo surgery using an operating microscope and followed up at the eye camp and base hospital for management of PCO, amblyopia, glaucoma and refractive changes.
In the current study, the major drawback of pediatric cataract surgery in the eye camp was increased loss to follow up. In our study, there was progressive loss to follow up in the eye camp setting with only 30% children presenting for follow up at 4 years compared to 67% at the hospital. Low socioeconomic status and rural background could be significant deterrents for children attending the eye camp. This is clinically important because children require frequent follow up for refractive care, treatment of amblyopia, and to address complications (particularly post-IOL opacities) After cataract surgery, many children require visual rehabilitation. Such services should be planned for these children and it may be incorporated within the existing community ophthalmology program. Training the staff in vision assessment of children should be part of the curriculum. A very common occurrence is attrition of children on follow up. To overcome these hurdle, clinicians should devise a defaulter retrieval system, perhaps, through vision centers to ensure follow-up of children who have undergone cataract surgery. Rural eye camps provide a safe and reasonable venue to diagnose and operate on childhood cataracts. Follow up care is a major concern for rural based families, and systems need to be created to adequately address long-term follow up.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Foster A, Gilbert C, Rahi J. Epidemiology of cataract in childhood. A global perspective. J Cataract Refract Surg. 1997;23(Suppl):S601–4. doi: 10.1016/s0886-3350(97)80040-5. [DOI] [PubMed] [Google Scholar]
- 2.Ram J. Cataract blindness in India. Lancet. 1994;343:1228. doi: 10.1016/s0140-6736(94)92439-2. [DOI] [PubMed] [Google Scholar]
- 3.Kapoor H, Chatterjee A, Daniel R, Foster A. Evaluation of visual outcome of cataract surgery in an Indian eye camp. Br J Ophthalmol. 1999;83:343–6. doi: 10.1136/bjo.83.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murthy GV, Sharma P. Cost analysis of eye camps and camp based cataract surgery. Natl Med J India. 1994;7:111–4. [PubMed] [Google Scholar]
- 5.Ruit S, Brian G, Hollows F. On the practicalities of eye camp cataract extraction and intraocular lens implantation in Nepal. Int Ophthalmol. 1990;21:862–5. [PubMed] [Google Scholar]
- 6.Ruit S, Tabin GC, Nissman SA, Paudyal G, Gurang R. Low-cost high volume extracapsular cataract extraction with posterior chamber intraocular lens implantation in Nepal. Ophthalmology. 1999;106:1887–92. doi: 10.1016/S0161-6420(99)90397-4. [DOI] [PubMed] [Google Scholar]
- 7.Singh AJ, Garner P, Floyd K. Cost-effectiveness of public-funded options for cataract surgery, Mysore India. Lancet. 2000;355:180–3. doi: 10.1016/s0140-6736(99)07430-9. [DOI] [PubMed] [Google Scholar]
- 8.Johnson GJ. Improving outcome of cataract surgery in the developing countries. Lancet. 2000;355:158–9. doi: 10.1016/S0140-6736(99)00404-3. [DOI] [PubMed] [Google Scholar]
- 9.Pokharel GP, Selvaraj S, Ellwien IB. Visual functioning and quality of life outcomes among operated and unoperated blind populations in Nepal. Br J Ophthalmol. 1998;82:606–10. doi: 10.1136/bjo.82.6.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anand R, Gupta A, Ram J, Singh U, Kumar U. Visual outcome following cataract surgery in rural Punjab. Indian J Ophthalmol. 2000;48:153–8. [PubMed] [Google Scholar]
- 11.Limburg H, Foster A, Vaidyanathan K, Murthy GV. Monitoring visual outcome of cataract surgery in India. Bull World Health Organ. 1999;77:455–60. [PMC free article] [PubMed] [Google Scholar]
- 12.Ram J, Brar GS, Kaushik S, Sukhija J, Bandyopadhyay S, Gupta A. Primary intraocular lens implantation in the first two years of life: Safety profile and visual results. Indian J Ophthalmol. 2007;55:185–9. doi: 10.4103/0301-4738.31937. [DOI] [PubMed] [Google Scholar]
- 13.Brar GS, Grewal DS, Ram J, Singla M, Grewal SP. Square-edge polymethylmethacrylate intraocular lens design for reducing posterior capsule opacification following paediatric cataract surgery: Initial experience. Clin Experiment Ophthalmol. 2008;36:625–30. doi: 10.1111/j.1442-9071.2008.01818.x. [DOI] [PubMed] [Google Scholar]
- 14.Kuhli-Hattenbach C, Lüchtenberg M, Kohnen T, Hattenbach LO. Risk factors for complications after congenital cataract surgery without intraocular lens implantation in the first 18 months of life. Am J Ophthalmol. 2008;146:1–7. doi: 10.1016/j.ajo.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 15.Wilson ME, Trivedi RH. Multicenter randomized controlled clinical trial in pediatric cataract surgery: Efficacy and effectiveness. Am J Ophthalmol. 2007;144:616–7. doi: 10.1016/j.ajo.2007.06.033. [DOI] [PubMed] [Google Scholar]
- 16.Vasavada A, Chauhan H. Intraocular lens implantation in infants with congenital cataract. J Cataract Refract Surg. 1994;20:592–8. doi: 10.1016/s0886-3350(13)80644-x. [DOI] [PubMed] [Google Scholar]
- 17.Birch EE, Stager DR. The critical period for surgical treatment of dense, congenital, unilateral cataracts. Invest Ophthalmol Vis Sci. 1996;37:1532–8. [PubMed] [Google Scholar]
- 18.Nihalani BR, Vasavada AR. Single-piece AcrySof intraocular lens implantation in children with congenital and developmental cataract. J Cataract Refract Surg. 2006;32:1527–34. doi: 10.1016/j.jcrs.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 19.Wilson ME. Intraocular lens implantation. Has it become the standard of care for children? Ophthalmology. 1996;103:1719–20. doi: 10.1016/s0161-6420(96)30436-3. [DOI] [PubMed] [Google Scholar]
- 20.Pandey S, Ram J, Werner L, Brar GS, Jain A, Gupta A, et al. Visual results and postoperative complications of capsular bag and ciliary sulcus fixation of posterior chamber intraocular lenses in children with traumatic cataract. J Cataract Refract Surg. 1999;25:1576–84. doi: 10.1016/s0886-3350(99)00297-7. [DOI] [PubMed] [Google Scholar]
- 21.Ram J, Brar GS, Kaushik S, Gupta A, Gupta A. Role of posterior capsulotomy with vitrectomy and intraocular lens design and material in reducing posterior capsule opacification after pediatric cataract surgery. J Cataract Refract Surg. 2003;29:1579–84. doi: 10.1016/s0886-3350(03)00231-1. [DOI] [PubMed] [Google Scholar]
- 22.Zetterström C. Intraocular lens implantation in the pediatric eye. J Cataract Refract Surg. 1997;23:559–600. doi: 10.1016/s0886-3350(97)80039-9. [DOI] [PubMed] [Google Scholar]
- 23.Thakur J, Reddy H, Wilson ME, Jr, Paudyal G, Gurung R, Thapa S, et al. Pediatric cataract surgery in Nepal. J Cataract Refract Surg. 2004;30:1629–35. doi: 10.1016/j.jcrs.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 24.Simons BD, Siatkowski RM, Schiffman JC, Flynn JT, Capo H, Munoz M. Surgical technique, visual outcome, and complications of pediatric intraocular lens implantation. J Pediatr Ophthalmol Strabismus. 1999;36:118–24. doi: 10.3928/0191-3913-19990501-08. [DOI] [PubMed] [Google Scholar]
- 25.Sinskey RM, Stoppel JO, Amin PA. Long-term results of intraocular lens implantation in pediatric patients. J Cataract Refract Surg. 1993;19:405–8. doi: 10.1016/s0886-3350(13)80314-8. [DOI] [PubMed] [Google Scholar]
- 26.Zetterstrom C, Kugelberg U, Oscarson C. Cataract surgery in children with capsulorhexis of anterior and posterior capsules and heparin-surface-modified intraocular lenses. J Cataract Refract Surg. 1994;20:599–601. doi: 10.1016/s0886-3350(13)80645-1. [DOI] [PubMed] [Google Scholar]
- 27.Ben-Ezra D. Cataract surgery and intraocular lens implantation in children, and intraocular lens implantation in children. Am J Ophthalmol. 1996;121:224–6. doi: 10.1016/s0002-9394(14)70595-1. [DOI] [PubMed] [Google Scholar]
- 28.Zwaan J, Mullaney PB, Awad A, Al-Mesfer S, Wheeler DT. Pediatric intraocular lens implantation. Surgical results and complications in more than 300 patients. Ophthalmology. 1998;105:112–8. doi: 10.1016/s0161-6420(98)91568-8. discussion 118-9. [DOI] [PubMed] [Google Scholar]
- 29.Vasavada A, Desai J. Primary posterior capsulorhexis with and without anterior vitrectomy in congenital cataracts. J Cataract Refract Surg. 1997;23(Suppl):S645–51. doi: 10.1016/s0886-3350(97)80048-x. [DOI] [PubMed] [Google Scholar]
- 30.Basti S, Ravishankar U, Gupta S. Results of a prospective evaluation of three methods of management of pediatric cataracts. Ophthalmology. 1996;103:713–20. doi: 10.1016/s0161-6420(96)30624-6. [DOI] [PubMed] [Google Scholar]
- 31.Ben-Ezra D, Cohen E. Posterior capsulectomy in pediatric cataract surgery: The necessity of a choice. Ophthalmology. 1997;104:2168–74. doi: 10.1016/s0161-6420(97)30045-1. [DOI] [PubMed] [Google Scholar]
- 32.Gimbel HV. Posterior continuous curvilinear capsulorhexis and optic capture of the intraocular lens to prevent secondary opacification in pediatric cataract surgery. J Cataract Refract Surg. 1997;23(Suppl):S652–6. doi: 10.1016/s0886-3350(97)80049-1. [DOI] [PubMed] [Google Scholar]
- 33.Koch DD, Kohnen T. Retrospective comparison of techniques to prevent secondary cataract formation following posterior chamber intraocular lens implantation in infants and children. J Cataract Refract Surg. 1997;23 Suppl:S657–63. [PubMed] [Google Scholar]
- 34.Mackool RJ. Management of posterior capsule during intraocular lens implantation. Am J Ophthalmol. 1994;117:121–3. doi: 10.1016/s0002-9394(14)73033-8. [DOI] [PubMed] [Google Scholar]
- 35.Zwaan J. Simultaneous surgery for bilateral pediatric cataracts. Ophthalmic Surg Lasers. 1996;27:15–20. [PubMed] [Google Scholar]
- 36.Totan Y, Bayramlar H, Cekic O, Aydin E, Erten A, Daglioglu MC. Bilateral cataract surgery in adult and pediatric patients in a single session. J Cataract Refract Surg. 2000;26:1008–11. doi: 10.1016/s0886-3350(00)00380-1. [DOI] [PubMed] [Google Scholar]
- 37.Bourne RR, Dineen BP, Ali SM, Huq DM, Johnson GJ. Outcomes of cataract surgery in Bangladesh: Results from a population based nationwide survey. Br J Ophthalmol. 2003;87:813–9. doi: 10.1136/bjo.87.7.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murthy GV, Ellwein LB, Gupta S, Tanikachalam K, Ray M, Dada VK. A population-based eye survey of older adults in a rural district of Rajasthan: II. Outcomes of cataract surgery. Ophthalmology. 2001;108:686–92. doi: 10.1016/s0161-6420(00)00578-9. [DOI] [PubMed] [Google Scholar]


