Abstract
Orbital cellulitis is an uncommon condition previously associated with severe complications. If untreated, orbital cellulitis can be potentially sight and life threatening. It can affect both adults and children but has a greater tendency to occur in the pediatric age group. The infection most commonly originates from sinuses, eyelids or face, retained foreign bodies, or distant soources by hematogenous spread. It is characterized by eyelid edema, erythema, chemosis, proptosis, blurred vision, fever, headache, and double vision. A history of upper respiratory tract infection prior to the onset is very common especially in children. In the era prior to antibiotics, vision loss from orbital cellulitis was a dreaded complication. Currently, imaging studies for detection of orbital abcess, the use of antibiotics and early drainage have mitigated visual morbidity significantly. The purpose of this review is to describe current investigative strategies and management options in the treatment of orbital cellulitis, establish their effectiveness and possible complications due to late intervention.
Keywords: Diagnosis, Intracranial Extension, Management, Orbital Abscess, Orbital Cellulitis, Vision Loss
INTRODUCTION
Orbital cellulitis is a relatively uncommon infective process involving ocular adnexal structures posterior to the orbital septum.1 Inflammation anterior to the orbital septum or preseptal cellulitis is common in young children. It rarely involves postseptal anatomy, and physical examination reveals eyelid edema in the absence of orbital signs such as gaze restriction and proptosis.2 Orbital cellulitis is a condition that rarely causes complete loss of vision if treated in a timely fashion. A history of upper respiratory tract infection prior to the onset is very common especially in children. For simplification, Chandler et al.3 has classified the disease into five categories and emphasized the possibility of fatality due to cavernous sinus thrombosis and intracranial abscess. Despite advances in antimicrobial therapy and surgical methods, intracranial abscess remains a challenging problem and the mortality rate can be as high as 40%.4 In the past, orbital cellulitis has been associated with a number of serious complications including loss of visual acuity, cavernous sinus thrombosis, meningitis, frontal abscess and osteomyelitis, and even death.1,5 Since the advent of effective antibiotic treatment, these serious complications have become much less frequent. Prior to the availability of antibiotics, blindness was a relatively common complication of orbital cellulitis, reported in approximately 20% of cases.6 Case reports of blindness following bacterial orbital cellulitis in the postantibiotic era are rare. For example, Connel et al.,7 reported a case of a 69-year-old male who presented with fulminant onset of proptosis, significant ophthalmoplegia and no light perception. Despite emergent drainage of an orbital abscess and aggressive intravenous antibiotic therapy, there was no improvement in vision; although ocular motility returned to normal.7 The mechanism of vision loss in Connel et al.7 case remained unknown. The authors postulated streptococcal-related ischemic necrosis of the posterior aspect of the optic nerve as a possible mechanism of vision loss. In a recent survey of 52 patients with orbital cellulitis, 18 (35%) presented with decreased visual acuity; however, with long-term follow-up, only two (4%) patients had decreased vision.5
PRESENTATION
The clinical features of orbital cellulitis included proptosis, swelling of the eyelids, conjunctival chemosis, and limited ocular motility.1 There may be exposure keratopathy resulting in corneal ulceration. The vast majority of these patients present with local symptoms such as edema, erythema, pain, chemosis, decreased ocular motility, and proptosis [Figure 1]. To differentiate between more superficial infections and orbital cellulitis, signs, and symptoms resulting from inflammation may be helpful.2 Specifically, the incidences of decreased visual acuity, proptosis and external ophthalmoplegia are more closely associated to orbital cellulitis.1 Temperature greater than 37.5°C and leukocytosis resulting in fever is a more prominent feature in the pediatric group. External ophthalmoplegia and proptosis may be the most common features, while decreased visual acuity and chemosis may be less frequent in pediatric cases as well as in adults. Involvement of the optic nerve may produce papilledema or neuritis with rapidly progressing atrophy resulting in blindness. One factor in determining the atrophy is mechanical pressure. A second is compression of the central retinal and other feeding arteries,8 but the orbital inflammation may spread directly into the substance of the nerve with the appearance of small necrotic areas or an abscess.6 In addition to the infarction of the optic nerve, infarction of the sclera, choroid, and the retina may occur. A septic uveitis, iridocyclitis, or choroiditis with cloudy vitreous, including septic panophthalmitis may develop. Glaucoma may be a rare complication of orbital cellulitis in which case the patient may present with reduction in the visual field or an enlarged blind spot. In some cases, there may be no pathologic evidence in the fundus.
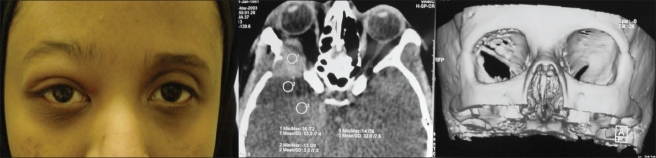
Figure 1.

External photograph of a 10-year-old male child who presented with right eyelid edema, swelling along with proptosis who was found to have evidence of ethmoiditis and maxillary sinusitis along with subperiosteal abscess requiring drainage
PREDISPOSING FACTORS
The most common predisposing factor for orbital cellulitis is sinus disease, particularly in the younger age groups.1,5 The infection most commonly originates from sinuses [Figure 2], eyelids, face, dental abscess, retained foreign bodies, or distant soources by hematogenous spread.1,5,9–11 Chandler et al.3 has grouped complications of sinusitis into five classes. In group 1, the eyelids are swollen with the presence of orbital content edema (preseptal cellulitis). The swelling reflects an impedance to drainage through ethmoid vessels. Venous congestion is transmitted through the valveless veins to the eyelids and through the superior ophthalmic vein to the orbit. In group II (orbital cellulitis), there is a diffuse infiltration of orbital tissues with inflammatory cells. The eyelids may be swollen and there may be conjunctival chemosis with variable degree of proptosis and visual loss. In group III (subperiosteal abscess), purulent material collects periorbitally and in the bony walls of the orbit. There is pronounced eyelid edema, conjunctival chemosis, and tenderness along the affected orbital rim with variable degree of motility, proptosis, and visual acuity changes depending on the size and location of the abscess. In group IV (orbital abscess), there is a collection of pus inside or outside the muscle cone due to progressive and untreated orbital cellulitis. Proptosis, conjunctival chemosis, decreased ocular motility, and visual loss may be severe in these cases. In group V (cavernous sinus thrombosis), there is an extension of orbital infection into the cavernous sinus that can lead to bilateral marked eyelid edema and involvement of the third, fifth, and sixth cranial nerves. There may be associated generalized sepsis, nausea, vomiting, and signs of altered mentation. An orbital apex syndrome, characterized by proptosis, eyelid edema, optic neuritis, ophthalmoplegia, and neuralgia of the ophthalmic division of the fifth cranial nerve is caused by sinus disease around the optic foramen and superior orbital fissure.12
Figure 2.
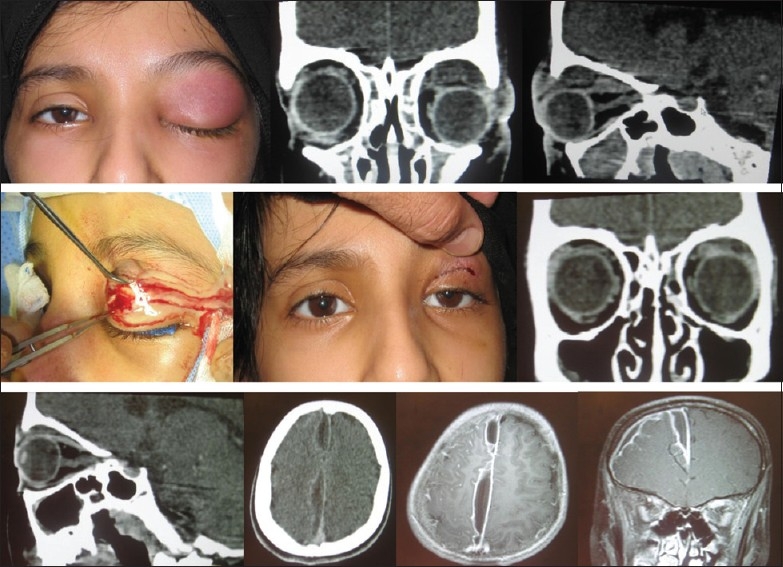
A 12-year-old female who presented with left upper eyelid swelling, pain and proptosis of left eye who was found to have evidence of panophthalmitis and superior orbital abscess. Soon after orbital abscess drainage, patient's upper eyelid swelling and diplopia resolved. Repeat CT-scan revealed evidence of the treated sinusitis as well as orbital abscess. Prior to discharge the patient complained of nausea, vomiting and lethargy. Repeat imaging studies CT-scan and MRI of orbits and brain revealed a sudural empyema and meningitis for which she was treated successfully
The outcomes from one of the largest series of orbital cellulitis from a developing country confirms previous observations from Western countries in which sinus infection has been implicated as the cause of orbital cellulitis in most of the reported cases.1 Specifically in the pediatric population, up to 90% of patients with orbital cellulitis had existing sinusitis, with almost half having multiple sinus involvement. Unlike patients in Western countries, most patients with sinusitis and orbital cellulitis sought treatment later in the course of their disease in this study. After sinusitis, periocular trauma and history of ocular or periocular surgery were the cause of a significant number of cases of orbital cellulitis among these patients, compared with the studies of orbital cellulitis from Western countries.5,8 Less commonly reported causes of orbital cellulitis, such as dacryocystitis, dental infection, and endophthalmitis also were found among these patients [Figure 3]. Sinusitis may also produce osteomyelitis and intracranial abscess. Osteomyelitis, commonly involving the frontal bone, is a direct extension of frontal infection or septic thrombophlebitis via the valveless sinus of Breschet.13 Osteomyelitis is rare in the ethmoids because from this location, infection can rapidly spread through the thin lamina papyracea into the orbit or maxilla, where arterial anastomoses are sufficient to prevent necrosis due to septic thrombosis of a single artery. Although meningitis is the most common intracranial complication of sinus disease, epidural, subdural, and brain parenchymal abscess can also occur.13
Figure 3.
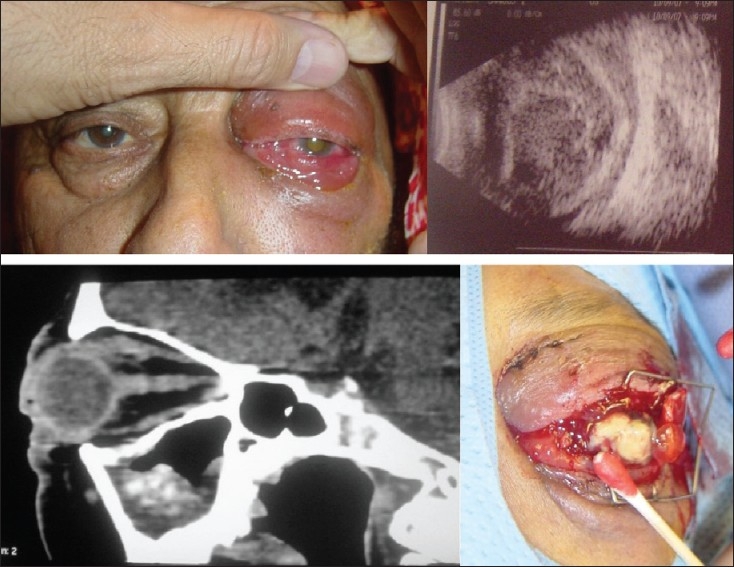
A 68-year-old male with diabetes presented with left eyelid swelling, proptosis, and decreased vision. Imaging studies revealed evidence of panendophthalmitis along with orbital cellulitis. Sinus surgery as well as evisceration revealed evidence of fungal infection
SOURCES OF INFECTION
Orbital cellulitis is a disease primarily of children and adolescents with an age distribution ranging between 0–15 years. The relatively incomplete immunologic development in this age group is proposed as the cause of the higher occurrence in children and adolescents.5 In the reported series, sinus disease has been found to be the most common predisposing factor. In the pediatric group, 91% of patients may have radiologically confirmed sinus disease, the most common being ethmoid and maxillary sinuses.1,5 Ethmoidal sinusitis has been demonstrated as the source of infection ranging from 43% to 75% of patients in various series.14,15 Ethmoidal disease is usually present with maxillary infection on the same side.15,16 Frontal sinus disease has been frequently identified especially in series with study population comprised of large numbers of adolescents and adults.8,14,16
Up to 38% of children may have multiple sinus involvement and in adult patients, up to 50% may have underlying sinus disease, while up to 11% may have multiple sinus involvement.1,5 Preceding upper respiratory tract infection, dental abscess may also result in orbital cellulitis. Other etiological factors resulting in orbital cellulitis may include dacryocystitis with orbital extension, retained foreign body, panophthalmitis, infected tumor, and mucormycosis.1 As orbital cellulitis has a close relationship with sinus and upper respiratory disease, a seasonal distribution paralleling that of upper respiratory infections has been documented with a bi-model seasonal distribution of cases with peak occurance in late winter/early spring.1,5 A subperiosteal abscess results from the accumulation of purulent material between the periorbita and the orbital bones, and usually occurs as a complication of bacterial sinusitis.3,16 The recognition of subperiosteal abscess as a specific entity within the general clinical setting of orbital cellulitis has increased dramatically since the introduction of computed tomography scanning (CT-scan) and has been the subject of numerous studies, and management has been the source of some controversy.16,17 Citing reports of rapidly progressive visual and intracranial complications from such an abscess, some authors have forcefully argued for prompt surgical drainage of the abscess and paranasal sinuses when a subperiosteal abscess is first diagnosed with CT scanning.13,16–21
EPIDEMIOLOGY
The frequency of orbital complications from sinus infection ranges from 0.5% to 3.9%; however, the incidence of orbital or periorbital abscesses varies considerably from 0% to 25% in different studies.13 Reviews from Children's Memorial Hospital in Chicago (87 patients) and Children's Hospital in Pittsburgh (104 patients) reported no cases of abscess formation among patients admitted for preseptal and orbital cellulitis.22,23 A much larger study from Hospital for Sick Children in Toronto (6770 patients) reported that 159 developed orbital complications (2.3%); of these, 17 (10.7%) had abscess formation.15 Among 158 patients admitted to Children's Hospital National Medical Center with preseptal/orbital cellulitis, there was a 20.8% incidence of orbital or periorbital abscess formation.24
Among other series which have reported orbital complications of sinus disease, the incidence of abscess formation varies from 6.25% to 20% to as high as 78.6%.14,25,26 The differences among these studies may be due to inclusion criteria, age group and the severity of the complications. Although, the incidence of major complications following sinusitis is low, such complications are associated with considerable morbidity and mortality.1,13 In the preantibiotic era, orbital cellulitis resulted in death from meningitis in 17% of cases and blindness in 20%.3 Once antibiotics were available, 1.9% of patients with orbital cellulitis developed meningitis, despite prompt treatment with systemic antibiotics.27 Despite aggressive treatment with antibiotic and drainage surgery, orbital abscesses may be devastating.13 In a series in which final visual results were reported, 7.1% to 23.6% of patients were left with blind eyes.8 Visual loss may be due to optic atrophy, central retinal artery occlusion, or exposure keratopathy with ulcer formation.1,8,15 Other hypothesized mechanisms of visual loss are septic optic neuritis, embolic, or thrombotic lesions in the vascular supply to the retina, choroid, or optic nerve, and a rapid elevation of intraocular pressure. Delayed surgical intervention is likely to produce poor visual results.15–20
INVESTIGATIONS
Although ultrasonography (U/S) can be useful as an in-office screening procedure in cases of suspected orbital abscesses, CT-scan is necessary to assess the sinuses and intracranial extension. On orbital U/S, orbital abscess may show low internal reflectivity. On CT-scan, one may see a localized, generally homogenous elevation of the periorbita adjacent to an opacified sinus. Imaging studies may show evidence of inflammatory or infective changes in the orbital structures. In the pediatric group, more patients may have subperiosteal abscess as compared to the adult group at the time of initial presentation. For example, in the series reported by Ferguson and McNab,5 among children, 29% had inflammatory change only, 62% had a subperiosteal abscess, while only 9% had orbital abscesses, compared with 72%, 5%, and 22%, respectively, in the adult group. In addition to its essential role in the diagnosis of orbital abscess, CT-scan may also influence the initial therapeutic plan by demonstrating the size and location of the abscess and the specific sinuses involved, factors that may be considered if surgical drainage is considered.1,16 However, CT-scan characteristics of subperiosteal collection may not be predictive of the clinical course. For example, the findings in patients who recovered with antibiotic therapy alone were similar to the findings in patients who underwent surgical drainage.17 It has been shown that the size of an orbital abscess on imaging studies may increase during the first few days of intravenous antibiotics regardless of the bacteriologic response to the treatment.17 The identification of orbital abcess is a diagnostic challenge. The reliability of CT-scan in demonstrating orbital abcess has been questioned. In a series of 25 cases of orbital infection, all 15 orbital abscesses were satisfactorily demonstrated provided the CT examination included coronal sections.28 According to this study, one-third of abscesses would have been missed if coronal sections had been omitted. Magnetic resonance imaging (MRI) may be necessary in some cases where CT-scan have not satisfactorily addressed clinician's concerns with other imaging techniques.
The development of an orbital abscess does not correlate specifically with visual acuity, proptosis, chemosis, or any other sign.13 Therefore, diagnostic procedures are essential in evaluating the patient with orbital cellulitis for possible abscess or retained orbital foreign body. Sinus x-ray can demonstrate an air-fluid level, if present, in an abscess cavity; however, gas-free abscesses may not be readily visible.13 Ultrasound can detect an abscess of the anterior orbit or medial wall with 90% efficiency,20 although an acute abscess may be poorly delineated. The investigative procedure of choice to diagnose orbital infection is the CT-scan.1,29 Orbital walls, extraocular muscles, optic nerve, intraconal area, and adipose tissue can be clearly seen. An orbital abscess is visualized as a homogenous, a ring-like, or a heterogeneous mass and the site of origin, orbital or subperiosteal, and extent of abscess are readily visible.1,17 Contrast-media can enhance the surrounding wall of an abscess. CT-scan does not differentiate between preseptal cellulitis and eyelid edema but will differentiate between preseptal and orbital cellulitis.13 Sinus disease and intracranial complications will also be evident on CT-scan, as will most foreign bodies. Thus, CT-scan is the most comprehensive source of information on orbital infections and the most sensitive means of monitoring the resolution of orbital or intracranial lesions. CT-scan is indicated in all patients with periorbital inflammation in whom proptosis, ophthalmoplegia, or a decrease in visual acuity develops, also in cases where a foreign body or an abscess is suspected, in cases where severe eyelid edema prevents an adequate examination, or in whom surgery is contemplated.1,13,16,17,29
BACTERIOLOGY OF ORBITAL ABSCESSES
Commonly reported bacteria from the abscesses of the orbit include Staphylococcus aureus, Staphylococcus epidermidis, Streptococci, Diphtheroids, Haemophilus influenza, Escherichia coli and multiple species including aerobes and anaerobes. No growth in up to 25% of abscesses.13 The results of microbiological investigation by Ferguson and McNab5 varied with differences in the rate of testing between the pediatric age group and the older age group. Some form of culture was performed in 93% of their patients.5 Among 50% of patients, who had blood cultures performed, none yielded positive results.5 In their5 study, cultures taken from abscesses were more likely to produce positive results. There was no correlation between conjunctival swab cultures and the etiological organism recovered from the abscesses of patients with positive cultures.5 S. aureus was the most common pathogen.5 In the pediatric group various species of Streptococcus predominated.5 Anaerobic Streptococcus was isolated in four pediatric patients, two cases with mixed anaerobes and one with Clostridium bifermentans.5 Anaerobic orbital cellulitis was much less common in adults, with only one case of mixed anaerobes. Multiple organisms were isolated in only five adults and four pediatric patients. No pathogens were isolated from six adults and 15 pediatric patient by Ferguson and McNab.5 In the past, H. influenza was a major pathogen responsible for orbital cellulitis in the pediatric age group.1,13 In the series reported by Ferguson and McNab,5 no cases of H. influenza were detected in the pediatric age group and only one case was found in an adult patient. The authors5 attributed this observation due to the general immunization of children with H. influenza type B vaccine since the early 1990s.
The bacteriology of orbital abscesses has received little attention. In a study of cultures of the contents of the abscess cavity, a wide range of organisms including S. aureus, S. epidermidis and Streptococci, H. influenza, E. coli, and diptheroids have been reported. The role of anaerobes, not usually considered pathogens in sinus disease, is unclear. However, a considerable number of cultures in adults have yielded anaerobes.1,16,18 Patients in the first decade of life generally have infections caused by single aerobic pathogens which are usually responsive to medical therapy alone. Patients older than 15 years of age have complex infections caused by multiple aerobic and anaerobic organisms that are slow to clear despite medical and surgical intervention.18 The complexity of pathogens and responsiveness to antimicrobial therapy appear to be age related.16,30 As the size of the sinus cavities enlarge, the ostia appear to narrow with increasing age creating optimal conditions for anaerobic bacterial growth. With increasing age, there is a trend toward more complex infections. In mixed infections, aerobes consume oxygen which encourages anaerobic microbial growth. Additionally, anaerobes produce B-lactamase that renders antibiotics ineffective. Harris,16 reviewed the microbiology results of 37 of his patients with orbital abscesses. Twelve patients were younger than 9 years. Of these, 58% were culture negative and the rest had a single aerobic pathogen. Sixteen patients between ages 9–14 years showed a transition toward more complex infections.16 Nine patients older than 15 years, were all culture positive after more than 3 days of antibiotic therapy. From the older group, polymicrobial infections were recovered more often and anaerobes were found in all cases.16
From their vast experience with orbital abscesses, Harris and Garcia,18 concluded that surgical therapy for orbital abscesses should be influenced by several factors, including the visual status, the size and location of the orbital abscess, intracranial complications, the sinuses involved, the presumed pathogens, and the anticipated bacterial response to antibiotic treatment. Harris and Garcia recommended emergency drainage of the orbital abscesses and sinuses of patients of any age whose optic nerve or retinal function is compromised. Urgent drainage was also recommended for large abscesses or extensive superior or inferior abscesses that might not resolve quickly, even if sinusitis is medically cleared. Urgent drainage was also recommended for intracranial complications at the time of presentation and in frontal sinusitis, in which the risk of intracranial extension is increased, and when complex infections that include anaerobesare suspected. An expectant approach has been recommended for patients younger than 9 years of age in whom simple infections are suspected. Surgery may be warranted if: there is no clinical improvement in a timely manner; relative afferent pupillary defect develops at any time; fever does not abate within 36 h, suggesting that the bacteremia is not responding to the choice of antibiotics; if there has been deterioration despite 48 h of appropriate antibiotic therapy or no improvement despite 72 h of treatment. Improvement of CT findings should be expected to lag behind the clinical picture. In fact, the CT findings may seem worse during the first few days of hospitalization despite successful treatment with antibiotics alone.17
Microbes can cause necrotizing lid disease that is often referred as necrotizing fascitis.7,31–33 This may progress to systemic manifestation including potentially fatal toxic streptococcus syndrome, characterized by multiorgan failure.31,33 These complications can occur in the absence of antecedent health problems or history of trauma.7,32,33 The virulence of this organism is related to the production of M proteins and exotoxins A and B.34 These proteins act as super-antigens in vitro and mediate tissue necrosis by causing massive release of cytokines such as tumor necrosis factors and interleukins.
TREATMENT
Intravenous antibiotics are usually started once the diagnosis of orbital cellulitis is suspected. Broad-spectrum antibiotics that cover most gram positive and gram negative bacteria should be selected. Antibiotic recommendations are based on the microorganisms most frequently recovered from abscesses; S. aureus, S. epidermidis, Streptococci, and Haemophilus species.13 Mixed infections including aerobic and anaerobic species may be found.16 Cultures from the conjunctiva, nose and throat are usually not representative of the pathogens cultured from the abscesses and blood cultures may be frequently negative.13 In many studies, a combination of a third-generation cephalosporin and flucloxacillin is used.1,5 Most patients receive oral antibiotics on discharge for varying periods of time. For example, all patients in the Ferguson and McNab5 study received intravenous antibiotic treatment and most of their patients had received multidrug therapy with up to five different antibiotics. In all cases treatment regimens were empirically based and instituted prior to identification of the pathogens.5
Patient age has been identified as a factor in the bacteriology and response to treatment of orbital abscess. In general, children less than 9 years of age have been found to have simpler, more responsive infections, primarily involving a single aerobic pathogen. Older children and adults may have more complex infections caused by multiple aerobic and anaerobic organisms, refractory to both medical and surgical treatment.16 In addition to starting intravenous antibiotics, emergent drainage of the orbital abscesses has been suggested in patients with compromised vision regardless of age. Urgent drainage (within 24 h of presentation) has been recommended for large abscesses, for extensive superior or inferior orbital abscesses, for patients with intracranial complications, for infections of known dental origin in which anaerobes might be expected.16 An individualized therapeutic approach requires a clinician to carefully follow these children and to exercise surgical option if improvement does not occur in a timely fashion. Careful monitoring of the clinical course is mandatory and comparison of serial CT-scan may be necessary as an adjunct to clinical judgment. In a previous study by Harris,16 children younger than 9 years old recovered with antibiotic treatment alone with successful clinical outcomes. Harris16 describes a “sliding scale” of risk associated with increasing age and argues that patients in the older age group who present with orbital cellulitis should undergo prompt sinus surgery, even before orbital or intracranial abscesses develop. Once sinus infection in older children or adults has extended in the orbit as an abscess, urgent drainage should include the orbit and all infected sinuses.16 CT-scan may not be accurate in assessing clinical course in some of these patients. In a review of 37 cases of orbital abscesses, Harris16, found that subperiosteal material could not be predicted from the size or relative radiodensity of the collections in CT scans.17 Initial scans were not predictive of the clinical course. Serial scans showed enlargement of abscesses during the first few days of intravenous antibiotic therapy, regardless of the ultimate response to treatment. Harris, concluded that expansion of orbital abscess in serial CT scans during the first few days of treatment should not be equated to failure of the infection to respond to antibiotics alone.17
SURGICAL INTERVENTION
Surgical treatment is indicated for significant underlying sinus disease, orbital or subperiosteal abscess or both in the pediatric age group. In adults, sinus surgery remains the most common surgical intervention. The argument remains between early drainage of orbital abscess to prevent complications versus the possibility of seeding the infection through early surgery.16 Harris has outlived a useful approach in the management of an orbital abscess.16 He recommends emergency drainage for patients of any age, whose visual function is compromised. Urgent drainage, usually within 24 h, is indicated for the following: large orbital abscess causing discomfort, superior or inferior orbital abscess, evidence of intracranial extension, involvement of frontal sinuses, and a known dental source of the infection in patients older than 9 years [Figure 4].16 An expectant approach is indicated for patients younger than 9 years with medial subperiosteal abscess of modest size, no visual loss and no intracranial or frontal sinus involvement. Careful evaluation and close monitoring of the optic nerve function and the level of consciousness and mental state of the patient is very important. An incision down to the periosteum at the inner quadrant of the orbit may be made to drain the subperiosteal abscess. A drain may be inserted and tissues may not need to be sutured, but left to granulate. The drain may be left in place for 7–8 days. Functional endoscopic sinus surgery (FESS) has been shown to be effective for the treatment subperiosteal abscess due to complication of paranasal sinusitis. The advantage of FESS is the avoidance of external ethmoidectomy and associated external facial scar and an early drainage of the affected sinuses and subperosteal abcess.35
Figure 4.

External photograph of a 27-year-old female patient who presented with left periocular edema, pain and decreased vision after a fall several days earlier. Imaging studies confirmed evidence of sinusitis and orbital fracture. Ultrasonography of her left eye revealed a stretched optic nerve along with compression on the eye. During exploration, an abscess was drained from the left lower eyelid that was connected to her maxillary sinus
COMPLICATIONS
There are few major complications following treatment of orbital cellulitis. Ferguson and, McNab5 reported no loss of vision after resolution of infections. Only one patient from the pediatric age group had proptosis on follow-up; one had ophthalmoplegia and one had recollection of abscess.5 One of their5 adult patients developed presumed meningitis, and another adult patient required enucleation.
MECHANISM OF VISUAL LOSS IN ORBITAL CELLULITIS
Permanent loss of vision has been noted as a complication of orbital infection since 1893 and blindness was reported in up to 20% of patients with postseptal inflammation in the preantibiotics era.6 However, permanent loss of vision resulting from orbital inflammation is unusual in this era of antibiotics.20,21 In a previous study, 4 of 38 patients with postseptal disease had permanent loss of vision with one of these patients progressing to no light perception.21 The mechanism for loss of vision with orbital inflammation may involve: (1) optic neuritis as a reaction to adjacent or nearby infection; (2) ischemia resulting from thrombophlebitis along the valveless orbital veins or; (3) compressive/pressure ischemia possibly resulting in central artery occlusion.6,21 Because clinical examination by itself may not exactly delineate the nature of postseptal inflammatory processes, clinicians may have to rely on imaging studies to select potential surgical candidates. Despite modern imaging techniques, the clinician must rely on the clinical progression of the inflammation based on visual acuity testing, pupillary reactivity, and ocular motility assessment. Patt and Manning,21 reported four cases of permanent blindness as a result of postseptal orbital inflammation. In each case, CT-scan readings of “no definite abscess” contributed to delay in diagnosis of orbital abscess, with a resultant delay in surgical drainage.
The ethmoidal sinuses are separated from the orbital contents by the lamina papyracea and anterior and posterior ethmoidal foramina serve as additional connections that may allow infection to gain access from ethmoidal air cells to the orbital contents. The periorbita in this area is loosely attached to bone and may be elevated by a purulent collection, resulting in subperiosteal abscess. Severe irreversible visual loss may occur in cases with orbital and subperiosteal abscess. In a survey of 46 cases with a confirmed diagnosis of orbital and subperiosteal abscess in which visual results were reported, permanent blindness developed in seven (15%) cases.36 In four cases, blindness was attributed to central retinal artery occlusion, in two cases optic atrophy occurred, and in one case no details were provided. Irreversible visual loss in orbital cellulitis probably has a vascular cause, whereas cases with reversible visual loss that respond to antibiotic therapy and drainage procedures most likely are due to infiltrative or compressive optic neuropathy. The confinement of the optic nerve in the orbital apex and within the bony canal and its proximity to the posterior ethmoid and sphenoid sinuses magnify the importance of the casual factors in posterior orbital cellulitis. Clinicians should be aware that patients with sinusitis and associated orbital cellulitis are at risk for developing severe visual loss and should be treated promptly. Hornblass13 reviewed 148 patients from 13 series reporting orbital abscess and found three cases of no light perception vision.
Acute visual loss may be associated with acute sinusitis either secondary to complicated orbital cellulitis or as a part of the orbital apex syndrome.37 El-Sayed and Muhaimeid,37 reported two cases of acute visual loss as a complication of orbital cellulitis due to sinusitis. In one patient dramatic improvement in vision from hand motion to normal vision resulted after intravenous treatment of pansinusitis and associated orbital cellulitis.37 A second patient (a 10-year-old female) recovered vision from no light perception to normal levels after exploration of the sphenoid and ethmoid sinuses along-with intravenous antibiotics. Slavin and Glaser,36,37 described three cases of sphenoethmoiditis causing irreversible visual loss associated with minimal signs of orbital inflammation and renamed the entity “posterior orbital cellulitis.” Slavin and Glaser36,37 defined it as a clinical syndrome in which early severe visual loss overshadows or precedes accompanying inflammatory orbital signs. Acute blindness may also result from orbital infarction syndrome. Orbital infarction is a disorder that may occur secondary to different mechanisms such as: (i) acute perfusion failure, that is, common carotid artery occlusion; (ii) systemic vasculitis, that is, giant-cell arteritis; (iii) orbital cellulitis with vasculitis, that is, mucurmycosis. The blindness and retinal and optic nerve damage can be permanent.38 In developing countries, most patients with sinusitis and orbital abscess tend to present late in the course of the disease. Most patients with refractory or complicated subperiosteal abscesses are older children or adults. For example, in one of the largest studies reported, four patients were permanently blind out of 159 patients with orbital complications of sinusitis.21 All four had surgically confirmed subperiosteal abscess, and all were 15 years of age or older. In another study, among the 13 patients with intracranial abscess that resulted from sinusitis or orbital abscesses, two patients were 9 to 14 years of age and 11 were 15 years of age or older.4
INTRACRANIAL EXTENSION OF ORBITAL ABSCESS
Sinus infections appear to be a more common cause of intracranial abscess, the most common being frontal sinus, followed by ethmoid and maxillary sinuses. In the preantibiotic era, Birch–Hirschfeld, reported that 19% of the patients died among the 275 cases of orbital cellulitis studies from 1907–1930 due to the intracranial complications.6 Hartstein et al.39 reported case-records of three patients who were found to have pansinusitis progressing to subperiosteal abscess of the orbit and subsequent intracranial abscess. All three patients were treated with intravenous antibiotics and surgical drainage of the orbital abscess and sinuses. Two of the three patients required drainage of the intracranial abscess. Maniglia et al.4 reported 19 cases of intracranial abscess secondary to mid-face infection, anaerobic organisms being the predominant cause of abscess. These intracranial complications were secondary to nasal, sinus and orbital disease, cavernous sinus thrombosis occurred in only one patient. Frontal lobe, epidural and subdural abscesses were more common. Handler et al.40 recommend surgical drainage for those with a deterioration of ocular motility and vision. Ethmoid sinusitis was an overwhelming predisposing cause in their study and intracranial spread occurred in 6 of 65 patients with orbital cellulitis.
The superior ophthalmic vein drains into the cavernous sinus, the inferior ophthalmic vein, however, may drain either into the cavernous sinus through the superior orbital fissure or into the pterygoid plexus through the inferior orbital fissure.13 Valveless veins interconnect the orbit with sinuses, eyelids and cavernous sinus. Although rare, intracranial abscess is a life-threatening complication of orbital abscess that may require aggressive intervention by a multidisciplinary team [Figure 5]. Fatal complications of intracranial abscess may result from cavernous sinus thrombosis and intracranial rupture of the abscess. Patient with intracranial abscess may be asymptomatic or present with nausea, vomiting, seizures and change in mental status. Neurological signs of intracranial abscess may include fever or altered mental status [Figure 2]. In the past, intracranial abscess formation had a poor prognosis with a significant mortality rate. The classic neurological presentation of intracranial abscess seen in adults is often subtle. These symptoms can be minimal or absent in children.
Figure 5.
External photograph of a 21-year-old female who was diagnosed with right-sided orbital abscess which did not undergo drainage. Chronically untreated orbital abscess resulted in erosion of her orbital wall and intracranial extension
Cavernous sinus thrombosis represents the most severe form of postseptal cellulitis. Cavernous sinus thrombosis is suspected clinically by bilateral disease with ophthalmoplegia and loss of vision.41,42 Imaging studies are indicated when neurologic signs are present, to rule out associated epidural or subdural empyema, brain abscess, or cavernous sinus thrombosis.43–45 MRI with fat suppression can be useful for visualizing the intracranial component in suspected cases. Follow-up imaging studies may be indicated based on the clinical examination. Successful management may include a multidisciplinary team including an oculoplastics surgeon, otolaryntologists, neurosurgeon, and infectious disease expert.
Most intracranial suppurative complications of sinusitis are polymicrobial, with anaerobes, being the most common pathogens.39–42,46 No specific species or combination of organisms are predominant; however, Streptococcus, Staphylococcus, Bacteriodes, and Fusobacterium species are frequently encountered. Initial treatment of such patients includes broad-spectrum antibiotics including beta-lactamase resistant antibiotics with good anaerobic coverage and good CNS penetration because of mixed nature of these infections.16,18,39
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chaudhry IA, Shamsi FA, Elzaridi E, Al-Rashed W, Al-Amri A, Al-Anezi F, et al. Outcome of treated orbital cellulitis in a tertiary eye care center in the middle East. Ophthalmology. 2007;114:345–54. doi: 10.1016/j.ophtha.2006.07.059. [DOI] [PubMed] [Google Scholar]
- 2.Chaudhry IA, Shamsi FA, Elzaridi E, Al-Rashed W, Al-Amri A, Arat YO. Inpatient preseptal cellulitis: experience from a tertiary eye care centre. Br J Ophthalmol. 2008;92:1337–41. doi: 10.1136/bjo.2007.128975. [DOI] [PubMed] [Google Scholar]
- 3.Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80:1414–28. doi: 10.1288/00005537-197009000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Maniglia AJ, Goodwin WJ, Arnold JE, Ganz E. Intracranial abscesses secondary to nasal, sinus, and orbital infections in adults and children. Arch Otolaryngol Head Neck Surg. 1989;115:1424–9. doi: 10.1001/archotol.1989.01860360026011. [DOI] [PubMed] [Google Scholar]
- 5.Ferguson MP, McNab AA. Current treatment and outcome in orbital cellulitis. Aust N Z J Ophthalmol. 1999;27:375–9. doi: 10.1046/j.1440-1606.1999.00242.x. [DOI] [PubMed] [Google Scholar]
- 6.Duke-Elder S, MacFaul PA. The ocular adnexa: part 2. Lacrimal orbital and para orbital diseases. In: Duke-Elder S, editor. System of Ophthalmology. London: Henry Kimpton; 1974. pp. 859–89. [Google Scholar]
- 7.Connel B, Kamal Z, McNab AA. Fulminant orbital cellulits with complete loss of vision. Clin Exp Ophthalmol. 2001;29:260–1. doi: 10.1046/j.1442-9071.2001.00421.x. [DOI] [PubMed] [Google Scholar]
- 8.Jarrett WH, Gutman FA. Ocular complications of infection in the paranasal sinuses. Arch Ophthalmol. 1969;81:683–8. doi: 10.1001/archopht.1969.00990010685013. [DOI] [PubMed] [Google Scholar]
- 9.Chaudhry IA, Shamsi FA, Morales J. Orbital cellulitis following implantation of aqueous drainage devices for glaucoma. Eur J Ophthalmol. 2007;17:136–40. doi: 10.1177/112067210701700122. [DOI] [PubMed] [Google Scholar]
- 10.Fezza J, Chaudhry IA, Kwon YH, Grannum E, Sinard J, Wolfley DE. Orbital melanoma presenting as orbital cellulities: A clinicopathologic report. Ophthal Plastic Reconstr Surg. 1998;14:286–9. doi: 10.1097/00002341-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Chaudhry IA. Herpes Zoster Presenting with Orbital Cellulitis, Proptosis, and Ophthalmoplegia. Middle East J Ophthalmol. 2006;13:167–9. [Google Scholar]
- 12.Krouschnabel EF. Orbital apex syndrome due to sinus infection. Laryngoscope. 1974;84:353–71. doi: 10.1288/00005537-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Hornblass A, Herschorn BJ, Stern K, Grimes C. Orbital abscess. Surv Ophthalmol. 1984;29:169–78. doi: 10.1016/0039-6257(84)90202-9. [DOI] [PubMed] [Google Scholar]
- 14.Morgan PR, Morrison WV. Complications of frontal and ethmoid sinusitis. Laryngoscope. 1980;90:661–6. doi: 10.1288/00005537-198004000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Fearon B, Edmonds B, Bird R. Orbital-facial complication of sinusitis in children. Laryngoscope. 1979;86:947–53. doi: 10.1288/00005537-197906000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Harris GJ. Subperiosteal abscess of the orbit: age as a factor in the bacteriology and response to treatment. Ophthalmology. 1994;101:585–95. doi: 10.1016/s0161-6420(94)31297-8. [DOI] [PubMed] [Google Scholar]
- 17.Harris GJ. Subperiosteal abscess of the orbit: computed tomography and the clinical course. Ophthal Plast Reconstr Surg. 1996;12:1–8. doi: 10.1097/00002341-199603000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Garcia GJ, Harris GJ. Criteria from nonsurgical management of subperiosteal abscess of the orbit: analysis of outcomes 1988-1998. Ophthalmology. 2000;107:1454–8. doi: 10.1016/s0161-6420(00)00242-6. [DOI] [PubMed] [Google Scholar]
- 19.Harris GJ. Subperiosteal abscess of the orbit: older children and adults require aggressive treatment: Editorial. Ophthal Plast Reconstr Surg. 2001;17:395–7. doi: 10.1097/00002341-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Schramm VL, Myres EN, Kennerdell JS. Orbital complications of acute sinusitis: Evaluation, management and outcome. ORL Digest. 1979;86:221–30. doi: 10.1177/019459987808600209. [DOI] [PubMed] [Google Scholar]
- 21.Patt BS, Manning SC. Blindness resulting from orbital complications of sinusitis. Otolaryngol Head Neck Surg. 1991;104:789–95. doi: 10.1177/019459989110400604. [DOI] [PubMed] [Google Scholar]
- 22.Gellady AM, Shulman ST, Ayoub EM. Periorbital and orbital cellulitis in Children. Pediatrics. 1978;61:272–7. [PubMed] [Google Scholar]
- 23.Watters EC, Waller PH. Acute orbital cellulitis. Arch Ophthalmol. 1976;94:785. doi: 10.1001/archopht.1976.03910030387007. [DOI] [PubMed] [Google Scholar]
- 24.Weiss A, Friendly D, Eglin K. Bacterial periorbital and orbital cellulitis in childhood. Ophthalmology. 1983;90:195–204. doi: 10.1016/s0161-6420(83)34573-5. [DOI] [PubMed] [Google Scholar]
- 25.Welsh LW, Welsh JJ. Orbital complications of sinus disease. Laryngoscope. 1974;84:848–56. doi: 10.1288/00005537-197405000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Giletto JB, Scherr SA, Mikaelian DO. Orbital complications of acute sinusitis in children. Trans Pa Acad Ophthalmol Otolaryngol. 1980;34:60. [PubMed] [Google Scholar]
- 27.Smith AT, Spencer JT. Orbital complications resulting from lesions of sinuses. Ann Otol Rhinol Laryngol. 1948;57:5. doi: 10.1177/000348944805700101. [DOI] [PubMed] [Google Scholar]
- 28.Langham-Brown JJ, Rhys-Williams S. Computed tomography of acute orbital infection: the importance of coronal sections. Clin Radiol. 1989;40:471–4. doi: 10.1016/s0009-9260(89)80247-8. [DOI] [PubMed] [Google Scholar]
- 29.Hilal SK. Computed tomography of the orbit. Ophthalmology. 1979;86:864. doi: 10.1016/s0161-6420(79)35434-3. [DOI] [PubMed] [Google Scholar]
- 30.Donahue SP, Schwartz G. Preseptal and orbital cellulitis in childhood: A changing microbiologic spectrum. Ophthalmology. 1998;105:585–95. doi: 10.1016/S0161-6420(98)91038-7. [DOI] [PubMed] [Google Scholar]
- 31.Ingraham HJ, Ryan ME, Burns JT. Streptococcal preseptal cellulitis complicated by the toxic streptococcus syndrome. Ophthalmology. 1994;102:1223–6. doi: 10.1016/s0161-6420(95)30886-x. [DOI] [PubMed] [Google Scholar]
- 32.Shayegani A, MacFarlane D, Kazim M. Streptococcal gangrene of the eyelids and orbit. Am J Ophthalmol. 1995;120:784–92. doi: 10.1016/s0002-9394(14)72732-1. [DOI] [PubMed] [Google Scholar]
- 33.Marshall DH, Jordan DR, Gilberg SM. Periocular necrotizing fasciitis: a review of five cases. Ophthalmology. 1996;104:1857–62. doi: 10.1016/s0161-6420(97)30016-5. [DOI] [PubMed] [Google Scholar]
- 34.Meyer MA. Streptococcal toxic shock syndrome complicating preseptal cellulitis. Am J Ophthalmol. 1996;123:841–3. doi: 10.1016/s0002-9394(14)71138-9. [DOI] [PubMed] [Google Scholar]
- 35.Bhargava D, Saukhla D, Ganesan A, Chand P. Endoscopic sinus surgery for orbital subperiosteal abscess secondaryto sinusitis. Rhinology. 2001;39:151–5. [PubMed] [Google Scholar]
- 36.Slavin ML, Glaser J. Acute severe irreversible visual loss with sphenoethmoiditis - ‘posterior’ orbital cellulitis. Arch Ophthalmol. 1987;105:345–8. doi: 10.1001/archopht.1987.01060030065027. [DOI] [PubMed] [Google Scholar]
- 37.El-Sayed Y, Al-Muhaimeid H. Acute visual loss in association with sinusitis. J Laryngol Otol. 1993;107:840–2. doi: 10.1017/s0022215100124582. [DOI] [PubMed] [Google Scholar]
- 38.Borruat FX, Bogousslavasky J, Uffer S, Klainguti G, Schatz NJ. Orbital infarction syndrome. Ophthalmology. 1993;100:562–8. doi: 10.1016/s0161-6420(93)31606-4. [DOI] [PubMed] [Google Scholar]
- 39.Hartstein ME, Steinvurzel MD, Choen CP. Intracranial abscess as a complication of subperiosteal abscess of the orbit. Ophthal Plast Reconstr Surg. 2001;17:398–403. doi: 10.1097/00002341-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Handler LC, Davey IC, Hill JC, Lauryssen C. The acute orbit: differentiation of orbital cellulitis from subperiosteal abscess by computerized tomography. Neuroradiology. 1991;33:15–8. doi: 10.1007/BF00593326. [DOI] [PubMed] [Google Scholar]
- 41.Giannoni CM, Stewart MG, Alford EL. Intracranial complications of sinusitis. Laryngoscope. 1997;107:863–7. doi: 10.1097/00005537-199707000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Brook I. Bacteriology of intracranial abscess in children. J Neurosurg. 1981;54:484–8. doi: 10.3171/jns.1981.54.4.0484. [DOI] [PubMed] [Google Scholar]
- 43.Weber AL, Mikuli D. Inflammatory disorders of the periorbital sinuses and their complications. Radiol Clin North Am. 1987;25:615–30. [PubMed] [Google Scholar]
- 44.Towbin R, Han B, Kaufmann R, Burke M. Postseptal cellulitis: CT in diagnosis and management. Radiology. 1986;158:735–7. doi: 10.1148/radiology.158.3.3945747. [DOI] [PubMed] [Google Scholar]
- 45.Harr DL, Quencer RM, Abrams GW. Computed tomography and ultrasound in the evaluation of orbital infection and pseudotumor. Radiology. 1982;152:395. doi: 10.1148/radiology.142.2.7054828. [DOI] [PubMed] [Google Scholar]
- 46.Brook I, Frazier EH. Microbiology of subperiosteal orbital abscess and associated maxillary sinusitis. Laryngoscope. 1996;106:1010–3. doi: 10.1097/00005537-199608000-00019. [DOI] [PubMed] [Google Scholar]