Abstract
Context:
Juxtafacet cysts of the lumbar spine are extradural degenerative lesions associated with symptoms of lower back pain and radiculopathy. Surgical treatment is indicated when there is failure of conservative measures. Primary spinal fusion at the time of surgical excision of the cyst is a matter of controversy. Few reports have described long-term follow-up for surgical treatment of spinal cysts.
Aim:
The purpose of this study is to assess the long-term outcome of the surgical excision of a Juxtafacet cyst without spinal fusion.
Study Design:
This is a retrospective case series study, level IV evidence.
Materials and Methods:
This is a retrospective case series study on 13 patients with Juxtafacet cysts, who were treated with surgical excision of the cysts without spinal fusion. A questionnaire scoring system was used for evaluation of the surgical outcome.
Results:
The study was conducted on 13 patients, seven females (54%) and six males (46%), their age ranging from 38 to 69 years, with a mean age of 52 (±9.93 STD) years. The mean duration of the symptoms was 10.5 (±6.22 STD) months. All patients got benefit from surgery, with six excellent (46%), six good (46%), and one fair outcome (8%), with no surgery-related complications. The mean follow-up period of the patients at the time of this study was 4.2 years (±1.43 STD).
Conclusion:
Long-term follow-up for surgical excision of symptomatic Juxtafacet cysts without spinal fusion revealed excellent to good results in 92% of the patients, with a satisfaction rate of 80% (±8.41 STD).
Keywords: Facet joint, ganglion cyst, Juxtafacet cyst, radiculopathy, synovial cyst
Introduction
The first description of a spinal synovial cyst was reported by Ayberk G,[1] in a postmortem examination. In 1950, Vossschulte and Borger[2] reported the first case of spinal synovial cyst causing root compression. The term Juxtafacet cyst ( JFC) was originated by Kao et al.,[3] to include both synovial cysts and ganglion cysts adjacent to a spinal facet joint or arising from the ligamentum flavum. Distinction between these two types of cysts could be difficult and was clinically unimportant.[4–6]
The etiology of JFC is unknown; possibilities include synovial fluid extrusion from the joint capsule, latent growth of a developmental rest, myxoid degeneration, and cyst formation in the connective tissue. Increased motion seems to have a role in many cysts, and the role of trauma is debated, but it probably plays a role in a small number of cases.[7]
These lesions occur most frequently in the lumbar spine (88-99%), up to 8% occur in the thoracic region, and 1 to 4% in the cervical region.[8] Juxtafacet cysts of the lumbar spine are extradural degenerative lesions associated with symptoms of lower back pain and radiculopathy, and may sometimes be mistaken for free fragments of herniated lumbar disc or other epidural mass.[9] Magnetic resonance imaging is the investigation of choice.[10] Optimal treatment is a matter of controversy.[11] If symptoms persist with conservative treatment, some authors recommend cyst aspiration or facet injection with steroids, while most surgeons prefer surgical excision of the cyst.[12] A JFC may indicate possible instability, which must be evaluated. Some recommend primary spinal fusion in conjunction with surgical excision of the JFC. However, it appears that in many cases fusion is not required for a good result.[12] Few reports have described the long-term follow-up of the surgical excision of JFC. In this cases series study, we describe the long-term outcome of the surgical excision of JFC without primary spinal fusion.
Materials and Methods
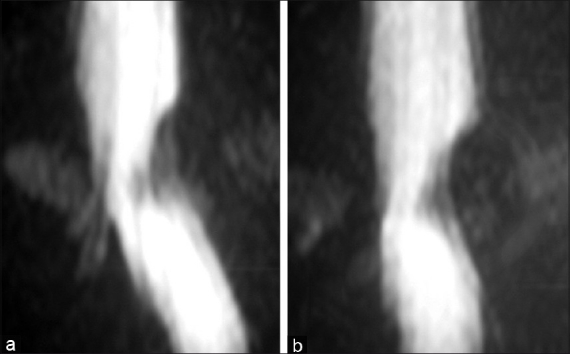
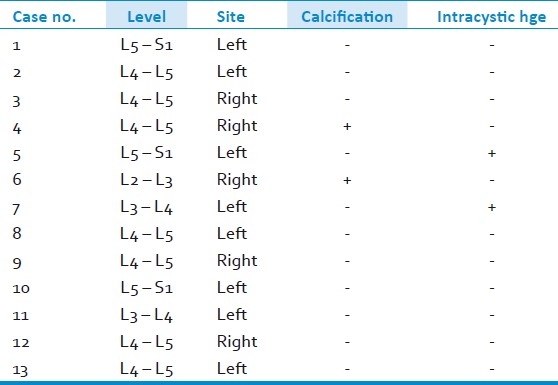
This is a retrospective case series study on 13 patients with a Juxtafacet cysts, who were treated with surgical excision, for the period from December 2003 to December 2008. Careful history taking and a thorough clinical examination were performed for all patients. The patients’ symptoms and physical signs are listed in Table 1.
Table 1.
The presenting symptoms and physical signs in the patient population
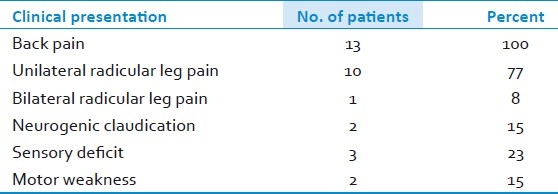
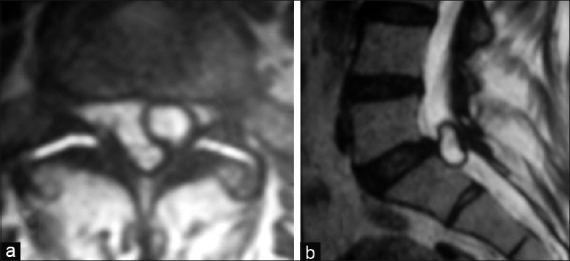
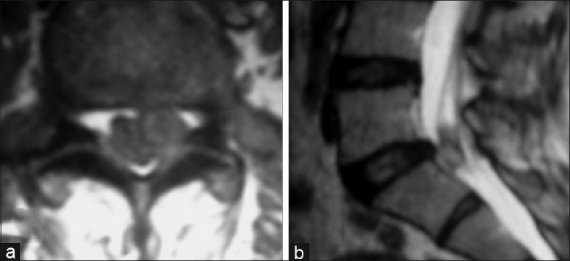
All the patients had dynamic flexion/extension X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) before surgery. Diagnosis of a Juxtafacet cyst was done based on the correlation of the MRI findings with the clinical findings. In T2-weighted images, Juxtafacet cysts showed a typical pattern consisting of a hyperintense center and hypointense rim [Figure 1]. In two cases there were inhomogeneous/isointense centers, because of subacute hemorrhage in the cyst [Figure 2]. In the MRI myelography the lesion appeared as a round extradural posterolateral filling defect [Figure 3].
Figure 1.
T2WI MRI axial (a) and sagittal (b) cuts show a lumbar Juxtafacet cyst typically with a hyperintense center and a hypointense rim
Figure 2.
T2WI MRI axial (a) and sagittal (b) cuts show a lumbar Juxtafacet cyst with an inhomogeneous/isointense center because of subacute hemorrhage in the cyst
Figure 3.
MRI myelography lateral (a) and A-P (b) views show a posterolateral filling defect, with a round extradural appearance in case of a juxtafacet cyst
Surgical technique
Under general anesthesia, the patient lay in the prone position. All patients underwent identical procedures, which involved muscle separation, laminectomy (10 patients had partial hemilaminectomy and three patients had bilateral decompressive laminectomies), flavectomy, and piecemeal excision of the cyst. The cyst was found to compress the dura and/or the nerve root in all cases. None of the cases had spinal fusion after excision of the cyst. Closure was done with a submascular drain.
Follow-up of the patients was done at regular intervals, for two years. The surgical outcome was evaluated according to a questionnaire scoring system [Table 2].[13]
Table 2.
The questionnaire scoring system
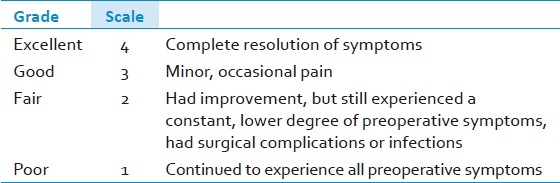
The questionnaire was repeated at the time of this study and a retrospective measurement of the patients’ satisfaction with the procedure was done at the time of this study via telephone interviews with them. The patients were asked to rate their satisfaction with the procedure (0% totally unsatisfied, 100% totally satisfied).
Results
The study was conducted on 13 patients, seven females (54%) and six males (46%) ranging in age from 38 to 69 years with a mean age of 52 (±9.93 STD) years. The mean duration of the symptoms was 10.5 (±6.22 STD) months (range 2 – 24 months).
With regard to the level of facet cysts, seven patients (54%) had the cyst at the level of L4–L5, three patients (23%) at L5–S1, two patients (15%) at L3–L4, and one patient (8%) at L2–L3. The cysts were arising from the left side in eight cases (62%) and from the right side in five cases (38%). The other radiological findings are listed in Table 3.
Table 3.
The preoperative radiological findings
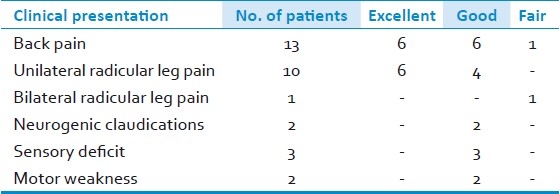
The mean duration of hospitalization was three (±1.09 STD) days (range 2-5 days). Surgery-related complications were not present. All patients got benefit from the surgery, with six excellent (46%), six good (46%), and one fair outcome (8%). Patients presented with motor and/or sensory deficits, had complete resolution of their neurological deficits although they still had minor, occasional pain [Table 4]. After surgery there was no case of a recurrent cyst during the follow-up period. However, subsequent fusion was required in only one patient who developed symptomatic spondylolisthesis two years after surgery (the patient was with fair outcome). The mean follow-up period of patients at the time of this study was 4.2 years (±1.43 STD). The mean satisfaction rate of patients with the procedure was 80% (±8.41 STD).
Table 4.
The postoperative outcome in relation to the presenting symptom
Discussion
At the end of the last decade several publications on lumbar Juxtafacet cysts have led to reconsideration of its incidence in lumbar spine degenerative diseases. Doyle and Merrilees reported a retrospective MRI study of 303 patients with symptomatic (low-back pain or radiculopathy) degenerative lumbar spine disease and found a synovial cyst in almost 10% of the cases.[14]
Cysts may be asymptomatic and found incidentally. Most of the symptomatic patients present with radicular pain and neurologic deficits. A history of low back pain invariably precedes the radicular pain. In addition, clinical syndromes such as caudaequina, lateral recess, and spinal stenosis syndromes have been described.[15–17]
In our series, all patients had back pain (100%), while ten also experienced unilateral radicular leg pain (77%), and one had bilateral leg pain (8%). Two patients had neurogenic claudication (15%). However, sensory loss in three patients (23%) and motor weakness in two patients (15%) were also presenting symptoms. Our findings were consistent with reports found in other surgically treated cases in the literature.[5]
MRI is the tool of choice for diagnosis of Juxtafacet cysts.[13] The majority of the cysts in this study have occurred at the L4–L5 level (54%), which corresponds with the data from other studies. The predilection for cysts to occur adjacent to this facet joint level has been attributed to the amount of degenerative spondylosis and spinal instability (the site of maximum instability).[13,18,19] No radiological evidence of instability had been observed in any of our patients preoperatively.
These cysts can, on rare occasions, hemorrhage and bleed into the surrounding soft tissues and/or the spinal canal, causing acute compression of the nerve root.[17,18] Intracystic hemorrhage can be predicted radiologically by an MRI (inhomogeneous center In T2-weighted images and irregular hyperintensity in T1-weighted images).[10] In our study intracystic hemorrhage was demonstrated in two patients (15%). This finding did not, however, correlate with the acute onset of symptoms.
Although relevant reports in the international literature are increasing, the controversy about conservative versus surgical treatment and the need for concomitant fusion still exists. The optimal treatment is not known. There is one case report of a cyst that resolved spontaneously.[11] Conservative treatment has been proposed by certain authors, including bed rest, medications, and orthopedic corsets, but with disappointing results and are not reported to be efficacious.[20,21]
Steroid injection was described as an alternative procedure for management of intraspinal Juxtafacet cysts. There is little information available on the efficacy and outcome with treatment of lumbar facet joint synovial cysts by percutaneous, fluoroscopic, facet joint steroid injections, with cyst distention and rupture. However, these treatments often show short-term improvement or no improvement at all. Also complications such as dural puncture, spinal nerve injury, bleeding, and infection have been reported.[20,22–24]
Surgical treatment is largely recommended in all cases of intractable pain or neurologic deficit.[7,16,18–20] The current therapy for Juxtafacet cysts includes excision of the mass and lumbar decompression. In our series, all patients underwent laminectomy and resection of the cyst, 10 patients had partial hemilaminectomy, and three patients had bilateral decompressive laminectomies, one of them presented with bilateral radiculopathy and the other two presented with neurogenic claudication.
Many authors reported that no difference in surgical outcome was found between patients having fusion and those who did not have it.[25,26] While others concluded that, a concomitant fusion procedure may be performed in selected cases.[9,18]
Métellus et al.[9] has concluded that there is no reliable criterion that allows the development of a symptomatic spinal instability to be predicted in patients with preoperative spondylolisthesis, and therefore, fusion as a first line procedure is still debatable. Others have mentioned an association between spinal cysts and spondylolisthesis/instability and better surgical outcomes in patients having fusion than in those who did not have it.[13,26–28]
In our series no radiological evidence of instability was observed in any patient preoperatively. Concomitant fusion was not performed in any of the patients. However, subsequent fusion was required in only one patient, who developed symptomatic spondylolisthesis two years after surgery.
Our study presents a long-term follow-up (4.2 years±1.43 STD) for surgical excision of Juxtafacet cysts, without concomitant spinal fusion. We reported excellent to good results in 92% of the patients with a satisfaction rate of 80%. The main limitation of our study was the limited number of cases, which did not allow assessment of the statistical significance of the surgical outcome. However this is due to the low incidence of cases with low back pain or lumbar radicular pain attributed to isolated juxtfacet cyst without other pathology.
Conclusion
Long-term follow-up for surgical excision of a symptomatic Juxtafacet cyst without spinal fusion revealed excellent-to-good results in 92% of the patients, with a satisfaction rate of 80%.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ayberk G, Özveren F, Gök B, Yazgan A, Tosun H, Seçkin Z, et al. Lumbar synovial cysts: Experience with nine cases. Neurol Med Chir (Tokyo) 2008;48:298–303. doi: 10.2176/nmc.48.298. [DOI] [PubMed] [Google Scholar]
- 2.Vossschulte K, Börger G. Anatomic and functional studies of intervertebral disk hernia. Langenbecks Arch Klin ChirVer Dtsch Z Chir. 1950;265:329–55. [PubMed] [Google Scholar]
- 3.Kao CC, Winkler SS, Turner JH. Synovial cyst of spinal facet.Case report. J Neurosurg. 1974;41:372–6. doi: 10.3171/jns.1974.41.3.0372. [DOI] [PubMed] [Google Scholar]
- 4.Freidberg SR, Fellows T, Thomas CB, Mancall AC. Experience with symptomatic epidural cysts. Neurosurgery. 1994;34:989–93. doi: 10.1227/00006123-199406000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Howington JU, Connolly ES, Voorhies RM. Intraspinal synovial cysts: 10-year experience at the Ochsner Clinic. J Neurosurg. 1999;91(2 Suppl):193–9. doi: 10.3171/spi.1999.91.2.0193. [DOI] [PubMed] [Google Scholar]
- 6.Onofrio BM, Mih AD. Synovial cysts of the spine. Neurosurgery. 1988;22:642–7. doi: 10.1227/00006123-198804000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Sabo RA, Tracy PT, Weinger JM. A series of 60 juxtafacet cysts: Clinical presentation, the role of spinal instability, and treatment. J Neurosurg. 1996;85:560–5. doi: 10.3171/jns.1996.85.4.0560. [DOI] [PubMed] [Google Scholar]
- 8.Choudhri HF, Perling LH. Diagnosis and management of juxtafacet cysts. Neurosurg Focus. 2006;20:E1. doi: 10.3171/foc.2006.20.3.2. [DOI] [PubMed] [Google Scholar]
- 9.Métellus P, Fuentes S, Adetchessi T, Levrier O, Flores-Parra I, Talianu D, et al. Retrospective study of 77 patients harbouring lumbar synovial cysts: Functional and neurological outcome. ActaNeurochir(Wein) 2006;148:47–54. doi: 10.1007/s00701-005-0650-z. [DOI] [PubMed] [Google Scholar]
- 10.Schmid G, Willburger R, Jergas M, Pennekamp W, Bickert U, Köster O. Lumbar intraspinaljuxtafacet cysts. MR imaging and CT-arthrography. Rofo. 2002;174:1247–52. doi: 10.1055/s-2002-34561. [DOI] [PubMed] [Google Scholar]
- 11.Mercader J, Gomez J, CardenalC Intraspinal synovial cyst: Diagnosis by CT.Follow up and spontaneous remission. Neuroradiology. 1985;27:346–8. doi: 10.1007/BF00339570. [DOI] [PubMed] [Google Scholar]
- 12.Kurz LT, Garfin SR, Unger AS, Thorne R, Rothman RH. Intraspinal synovial cyst causing sciatica. J Bone Joint Surg Am. 1985;67:865–71. [PubMed] [Google Scholar]
- 13.Khan AM, Synnot K, Cammisa FP, Girardi FP. Lumbar synovial cysts of the spine: An evaluation of surgical outcome. J Spinal Disord Tech. 2005;18:127–31. doi: 10.1097/01.bsd.0000156830.68431.70. [DOI] [PubMed] [Google Scholar]
- 14.Doyle AJ, Merrilees M. Synovial cysts of the lumbar facet joints in a symptomatic population: Prevalence on magnetic resonance imaging. Spine (Phila Pa 1976) 2004;29:874–8. doi: 10.1097/00007632-200404150-00010. [DOI] [PubMed] [Google Scholar]
- 15.Fardon DF, Simmons JD. Gas-filled intraspinal synovial cyst. A case report. Spine (Phila Pa 1976) 1989;14:127–9. doi: 10.1097/00007632-198901000-00029. [DOI] [PubMed] [Google Scholar]
- 16.Hemminghytt S, Daniels DL, Williams AL, Haughton VM. Intraspinal synovial cysts: Natural history and diagnosis by CT. Radiology. 1982;145:375–6. doi: 10.1148/radiology.145.2.7134440. [DOI] [PubMed] [Google Scholar]
- 17.Tatter SB, Cosgrove GR. Hemorrhage into a lumbar synovial cyst causing an acute caudaequina syndrome.Case report. J Neurosurg. 1994;81:449–52. doi: 10.3171/jns.1994.81.3.0449. [DOI] [PubMed] [Google Scholar]
- 18.Lyons MK, Atkinson JL, Wharen RE, Deen HG, Zimmerman RS, Lemens SM. Surgical evaluation and management of lumbar synovial cysts: The Mayo Clinic experience. J Neurosurg. 2000;93(1 Suppl):53–7. doi: 10.3171/spi.2000.93.1.0053. [DOI] [PubMed] [Google Scholar]
- 19.Yarde WL, Arnold PM, Kepes JJ, O’Boynick PL, Wilkinson SB, Batnitzky S. Synovial cysts of the lumbar spine: Diagnosis, surgical management, and pathogenesis. Report of eight cases. SurgNeurol. 1995;43:459–64. doi: 10.1016/0090-3019(95)80090-4. [DOI] [PubMed] [Google Scholar]
- 20.Hsu KY, Zucherman JF, Shea WJ, Jeffrey RA. Lumbar intraspinal synovial and ganglion cysts (facet cysts).Ten-year experience in evaluation and treatment. Spine (Phila Pa 1976) 1995;20:80–9. doi: 10.1097/00007632-199501000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Shah RV, Lutz GE. Lumbar intraspinal synovial cysts: Conservative management and review of the world's literature. Spine J. 2003;3:479–88. doi: 10.1016/s1529-9430(03)00148-7. [DOI] [PubMed] [Google Scholar]
- 22.Allen TL, Tatli Y, Lutz GE. Fluoroscopic percutaneous lumbar zygapophyseal joint cyst rupture: A clinical outcome study. Spine J. 2009;9:387–95. doi: 10.1016/j.spinee.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Lim AK, Higgins SJ, Saifuddin A, Lehovsky J. Symptomatic lumbar synovial cyst: Management with direct CT-guided puncture and steroid injection. ClinRadiol. 2001;56:990–3. doi: 10.1053/crad.2001.0710. [DOI] [PubMed] [Google Scholar]
- 24.Martha JF, Swaim B, Wang DA, Kim DH, Hill J, Bode R, et al. Outcome of percutaneous rupture of lumbar synovial cysts: A case series of 101 patients. Spine J. 2009;9:899–904. doi: 10.1016/j.spinee.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 25.Boviatsis EJ, Stavrinou LC, Kouyialis AT, Gavra MM, Stavrinou PC, Themistokleous M, et al. Spinal synovial cysts: Pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J. 2008;17:831–7. doi: 10.1007/s00586-007-0563-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pirotte B, Gabrovsky N, Massager N, Levivier M, David P, Brotchi J. Synovial cysts of the lumbar spine: Surgery-related results and outcome. J Neurosurg. 2003;99(1 Suppl):14–9. doi: 10.3171/spi.2003.99.1.0014. [DOI] [PubMed] [Google Scholar]
- 27.Bydon A, Xu R, Parker SL, McGirt MJ, Bydon M, Gokaslan ZL, et al. Recurrent back and leg pain and cyst reformation after surgical resection of spinal synovial cysts: Systematic review of reported postoperative outcomes. Spine J. 2010;10:820–6. doi: 10.1016/j.spinee.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Tillich M, Trummer M, Lindbichler F, Flaschka G. Symptomatic intraspinal synovial cysts of the lumbar spine: Correlation of MR and surgical findings. Neuroradiology. 2001;43:1070–5. doi: 10.1007/s002340100682. [DOI] [PubMed] [Google Scholar]


