Video abstract
Video
Keywords: pharmacist interventions, adherence to medication, depression, antidepressants, systematic review
Abstract
Background
Pharmacist intervention in improving patient adherence to antidepressants is coupled with better outcomes.
Aims
The aim of this investigation was to systematically examine the published literature to explore different types of pharmacist interventions used for enhancing patient adherence to antidepressant medications. Three specific questions guided the review: what is the impact of pharmacist interventions on adherence to antidepressant medication? What is the impact of pharmacist interventions on patient-reported outcomes and patient satisfactions? What are the types of interventions used by pharmacists to enhance patients’ adherence to antidepressants?
Search strategies
A systematic review of the literature was conducted during August–November 2010 using PubMed, BIOSIS Previews® Web of Science, ScienceDirect, the Cochrane Library, PsycINFO®, IngentaConnect™, Cambridge Journals Online, and Medscape databases. Key text words and medical subject headings included pharmacist intervention, medication intervention, depression, medication adherence, health-related quality of life, patient-reported outcomes, and antidepressants.
Results
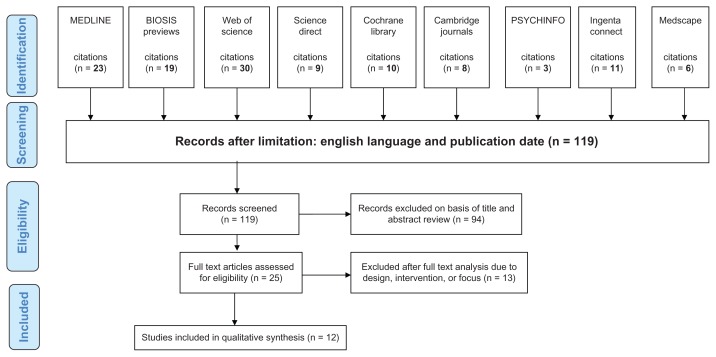
A total of 119 peer-reviewed papers were retrieved; 94 were excluded on the basis of abstract review and 13 after full-text analysis, resulting in twelve studies suitable for inclusion and intensive review. The most common intervention strategy that pharmacists utilized was a combination of patient education and drug monitoring. A cumulative patient adherence improvement in this review ranged from 15% to 27% attributed to utilization of different interventions and different combinations of interventions together with patient satisfaction with the treatment when depression improved.
Conclusion
This review suggests that pharmacist intervention is effective in the improvement of patient adherence to antidepressants. This may be a basis for more studies examining the effectiveness of innovative interventions by pharmacists to enhance patient adherence to antidepressant medications.
Introduction
Depressive illness is a public health issue of major significance. Lifetime prevalence is estimated at about 15% and most depressed patients are treated in general practice.1 Despite the proven efficacy of antidepressant medication, many depressed patients do not receive an adequate dosage and duration of treatment.2 Shortcomings in treatment for depression are frequently noted both in primary care and specialized settings. The effectiveness of antidepressants is also reduced by patients’ non-adherence. Observational studies found discontinuation rates of 28% at 1 month and 44% to 52% at 3 months.3 Non-adherence may result in serious consequences such as treatment failure, relapse, a chronic course of depression, complications, high medical care utilization, increased costs, and impairment in work functioning and other activities.3
The role of pharmacists in the medical field has recently grown well beyond the dispensing function and expanded to clinical trials, health economics, patient education, and other related roles.4 Pharmacist interventions have proved to be beneficial for improving treatment outcomes in a variety of healthcare settings.5 Because of their excellent position of having direct patient contact, pharmacists can help patients to address barriers to adherence which may include, inter alia, concerns about adverse effects, increased duration of therapy, frequency of drug administration, cost-effectiveness, and pill burden; they incorporate interventions into the care of their patients with the use of different strategies such as patient education, drug monitoring, and management of adverse reactions.
Aims
The aim of this investigation was to systematically examine the published literature to explore different types of pharmacist interventions used in order to enhance patients’ adherence to antidepressant medication. Three specific questions guided the review:
What is the impact of pharmacist interventions on adherence to antidepressant medication?
What is the impact of pharmacist interventions on patient-reported outcomes and patient satisfaction?
What are the types of interventions used by pharmacists to enhance patients’ adherence to antidepressants?
Methods
A systematic review of the published literature was conducted to identify all studies that had examined pharmacist interventions to improve adherence to antidepressant medication published from 2000–2010. The reasons for selecting this cutoff period were: most studies focusing on pharmacists’ interventions in patients with depression were conducted during this period; the role of pharmacists began to change and expand from just dispensing and compounding drugs to providing pharmaceutical care in the late 1990s and include reviewing of prescribed drugs, taking part in clinical rounds, becoming an important member of the clinical team, counseling in outpatient and inpatient settings, and others.6–8 These papers were analyzed in line with qualitative review methodology to produce a number of data themes that were later grouped together to produce the dominant categories. In addition, the quality of the studies was assessed using the Jadad scale,9 which is easy to use, contains many of the important elements that have empirically been shown to correlate with bias, has known reliability and external validity, and is most widely used worldwide for such assessments.10 The Jadad scale is a three-item scale that considers three features of a study: randomization, double-blinding, and flow of patients. Adequate description of allocation concealment was also evaluated. Total summed scores ranged from 0 to 7, with the higher scores indicating higher quality.11 However, blinding of pharmacists and participants was not possible because of the type of intervention assessed in this systematic review; therefore, total scores ranged from 0 to 5 (Table 1). Although the Jadad scale is a little out of date, it nonetheless still has all the statistical qualities and practical applications for assessing the quality of current randomized clinical trials.12 In light of the more elaborate scales that are emerging, whether or not the use of the Jadad scale is a weakness or strength of this research is a moot point.12
Table 1.
Quality of studies using the Jadad scale for reporting randomized controlled trials
| Studies | Adequate description of allocation concealment | Flow of patients is described and adequate | Flow of patients is described | Method of blinding is appropriate | Blinding is mentioned | Method of randomization is appropriate | Randomization is mentioned | Total |
|---|---|---|---|---|---|---|---|---|
| Canales13 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 3 |
| Bultman14 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 3 |
| Finley15 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 3 |
| Finley16 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 4 |
| Adler17 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 5 |
| Capoccia18 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 2 |
| Rickles19 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 5 |
| Brook20 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 3 |
| Al-Saffar21 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 4 |
| Crockett22 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 2 |
| Rickles23 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 5 |
| Bosmans24 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 4 |
Information sources and searches
During August to November 2010, the following databases were searched for articles published between 2000 and 2010: PubMed, BIOSIS Previews, Web of Science, ScienceDirect, The Cochrane Library, PsycINFO, IngentaConnect, Cambridge Journals Online, and Medscape databases. A variety of key medical subject headings terms and text words were constructed for use within the databases: pharmacist intervention, medication intervention, depression, medication adherence, compliance, health-related quality of life, and patient-reported outcomes. The key words “pharmacist intervention” were then combined with “medication adherence”, “antidepressant medications”, “depression”, “health quality”, “patient-reported outcomes”, “randomized clinical trials”, “systematic reviews”, and “quality reports” for the purpose of the second round of the computer search.
Notably, “adherence”, “compliance”, and “persistence” have different meanings when used stringently. Adherence to medication is defined as: “the extent to which a person’s behavior, taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health-care provider”.25 The term “adherence” rather than “compliance” is now advocated because compliance implies that the instructions of the health-care provider have to be followed in a passive way and that the patient is not expected to engage in a therapeutic association or any agreement with the healthcare provider.26 On the other hand, persistence is described as continuous refilling of prescriptions in accordance with the suggested duration of the therapy, which is determined by evaluating solely whether or not the patient continues treatment.27 In general, pharmacists’ interventions usually focus on medication; consequently, adherence is the primary outcome in most of these studies. For this particular reason, the two reviewers decided to focus on medication adherence rather than compliance or persistence in this systematic review.
Study selection
The titles and abstracts of all articles were scanned for randomized control studies that had investigated the impact of pharmacists’ intervention on patient adherence to antidepressant medication published from 2000 to 2010. The abstracts and studies were screened then discarded if they did not fit the selection criteria (Table 2). Studies that were identified as potentially relevant were retrieved where possible and further screened for relevance. A total of 119 papers were retrieved, with 94 excluded on the basis of abstract review and 13 after full-text analysis, resulting in the retention of 12 studies suitable for inclusion. The papers were analyzed qualitatively by applying the Jadad scale. The methodology for research that had been adopted in papers included in this review was that of randomized controlled trials. This is because randomized controlled trials are considered to be the optimal study design for minimizing bias and providing the most accurate estimate of complex interventions in terms of benefits; also, it is the only trial design to establish causal effects.28
Table 2.
Summary of studies included in this review, 2000–2010
| Study | Methodology | Study location | Sample size | Brief description of study aims |
|---|---|---|---|---|
| Canales13 | Carried out in two phases. Control and experimental groups | Texas, USA | 93 | To determine the effects of a psychiatric pharmacist on clinical outcomes of acute care psychiatric inpatients. and to monitor hospitalization costs |
| Bultman14 | Systematic, random sample of pharmacies and field study, interviewed patients | Wisconsin, USA | 100 | To examine the effects of pharmacist monitoring on patient satisfaction and adherence to antidepressant medication therapy |
| Finley15 | Pharmacist follow-up of patients for 6 months through a combination of scheduled office visits and telephone calls. Working closely with psychiatric liaisons | California, USA | 220 | To examine efforts to improve patient adherence to antidepressant drug therapy and outcomes |
| Finley16 | A randomized controlled trial comparing the outcomes of subjects treated in care model intervention with subjects receiving usual care | California, USA | 150 | To measure the effects of a collaborative care model that emphasized the role of clinical pharmacists in providing drug therapy management and treatment follow-up to patients with depression |
| Adler17 | A randomized clinical trial of a pharmacist intervention for depressed patients reporting antidepressant use and depression severity outcomes at 6 months | Massachusetts, USA | 533 | To evaluate outcomes of a pharmacist intervention for depressed patients in primary care |
| Capoccia18 | Randomized to enhanced care or usual care for 1 year | Washington, USA | 74 | To evaluate the impact of pharmacist interventions in collaborative care to improve the care of and outcomes for patients with depression, to test the effectiveness of pharmacist interventions in the collaboration model |
| Rickles19 | Randomized, controlled unblended, mixed experimental design | Wisconsin, USA | 63 | To explore the impact of telephonebased education and monitoring by community pharmacists on multiple outcomes of pharmacist–patient collaboration |
| Brook20 | Randomized controlled trial with 6-month follow-up | The Netherlands | 147 | To improve adherence to antidepressant regimens through pharmacist intervention |
| Crockett22 | Parallel-groups design with a control and intervention group | New South Wales, Australia | 106 | Documentation and evaluation of patient outcomes into the role of rural community pharmacists in the management of depression |
| Rickles23 | Randomized controlled, experimental design | Wisconsin, USA | 60 | To determine whether or not telephone follow-up can influence the nature and extent to which antidepressant users provide feedback to pharmacists, whether patient characteristics are associated with the extent of patient feedback, how patient feedback affects subsequent outcomes after controlling for patient characteristics |
| Bosmans24 | An economic evaluation performed alongside a 6-month randomized controlled trial | The Netherlands | 88 | To evaluate the cost-effectiveness of a pharmacy-based intervention to improve adherence to antidepressant therapy in adult patients receiving treatment in primary care |
| Al-Saffar21 | Randomized into a control and two treatment groups. Treatment groups additionally received a patient information leaflet. Adherence was monitored at 2 and 5 months | Kuwait | 270 | To assess the acceptability and effectiveness of two educational initiatives on patterns of antidepressant medication use among depressed Kuwaiti patients |
Inclusion criteria
The considered inclusion criteria were as follows: published in English language; study is primary in nature; published in a peer-reviewed journal; full-text articles and publication dates match the years lying between 2000 to 2010; study design a randomized control study; recruited to investigate depressed adult patients, and the main outcome finding adherence to antidepressant medications.
Exclusion criteria
Studies without control groups or randomization, descriptive studies, pilot studies, results of postal surveys, and qualitative interviews were excluded from this review. Non-English papers were also discarded to prevent cultural and linguistic bias in translation. Studies were also excluded if the pharmacist was not involved in the intervention or service provided to patients. In addition, papers were excluded if no participants in the sample were diagnosed with depression. Other exclusion criteria were depressed adolescent patients, editorials, book chapters and duplicate articles, and systematic reviews, and if the focus of the study was not on adherence. Each study meeting the inclusion and exclusion criteria was sorted on the basis of the pharmacist intervention, sample size, follow-up, outcome measures, findings, country of origin, setting, and number of involved pharmacists.
Data abstraction
A grid was created to record the summaries of the articles for further conceptualization of the literature and later construction of the literature review. PICOS (participants, interventions, comparisons, outcomes, and study design) was used for data extraction. This initial tabulation presented information about the study characteristics, including the year of the study, the number of participants, type of intervention, comparison, country, research design, outcomes, and a brief description of study aims. For the main analysis, data from the findings of these original studies were summarized into a model to display the themes that presented the type of pharmacist intervention, patients’ outcome measures, and change in adherence rate. Data from each study were extracted and checked independently by the two reviewers. Any point of inconsistency was discussed between the two investigators in order to reach 100% agreement regarding data abstracted from the selected studies.
Results
The search yielded 119 citations. Of these, 94 studies were excluded after review of the title and abstract (Figure 1). Of the remaining 25 studies, 13 studies were excluded because they did not meet the inclusion criteria for method design, or the intervention was conducted by non pharmacists, or focused on other patient groups. Twelve studies met the criteria for inclusion in this review and were, therefore, selected for analysis. This section summarizes the results of the 12 core studies, which investigated pharmacists’ intervention to enhance patients’ adherence to antidepressant medication and related patient outcomes. A summary of findings from these peer-reviewed papers is shown in Tables 2–6. The 12 included studies published between 2000 and 2010 were carried out in the USA, Canada, the Netherlands, Australia, and Kuwait.
Figure 1.
Results of search strategy and identification of publications included in the review.
Table 6.
Summary of pharmacies contact and intervention
| Study | Total number of contact | Direct contact | Indirect contact | Total number of pharmacist intervention | Type of pharmacist intervention | Study participants | Sample size | Follow up | Rate of adherence | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Control/intervention | ||||||||||||||
| Canales13 | 4 | 4 | 0 | 3 | PE | M | DP | 2 | 93 | 7 months | −7% | 27% | ||
| −7% | 22% | |||||||||||||
| Bultman14 | 2 | 2 | 0 | 1 | PE | 23 | 100 | 2 months | 87% | 63% | ||||
| Finley15 | 8 | 3 | 5 | 3 | PE | DP | PC | 2 | 220 | 6 months | 66% | 81% | ||
| Finley16 | 6 | 1 | 5 | 4 | PE | M | DP | PC | 2 | 150 | 6 months | 48% | 67% | |
| Adler17 | 14 | 9 | 5 | 2 | PE | M | 5 | 533 | 12 months | 48.9% | 60.6% | |||
| Capoccia18 | 4 | 2 | 2 | 4 | PE | M | DP | PC | 2 | 74 | 12 months | 57% | 59% | |
| Rickles19 | 4 | 1 | 3 | 3 | PE | M | PC | 14 | 63 | 3 months | 51% | 70% | ||
| Brook20 | 4 | 1 | 3 | 3 | PE | PC | THV | 19 | 147 | 6 months | 73% | 90% | ||
| Al-Saffar21 | 4 | 3 | 1 | 1 | PE | 7 | 270 | 7 months | 10% 10% |
39% 43% |
||||
| Crockett22 | 3 | 1 | 2 | 1 | PE | 32 | 106 | 2 months | 96% | 95% | ||||
| Rickles23 | 4 | 1 | 3 | 2 | PE | PC | 14 | 60 | 3 months | 51% | 70% | |||
| Bosmans24 | 3 | 3 | 0 | 2 | PE | THV | 19 | 88 | 6 months | 86% | 88% | |||
Abbreviations: PE, patients education; M, drug monitoring; DP, drug prescriptions; PC, phone call; THV, take home video.
Quality of included studies
Twelve studies met the criteria for inclusion in this review and were therefore selected for analysis (Table 2). No systematic reviews were identified. All investigations were presented as original research papers published in peer-reviewed indexed journals. While only one study investigated the impact of pharmacist intervention in inpatient sites, the remaining investigations were conducted in either community pharmacies or primary care pharmacy settings.
All studies involved patients with depression and pharmacist interventions. In toto, 1904 patients and 136 pharmacists participated in the selected studies, which had short follow-up; only two studies continued up to 12 months.17,18 Moreover, in all of these trials neither patients nor pharmacists were blinded, which led to a decrease in the quality of studies, ie, a score less than 5 in terms of the Jadad scale.
The majority of the studies involved fewer than seven pharmacists, and four papers described interventions by just two pharmacists.13,15,18,29 Although involving small numbers of pharmacists may make for good internal consistency, the results obtained may not be generalizable to the outcomes of services provided by the wider pharmacy profession. Overall, the studies involved a pharmacist–patient ratio of 1:14, which is not commensurate with clinical practice.
Methodological quality ranged from 2 to 5 on the Jadad scale, and nine of the studies scored 3 or more which represents high-quality studies with adequate randomization, flow, and fate of all patients in the trial known; in case of no data, the reasons were stated. The most commonly absent item was an adequate description of concealment of allocation. Only two studies18,22 – which had a score of less than 3 on the Jadad scale and hence reflected poor-quality research – reasonably reported no change in adherence rate.
Adherence to antidepressants
Researchers utilized numerous measurements to measure the change of medication adherence in these papers: patient self-reports (n = 6), pill counts (n = 3), prescription claims (n = 2), and an electronic pill container (n = 1). This led to the widely mixed results observed in these papers. All the investigators during the study included one method to measure the change in adherence either subjectively or objectively.
The impact of interventions by pharmacists on medication adherence as outlined in the studies in this review is summarized in Table 3. Seven investigations reported an improvement in patients’ adherence and two studies reported no significant change in patients’ adherence between control and tested groups; only three studies reported no change in adherence rate. All the latter three studies were conducted in an outpatient setting with a relatively small sample size reflecting an underpowered study.18,22,24 Notably, two of the studies18,19 that failed to show differences in effect on patients’ adherence had multiple interventions, ie, three or more different types of intervention.
Table 3.
Impact of pharmacist intervention on adherence to antidepressant medication
| Study | Pharmacist intervention | Adherence measures | Outcomes | Rate of adherence | |
|---|---|---|---|---|---|
|
| |||||
| Control/intervention | |||||
| Canales13 | Monitoring drug reactions, conducting patient drug education weekly, and counseling | Barnes rating scale | A significant improvement in adherence rate up to 27% | 27% | −7% |
| Simpson–Angus rating scale | 22% | −7% | |||
| Bultman14 | Performing patient interviews to assess medication history, drug knowledge and drug belief, patient satisfaction, medication adherence | Health communication model |
|
63% | 87% |
| Finley15 | Intake and follow-up interviews (three clinic visits and five telephone calls); drug prescribing and dose changes under protocol; drug information counseling | Prescription refills, clinic visit frequency |
|
81% | 66% |
| Finley16 | Drug monitoring; patient education; routine follow-up extensive phone calls at weeks 1, 2, 4, 10, and 16; Drug prescribing and medication change under protocol | Prescription refills, clinic visit frequency |
|
67% | 48% |
| Adler17 | Contacting patients nine times over the 18-month study; monitoring drug treatment; educating patients to maintain antidepressant medication | Antidepressant use rate |
|
60.6% | 48.9% |
| Capoccia18 | Performing patient follow-up by phone, interviewing patients twice during clinic visits. Patient contact during clinic visits (weeks 4 and 12); monitoring drug treatment; educating patients; providing drug refills and medication-dose adjustment |
Patient self-report Clinical visits |
|
59% | 57% |
| Rickles23 | Conducting three monthly phone calls to patients: during first call, assessing patient’s drug knowledge and belief, adverse effects, drug use status, treatment goals, and self-rated depression severity; follow up during second and third call | Frequency of feedback to pharmacist |
|
70% | 51% |
| Brook20 | Offered three telephone calls (10–20 minutes); provided a take-home video emphasizing medication adherence; documented number of pills and refill date | Pills consumed/day |
|
90% | 73% |
| Crockett22 | Pharmacists were given video-conference training on the nature and management of depression by a psychiatrist, psychologist, and general practitioner and asked to dispense medication with extra advice and support | Patient self-report | Adherence to medications was high in both groups (95% vs 96%) | 95% | 96% |
| Rickles23 | Three monthly telephone calls from pharmacists providing structured education and monitoring | Percentage of missed doses | Significantly more feedback to pharmacists regarding different aspects of their antidepressant therapy | ||
| Bosmans24 | Offered three education and coaching programs and a take-home video reviewing important facts on depression and antidepressant drugs | Electronic pill container | There were no significant differences in adherence | 88% | 86% |
| Al-Saffar21 | Patients received a patient information leaflet written in Arabic with counseling | Patient self-report | Good medication adherence at 2 and 5 months was more common in patients who were given a patient information leaflet (odds ratio 3.0, confidence interval 1.7–5.3) or a patient information leaflet plus counseling (odds ratio 5.5, confidence interval 3.2–9.6) | 39% | 10% |
| Tablet counting | 43% | 10% | |||
Impact of intervention on patients’ reported outcomes and depression severity
According to this systematic review, the majority of the papers monitored psychological dimensions such as depressive symptoms, mood, satisfaction, knowledge, and others. Eight studies measured depressive symptoms and six of them reported no statistical difference in improvement in depressive symptoms between the pharmacist intervention group and the control group. Only two studies13,24 reported improvement in depressive symptoms at various levels using various measures. Only four studies13,14,16,21 reported an improvement in patients’ satisfaction with the treatment and three studies reported a change in patients drug knowledge14,19,21 after pharmacist intervention. The improvement in depression severity and patients’ reported outcomes are summarized in Table 4, with an in-depth analysis of these studies shown in Table 5.
Table 4.
Impact of pharmacist intervention on patient reported outcome and depression
| Study | Pharmacist intervention | Outcome measures | Significant outcomes |
|---|---|---|---|
| Canales13 | Performing baseline assessment and weekly review; reviewing medical history and drug administration records; monitoring drug reactions; providing treatment recommendation; conducting patient drug education weekly and counseling | Depressive symptoms; cognitive function; quality of life; thought disorder; mood disorder |
|
| Bultman14 | Performing patient interviews twice to assess medication history, drug knowledge, and drug belief, patient satisfaction, medication adherence and monitoring patient behavior | Patient beliefs; patient knowledge; patient satisfaction with therapy; and adherence rate |
|
| Finley15 | Intake and follow-up interviews (three clinic visits and five phone calls); medical history review; drug prescribing and dose changes under protocol; drug information counseling | Patient satisfaction; clinic visit frequency; Resource utilization |
|
| Finley16 | Drug monitoring; patient education; routine follow-up extensive phone calls at weeks 1, 2, 4, 10, and 16; drug prescribing and medication change under protocol | Patient satisfaction; clinic visit frequency; resource utilization |
|
| Adler17 | Contacting patients nine times over the 18-month study; reviewing medication history, drug side effects and efficacy; assisting drug choice, dose, and regimen; providing social support; educating patients to maintain medication | Depression severity |
|
| Capoccia18 | Performing patient follow-up by phone Interviewing patients two times during clinic visits; patient contact during clinic visits (weeks 4 and 12); monitoring drug treatment (time drugs taken, change of drugs and other treatment); educating patients on side effects; providing drug refills and medication dose adjustment | Depressive symptoms; patient satisfaction, and clinical visits |
|
| Rickles19 | Conducting three monthly phone calls to patients: during first call, assessing patient’s drug knowledge and belief, adverse effects, drug use status, treatment goals, and self-rated depression severity; follow-up during second and third call. | Frequency of feedback to pharmacist; depressive symptoms; antidepressant knowledge and drug belief |
|
| Brook20 | Offered three phone calls (10–20 minutes); Provided a take-home video emphasizing medication adherence; documented number of pills and refill date | Depressive symptoms | No improvement in depressive symptoms was observed |
| Al-Saffar21 | Patients received a patient information leaflet written in Arabic with counseling | Interview questionnaires |
|
| Crockett22 | Pharmacists were given video-conference training on the nature and management of depression by a psychiatrist, psychologist and general practitioner and asked to dispense medication with extra advice and support | K10 and Drug Attitude Index |
|
| Rickles23 | Three monthly telephone calls from pharmacists providing structured education and monitoring | Frequency of patient feedback to pharmacists, antidepressant knowledge, depressive symptoms | Significantly more feedback to pharmacists regarding different aspects of their antidepressant therapy |
| Bosmans24 | Offered three education and coaching programs and a take-home video reviewing important facts on depression and antidepressant treatment | Hopkins Symptom Checklist | Improvements in the Hopkins Symptom Checklist depression mean item score and costs |
Table 5.
Detailed information about studies included in this review, 2000–2010
| Study | Type of publication | Year of publication | Year study conducted | Methodology | Study location | Setting | Study participants | Sample size | Brief description of study aims |
|---|---|---|---|---|---|---|---|---|---|
| Canales13 | Paper published in indexed American Journal of Health-System Pharmacy | 2001 | October 1996 to December 1997 | Carried out in two phases; control and experimental groups | Texas, USA | Inpatient | 2 | 93 | To determine the effects of a psychiatric pharmacist on clinical outcomes of acute care psychiatric inpatients and to monitor hospitalization costs |
| Bultman14 | Paper published in indexed Journal of the American Pharmacists Association | 2002 | November 1995 to July 1996 | Systematic, random sample of pharmacies and field study, patients were interviewed two times during the study | Wisconsin, USA | Community pharmacy | 23 | 100 | To examine the effects of pharmacist monitoring on patient satisfaction and adherence to antidepressant medication therapy |
| Finley15 | Paper published in indexed American Journal of Health-System Pharmacy | 2002 | July 1999 to June 2000, 10 months enrolment phase | Pharmacist follows up the patients through a combination of scheduled office visits and telephone calls. Working closely with psychiatric liaisons | California, USA | Primary care pharmacy | 2 | 220 | To examine effort to improve patient adherence to antidepressant drug therapy and outcomes |
| Finley16 | Paper published in indexed Pharmacotherapy | 2003 | Study conducted for 15 months, 9 months enrolment phase | A randomized controlled trial, compared the outcomes of intervention in care model with subjects receiving usual care | California, USA | Primary care pharmacy | 2 | 150 | To measure the effects of a collaborative care model that emphasized the role of clinical pharmacists in providing drug therapy management and treatment follow-up to patients with depression |
| Adler17 | Paper published in indexed General Hospital Psychiatry | 2004 | 1998 to 2000 | A randomized clinical trial of a pharmacist intervention for depressed patients, report antidepressant use and depression severity outcomes | Massachusetts, USA | Primary care pharmacy | 5 | 533 | To evaluate outcomes of a pharmacist intervention for depressed patients in primary care |
| Capoccia18 | Paper published in indexed American Journal of Health-System Pharmacy | 2004 | Study conducted for 16 months, November 1999 to March 2001 | Patients were randomized to enhanced care or usual care groups, for 1 year | Washington, USA | Primary care pharmacy | 2 | 74 | To evaluate the impact of pharmacist’s interventions in collaborative care to improve the care of, and outcomes for, patients with depression, to test the effectiveness of pharmacist interventions in collaboration models |
| Rickles19 | Paper published in indexed Journal of the American Pharmacists Association | 2005 | October 1, 2001 to September 30, 2002 | Randomized, controlled, unblended, mixed experimental design | Wisconsin, USA | Community pharmacy | 14 | 63 | To explore the impact of telephone-based education and monitoring by community pharmacists on multiple outcomes of pharmacist– patient collaboration |
| Brook20 | Paper published in indexed Journal of Psychiatric Services | 2005 | April 2000 to April 2001 | Randomized controlled trial with 6-month follow-up | The Netherlands | Community pharmacy | 19 | 147 | To improve adherence to antidepressant regimens through a pharmacist intervention |
| Al-Saffar21 | Paper published in indexed Journal of International Journal of Pharmacy Practice | 2005 | Study conducted for 18 months, 1999 to 2001 | Randomized into a control and two treatment groups. Treatment groups additionally received a patient information leaflet | Kuwait | Outpatient | 7 | 270 | To assess the acceptability and effectiveness of two educational initiatives on patterns of antidepressant medication use in depressed Kuwaiti patients |
| Crockett22 | Paper published in indexed The Australian Journal of Rural Health | 2006 | Parallel-groups design with a control and intervention group | New South Wales, Australia | Community pharmacy | 32 | 106 | Documentation and evaluation of patient outcomes into the role of rural community pharmacists in the management of depression | |
| Rickles23 | Paper published in indexed Journal of the American Pharmacists Association | 2006 | October 1, 2001 to September 30, 2002 | Randomized, controlled, experimental design | Wisconsin, USA | Community pharmacy | 14 | 60 | To determine whether telephone follow-up can influence the nature and extent to which antidepressant users provide feedback to pharmacists, whether patient characteristics are associated with the extent of patient feedback, how patient feedback affects subsequent outcomes after controlling for patient characteristics |
| Bosmans24 | Paper published in indexed Journal of PharmacoEconomics | 2007 | April 2000 to April 2001 | An economic evaluation performed alongside a 6-month randomized controlled trial | The Netherlands | Community pharmacy | 19 | 88 | To evaluate the cost effectiveness of a pharmacy-based intervention to improve adherence to antidepressant therapy in adult patients receiving treatment in primary care |
Types of pharmacist intervention
Five different types of pharmacist intervention were implemented in studies included in this review, which were as follows: (1) educating and counseling patients about the importance of adherence, explaining the side effects of medications and reviewing regimens; (2) monitoring drugs and following up drug reactions; (3) prescribing drug and dose changes to simplify regimens under protocol; (4) following up patients by phone calls and providing all information and response to patients enquiries, and (5) educating patients by providing a take-home video emphasizing the importance of medication adherence.13–24 The most common intervention strategy that pharmacists utilized was a combination of drug monitoring, drug counseling, and patient education. Four studies reported that pharmacists were authorized to prescribe medications and change doses under the supervision of psychiatrists or physicians.
A telephone call or a reminder was found to be an effective approach to improve medication adherence (Table 6). Five of six studies that included telephone contact with patients in the intervention reported a substantial improvement in medication adherence. The results of the only study that reported no significant change in adherence18 were probably due to a high adherence rate in the control group; a low ratio of pharmacists’ contact with patients that is one contact every 3 months, and an underpowered sample size (n = 74). However, the strategy of telephone support is limited in the extent to which it can be generalized for clinical practices because of time and cost considerations. Telephone contact can also be a barrier to clear communication and thus may affect the patients’ level of understanding.
Five studies assessed the impact of pharmacist intervention by providing patient education and monitoring.13,16–19 Four of the five studies demonstrated that involvement of the pharmacist was associated with a significant improvement in medication adherence.13,16,17,19 Again, it was the study reported by Capoccia and associates18 that found no significant change in adherence, which can be related to the aforementioned factors. The general findings from previous literature intervention studies and this review have shown that psychoeducation is an effective means of enhancing treatment adherence by offering structured and detailed information to patients about their treatments.3,30–32 This positive outcome may also be related to patients’ ever-changing belief systems about their antidepressant medications.33
Discussion
The challenge of evaluating complex and multifactorial pharmacist interventions with a combination of different adherence strategies has resulted in mixed outcomes and made it difficult to identify the most effective role that pharmacists may assume. In addition, heterogeneity in pharmacist interventions, treatment settings, patient populations, and measured outcomes is apparently large enough to discourage a meta-analysis of these findings.
This systematic review addressed an important role of pharmacists in providing pharmaceutical care to patients with depression. This critical narrative review revealed a positive effect of pharmacist interventions on antidepressant medication adherence by patients. The findings of this study are consistent with those of other researchers.34 In addition to revealing a positive effect of pharmacists’ intervention; this review also substantiated claims of improved medication adherence among depressed people who were treated by antidepressant medications prescribed by community mental health teams in Australia.34
There are some limitations in this research. Firstly, though a positive outcome in patient adherence to antidepressant medication was identified, it is unclear whether or not this will result in an improvement in depressive symptoms. However, previous studies have reported a positive association between improved antidepressant medication adherence and depressive symptoms, attributed to substantial changes in adherence to antidepressant medications.35 Secondly, the randomized controlled trials included had different methodological approaches, such as the pharmacy settings in terms of outpatient and inpatient pharmacy, type of diagnostic measures, adherence measures, and types of intervention performed. The different methodologies applied in the reviewed studies make the interpretation of results difficult. Thirdly, no study measured the relation between the change in adherence and relapse of depression because most studies were of less than 7 months’ duration. It has been suggested that in order to assess the effectiveness of an intervention on relapse of depression, the intervention and follow-up duration should be extended to at least 2 years.12 Largely, a 6-month follow-up period is a short time when referring to antidepressant treatment given to patients with multiple relapses of depression. This period needs to be extended to at least 6 months when remission of an episode of depression is expected. However, evidently dropouts occur mostly at the beginning of treatment with antidepressant medications. In some trials, the 2-month follow-up period did not alter the results including effect sizes.22
Fourthly, the included studies used different medication adherence measures as there is no cornerstone measurement for medication adherence. The objective (pill counts, electronic monitoring, and monitoring blood plasma concentration) versus subjective (self-administered questionnaires, self-reports, and physicians evaluation reports) medication adherence measurements tend to cause varied results in medication adherence studies. However, limiting the measurement to just one method increases the possibility of imprecise measurement of changes in adherence, while using two methods will overcome the disadvantage of each method alone. Only Al-Saffar and colleagues21 utilized two methods: tablet counting and patient self-report. For instance, Velligan et al36 reported that the data from objective measurements to oral antipsychotic medications were strongly correlated (r[k] = 0.61) but subjective measurements were weakly correlated with objective measurements, when adherence scores were examined by rank-order correlations (r[k] = 0.18–0.32). Blood plasma concentrations, an objective measurement, were not correlated with any other measures of adherence (kappa ≤ 20). They also found that the data from subjective measurement reports were best correlated with clinical state, which can be reliably utilized in daily clinical practices.
Fifthly, most of the included articles were published in pharmacy journals, ie, nine out of 12; it is quite possible that a publication bias influenced this trend. The majority of the studies involved compared the effectiveness of intervention between pharmacists’ intervention group and usual care control group. However, none of these studies directly compared the effectiveness of intervention between pharmacists and other healthcare providers. Adverse drug side effects was cited as the leading cause of early discontinuation of medication and non-adherence to treatment: none of these studies indicated pharmacist intervention to manage these side effects.
Finally, in spite of these limitations, this study is, to the best of our knowledge, the first published systematic review of pharmacist interventions in patients with depression. Our review indicates that pharmacist interventions can improve patient adherence to antidepressant medications and also highlights the role of pharmacists in psychiatric pharmaceutical care services. These data show that patient counseling and treatment monitoring conducted by pharmacists can improve adherence to antidepressant medication.
Conclusion
This systematic review of the literature highlighted the expanded roles of pharmacists, especially their interventions in the management of patients with depression in particular adherence to drug regimen. Notably, the data showed that patient counseling and treatment monitoring conducted by pharmacists can improve adherence to antidepressant medications. Pharmacist-conducted medication reviews and resulting recommendations to optimize medication use by patients with depression may reduce the complexity of the medication regimen and adherence. The available published evidence-based data tend to support the continued expansion of the pharmacist’s role in the care of patients with depression and adherence to the treatment. Further studies are needed to assess the clinical outcomes of innovative pharmacist interventions based on theories that can explain the outcome and mechanisms of change with regard to patient adherence to medication. In summary, evidence from the studies reviewed strongly support the role of pharmacists in providing different types of interventions to improve medication adherence to antidepressant treatment by patients with depression in different settings.
Special note
In major psychiatric treatment settings in the Kingdom of Saudi Arabia, pharmacist clinics have been established to provide counseling, review of prescribed medications, and collaborative management of the adverse effects of psychotropic drugs in outpatient settings. In addition, clinical pharmacists are important active players in multidisciplinary clinical teams that undertake regular rounds of inpatients and discuss different issues, including medications. Pharmacists contribute to the safe prescription and dispensing of drugs to health consumers, coupled with brief counseling focusing on adherence to treatment and its benefits. There is no database regarding their multiple roles and their effectiveness in clinical pharmacy services. Therefore, it would be timely to conduct studies in the Kingdom of Saudi Arabia that focus on pharmacist interventions and how to enhance medication adherence in the psychiatric population in general but in particular in patients with depression.
Footnotes
Disclosure
The authors did not disclose any conflicts of interest in this systematic review.
References
- 1.Vergouwen AC, Burger H, Verheij TJ, Koerselman F. Improving patients’ beliefs about antidepressants in primary care: A cluster-randomized controlled trial of the effect of a depression care program. Prim Care Companion J Clin Psychiatry. 2009;11(2):48–52. doi: 10.4088/pcc.08m00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katon W, Von Korff M, Lin E, Bush T, Ormel J. Adequacy and duration of antidepressant treatment in primary care. Med Care. 1992;30:67–76. doi: 10.1097/00005650-199201000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Vergouwen ACM, Bakker A, Katon WJ, Verheij TJM, Koerselman F. Improving adherence to antidepressants: a systematic review of interventions. J Clin Psychiatry. 2003;64:1415–1420. doi: 10.4088/jcp.v64n1203. [DOI] [PubMed] [Google Scholar]
- 4.Rubio-Valera M, Serrano-Blanco A, Travé P, Penarrubia-Maria MT, Ruiz M, Pujol M. Community pharmacist intervention in depressed primary care patients (PRODEFAR study): randomized controlled trial protocol. BMC Public Health. 2009;9:284–292. doi: 10.1186/1471-2458-9-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanlon JT, Artz MB. Drug-related problems and pharmaceutical care. Medical Care. 2001;39(2):109–112. doi: 10.1097/00005650-200102000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Adamcik BA, Ransford HE, Oppenheimer PR, Brown JF, Eagan PA, Weissman FG. New clinical roles for pharmacists: A study of role expansion. Soc Sci Med. 1986;23:1187–1200. doi: 10.1016/0277-9536(86)90338-2. [DOI] [PubMed] [Google Scholar]
- 7.White EV, Latif DA. Reengineering pharmacotherapy delivery to maximize the role of the pharmacist and improve patient outcomes. Res Social Adm Pharm. 2007;3:223–235. doi: 10.1016/j.sapharm.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Kenreigh CA, Wagner LM. Pharmacists’ role in healthcare still evolving. [Accessed November 23, 2011];Medscape Today News. 2006 8(2) [cited November 3, 2006] http://www.medscape.com/viewarticle/546717. [Google Scholar]
- 9.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 10.Olivo SA, Macedo LG, Gadotti IC, Fuentes J, Stanton T, Magee DJ. Scales to assess the quality of randomized controlled trials: a systematic review. Phys Ther. 2008;88(2):156–175. doi: 10.2522/ptj.20070147. Epub December 11, 2007. [DOI] [PubMed] [Google Scholar]
- 11.Garcia-Campayo J, Magdalena J, Magallón R, Fernández-García E, Salas M, Andrés E. A meta-analysis of the efficacy of fibromyalgia treatment according to level of care. Arthritis Res Therapy. 2008;10:1–15. doi: 10.1186/ar2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Towheed TE. Is the Jadad Score the proper evaluation of trials? J Rheumatol. 2006;33:1711. (correspondence) [PubMed] [Google Scholar]
- 13.Canales P, Dorson P, Crismon M. Outcome assessment of clinical pharmacy services in a psychiatric inpatient setting. Am J Health Syst Pharm. 2001;58(13):1309–1316. doi: 10.1093/ajhp/58.14.1309. [DOI] [PubMed] [Google Scholar]
- 14.Bultman D, Svarstad B. Effects of pharmacist monitoring on patient satisfaction with antidepressant medication therapy. J Am Pharm Assoc (Wash) 2002;42(1):36–43. doi: 10.1331/108658002763538053. [DOI] [PubMed] [Google Scholar]
- 15.Finley P, Rens H, Pont J, et al. Impact of a collaborative pharmacy practice model on the treatment of depression in primary care. Am J Health Syst Pharm. 2002;59(16):1518–1526. doi: 10.1093/ajhp/59.16.1518. [DOI] [PubMed] [Google Scholar]
- 16.Finley P, Rens H, Pont J, et al. Impact of a collaborative care model on depression in a primary care setting: a randomised controlled trial. Pharmacotherapy. 2003;23(9):1175–1185. doi: 10.1592/phco.23.10.1175.32760. [DOI] [PubMed] [Google Scholar]
- 17.Adler DA, Bungay KM, Wilson IB, et al. The impact of a pharmacist intervention on 6-month outcomes in depressed primary care patients. Gen Hosp Psychiatry. 2004;26(3):199–209. doi: 10.1016/j.genhosppsych.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 18.Capoccia KL, Boudreau DM, Blough DK, et al. Randomized trial of pharmacist interventions to improve depression care and outcomes in primary care. Am J Health Syst Pharm. 2004;61(4):364–372. doi: 10.1093/ajhp/61.4.364. [DOI] [PubMed] [Google Scholar]
- 19.Rickles N, Svarstad B, Statz-Paynter J, Taylor L, Kobak K. Pharmacist telemonitoring of antidepressant use: effects on pharmacist–patient collaboration. J Am Pharm Assoc. 2005;45(3):344–353. doi: 10.1331/1544345054003732. [DOI] [PubMed] [Google Scholar]
- 20.Brook OH, van Hout H, Stalman W, et al. A pharmacy-based coaching program to improve adherence to antidepressant treatment among primary care patients. Psychiatr Serv. 2005;56(4):487–489. doi: 10.1176/appi.ps.56.4.487. [DOI] [PubMed] [Google Scholar]
- 21.Al-Saffar N, Deshmukh AA, Adib SM. Effect of information leaflets and counselling on antidepressant adherence: open randomized controlled trial in a psychiatric hospital in Kuwait. Int J Pharm Practice. 2005;13:123–131. [Google Scholar]
- 22.Crockett J, Taylor S, Grabham A, Stanford P. Patient outcomes following an intervention involving community pharmacists in the management of depression. Aust J Rural Health. 2006;14(6):263–269. doi: 10.1111/j.1440-1584.2006.00827.x. [DOI] [PubMed] [Google Scholar]
- 23.Rickles NM, Svarstad BL, Statz-Paynter JL, Taylor LV, Kobak KA. Improving patient feedback about and outcomes with antidepressant treatment: a study in eight community pharmacies. J Am Pharm Assoc. 2006;46(1):25–32. doi: 10.1331/154434506775268715. [DOI] [PubMed] [Google Scholar]
- 24.Bosmans JE, Brook OH, van Hout HPJ, et al. Cost-effectiveness of a pharmacy-based coaching programme to improve adherence to antidepressants. Pharmacoeconomics. 2007;25(1):25–37. doi: 10.2165/00019053-200725010-00004. [DOI] [PubMed] [Google Scholar]
- 25.Sabaté E, editor. Adherence to Long-term Therapies: Evidence for Action. Geneva: World Health Organization; 2003. [Accessed December 13, 2012]. Available from: http://www.who.int/chp/knowledge/publications/adherence_report/en/ [Google Scholar]
- 26.Steiner JF, Earnest MA. The language of medication-taking. Ann Intern Med. 2000;132(11):926–930. doi: 10.7326/0003-4819-132-11-200006060-00026. [DOI] [PubMed] [Google Scholar]
- 27.Sawada N, Uchida H, Suzuki T, et al. Persistence and compliance to antidepressant treatment in patients with depression: A chart review. BMC Psychiatry. 2009;9:38. doi: 10.1186/1471-244X-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bausewein C, Higginson IJ. Appropriate methods to assess the effectiveness and efficacy of treatments or interventions to control cancer pain. J Palliat Med. 2004;7(3):423–430. doi: 10.1089/1096621041349572. [DOI] [PubMed] [Google Scholar]
- 29.Finley PR, Crismon ML, Rush AJ. Evaluating the impact of pharmacists in mental health: a systematic review. Pharmacotherapy. 2003;23(12):1634–1644. doi: 10.1592/phco.23.15.1634.31952. [DOI] [PubMed] [Google Scholar]
- 30.Demyttenaere K, Haddad P. Compliance with antidepressant therapy and antidepressant discontinuation symptoms. Acta Psychiatr Scand. 2000;1(Suppl 403):50–56. doi: 10.1111/j.1600-0447.2000.tb10948.x. [DOI] [PubMed] [Google Scholar]
- 31.Lin EH, Von Korff M, Ludman EJ, et al. Enhancing adherence to prevent depression relapse in primary care. Gen Hosp Psychiatry. 2003;25(5):303–310. doi: 10.1016/s0163-8343(03)00074-4. [DOI] [PubMed] [Google Scholar]
- 32.Demyttenaere K. Noncompliance with antidepressants: who’s to blame? Int Clin Psychopharmacol. 1998;13(Suppl 2):S19–25. [PubMed] [Google Scholar]
- 33.Holma AK, Holma KM, Melartin TK, Isometsä ET. Treatment attitudes and adherence of psychiatric patients with major depressive disorder: A five-year prospective study. J Affect Disord. 2010;127(1):102–111. doi: 10.1016/j.jad.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 34.Bell S, McLachlan AJ, Aslani P, Whitehead P, Chen TF. Community pharmacy services to optimise the use of medications for mental illness: a systematic review: a systematic review. Aust New Zealand Health Policy. 2005;2:29. doi: 10.1186/1743-8462-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bower P, Gilbody S, Richards D, Fletcher J, Sutton A. Collaborative care for depression in primary care. Making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry. 2006;189:484–493. doi: 10.1192/bjp.bp.106.023655. [DOI] [PubMed] [Google Scholar]
- 36.Velligan DI, Wang M, Diamond P, et al. Relationships among subjective and objective measures of adherence to oral antipsychotic medications. Psychiatr Serv. 2007;58:1187–1192. doi: 10.1176/ps.2007.58.9.1187. [DOI] [PubMed] [Google Scholar]