Abstract
Anterior gradient-2 (AGR2) promotes tumor growth, cell migration, and cellular transformation, and is one of the specific mRNA markers for circulating tumor cells in patients with gastrointestinal cancer. We investigated the feasibility of AGR2 as a potent antigen for tumor immunotherapy against colorectal cancer (CRC) cells using dendritic cells (DCs) transduced with a recombinant adenovirus harboring the AGR2 gene (AdAGR2). DCs transduced with a recombinant adenovirus encoding the AGR2 gene (AdAGR2/DCs) were characterized. These genetically-modified DCs expressed AGR2 mRNA as well as AGR2 protein at a multiplicity of infection of 1,000 without any significant alterations in DC viability and cytokine secretion (IL-10 and IL-12p70) compared with unmodified DCs as a control. In addition, AdAGR2 transduction did not impair DC maturation, but enhanced expression of HLA-DR, CD80, and CD86. AdAGR2/DCs augmented the number of IFN-γ-secreting T-cells and elicited potent AGR2-specific cytotoxic T lymphocytes capable of lysing AGR2-expressing CRC cell lines. These results suggest that AGR2 act as a potentially important antigen for immunotherapy against CRC in clinical applications.
Keywords: AGR2 protein, human; antigens, neoplasm; colorectal neoplasms; dendritic cells; immunotherapy, active
Introduction
Cancer immunotherapy based on dendritic cell (DC) vaccination is an exciting prospect for the treatment of cancer (Banchereau and Palucka, 2005). A central tenet of cancer immunotherapy is the generation of an antigen-specific cytotoxic T lymphocyte (CTL) response (Melief et al., 2002). The CTL response is dependent on suitable tumor-associated antigens (TAAs). In turn, TAAs can induce T lymphocytes that recognize tumors, but not normal tissues (Parmiani et al., 2007). TAAs should be expressed in a significant proportion of tumor cells and are obligatory for the survival of tumor cells. DCs pulsed with various TAAs have been shown to be effective in producing specific anti-tumor effects in vitro and in vivo (Nakamura et al., 2005).
One of the most interesting tumor antigens in colorectal cancer (CRC) is the carcinoembryonic antigen (CEA) because CEA is extensively expressed in the vast majority of patients with CRC. However, the induction of immune responses against antigens that are expressed not only by tumor cells but also by benign tissues, such as CEA, is more difficult because rapid induction of tolerance against the so-called "self antigens" occurs (Thompson et al., 1991). Human tumors express a number of specific antigens that can be recognized by T cells, thus the discovery of a variety of novel TAAs, especially those shared among patients, is needed to improve the efficacy of DC-based cancer immunotherapy in patients with CRC.
Different strategies have been attempted to load DCs with tumor antigens, including irradiated tumor cells, tumor lysates, tumor RNA, antigen peptides, or antigen-gene transfer via non-viral or viral vectors (Mayordomo et al., 1995; Ashley et al., 1997; Nestle et al., 1998). The most commonly used method, loading with peptides or proteins, is not a very efficient method because the half-life of complexes of MHC molecules and peptides is very short. Prolonged presentation due to stable antigen expression by a genetic modification of DCs appears to be a more promising method. Recently, several studies have reported that TAA gene-modified DCs can provide extended antigen presentation and induce antigen-specific CTLs more efficiently than peptide pulsing (Oh et al., 2006). In previous studies, DCs have been shown to be amenable to adenovirus (Ad) vector infection in vitro (Zhong et al., 1999). Moreover, an Ad-modified DC vaccine, produced using the Ad to transfer the TAA ex vivo, successfully induced T cell immunity against target tumor cells expressing relevant antigen in vitro and in vivo in experimental tumor models (Song et al., 1997).
Anterior gradient-2 (AGR2) is a secreted protein, which was initially described in Xenopus laevis, and identified in a screen for differentially-expressed genes in neural development (Aberger et al., 1998). In humans, AGR2 was first identified in studies which focused on differentially-expressed genes in estrogen receptor-positive breast cancers. Subsequent studies showed elevated AGR2 expression in adenocarcinomas of the breast (Liu et al., 2005), esophagus (Hao et al., 2006), pancreas (Ramachandran et al., 2008), and prostate (Zhang et al., 2007). Recently, it has been reported that AGR2 promotes tumor growth, cell migration, and cellular transformation and is one of the specific mRNA markers for circulating tumor cells in cancer patients with gastrointestinal cancer (Valladares-Ayerbes et al., 2008). The fact that AGR2 overexpression may provide a survival benefit for tumor cells and the enhanced expression is almost completely restricted to malignant tissues makes AGR2 an interesting target for the development of immunotherapeutic strategies.
In the present study the efficiency of Ad encoding AGR2 transduction in monocyte-derived DCs was evaluated. We showed that AdAGR2 is capable of transducing human DCs, the transduction was not compromised, and the transduced DCs were able to elicit AGR2-specific CTL responses against AGR2-expressing CRC cells. Taken together, the results of the current study have shown that AGR2 is a potentially useful antigenic target for cancer immunotherapy using DCs against CRC.
Results
Adenoviral transduction of DCs in vitro
In preliminary experiments (submitted), most CRC cell lines were shown to express AGR2 protein based on WB and flow cytometric analyses (AGR2+ cell lines: KM12C, HCT-8, DLD1, DK01, and HT-29; AGR2- cell lines: HCT-116 and SW620).
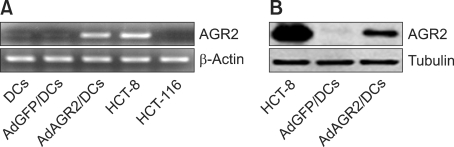
To produce recombinant adenovirus encoding AGR2 (AdAGR2), the AGR2 gene was cloned into BglII/XhoI sites of an Ad transfer vector pShuttle-CMV. Recombinant AdAGR2 stocks were generated using a helper virus-free packaging system. The infectious titer of AdAGR2 was 2 × 1011 viral particles per ml. The transduction efficiency of AdAGR2 in DCs at a multiplicity of infection (MOI) of 1,000 was determined by RT-PCR and WB. DCs expressed AGR2 mRNA (Figure 1A) and protein (Figure 1B) efficiently. HCT-8 and HCT-116 CRC cell lines were used as positive and negative controls, respectively.
Figure 1.
Ad-mediated gene transfer and expression in DCs in vitro. AGR2 gene was cloned and monocyte-derived DCs were infected with AdAGR2 at a multiplicity of infection (MOI) of 1,000. Seventy-two hours later, the expression of AGR2 was analyzed by RT-PCR (A) and WB (B). HCT-8 and HCT-116 cells were used as AGR2-positive and -negative controls, respectively.
Characteristics of AdAGR2-transduced DCs
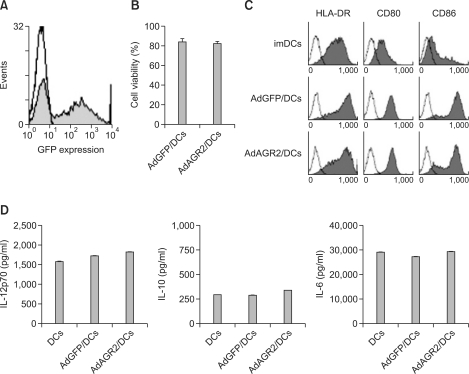
An MOI of 1,000 accomplished transgene expression in 47.1 ± 6.5% of the DCs (Figure 2A). To evaluate the effect of AdAGR2 transduction on DCs, viability, phenotypic expression, and cytokine secretions were analyzed. AdAGR2 transduction did not show any detrimental effect on the viability of DCs, as estimated by intravital staining with trypan blue (Figure 2B). As shown in Figure 2C, AdGFP- and AdAGR2-transduced DCs exhibited a strongly increased expression of CD80, CD86, and HLA-DR compared to imDCs. However, there was no significant difference between AdGFP- and AdAGR2-transduced DCs. In addition, the production of IL-12p70, IL-10, and IL-6 from DCs was not altered by AdAGR2-transduction compared to untreated and AdGFP-transduced DCs (Figure 2D).
Figure 2.
Ad transduction efficiency in DCs and characterization of AdAGR2-transduced DCs. Monocyte-derived DCs were transduced with AdGFP on day 5, then 2 days after maturation cells were analyzed for the expression of GFP by flow cytometry. The results showed 47.13 ± 6.48% cells were GFP-positive at a MOI of 1,000 (A). Data represent the mean ± SD of 5 independent experiments. Cell viability after transduction in DCs was measured by 0.4% trypan blue exclusion (B). FACS was performed to analyze the cell surface markers of DCs and the expression of CD80, CD86, and HLA-DR molecules was enhanced by AdAGR2 transduction (C). Isotype control in each group is indicated in white. Three experiments with similar results were performed. Cytokine secretion of IL-12p70, IL-10, and IL-6 after transduction was measured by ELISA (D)
Induction of AGR2-specific CTL responses by AdAGR2-transduced DCs
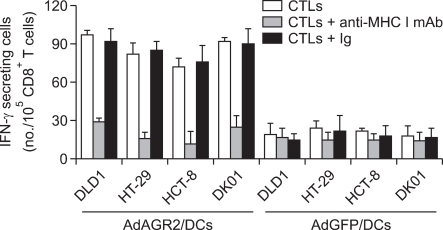
Autologous CD8+ T cells were sensitized for CTL induction with AdAGR2-transduced or untreated DCs. The effector T cells were compared to the ability to recognize AGR2-positive CRC cell lines, such as DLD1, HT-29, HCT-8, and DK01, by an IFN-γ ELISPOT assay at an E:T ratio of 20:1 (Figure 3). CTLs generated by AdAGR2-transduced DCs recognized the AGR2-positive CRC cell lines and the responses were specifically inhibited by MHC class I blockade. HCT-8 and HT-29 cell lines were shown to have more sensitive targeting to AGR2-specific CTLs, whereas no significant IFN-γ secretion occurred in the control group using AdGFP-transduced DCs.
Figure 3.
AGR2-specific CTL response by transduced DCs. ELISPOT assay showing the number of IFN-γ-secreting cells per 105 CD8+ T cells induced by AdGFP- and AdAGR2-transduced DCs, respectively, at an E:T ratio of 20:1. Several AGR2-expressing CRC cell lines were used as targets. MHC class I restriction of the CTLs was analyzed using a MHC class I specific monoclonal Ab (clone W6/32). Nonspecific response was determined by irrelevant Ig blockade. Representative results of 4 independent experiments are shown.
Characterization of AGR2-specific CTLs induced by AdAGR2-transduced DCs
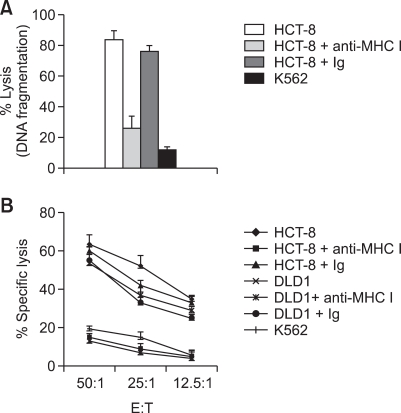
The functional capability of the CTL response to AdAGR2-transduced DCs was tested by determining whether or not the CTLs could specifically lyse target cells using the JAM and 4-h standard 51Cr-release assays. In the JAM assay (Figure 4A), the CTLs sensitized by AdAGR2-transduced DCs had high lytic activity against the AGR2-positive HCT-8 CRC cell line at an E:T ratio of 40:1. The response was specifically inhibited by MHC class I mAbs. No significant killing activity was observed against the K562 cell line, excluding the possibility that NK cells contributed to the cytotoxicity. We next examined the cytotoxic activity of these CTLs against AGR2-positive CRC cell lines, including HCT-8 and DLD1, using a standard 4-h 51Cr-release assay. As shown in Figure 4B, CTLs induced by AdAGR2-transduced DCs effectively lysed AGR2-positive CRC cell lines, such as HCT-8 and DLD1, in a dose-dependent manner according to the E:T ratio. MHC class I restriction of the CTLs was detected using a MHC class I-specific mAb. No killing was observed against the K562 cell line. The results demonstrated that CTLs generated by autologous DCs transduced with AdAGR2 showed strong cytotoxic activity against AGR2-positive CRC cell lines in vitro. These findings suggest that an AdAGR2/DCs vaccine may serve as a feasible approach for the treatment of patients with AGR2-associated CRC.
Figure 4.
Cytotoxicity of AGR2-specific CTLs. CTLs were generated by autologous CD8+ T cells from healthy donors stimulated with AdAGR2-transduced DCs. Lytic activity of CTLs generated by AdAGR2-transduced DCs was analyzed by DNA fragmentation at an E:T ratio of 20:1 (A) and 4-h standard 51Cr-release assay at different E:T ratios (50:1, 25:1, and 12.5:1) (B) against AGR2-positive HCT-8 and DLD1 target cells. MHC class I restriction of the CTLs was analyzed using a MHC class I-specific mAb. Nonspecific response was determined by irrelevant Ig blockade. The NK-sensitive K562 cell line was used to exclude the possibility that NK cells contributed to the cytotoxicity. Results of 4 independent experiments are shown.
Discussion
Identification of appropriate target TAAs and effective delivery into DCs with stable expression are major limitations for DC-based immunotherapy. Recently, several studies have revealed that TAA gene-modified DCs can provide extended antigen presentation and induce antigen-specific CTLs more efficiently than peptide pulsing (Nakamura et al., 2005). Previous studies have shown that self-antigens overexpressed in malignant tissue can provide a basis for a tumor-specific immune response. The majority of TAAs recognized thus far by tumor-infiltrating T cells in patients are non-mutated proteins (Rosenberg, 1997). It is therefore of great interest to establish whether or not these self-antigens can be used to stimulate a tumor-specific T cell response.
Several studies have shown elevated AGR2 expression in adenocarcinomas of the breast, esophagus, pancreas, and prostate (Liu et al., 2005; Hao et al., 2006; Zhang et al., 2007; Ramachandran et al., 2008). The aberrant expression of AGR2 in CRC remains unknown. Recently, it has been reported that AGR2 promotes tumor growth, cell migration, and cellular transformation and is one of the specific mRNA markers for circulating tumor cells in cancer patients with gastrointestinal cancer (Valladares-Ayerbes et al., 2008). Here, for the first time, we report that AGR2 protein was expressed at a high level in CRC cells. The fact that AGR2 overexpression may provide a survival benefit for tumor cells and the enhanced expression is almost completely restricted to malignant tissues, thus making AGR2 an interesting target for the development of immunotherapeutic strategies. Also, recombinant adenovirus encoding AGR2 was efficiently transduced in DCs without alteration of functional DC capacity, elicited AGR2-specific CTL generation, and lysed AGR2-positive CRC target cells.
Gene transfer is a powerful means to manipulate the properties of DCs for therapeutic advantage to augment the immune response and is currently under extensive evaluation in pre-clinical and clinical trials. Most investigations have focused on transferring genes encoding activating cytokines and tumor antigens to DCs (Gong et al., 1997). While a variety of vectors, including adenovirus, adeno-associated virus, retrovirus, and lentivirus, are capable of producing gene transfer to DCs (Aicher et al., 1997), adenoviral vectors hold several distinct advantages. First, adenovirus is one of the most efficient vehicles for DC gene therapy (Di Nicola et al., 1998). Moreover, in addition to achieving a high degree of transgene expression (Benihoud et al., 1999), the adenoviral vector itself, without the addition of a therapeutic transgene, matures and activates DCs by enhancing the expression of MHC and co-stimulatory molecules in human (Rea et al., 1999) and murine (Hirschowitz et al., 2000) models. In addition, it has been reported that adenoviral gene transduction to DCs produce IL-12 in significant amounts and increased CCR7 expression on DCs, leading to enhanced migratory capacity of DCs to draining LNs in which DCs can stimulate T cells (Hirschowitz et al., 2000; Nakamura et al., 2005).
In the present study we revealed that recombinant adenovirus efficiently transduced in DCs and GFP expression in DCs was successfully accomplished at a MOI of 1,000 without significant cell death. Hirschowitz et al. reported that adenovirus infection increases DC surface expression of MHC class II proteins and B7 co-stimulatory molecules. Consistent with previous reports (Benihoud et al., 1999; Rea et al., 1999; Hirschowitz et al., 2000), AdAGR2 transduction in DCs enhanced DC activation and maturation by showing higher expression of CD80, CD86, and HLA-DR than untreated DCs. However, cytokine production, such as IL-12p70, IL-6, and IL-10 from transduced DCs, was not altered compared to the untreated DCs in the current study.
In conclusion, cancer immunotherapy using DCs transduced with the entire gene encoding AGR2 elicited efficient immune responses against CRC, as shown by AGR2-specific CTL generation. Thus, this study is the first to provide strong and direct evidence to support the application of AGR2-based immunotherapy in CRC. In addition, the identification of T-cell epitopes from AGR2 as a TAA protein in CRC is available. Further studies to enhance the in vivo anti-tumor effect of AGR2 as a tumor antigen against CRC will be necessary before clinical application.
Methods
Target cell lines
The following human CRC cell lines were used as target cells: DK01; DLD1; HCT-8 (all HLA-A*0201+, A*2402+); HCT-116 (HLA-A*0101+ and A*0201+); and HT-29 (HLA-A* 24+). All cell lines were purchased from the American Type Culture Collection (ATCC; Rockville, MD) and maintained in RPMI-1640 supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin (PS; all from Gibco-BRL, Grand Island, NY). K562 cells were obtained from the Korea Cell Line Bank (KCLB; Seoul, Korea) and used as natural killer (NK) cell-sensitive targets.
Construction and production of recombinant Ad encoding AGR2
The recombinant Ad encoding AGR2 (AdAGR2) was constructed using the AdEasy™ vector system (Qbiogene Inc., Carlsbad, CA), according to the manufacturer's instructions. Briefly, the full length of AGR2 cDNA was amplified by a polymerase chain reaction (PCR) using AGR2 sense primer 5'-atggagaaaattccagtgtca-3' containing the Bgl II site and AGR2 antisense primer 5'-ttacaattcagtcttcagcaa-3' containing the Xho I site. The obtained PCR products were cloned in Ad transfer vector (pShuttle-CMV; AES1021) at the BamHI and Xho I enzymes in multiple cloning sites (MCS), and sequenced to identify possible Taq polymerase errors. Subsequently, the AGR2 expression cassette was inserted into viral DNA vector (pAdEasy-1; AES1010). After packaging the recombinant adenoviral DNA into infectious Ad by transfecting HEK 293A cells, the adenovirus containing AGR2 gene was amplified and purified from cell lysates by banding twice in CsCl density gradients, as described previously (Eloit et al., 1990). Viral products were desalted and stored at -80℃ in phosphate-buffered saline (PBS) containing 10% glycerol (v/v). A similar protocol was used to generate recombinant Ad encoding green fluorescent protein (GFP; AdGFP). The titer of the viral stock was determined using the tissue culture infectious dose (TCID50) method.
Generation of DCs
Peripheral blood was collected from healthy donors with HLA-A0201+ after obtaining informed consent and approval by the institution ethical committee of the Chonnam National University Hwasun Hospital. The monocytes were isolated by two-step density gradient centrifugation followed by plastic adherence, as previously described (Muthuswamy et al., 2008). Briefly, the adherent monocytes (purity > 95 %) were cultured for 6 days at 5 × 105 cells per well in 24-well plates (BD Biosciences-Labware, San Jose, CA) in Iscove's modified Dulbecco's medium (IMDM) supplemented with 10% FBS and 1% PS in the presence of recombinant human granulocyte macrophage-colony-stimulating factor (rhGM-CSF, 50 ng/ml; LG Biochemical, Daejeon, Korea) and interleukin-4 (rhIL-4, 20 ng/ml; PEPROTECH, Rocky Hill, NJ). For the generation of AGR2-specific CTL lines, the immature DCs were cultured for an additional 2 days using αDC1-polarizing cocktails composed of IL-1β (25 ng/ml; PEPROTECH), TNF-α (50 ng/ml; PEPROTECH), IFN-α (3,000 units/ml, Intron-A-IFN-α-2b; Schering-Plough International, Kenilworth, NJ), IFN-γ (1,000 units/ml; Strathmann Biotech GmbH, Hannover, Germany), and poly-I:C (20 µg/ml; Sigma-Aldrich, St. Louis, MO) for final maturation.
Ad transduction in DCs
To determine transduction efficiency, 1 × 106 immature DCs were suspended in IMDM with 10% FBS and exposed to AdGFP at a multiplicity of infection (MOI) of 1,000 for 2 h at 37℃. After washing twice, the transduced DCs were resuspended in fresh cytokine-supplemented medium and cultured for an additional 2 days using a maturation cytokine cocktail. Subsequently, the expressions of GFP and DC phenotypes were assayed by a FACSAria cell sorter (Becton Dickinson, San Jose, CA) and the data were analyzed with FACSDiva™ (Becton Dickinson) and WinMDI™ version 2.9.
Immunophenotyping of DCs
For phenotype analysis, AdGFP- and AdAGR2-infected DCs were stained with phycoerythrin (PE)-conjugated CD1a, CD11c, CD38, CD54, CD80, and CD86 (AdGFP/DCs and AdAGR2/DCs; Becton Dickinson) and fluorescein isothiocyanate (FITC)-conjugated CD14, CD40, CD83, HLA-DR, and CCR7 for unmodified and AdAGR2/DCs (Becton Dickinson).
AGR2 expression
AGR2 surface expression of CRC cell lines was determined by serial incubation with primary rabbit anti-AGR2 monoclonal antibody [Ab] (ab76473; Abcam, Cambridge, UK) and secondary AffiniPure goat anti-rabbit IgG(H+L) conjugated with FITC (Jackson ImmunoResearch Laboratories, Inc., West Grove, PA). For Western blot (WB) analysis, proteins in the cell extracts were separated by 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), then transferred onto a nitrocellulose (NC) membrane. The NC membrane was incubated with 5% non-fat milk in PBS, then with rabbit anti-human AGR2 polyclonal Ab (ab43043; Abcam) for 2 h at room temperature (RT). After washing, the membrane was incubated with a horseradish peroxidase-conjugated goat anti-rabbit IgG Ab (ab6721; Abcam) for 1 h at RT. Immunoreactive bands were detected using the WEST-one™ Western Blot Detection System (iNtRON BIOTECHNOLOGY, Daejeon, Korea) and were analyzed with a LAS-3000 imaging system (Fujifilm Corporation, Tokyo, Japan).
RT-PCR
Expression of AGR2 mRNA in DCs or AdAGR2 transduced-DCs and CRC tumor cell lines was assayed by RT-PCR amplification using a cellular mRNA control. The mRNA from the cells was extracted according to the manufacturer's instructions. Total RNA was isolated from tumor cells with a RNeasy Mini kit (QIAGEN, Valencia, CA). First-strand cDNA synthesis was performed using oligo (dT) 18 primers. The following PCR primers were used: AGR2 forward, 5'-ATTGGCAGAGCAGTTTGTCC-3' and reverse, 5'-GAGCTGTATCTGCAGGTTCGT-3'; and β-actin forward, 5'-CCCTCCATCGTCCACCGCAAATGCTTC-3' and reverse, 5'-CGACTGCTGTCACCTTCACCGTTCCAG-3'. Each of the primer sets was confirmed by running samples on agarose gels. β-actin transcript levels were used to normalize the amount of cDNA in each sample.
ELISA
ELISA for IL-12p70, IL-10, and IL-6 were used to measure the secreted cytokine. Supernatants of DCs were collected on day 8, and the amounts of secreted cytokines in the supernatants were quantified using commercially available ELISA kits (BD Biosciences, San Diego, CA).
Generation of AGR2-specific CTLs
AGR2-specific CTLs were generated in vitro by stimulation of autologous CD8+ T cells from healthy donors with autologous DCs transduced with AdAGR2. CD8+ T cells stimulated with autologous DCs without transduction was used as a control. Briefly, CD8+ T cells (purity > 90%) were positively isolated using a MACS system (Miltenyi Biotec Inc., Auburn, CA) from the lymphocyte fraction after Percoll isolation. CD8+ T cells (1 × 106) were sensitized by AdAGR2/DCs (1-2 × 105 cells) in 2 ml of medium (RPMI-1640: AIM-V = 1:1) containing 10% FBS and 1% PS. On day 3, 5 ng/ml of rhIL-2 and 10 ng/ml of rhIL-7 (both from PEPROTECH) were added in the medium and the medium was replenished with cytokines every 3 days. On day 10, the CTL lines were re-stimulated with the same DCs. On day 17, the number of AGR2-specific CTLs was analyzed by an IFN-γ ELISPOT kit (BD Biosciences) and the cytolytic activity of CTLs was evaluated by DNA fragmentation and standard 4-h 51Cr release assays.
Enzyme-linked immunosorbent spot (ELISPOT) assay
Detailed methods of the ELISPOT assay have been described previously (Yi et al., 1993). AGR2-positive CRC cell lines (DLD1, HT-29, HCT-8, and DK01) were used as target cells with or without anti-MHC class I mAb (30 µg/ml) for the antigen-specific IFN-γ ELISPOT assay. Nonspecific response was determined by irrelevant Ig blockade. The number of IFN-γ spots was enumerated by an automatic CTL immunospot® analyzer (Cellular Technology, LTD., Shaker Heights, OH). All samples were run in triplicate. Data are expressed as the mean number of IFN-γ-secreting cells ±SD per 105 CD8+ T cells.
DNA fragmentation assay (JAM assay)
The JAM assay was performed as described previously (Matzinger, 1991). Briefly, target cells (HCT-8) were labeled with [3H] thymidine for 4 h at a final concentration of 5 µCi/ml at 106 cells, washed, and plated into wells that contain CTLs (E:T ratio of 20:1). After co-culture for 8 h, cells were harvested onto glass fiber filter mats using a TOMTEC plate harvester (TOMTEC, Inc., Hamden, CT). Data are expressed as a percentage of DNA fragmentation based on the percentage decrease in counts per minute (cpm) as compared with untreated controls using the following formula: (% DNA fragmentation = [control cpm - sample cpm/control cpm] ×100; control and sample mean labeled target cells alone and labeled target cells plus CTLs, respectively).
51Cr-release cytotoxicity assay
The standard 4-h 51Cr-release assay was performed to measure cytolytic activity of the T cells with target cells, including AGR2-positive CRC cell lines (HCT-8 and DLD1). Target cells were incubated with 100 µCi of 51Cr-sodium chromate for 1 h, washed extensively, seeded (1 × 104 cells/well) into 96-well U-bottomed plates in T-cell medium, and co-cultured for 4 h with various numbers of T cells (E:T ratios of 50:1, 25:1, and 12.5:1). All assays were performed in triplicates. Results are expressed as the mean percentage of 51Cr-release calculated as follows: ([experimental release-spontaneous release] / [maximum release-spontaneous release]) ×100%. Maximum release was determined after adding 100 µl of 2% Triton X-100 solution to the targets and spontaneous release, which was always < 20% after incubating targets without effectors. Nonspecific response was determined by irrelevant Ig blockade. To determine whether or not the cytolytic activity was restricted by MHC class I molecules, 30 µg/ml of mAb against HLA-ABC (W6/32) were added to the cultures at the start of the assay.
Statistical analysis
All statistical analyses were performed with SPSS 13.0 for Windows. The Mann-Whitney U test was performed to analyze the statistical significance of non-parametric differences between the groups. P < 0.05 was considered statistically significant.
Acknowledgements
This study was financially supported by a grant of the Korea Healthcare technology R&D Project (A080489), Ministry of Health and Welfare; by General Researcher Program Type II (2011-0005285) of the National Research Foundation of Korea; from the Regional Technology Innovation Program (RTI05-01-01) of the Ministry of Commerce, Industry and Energy; from the Regional Industrial Technology Development Program (A000200058) of the Ministry of Knowledge and Economy; from the National R&D Program (1120390) for Cancer Control, Ministry for Health and Welfare; from Leading Foreign Research Institute Recruitment Program (2011-0030034) through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (MEST), Republic of Korea.
Abbreviations
- Ad
adenovirus
- AGR2
anterior gradient-2
- CEA
carcinoembryonic antigen
- CRC
colorectal cancer
- DC
dendritic cell
- MOI
multiplicity of infection
- TAA
tumor-associated antigen
References
- 1.Aberger F, Weidinger G, Grunz H, Richter K. Anterior specification of embryonic ectoderm: the role of the Xenopus cement gland-specific gene XAG-2. Mech Dev. 1998;72:115–130. doi: 10.1016/s0925-4773(98)00021-5. [DOI] [PubMed] [Google Scholar]
- 2.Aicher A, Westermann J, Cayeux S, Willimsky G, Daemen K, Blankenstein T, et al. Successful retroviral mediated transduction of a reporter gene in human dendritic cells: feasibility of therapy with gene-modified antigen presenting cells. Exp Hematol. 1997;25:39–44. [PubMed] [Google Scholar]
- 3.Ashley DM, Faiola B, Nair S, Hale LP, Bigner DD, Gilboa E. Bone marrow-generated dendritic cells pulsed with tumor extracts or tumor RNA induce antitumor immunity againstcentral nervous system tumors. J Exp Med. 1997;186:1177–1182. doi: 10.1084/jem.186.7.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banchereau J, Palucka AK. Dendritic cells as therapeutic vaccines against cancer. Nat Rev Immunol. 2005;5:296–306. doi: 10.1038/nri1592. [DOI] [PubMed] [Google Scholar]
- 5.Benihoud K, Yeh P, Perricaudet M. Adenovirus vectors for gene delivery. Curr Opin Biotechnol. 1999;10:440–447. doi: 10.1016/s0958-1669(99)00007-5. [DOI] [PubMed] [Google Scholar]
- 6.Di Nicola M, Siena S, Bregni M, Longoni P, Magni M, Milanesi M, et al. Gene transfer into human dendritic antigen-presenting cells by vaccinia virus and adenovirus vectors. Cancer Gene Ther. 1998;5:350–356. [PubMed] [Google Scholar]
- 7.Eloit M, Gilardi-Hebenstreit P, Toma B, Perricaudet M. Construction of a defective adenovirus vector expressing the pseudorabies virus glycoprotein gp50 and its use as a live vaccine. J Gen Virol. 1990;71:2425–2431. doi: 10.1099/0022-1317-71-10-2425. [DOI] [PubMed] [Google Scholar]
- 8.Gong J, Chen L, Chen D, Kashiwaba M, Manome Y, Tanaka T, et al. Induction of antigen-specific antitumor immunity with adenovirus-transduced dendritic cells. Gene Ther. 1997;4:1023–1028. doi: 10.1038/sj.gt.3300496. [DOI] [PubMed] [Google Scholar]
- 9.Hao Y, Triadafilopoulos G, Sahbaie P, Young HS, Omary MB, Lowe AW. Gene expression profiling reveals stromal genes expressed in common between Barrett's esophagus and adenocarcinoma. Gastroenterology. 2006;131:925–933. doi: 10.1053/j.gastro.2006.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hirschowitz EA, Weaver JD, Hidalgo GE, Doherty DE. Murine dendritic cells infected with adenovirus vectors show signs of activation. Gene Ther. 2000;7:1112–1120. doi: 10.1038/sj.gt.3301210. [DOI] [PubMed] [Google Scholar]
- 11.Liu D, Rudland PS, Sibson DR, Platt-Higgins A, Barraclough R. Human homologue of cement gland protein, a novel metastasis inducer associated with breast carcinomas. Cancer Res. 2005;65:3796–3805. doi: 10.1158/0008-5472.CAN-04-3823. [DOI] [PubMed] [Google Scholar]
- 12.Matzinger P. The JAM test. A simple assay for DNA fragmentation and cell death. J Immunol Methods. 1991;145:185–192. doi: 10.1016/0022-1759(91)90325-a. [DOI] [PubMed] [Google Scholar]
- 13.Mayordomo JI, Zorina T, Storkus WJ, Zitvogel L, Celluzzi C, Falo LD, et al. Bone marrow-derived dendritic cells pulsed with synthetic tumour peptides elicit protective and therapeutic antitumour immunity. Nat Med. 1995;1:1297–1302. doi: 10.1038/nm1295-1297. [DOI] [PubMed] [Google Scholar]
- 14.Melief CJ, Van Der Burg SH, Toes RE, Ossendorp F, Offringa R. Effective therapeutic anticancer vaccines based on precision guiding of cytolytic T lymphocytes. Immunol Rev. 2002;188:177–182. doi: 10.1034/j.1600-065x.2002.18816.x. [DOI] [PubMed] [Google Scholar]
- 15.Muthuswamy R, Urban J, Lee JJ, Reinhart TA, Bartlett D, Kalinski P. Ability of mature dendritic cells to interact with regulatory T cells is imprinted during maturation. Cancer Res. 2008;68:5972–5978. doi: 10.1158/0008-5472.CAN-07-6818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakamura M, Iwahashi M, Nakamori M, Ueda K, Ojima T, Naka T, et al. Dendritic cells transduced with tumor-associated antigen gene elicit potent therapeutic antitumor immunity: comparison with immunodominant peptidepulsed DCs. Oncology. 2005;68:163–170. doi: 10.1159/000086770. [DOI] [PubMed] [Google Scholar]
- 17.Nestle FO, Alijagic S, Gilliet M, Sun Y, Grabbe S, Dummer R, et al. Vaccination of melanoma patients with peptide- or tumor lysate-pulsed dendritic cells. Nat Med. 1998;4:328–332. doi: 10.1038/nm0398-328. [DOI] [PubMed] [Google Scholar]
- 18.Oh ST, Kim CH, Park MY, Won EH, Sohn HJ, Cho HI, et al. Dendritic cells transduced with recombinant adenoviruses induce more efficient anti-tumor immunity than dendritic cells pulsed with peptide. Vaccine. 2006;24:2860–2868. doi: 10.1016/j.vaccine.2005.12.056. [DOI] [PubMed] [Google Scholar]
- 19.Parmiani G, De Filippo A, Novellino L, Castelli C. Unique human tumor antigens: immunobiology and use in clinical trials. J Immunol. 2007;178:1975–1979. doi: 10.4049/jimmunol.178.4.1975. [DOI] [PubMed] [Google Scholar]
- 20.Ramachandran V, Arumugam T, Wang H, Logsdon CD. Anterior gradient 2 is expressed and secreted during the development of pancreatic cancer and promotes cancer cell survival. Cancer Res. 2008;68:7811–7818. doi: 10.1158/0008-5472.CAN-08-1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rea D, Schagen FH, Hoeben RC, Mehtali M, Havenga MJ, Toes RE, et al. Adenoviruses activate human dendritic cells without polarization toward a T-helper type 1-inducing subset. J Virol. 1999;73:10245–10253. doi: 10.1128/jvi.73.12.10245-10253.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenberg SA. Cancer vaccines based on the identification of genes encoding cancer regression antigens. Immunol Today. 1997;18:175–182. doi: 10.1016/s0167-5699(97)84664-6. [DOI] [PubMed] [Google Scholar]
- 23.Song W, Kong HL, Carpenter H, Torii H, Granstein R, Rafii S, et al. Dendritic cells genetically modified with an adenovirus vector encoding the cDNA for a model antigen induce protective and therapeutic antitumor immunity. J Exp Med. 1997;186:1247–1256. doi: 10.1084/jem.186.8.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thompson JA, Grunert F, Zimmermann W. Carcinoembryonic antigen gene family: molecular biology and clinical perspectives. J Clin Lab Anal. 1991;5:344–366. doi: 10.1002/jcla.1860050510. [DOI] [PubMed] [Google Scholar]
- 25.Valladares-Ayerbes M, Diaz-Prado S, Reboredo M, Medina V, Iglesias-Diaz P, Lorenzo-Patino MJ, et al. Bioinformatics approach to mRNA markers discovery for detection of circulating tumor cells in patients with gastrointestinal cancer. Cancer Detect Prev. 2008;32:236–250. doi: 10.1016/j.cdp.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Yi Q, Bergenbrant S, Osterborg A, Osby E, Ostman R, Bjorkholm M, et al. T-cell stimulation induced by idiotypes on monoclonal immunoglobulins in patients with monoclonal gammopathies. Scand J Immunol. 1993;38:529–534. doi: 10.1111/j.1365-3083.1993.tb03236.x. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y, Forootan SS, Liu D, Barraclough R, Foster CS, Rudland PS, et al. Increased expression of anterior gradient-2 is significantly associated with poor survival of prostate cancer patients. Prostate Cancer Prostatic Dis. 2007;10:293–300. doi: 10.1038/sj.pcan.4500960. [DOI] [PubMed] [Google Scholar]
- 28.Zhong L, Granelli-Piperno A, Choi Y, Steinman RM. Recombinant adenovirus is an efficient and non-perturbing genetic vector for human dendritic cells. Eur J Immunol. 1999;29:964–972. doi: 10.1002/(SICI)1521-4141(199903)29:03<964::AID-IMMU964>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]