Abstract
Objectives
To explore the prevalence and characteristics associated with college students who misuse their prescribed stimulants for attention-deficit hyperactivity disorder (ADHD) and examine diversion and substance use behaviors as a function of misuse.
Methods
Cohort of 55 past-year prescribed stimulant users was identified from a random sample (n = 1738) at a large Midwestern research university following the self-administration of a web-based survey. An index was created to assess misuse of prescribed stimulants (i.e., Misuse Index).
Results
Of 55 college students who reported past-year use of prescribed stimulants for ADHD, 22 (40%) endorsed at least one item on the misuse index. The most frequently endorsed misuse items were used too much (36%), self-reported misuse (19%), and intentionally used with alcohol or other drugs (19%). Misusers of prescribed stimulant medication were more likely to report cigarette smoking (p = 0.022), binge drinking (p = 0.022), illicit use of cocaine (p = 0.032), and screen positive on the Drug Abuse Screening test (DAST-10) criteria (p = 0.002). The bivariate odds ratio for the DAST-10 findings was 8.4 (95% CI: 2.0–34.6). Diversion of prescribed stimulants was common (36%) and occurred more frequently among stimulant misusers (57%; p = 0.008).
Conclusion
There is a strong relationship between misuse of prescribed stimulants for ADHD and substance use behaviors, as well as other deleterious behaviors such as diversion. These findings suggest the need for close screening, assessment, and therapeutic monitoring of medication use in the college population.
Keywords: attention-deficit hyperactivity disorder, medication, stimulant, misuse, diversion, amphetamine
Introduction
Prescription stimulants are the most commonly prescribed medications for the treatment of attention-deficit hyperactivity disorder (ADHD),1 a behavioral condition that affects approximately 2% to 8% of college students in the United States.2 Over the past decade, there has been an increase in the rate of prescribing stimulants used to treat ADHD.3–5 This upward trend may be attributed to broader diagnostic criteria for symptoms of ADHD, prolonged duration of treatment,6–8 and awareness of the continuation of the disorder into adulthood.9 Although evidence-based medicine supports the safety and efficacy of prescription stimulants for the treatment of ADHD,10,11 controversy centers on the increased access to these agents, their abuse potential,1 and the likelihood of their nonmedical use and diversion, specifically among college students.12 For the purpose of this study, nonmedical use refers to the use of a psychostimulant medication without a prescription, while misuse (which will be explicitly defined below) refers to the inappropriate use of a stimulant medication that was initially prescribed for the treatment of ADHD.
Several college-based studies have extensively documented the prevalence of nonmedical use of prescription stimulants.12–18 For example, in a random sample of 4580 students at a Midwestern university, 5.9% of undergraduate college students self-reported past-year nonmedical use of prescription stimulants (eg, Ritalin, Dexedrine, Adderall, Concerta, and methylphenidate).17 Further, data from the College Alcohol Study (CAS) found the past-year prevalence rates of nonmedical use of prescription stimulants (Ritalin, Dexedrine, or Adderall) in a nationally representative sample of US colleges ranged from 0% to 25%.12 It is evident that the rates of nonmedical use of prescription stimulants continue to be a matter of public health concern.
Studies have identified several demographic characteristics associated with nonmedical prescription stimulant use among college students, including being male, white, Jewish, and reporting fraternity or sorority affiliation.12,18,19 Furthermore, college students who endorse nonmedical use of prescription stimulants are more likely to use alcohol and other drugs (AODs) compared to college students who deny the nonmedical use of these agents.12,15 Of particular interest, previous data suggest the motives behind the nonmedical use of prescription stimulants among college students are to improve concentration, increase alertness and energy, attain euphoria, and as a study aid.13,16,17,20 The aforementioned motives are strongly associated with academic performance, which may help explain an observed decline in the prevalence of nonmedical use of prescription stimulants after the traditional college age of 18 to 24 years.13,14
Another concerning phenomenon that has been described in the literature is the diversion of prescription stimulants used for the treatment of ADHD, which may facilitate access to these medications for those without a prescription (i.e., nonmedical use).18 Among college students who are treated with prescription stimulants for ADHD, a majority (54%) are approached to sell, trade, or give away their medication each year.18 However, little is known about the prevalence of actual diversion among college students who are prescribed stimulants for ADHD after they are approached to sell, trade, or give them away. What is known regarding diversion, among those using these medications nonmedically is that the most frequently reported channel of diversion is friends and peers.18,21 For instance, among nonmedical users who specified a source, 92% indicated obtaining prescription stimulants from friend and peer sources.18
To our knowledge, there is a scarcity of studies that have evaluated the prevalence of diversion among college-aged youth from those who are prescribed a stimulant medication.22–24 These studies utilized different methodologies but provide valuable information concerning the diversion of prescription stimulants. The first study found that 29% of college students treated for ADHD with prescription stimulants (n = 76) reported having ever sold or given away their medication.22 The second study evaluated a clinical sample of subjects (mean age 20.8 years) with ADHD (n = 55) and found that 11% of patients had sold their prescribed stimulant medication within a 4-year period.23 Utilizing face-to-face interviews with college students, the third study identified a larger percentage of students (61.7%) who had diverted their ADHD medication.24 Despite a range of findings, these studies suggest that some individuals who have a prescription for a stimulant medication for ADHD are not using them as prescribed by their clinician.
Although limited, information exists describing the misuse of prescribed stimulants for ADHD.22,23,25–29 For instance, Upadhyaya et al evaluated a convenience sample of 344 college students and revealed that 25% of the respondents used their own prescription stimulants for ADHD to “get high.”22 However, this study may underestimate the true prevalence of this behavior as other types of misuse have also been described. For example, Wilens et al assessed multiple types of misuse and reported that within a clinical sample of ADHD subjects (n = 55), 22% misused or took too much of their prescribed stimulants, 10% “got high” on their prescribed stimulants, and 31% used their prescription stimulants with alcohol or other drugs.23 Although these studies have provided important insight into the misuse of stimulant medication among those with ADHD, no studies have examined the various forms of misuse of prescribed stimulants (ie, occurring when an individual misuses the ADHD stimulant that was prescribed to them) using a probability sample in order to assess the magnitude of this problem.
Not surprisingly, this preliminary literature corroborates why physicians are concerned with the potential for misuse and diversion of prescribed stimulants for ADHD when evaluating and treating their patients.30 From a clinical perspective, it would be beneficial for prescribers to be able to identify specific patient characteristics associated with the inappropriate use of prescription stimulants used for the treatment of ADHD. For example, in the study by Wilens et al, a relationship between ADHD subjects who misused their prescribed stimulants and the presence of a comorbid substance use disorder (SUD) was found. More precisely, 75% of the participants who misused their prescribed stimulants had a comorbid SUD.23
Lastly, using survey-based research, our team has been able to identify aberrant drug-taking behaviors associated with college students who are prescribed stimulant medication for ADHD.19 A subgroup of college students (approximately 31% of prescribed users) was identified who reported both the prescribed and nonmedical use of prescription stimulants.19 While this finding does not provide data regarding the misuse of prescribed stimulants, it reinforces the need for additional investigation into patterns of stimulant medication use, misuse, and nonmedical use among college students.
During examination of the large probability sample collected during the 2007 Student Life Survey (SLS; see Methods for a description of the SLS), a subgroup of college students was identified who self-reported the past-year misuse of prescribed stimulants for ADHD. Consequently, this exploratory study will attempt to characterize these individuals in order to gain a more complete understanding of behaviors relating to the misuse of prescribed stimulants. Furthermore, it has become apparent in the literature that the nonmedical use of prescription stimulants is strongly associated with AOD use.12 Therefore, we examined whether these same associations hold true among college students who misuse their prescribed stimulant medication.
Misuse by an individual was specifically defined for this study as any of the following behaviors as they relate to their prescribed stimulants for ADHD: (1) used too much and/or (2) intentionally used them with alcohol or other drugs and/or (3) self-reported “misuse” and/or (4) intentionally got high. Therefore, our primary objective was to assess the prevalence and characteristics (including substance use behaviors) associated with college students who misuse their prescribed stimulants for ADHD, and our secondary objective was to examine stimulant medication diversion as it relates to misuse.
Methods
Design
After receiving Institutional Review Board approval, this study was conducted drawing on a total undergraduate population of over 24 000 full-time students attending a large public research university located in the United States. In 2007, a simple random sample of 4000 full-time undergraduate students was obtained from this population. The entire sample was mailed a prenotification letter describing the study and inviting students to self-administer a Web survey by using a URL address and unique password. Informed consent was obtained online from each participant. Nonrespondents were sent reminder emails. The Web survey was maintained on an Internet site running under the secure socket layer protocol to ensure privacy and security. All potential respondents were sent a small monetary incentive and could elect to be entered into a sweepstakes that included cash and other prizes.
Instrument and Measures
The Student Life Survey (SLS) was originally developed at the University of Michigan Substance Abuse Research Center and pilot tested in 1993 and 1999. The SLS was constructed using items that were included in several national studies of AOD use.14,31,32 Detailed information regarding reliability and validity of the SLS measures are described elsewhere.33,34 Demographic measures included the following items: gender, race/ethnicity, and class year (Table 1).
Table 1.
Demographic Characteristics According to Prescribed Stimulant Use for attention-deficit hyperactivity disorder (ADHD)
| Past-year nonusers (n = 1600) N (%) |
Past-year non-misusers (n = 33) N (%) |
Past-year misusers (n = 22) N (%) |
|
|---|---|---|---|
| Gender | |||
| Women | 905 (56.6) | 15 (45.5) | 7 (31.8) |
| Men | 695 (43.4) | 18 (54.5) | 15 (68.2) |
| Race/ethnicity | |||
| White | 1071 (66.9) | 24 (72.7) | 16 (72.7) |
| African | 86 (5.4) | 2 (6.1) | 1 (4.5) |
| American | |||
| Asian | 209 (13.1) | 5 (15.2) | 3 (13.6) |
| Hispanic | 70 (4.4) | 1 (3.0) | 1 (4.5) |
| Other | 164 (10.3) | 1 (3.0) | 1 (4.5) |
| Class year | |||
| Freshman | 431 (26.9) | 7 (21.2) | 4 (18.2) |
| Sophomore | 409 (25.6) | 6 (18.2) | 5 (22.7) |
| Junior | 400 (25.0) | 12 (36.4) | 9 (40.9) |
| Senior | 340 (21.3) | 8 (24.2) | 4 (18.2) |
| Other | 20 (1.2) | 0 (0.0) | 0 (0.0) |
Use of prescribed stimulant medication for the treatment of ADHD was measured using the following survey items: “Based on a doctor’s prescription, on how many occasions in your lifetime have you used the following types of drugs?” “Stimulant medication for ADHD (eg, Ritalin®, Dexedrine®, Adderall®, Concerta®, methylphenidate)” was specified as 1 of 7 prescription drug categories. The response scale was (1) never, (2) 1–2 occasions, (3) 3–5 occasions, (4) 6–9 occasions, (5) 10–19 occasions, (6) 20–39 occasions, (7) 40 or more occasions, and (8) rather not say. If respondents indicated they were prescribed a stimulant medication for ADHD in their lifetime, they were then asked the same question in regard to their use of prescribed stimulants in the past 12 months. Of note, the remaining survey items listed below were given only to those respondents who indicated having ever used a prescribed stimulant in their lifetime (ie, skip-logic).
Specific formulation use of prescribed stimulants for the treatment of ADHD was assessed by the following item: “Please indicate if any of the following stimulant medications for ADHD have been prescribed to you in the past 12 months … select all that apply:” Please refer to Table 2 for a complete list of prescribed stimulant formulations included in the survey. The specific order in which the formulations appeared to each respondent was randomized in order to reduce survey selection bias. For analysis purposes, the responses were categorized based on short-/intermediate-acting (3–8 hours) and long-acting (8–12 hours) pharmacokinetic properties of each formulation.35 For analyses related to the specific formulations of prescription stimulants, those respondents who self-reported taking multiple medications (n = 10) within the past year were excluded in order to prevent confounding results.
Table 2.
Past-Year Prevalence of Specific Formulations of Prescribed Stimulant Medication for attention-deficit hyperactivity disorder (ADHD)a
| Prescribed Users (n = 55)b N (%) |
Non-Misusers (n = 33)b N (%) |
Misusers (n = 22)b N (%) |
Single-Agent Misusers (n = 16)c N (%) |
|
|---|---|---|---|---|
| Adderall | 19 (34.5) | 9 (27.3) | 10 (45.5) | 7 (43.8) |
| Adderall XR | 17 (30.9) | 9 (27.3) | 8 (36.4) | 4 (25.0) |
| Concerta | 13 (23.6) | 7 (21.2) | 6 (27.3) | 2 (12.5) |
| Methylphenidate | 4 (7.3) | 2 (6.1) | 2 (9.1) | 2 (12.5) |
| Ritalin | 2 (3.6) | 1 (3) | 1 (4.5) | 1 (6.2) |
| Ritalin LA | 2 (3.6) | 1 (3) | 1 (4.5) | – |
| Focalin XR | 2 (3.6) | 1 (3) | 1 (4.5) | – |
| Ritalin SR | 1 (1.8) | 0 (0) | 1 (4.5) | – |
| Metadate ER | 1 (1.8) | 0 (0) | 1 (4.5) | – |
| Methylin | 1 (1.9) | 1 (3) | 0 (0) | – |
| Daytrana | 1 (1.8) | 0 (0) | 1 (4.5) | – |
The following formulations were not endorsed by any of the respondents: methylphenidate extended release, Metadate CD, Methylin ER, Focalin, amphetamine/dextroamphetamine combination, dextroamphetamine, dextroamphetamine extended release, Dexedrine, Dexedrine Spansules, Dextrostat.
Specific formulations not mutually exclusive; percentages do not equal 100%.
Specific formulations are mutually exclusive; percentages equal 100%.
Misuse of prescribed stimulants for the treatment of ADHD was assessed by using a questionnaire adapted from Wilens et al.23 The following items were included: “On how many occasions (if any) in the past 12 months have you … (a) Used too much (eg, higher doses, more frequent doses) of your prescribed stimulant medication for ADHD? (b) Intentionally gotten high on your prescribed stimulant medication for ADHD? (c) Misused your prescribed stimulant medication for ADHD? (d) Intentionally used your prescribed stimulant medication for ADHD with alcohol or other drugs?” The response scale was the same as for the use of prescribed stimulant medication. A Misuse Index was created by an affirmative response to any one of the above items and respondents were then classified as prescribed stimulant misusers or non-misusers.
Diversion of prescribed stimulants for the treatment of ADHD was assessed by asking the following question: “On how many occasions (if any) in the past 12 months have you given away, loaned, or sold your prescribed stimulant medication for ADHD to someone?” The response scale was the same as for the use of prescribed stimulant medication.
Age at initiation of use of prescribed stimulants for the treatment of ADHD was assessed by asking the question, “Based on a doctor’s prescription, when did you first start using each prescription drug?” “Stimulant medication for ADHD (e.g., Ritalin, Dexedrine, Adderall, Concerta, methylphenidate)” was specified as 1 of the 7 prescription drug categories given and its response scale was as follows: (1) grades K-4, (2) grades 5–6, (3) grades 7–8, (4) grades 9–10, (5) grades 11–12, (6) college, and (7) rather not say.
Presence of active symptoms associated with ADHD was assessed using the Adult Symptom Rating scale (ASRSv1.1), which is a screening tool for adult ADHD.36 The ASRSv1.1 is a 2-part questionnaire (Part A and Part B) that can be utilized in population-based surveys to estimate the prevalence of adult ADHD. The items from Part A of the ASRSv1.1 are more predictive of ADHD and were used in the current study.36
Cigarette smoking was assessed with the following item: “How many cigarettes have you smoked in the past 30 days?” Response scale ranged from “none” to “2 or more packs per day.” Respondents were categorized as past 30-day smokers if they endorsed any cigarette use.
Binge drinking was assessed by asking students “What is the greatest number of drinks you consumed in a 2-hour period during the past 2 weeks?” A drink was defined as a glass of wine, a bottle of beer or wine cooler, a shot of liquor straight or in a mixed drink. Based on the definition advanced by the National Institute on Alcohol Abuse and Alcoholism Advisory Council, participants were classified as “past 2-week binge drinkers” if they reported consuming 5 or more drinks (male) or 4 or more drinks (female) at least 1 time in a 2-hour period during the past 2 weeks.
Alcohol abuse was assessed using a modified version of the standard Cut Down, Annoyance, Guilt, Eye-opener (CAGE) screening instrument.37 A positive response to 2 or more of the CAGE criteria in the past year was a proxy for suspected alcohol abuse.38,39
Adverse consequences of drinking included a variety of items assessing negative effects of alcohol consumption as well as criteria from the CAGE instrument. Respondents were provided with the following question: “Please indicate how often during the past 12 months you have experienced the following as a result of drinking.” A list of items was provided (eg, performed poorly on a test or important project, missed a class or work due to drinking, driven a car while under the influence of alcohol). The response scale was the same as for the use of prescribed stimulant medication. If college students self-reported experiencing 5 or more of the above consequences criteria, they were classified as screening positive for adverse consequences of drinking.
Illicit drug use was assessed with the following question: “On how many occasions in the past 12 months have you used the following types of drugs? Do not include drugs used under a doctor’s prescription.” A list of illicit substances (eg, marijuana, cocaine, LSD, etc) was provided. The response scale was the same as the use of prescribed stimulant medication.
Drug abuse-related problems were evaluated using the Drug Abuse Screening Test, Short Form (DAST-10), which screens for potential abuse of and dependence on multiple substances other than alcohol.40 An affirmative response to 3 or more of the DAST-10 criteria indicated potential drug abuse problems.
Data Analysis
Prevalence rates of prescribed stimulant use and misuse across subgroups were calculated by dividing the number of students reporting an outcome behavior by the total number of respondents to that question. Bivariate associations were tested using chi-square analyses, using SPSS statistical software. Bivariate odds ratios with 95% confidence intervals were conducted to examine the magnitude of effects where appropriate. Given the small size of the subgroups of interest, multivariate analyses were not performed and our findings should be considered preliminary.
Results
Sample
The overall response rate was 43.5%. The total sample included 1738 undergraduate college students whose mean age was 20.8 (standard deviation [SD] = 1.8) years. The subgroup of past-year prescribed stimulant users that are the focus of this study closely resembles the total sample demographics. Although there was a higher prevalence of males among past-year misusers as compared to non-misusers, baseline demographics (eg, age, race/ethnicity, gender, class standing) did not reach statistical significance (Table 1).
Use of Prescribed Stimulant Medication for the Treatment of ADHD
Based on a doctor’s prescription, approximately 4.8% (n = 80) of undergraduate college students who responded to the survey reported use of prescription stimulants for ADHD at least once in their lifetime. Of these lifetime users, 55 reported the use of these medications in the past year, 10 of which reported having used multiple prescribed stimulants. As shown in Table 2, the most commonly prescribed stimulant medications were the short-/intermediate-acting formulation Adderall and the long-acting formulations Adderall XR and Concerta.
Misuse of Prescribed Stimulant Medication for the Treatment of ADHD
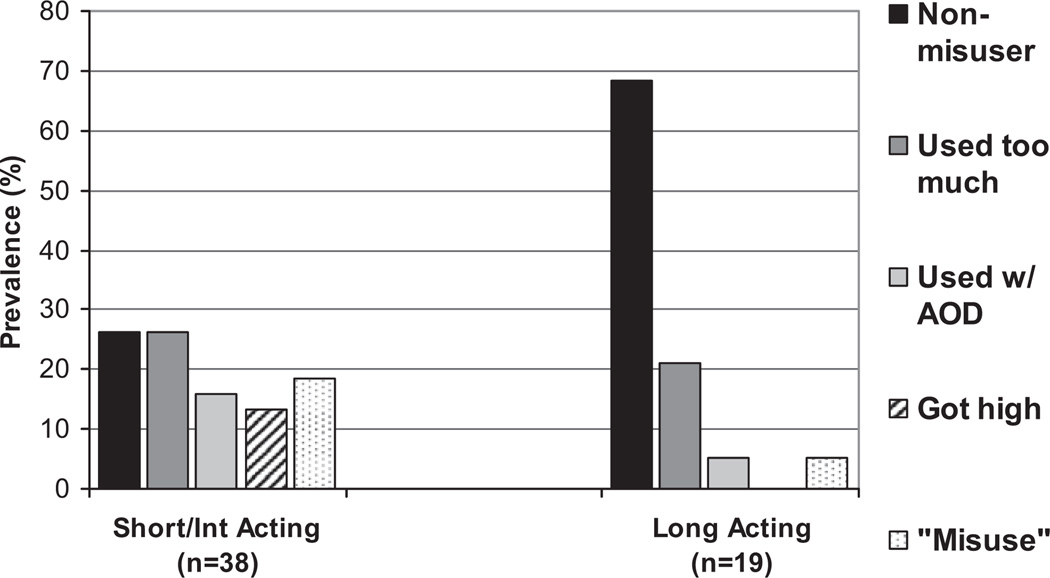
Among survey participants who reported past-year use of prescribed stimulants for ADHD (n = 55), the most frequently reported items of misuse were “used too much” (35.8%) and “self-reported misuse” (19.2%; Table 3). Twenty-two (40%) past-year prescribed stimulant users endorsed at least 1 misuse item, forming our Misuse Index. According to the individual items defining our Misuse Index, short-/intermediate-acting formulations were more likely to be misused compared to long-acting formulations (Figure 1). Most notably, all 5 respondents who endorsed the “got high” misuse item were prescribed a short-/intermediate-acting agent in the past year.
Table 3.
Past-Year Prevalence of Misuse of Prescribed Stimulant Medication for attention-deficit hyperactivity disorder (ADHD)a
| Past-year users of prescribed stimulant medication for ADHD N (%) |
|
|---|---|
| Used too much (eg, higher doses, more frequent doses) of your prescribed stimulant medication for ADHD (n = 53) | 19 (35.8) |
| Intentionally gotten high on your prescribed stimulant medication for ADHD (n = 53) | 5 (9.4) |
| Misused your prescribed stimulant medication for ADHD (n = 52) | 10 (19.2) |
| Intentionally used your prescribed stimulant medication for ADHD with alcohol or other drugs (n = 53) | 10 (18.9) |
| Misuse Index | 22 (40.0) |
Misuse Index includes past-year prescribed stimulant users who endorsed at least one of the misuse items.
Figure 1.
Prevalence of single-agent misuse of prescribed stimulants as a function of pharmacokinetic properties. Short-/intermediate-acting (3–8 hours); long-acting (8–12 hours) pharmacokinetic properties of each formulation.35
Diversion of Prescribed Stimulant Medication for the Treatment of ADHD
Diversion was reported by 36.0% (n = 18) of college students who indicated past-year prescribed use of stimulant medication for the treatment of ADHD (n = 55). Misusers were more likely to divert their prescribed stimulant medication (57.1%) than non-misusers (20.7; P < .01; Table 4). We further evaluated the data to determine whether there were differences between specific formulations being diverted among past-year prescribed stimulant users for ADHD. Of the most frequently prescribed stimulants, Adderall and Adderall XR were the most often diverted (n = 12), while there were no reports of diversion with Concerta.
Table 4.
Clinical Characteristics Associated With Past-Year Use of Prescribed Stimulants for ADHDa
| Non-misusers (n = 33) No. (%) |
Misusers (n = 22) No. (%) |
χ2 | P value | OR | 95% CI | |
|---|---|---|---|---|---|---|
| Past-month cigarette smoking (n = 55) | 8 (24.2) | 12 (54.5) | 5.2b | .022 | 3.7 | 1.2–11.9 |
| Past 2-week binge drinking (n = 55) | 17 (51.5) | 18 (81.8) | 5.2b | .022 | 4.2 | 1.2–15.2 |
| Adverse consequences of drinking (≥5 items; n = 52) | 11 (36.7) | 15 (68.2) | 5.0b | .025 | 3.7 | 1.1–11.8 |
| Past-year CAGE (score ≥ 2; n = 52) | 8 (26.7) | 11 (50) | 3.0 | .084 | 2.7 | 0.9–8.8 |
| Past-year use of marijuana (n = 55) | 23 (71.9) | 20 (90.9) | 2.9 | .088 | 3.9 | 0.7–20.3 |
| Past-year use of cocaine (n = 55) | 5 (15.2) | 9 (40.9) | 4.6b | .032 | 3.9 | 1.1–13.9 |
| Past-year use of other illicit drugs (n = 55) | 3 (9.1) | 7 (31.8) | 4.6b | .032 | 4.7 | 1.1–20.7 |
| Past-year DAST-10 (score ≥ 3; n = 42 drug users only) | 4 (18.2) | 13 (65) | 9.5c | .002 | 8.4 | 2.0–34.6 |
| Age at initiation (n = 55) | 10.0 | .075 | ||||
| K-4 | 4 (12.1) | 2 (9.1) | ||||
| 5–6 | 0 (0) | 2 (9.1) | ||||
| 7–8 | 6 (18.2) | 1 (4.5) | ||||
| 9–10 | 2 (6.1) | 3 (13.6) | ||||
| 11–12 | 10 (30.3) | 2 (9.1) | ||||
| College | 11 (33.3) | 12 (54.5) | ||||
| Presence of active symptoms of ADHD (≥4 symptoms per ASRSv1.1; n = 55) | 13 (39.4) | 13 (59.1) | 2.1 | .152 | 2.2 | 0.7–6.7 |
| Diversion (n = 50) | 6 (20.7) | 12 (57.1) | 7.0c | .008 | 5.1 | 1.5–17.8 |
Abbreviations: ADHD, attention-deficit hyperactivity disorder; DAST, Drug Abuse Screening Test–Short Form; CAGE, Cut Down, Annoyance, Guilt, Eye-opener; ASRS, Adult Symptom Rating scale; K, Kindergarten; OR = bivariate odds ratio, CI = 95% confidence interval.
All analyses in Table 4 are chi-square bivariate analyses. For all chi-square tests, df = 1 except for “age at initiation,” df = 5. Please note that if we applied a Bonferroni correction to the α level, only the group difference on the DAST-10 would remain statistically significant.
P <.05.
P < .01.
Age at Initiation of Prescribed Use of Stimulant Medication for Treatment of ADHD
Undergraduate students who reported past-year misuse of prescribed stimulants were more likely to initiate treatment in college compared to non-misusers (54.5% vs 33.3%, respectively). These differences, however, did not reach statistical significance. A closer look into the 12 college students who reported both misusing their prescribed stimulants and having initiated treatment during college, showed that of the 5 respondents who endorsed the “got high” misuse item, 80% of them were college initiators. Also, 70% (n = 7) of respondents who intentionally used their prescribed stimulant medication with AOD initiated treatment in college.
Presence of Active Symptoms Associated With ADHD
Among the 22 past-year misusers, 59.1% (n = 13) reported active symptoms of ADHD according to the ASRSv1.1. There were no statistically significant differences among misusers and non-misusers in relation to self-reported symptoms of ADHD.
Patterns of Substance Use Among Past-Year Users of Prescribed Stimulant Medication
Bivariate analyses (Table 4) demonstrated that cigarette smoking was more prevalent among past-year prescribed stimulant misusers (P < .05). Similarly, significant associations were noted for higher rates of binge drinking (P < .05) and adverse consequences of alcohol use (P < .05) among misusers. In addition, 1 (50.0%) of every 2 misusers scored positive on the CAGE measure, while less than 1 (26.7%) in every 3 of the non-misusers did the same (P < .10). Results indicated that 90.9% of misusers compared to 71.9% of non-misusers had used marijuana in the past 12 months (P < .10). In addition, 40.9% of misusers (n = 9) compared to 15.2% of non-misusers (n = 5) had used cocaine in the past 12 months (P < .05). Approximately, 31.8% of misusers compared to 9.1% of non-misusers used illicit drugs other than marijuana and cocaine (ie, LSD, other psychedelics, crystal methamphetamine, heroin, inhalants, and ecstasy) in the past 12 months (P < .05). Most notably, analysis on individuals who reported past-year drug use other than alcohol (n = 42) showed that 65% of misusers (n = 13) screened positive for drug abuse or dependence based on 3 or more drug-use-related problems on the DAST-10 questionnaire (P < .01) as compared to 18.2% of non-misusers (n = 4).
Discussion
Our main objective was to define the prevalence of misuse and diversion of prescribed stimulant medication for ADHD among an undergraduate college sample from a university in the United States. Our results revealed that although a majority of past-year users of stimulants for ADHD take these agents as prescribed, 40% of those with prescriptions misuse these medications. This prevalence of misuse concurs with other recent research that has measured misuse of prescribed stimulant medication. These studies have found similar rates of misuse up to approximately 30%.22,23,41 For example, in a more recent study by Rabiner et al, 31% of the students with a current prescription for ADHD medications reported behaviors defined as misuse.41 Our finding suggests that the misuse of prescribed stimulants for ADHD may be occurring more frequently than has been previously described. However, the differences in the prevalence of misuse may be attributed to differences in study design, including sample characteristics (e.g., clinical sample vs probability sample of college students).
To our knowledge, this is the first study to incorporate an individualized list of available brand and generic formulations of prescription stimulants for ADHD and to examine their association with the prevalence of misuse. Our results showed that short-/intermediate-acting prescription stimulants (e.g., Adderall) were more likely to be misused than long-acting agents (e.g., Concerta). However, in order to determine whether this finding is simply due to availability, the motives and routes of administration among misusers with a prescription for specific formulations needs further investigation.
Secondarily, we sought to address the prevalence of diversion among past-year prescribed stimulant users within a college sample. It is evident from our results that the diversion of prescribed stimulants for ADHD is a matter of public concern. Our study showed that the diversion of prescribed stimulants for ADHD occurred more often with the amphetamine–dextroamphetamine formulations Adderall and Adderall XR, which concurs with other recent research.24 This finding is also consistent with the higher demand for amphetamine–dextroamphetamine (eg, Adderall) products for nonmedical use among college students.17 Therefore, it may be possible that the demand for these amphetamine–dextroamphetamine formulations are supplied by users of prescribed stimulants that divert their own medication. We also found that misusers were more likely to divert their prescribed stimulant medication. Ultimately, by addressing the misuse of prescribed stimulants among college students and reducing associated aberrant behaviors such as diversion, it may also be possible to reduce the prevalence of the nonmedical use of these medications.
The present study elucidated several potential characteristics associated with past-year misusers among our college sample. Most notably, our results demonstrated that misusers were more likely to endorse multiple substance use behaviors, which are consistent with previous research that found higher rates of SUD among those with ADHD who misuse their prescription stimulants.23 For instance, our results reveal that past-year misusers were more likely to report past month cigarette use. Given the high rates of active ADHD symptoms among the misusers, it is possible they are self-medicating with nicotine in order to compensate for not taking their medication as prescribed. Past studies have suggested that nicotine improves attention among individuals with ADHD and may serve as a way to alleviate symptoms when they are not effectively treated for their disorder.42–45
Similarly, our results show that past-year alcohol- and illicit drug-related problems were more prevalent among misusers of prescribed stimulant medication for ADHD. For instance, the current study found that misusers not only had higher rates of binge drinking but also met CAGE criteria more often. Of greater concern, the misusers were much more likely to acknowledge past-year cocaine use and to screen positive for drug abuse problems based on the DAST-10 criteria. While it is not clear which behavior preceded the other (i.e., misuse of prescribed stimulants vs other substance use behaviors) based on our current study, there is a definite pattern of higher rates of substance use among misusers and this signal deserves more attention.
Interestingly, over half of the misusers in the current study were college initiators, and previous work has shown that students who initiate treatment of ADHD in college report higher rates of AOD use.46 It is possible that college initiators in our study are contributing to the higher rates of substance use found among the misusers. Furthermore, these findings are consistent with previous research, demonstrating that effective pharmacotherapy for ADHD is protective against later substance use behaviors.47–49 Therefore, a prospective study that examines substance use patterns (including the misuse of prescribed stimulants) among subjects with ADHD who are early initiators versus late initiators is necessary in order to gain a more complete understanding of the present finding.
Based on our previous finding that medical users of prescription stimulants also report concurrent nonmedical use,18 we included this behavior as an additional misuse item in our index (data not shown). Although the overall results did not change, one notable exception was evident: age at initiation became statistically significant (P =.043) as 4 individuals shifted from the non-misuse subgroup to the misuse subgroup. This suggests the age at initiation variable is informative depending on which misuse items are included in the study and whether there are an adequate number of individuals in each subgroup for comparison.
Limitations
Several study limitations should be considered before forming any clinical judgment based on our results. First, our sample included 55 past-year users of prescribed stimulant medication from a larger probability sample assessing AOD use behaviors, which may impact the generalizability of our findings and limits the statistical power of our study. For example, we have observed differences in the nonmedical use of prescription stimulants by geographical region and by school type,12 and similar differences may exist for medical use and misuse as well. Therefore, it is essential to remember that our sample is from a single institution within a single geographic region. Second, some college students did not respond to the survey and may have introduced survey nonresponse bias. However, previous follow-up studies by our research group using similar methodology have shown no significant differences in prevalence rates of alcohol use, binge drinking, cigarette smoking, and other problem health behaviors between college student respondents and nonrespondents. Third, respondents were asked to recall information over a 12-month period for the majority of our outcome variables; therefore, the true prevalence of misuse of prescribed stimulant medication may have been underestimated. Fourth, it is possible that students who are more likely to report “negative” behaviors such as medication misuse are also more likely to report other “negative” behaviors such as alcohol or illicit drug use. Therefore, the relationships between medication misuse and other substance use must be interpreted with some caution. Finally, our Misuse Index was modeled after previous research and has not undergone formal psychometric evaluation. Additional types of misuse such as nonoral routes of administration may be associated with more adverse health consequences and delineates the need for future research in this area.
Conclusions
Clinicians must balance the risks and benefits of medications with abuse potential when assessing, treating, and monitoring their patients. Stimulant medications for the treatment of ADHD have demonstrated a long-standing history of effectiveness when used appropriately; however, they can be misused for a variety of purposes. Furthermore, this medication misuse appears to be related to other problematic behaviors such as diversion and alcohol and drug use. Therefore, in order to help clinicians minimize the misuse of these highly beneficial medications, we have previously proposed steps that can be taken in various clinical settings50:
Periodic screening and assessment can lead to the identification of those at risk for the misuse of prescription medications. Screening and assessment scales may be useful tools in this regard. Knowing who is at risk for misuse is a key step to the safe and effective use of abusable prescription medications.
Given that many individuals obtain diverted prescription medications for nonmedical use from friends, peers, and family members, clinicians prescribing these medications should exercise caution and periodically monitor their patients’ behavior over the course of treatment. They may consider limiting both the quantity of medication prescribed as well as the number of refills, which in turn requires more frequent clinician–patient interactions and therapeutic monitoring. These steps could result in both a reduction in the overall supply of controlled substances available for diversion and nonmedical use and improve the treatment of target symptoms for which the medications were initially prescribed.
Clinicians should be familiar with effective medication alternatives that carry less risk for abuse. Medications that carry less risk for abuse based on their pharmacological profile are available for many conditions. For example, the Food and Drug Administration approved atomoxetine, a nonstimulant norepinephrine reuptake inhibitor (lacking stimulant-like abuse potential) for the treatment of ADHD.
The use of pharmaceutical delivery systems that are not easily manipulated for alternate routes of administration (eg, injection, snorting) might help limit the abuse of some prescription medications. As technology improves, more and more delivery systems will become available that make it difficult to alter each medication’s pharmacokinetic profile (eg, absorption rate), which is key to reducing its abuse potential.
Furthermore, the use of additional aides to help safely and effectively prescribe and monitor medications, such as prescription drug monitoring programs (PDMPs), is appropriate.
In addition to these above steps, targeted prevention efforts need to be employed. For example, it is possible that individuals who divert their medications think they are helping others (eg, self-medicate). However, diversion circumvents the important medication education that accompanies proper treatment, which could lead to harm (eg, drug interactions). Based on the existing literature, we are just beginning to understand the extent of medication diversion. There are no proven methods to deter diversion and this represents an important area for future research.
Prescription stimulants are important tools in the armamentarium against the disabling symptoms of ADHD. The commitment to treat individuals with symptoms of ADHD, and other psychiatric and SUDs, should remain strong, and both clinical and prevention efforts should focus on proper identification and prescribing, therapeutic monitoring, patient education, and prescription monitoring.
Acknowledgments
Portions of earlier versions of this manuscript were presented as two research posters at the College on Problems of Drug Dependence Annual Meeting, June 14–19, 2008, San Juan, Puerto Rico. One of the research posters was invited as a CPDD Primm-Singleton Minority Travel Award (Awardee: Dalissa R. Sepúlveda).
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The development of this article was supported by research grants R01DA031160 and R03DA018239 (PI: Sean Esteban McCabe) and R01DA024678 and T32DA007267 (PI: Carol J. Boyd) from the National Institute on Drug Abuse, National Institutes of Health.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
References
- 1.Greenhill LL, Pliska S, Dulcan MK, et al. American Academy of Child and Adolescent Psychiatry. Practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. J Am Acad Child and Adolescent Psychiatry. 2002;41(2):26S–49S. doi: 10.1097/00004583-200202001-00003. [DOI] [PubMed] [Google Scholar]
- 2.Weyandt LL, DuPaul G. ADHD in college students. J Atten Disord. 2006;10(1):9–19. doi: 10.1177/1087054705286061. [DOI] [PubMed] [Google Scholar]
- 3.Olfson M, Gameroff MJ, Marcus SC, et al. National trends in the treatment of attention deficit hyperactivity disorder. Am J Psychiatry. 2003;160(6):1071–1077. doi: 10.1176/appi.ajp.160.6.1071. [DOI] [PubMed] [Google Scholar]
- 4.Thomas CP, Conrad P, Casler R, et al. Trends in the use of psychotropic medications among adolescents, 1994 to 2001. Psychiatr Serv. 2006;57(1):63–69. doi: 10.1176/appi.ps.57.1.63. [DOI] [PubMed] [Google Scholar]
- 5.Toh S. Trends in ADHD and stimulant use among children, 1993–2003. Psychiatr Serv. 2006;57(8):1091. doi: 10.1176/ps.2006.57.8.1091. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 7.Kelleher KJ, McInerny TK, Gardner WP, et al. Increasing identification of psychosocial problems: 1979–1996. Pediatrics. 2000;105(6):1313–1321. doi: 10.1542/peds.105.6.1313. [DOI] [PubMed] [Google Scholar]
- 8.Safer DJ, Zito ZM, Fine EM. Increased methylphenidate usage for attention deficit disorder in the 1990s. Pediatrics. 1996;98(6):1084–1088. [PubMed] [Google Scholar]
- 9.Wilens TE, Biederman J, Spencer TJ. Pharmacotherapy of attention deficit hyperactivity disorder in adults. CNS Drugs. 1998;5(9):347–356. [Google Scholar]
- 10.Biederman J, Frank AL, Boellner SW, et al. A randomized, double-blind, placebo-controlled, parallel-group study of SLI381 (Adderall XR) in children with attention-deficit/hyperactivity disorder. Pediatrics. 2002;110:258–266. doi: 10.1542/peds.110.2.258. [DOI] [PubMed] [Google Scholar]
- 11.Wolraich ML, Greenhill LL, Pelham W, et al. Randomized, controlled trials of OROS methylphenidate once a day in children with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108:883–892. doi: 10.1542/peds.108.4.883. [DOI] [PubMed] [Google Scholar]
- 12.McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;99:96–106. doi: 10.1111/j.1360-0443.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- 13.Babcock Q, Byrne T. Student perceptions of methylphenidate abuse at a public liberal arts college. J Am Coll Health. 2000;49:143–145. doi: 10.1080/07448480009596296. [DOI] [PubMed] [Google Scholar]
- 14.Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the Future: National Survey Results on Drug Use. Vol 2. Bethesda, MD: National Institute on Drug Abuse; 2006. 1975–2005. college students and adults ages 19–45 (NIH Publication No.06-5884) [Google Scholar]
- 15.Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609–617. doi: 10.1592/phco.23.5.609.34187. [DOI] [PubMed] [Google Scholar]
- 16.Teter CJ, McCabe SE, Cranford JA, et al. Prevalence and motives for illicit use of prescription stimulants in an undergraduate student sample. J Am Coll Health. 2005;53(6):253–262. doi: 10.3200/JACH.53.6.253-262. [DOI] [PubMed] [Google Scholar]
- 17.Teter CJ, McCabe SE, LaGrange K, et al. Illicit use of specific prescription stimulants among college students: prevalence, motives, and routes of administration. Pharmacotherapy. 2006;26(10):1501–1510. doi: 10.1592/phco.26.10.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006a;38(1):43–56. doi: 10.1080/02791072.2006.10399827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use, diversion of abusal prescription drugs. J Am Coll Health. 2006b;54(5):269–278. doi: 10.3200/JACH.54.5.269-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barrett SP, Pihl RO. Oral methylphenidate-alcohol co-abuse. J Clin Psychopharmacol. 2002;22:633–634. doi: 10.1097/00004714-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health; National Findings (Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 06-4194) Rockville, MD: Substance Abuse and Mental Health Services Administration; 2006. [Google Scholar]
- 22.Upadhyaya HP, Rose K, Wang W, et al. Attention-deficit/hyperactivity disorder, medication treatment, and substance use patterns among adolescents and young adults. J Child Adolesc Psychopharmacology. 2005;15(5):799–809. doi: 10.1089/cap.2005.15.799. [DOI] [PubMed] [Google Scholar]
- 23.Wilens TE, Gignac M, Swezey A, et al. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408–414. doi: 10.1097/01.chi.0000199027.68828.b3. [DOI] [PubMed] [Google Scholar]
- 24.Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71:262–269. doi: 10.4088/JCP.09m05189ecr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Corrigall R, Ford T. Methylphenidate euphoria. J Am Acad Child Adolesc Psychiatry. 1996;35:1421. doi: 10.1097/00004583-199611000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Garland EJ. Intranasal abuse of prescribed methylphenidate. J Am Acad Child Adolesc Psychiatry. 1998;37:573–574. doi: 10.1097/00004583-199806000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Goyer PF, Davis GC, Rapoport JL. Abuse of prescribed stimulant medication by a 13-year-old hyperactive boy. J Am Acad Child Adolesc Psychiatry. 1979;18:170–175. doi: 10.1016/s0002-7138(09)60486-6. [DOI] [PubMed] [Google Scholar]
- 28.Jaffe SL. Intranasal abuse of prescribed methylphenidate by an alcohol and drug abusing adolescent with ADHD. J Am Acad Child Adolesc Psychiatry. 1991;30:773–775. [PubMed] [Google Scholar]
- 29.Prudhomme White B, Becker-Blease KA, Grace-Bishop K. Stimulant medication use, misuse, and abuse in an undergraduate and graduate sample. J Am Coll Health. 2006;54(5):261–268. doi: 10.3200/JACH.54.5.261-268. [DOI] [PubMed] [Google Scholar]
- 30.Stockl KM, Hughes TE, Jarrar MA, Secnik K, Perwien AR. Physician perceptions of the use of medications for attention deficit hyperactivity disorder. J Man Care Pharm. 2003;9(5):416–423. doi: 10.18553/jmcp.2003.9.5.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Presley CA, Meilman PW, Cashin JR. Alcohol and Drugs on American College Campuses: Use, Consequences, and Perceptions of the Campus Environment. Volume IV: 1992–94. Carbondale, IL: Core Institute, Southern Illinois University; 1996. [Google Scholar]
- 32.Wechsler H, Oee HE, Kuo M, et al. Trend in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993–2001. Journal Am Coll Health. 2002;50:203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- 33.McCabe SE, Boyd CJ, Couper MP, et al. Mode effects for collecting alcohol and other drug use data: Web and U.S. mail. J Stud Alcohol. 2002b;63:755–761. doi: 10.15288/jsa.2002.63.755. [DOI] [PubMed] [Google Scholar]
- 34.McCabe SE. Comparison of web and mail surveys in collecting illicit drug use data: a randomized experiment. J Drug Educ. 2004;34:61–72. doi: 10.2190/4HEY-VWXL-DVR3-HAKV. [DOI] [PubMed] [Google Scholar]
- 35.Dopheide JA, Tesoro JT, Malkin M. Childhood Disorders in: Pharmacotherapy: a Pathophysiologic Approach. 6th ed. Stamford, CT: Appleton & Lange; 2005. pp. 1133–1145. [Google Scholar]
- 36.Kessler RC, Adler L, Ames M, et al. The world health organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- 37.Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–1123. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- 38.Knight JR, Sherritt L, Harris SK, et al. Validity of brief alcohol screening tests among adolescent medical patients. Pediatrics. 2000;105:948–953. [PubMed] [Google Scholar]
- 39.Knight JR, Goodman E, Pulerwitz T, et al. Reliabilities of short substance abuse screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcohol Clin Exp Res. 2003;27:67–73. doi: 10.1097/01.ALC.0000046598.59317.3A. [DOI] [PubMed] [Google Scholar]
- 40.Skinner H. The drug abuse screening test. Addict Behav. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 41.Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13:144–153. doi: 10.1177/1087054708320414. [DOI] [PubMed] [Google Scholar]
- 42.Gehricke JG, Whalen CK, Jamner LD, et al. The reinforcing effects of nicotine and stimulant medication in the everyday lives of adult smokers with ADHD: A preliminary examination. Nicotine & Tobacco Research. 2006;8(1):37–47. doi: 10.1080/14622200500431619. [DOI] [PubMed] [Google Scholar]
- 43.Kollins SH, McClernon FJ, Fuemmeler BF. Associations between smoking and attention-deficit/hyperactivity disorder symptoms in a population-based sample of young adults. Arch Gen Psychiatry. 2005;65:1142–1147. doi: 10.1001/archpsyc.62.10.1142. [DOI] [PubMed] [Google Scholar]
- 44.Levin ED, Rezvani AH. Development of nicotinic drug therapy for cognitive disorders. European Journal of Pharmacology. 2000;393:141–146. doi: 10.1016/s0014-2999(99)00885-7. [DOI] [PubMed] [Google Scholar]
- 45.Potter AS, Newhouse PA. Effects of acute nicotine administration on behavioral inhibition in adolescents with attention-deficit/hyperactivity disorder. Psychopharmacology. 2004;176:182–194. doi: 10.1007/s00213-004-1874-y. [DOI] [PubMed] [Google Scholar]
- 46.Kaloyanides KB, McCabe SE, Cranford JA, et al. Prevalence of illicit use and abuse of prescription stimulants, alcohol, and other drugs among college students: relationship with age at initiation of prescription stimulants. Pharmacotherapy. 2007;27(5):666–674. doi: 10.1592/phco.27.5.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Biederman J, Wilens TE, Mick E, et al. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics. 1999;104(2):e20. doi: 10.1542/peds.104.2.e20. [DOI] [PubMed] [Google Scholar]
- 48.Barkley RA, Murphy KR. Attention-Deficit/Hyperactivity Disorder: a Clinical Workbook. 2nd ed. New York, NY: Guilford Publications; 1998. [Google Scholar]
- 49.Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179–185. doi: 10.1542/peds.111.1.179. [DOI] [PubMed] [Google Scholar]
- 50.McCabe SE, Cranford JA, Teter CJ, et al. Use, misuse and diversion of scheduled prescription medications by college students. In: White HR, Rabiner D, editors. College Substance Use: Etiology, Consequences and Prevention. Thousand Oaks, CA: SAGE; (In press) [Google Scholar]