Summary
We describe a rare case of traumatic persistent trigeminal artery (PTA) - cavernous sinus fistula. Cerebral angiography showed direct communication between the right PTA and the cavernous sinus which was treated by transcathether arterial embolization. Although previous reports have indicated the use of more coils to treat this condition, we successfully treated the patient with only two coils placed near the orifice of the fistula after sufficient anatomical evaluation.
Key words: trigeminal artery, cavernous sinus fistula, embolization
Introduction
Persistent trigeminal artery (PTA) is the most common carotid-vertebrobasilar anastomosis. A fistula from PTA to the cavernous sinus is a rare condition and only 19 cases have been reported in the literature1,2. Most of the reported cases were treated by endovascular therapy. We describe a case of a traumatic PTA cavernous sinus fistula that was treated successfully with embolization using only two coils by a transarterial approach.
Case Report
A 42-year-old man was admitted to our hospital with severe trauma after falling down nine stairs. Plain head computed tomography (CT) showed subarachnoid hemorrhage, subdural hematoma and brain contusions. After conservative management, he recovered and was discharged to a rehabilitation facility. Two months after the trauma, the patient returned to the hospital with headache, chemosis and proptosis of the right eye. Physical and ophthalmological examinations revealed objective bruit over his right eye with increased intraocular pressure (right 22 mm Hg vs left 17 mm Hg). His visual field and visual acuity were normal. Traumatic carotid artery-cavernous sinus fistula was suspected, and he was readmitted to our hospital.
CT angiography (CTA) demonstrated a distended right cavernous sinus and the dilated right superior ophthalmic vein (SOV) as well as the right sphenoparietal sinus (Figure 1). The cisternal portion of the right PTA directed to the right cavernous sinus was revealed on both CTA and plain magnetic resonance angiography (MRA). CT with multiplanner reconstruction (MPR) also visualized the origins of the right PTA, but the cavernous portion of the PTA was obscured due to an abnormally visualized cavernous sinus on both CTA and MRA.
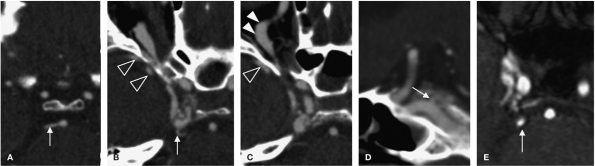
Figure 1.
Axial (A-C) and sagittal (D) views of computed tomography angiography. Axial view of magnetic resonance angiography (E). A-C) The right cavernous sinus is distended. Dilated superior ophthalmic vein (full arrowheads) and sphenoparietal sinus (empty arrowheads) are visualized, indicating drainage veins. A,D) The origin and cisternal portion of the persistent trigeminal artery are indicated (arrows). E) The cisternal portion of the right PTA is indicated by an arrow. The origin of the PTA and fistulous point is obscured.
Cerebral angiography was performed both to diagnose and to treat the fistula. The angiogram of the right internal carotid artery (ICA) revealed a branch originating from the cavernous portion of the right ICA, which communicated with the cavernous sinus posteriorly, draining via the dilated right superior ophthalmic vein, the right sphenoparietal sinus, cortical veins, and the basal vein of Rosenthal. The right inferior petrosal sinus was not dilated. The left vertebral arteriogram revealed the right PTA originating from the basilar artery and filled the fistula in a retrograde fashion (Figure 2). These findings were consistent with a PTA-cavernous sinus fistula. In addition, the bilateral posterior cerebral, bilateral superior cerebellar, and the basilar arteries were normally visualized by the left vertebral arteriogram. Before transarterial embolization, we adjusted an angle of flat panel detector to visualize the fistulous point between the PTA and the cavernous sinus. We inserted a microcatheter via the right ICA into the right cavernous sinus through the fistula. Two GDC vortex coils were placed in the cavernous sinus near the orifice of the fistula. After embolization, the angiogram of the right ICA revealed no residual fistula, with preservation of the right PTA (Figure 3). No neurological complications were encountered during the procedure.
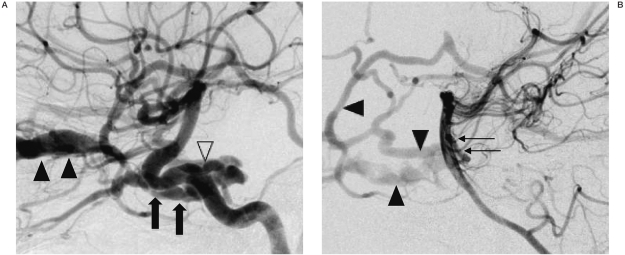
Figure 2.
A) Right internal carotid arteriogram, the cavernous sinus (arrows) and dilated SOV (full arrowheads) are seen in a lateral view, revealing the origin of the PTA (empty arrowhead). B) Left vertebral arteriogram, lateral view, showing the cisternal portion of the PTA (arrows) filling the fistula, indicating the PTA-cavernous sinus fistula. The cavernous sinus and dilated cortical veins (arrowheads) are also shown.
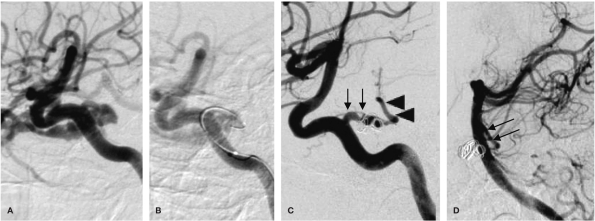
Figure 3.
A,B) Lateral oblique view during transarterial embolization. B) A microcatheter was inserted into the fistula, and the two GDC vortex coils were deployed to occlude the fistula. C) Right internal carotid arteriogram after coiling reveals a complete occlusion of the fistula. There is a connection between the preserved PTA (arrows) and the basilar artery (arrowheads). D) The left vertebral arteriogram shows filling of the PTA (arrows).
CTA and MRA performed two and three days after the procedure respectively, showed no signs of cavernous sinus fistula. However, only the distal portion of the PTA was visualized, indicating an occlusion of the PTA. The symptoms of the patient improved immediately after treatment, and disappeared three months later. There was no clinical evidence of recurrence one year after embolization.
Discussion
The PTA is the most common carotid-vertebrobasilar anastomosis, and its incidence is reported to be 0.1-0.6% in large angiographic series 3. The PTA arises from the cavernous portion of the ICA and runs posterior to the basilar artery. If the PTA is ruptured toward the cavernous sinus, it causes an arteriovenous fistula, and if it is ruptured toward the cistern, it causes subarachnoid hemorrhage. The PTA-carotid sinus fistula is a rare condition, and to the best of our knowledge, there have only been 19 reported cases in the English literature 1,2,4. The etiologies were either post-traumatic, as in our case, or spontaneous. Rupture of a preexisting PTA aneurysm has been reported as a cause of spontaneous PTA-CS fistula 4. In all of the cases, initial symptoms were related to the eye, and one case developed intracranial hemorrhage due to the varix on the draining vein three years after the appearance of diplopia5.
All previous studies, including ours, required cerebral angiography to diagnose this condition. It may be possible to say that the role of CTA and MRA in this condition is limited, only being necessary to detect and depict the anatomical type of PTA.
The goal of treatment is to close the fistula, and generally an endovascular approach is the first choice. Among the previous 19 cases, 16 initially received endovascular treatment, and 15 of these were treated successfully.
The one remaining case was treated by packing of a muslin stripe in the cavernous sinus after the failure of endovascular treatment6. In this case, the authors pointed out a lack of sufficient preoperative evaluation as a cause of treatment failure.
Either a transarterial or transvenous approach can be selected in this condition, depending on the case. For embolization, balloons, coils and liquid adhesive agents have been reported 1. We took a transarterial approach, using only two coils to close the fistula, while between five and 90 coils were used in the reported cases1,7,8. It is possible that the need for fewer coils in our case was due to the precise preoperative anatomical evaluation on the angiography.
Ohshiro et Al found branches from the PTA to supply the pons and trigeminal nerve in an autopsy case. Their finding indicates the possibility of ischemia in the brain stem after occlusion of the PTA9. However, there have been no previous reports of cases with brain stem infarction after occlusion of PTA1. It is therefore generally accepted that preservation is preferable, but that the PTA can be sacrificed if the posterior circulation is independent from the PTA. In our case, postoperative imaging findings indicated an occlusion of the PTA, but there were no symptoms relating to brain stem ischemia.
In conclusion, we were able to treat PTA cavernous fistula with the smallest number of coils by occlusion of the orifice of the fistula.
References
- 1.Geibprasert S, Jiarakonqmun P, et al. Trigeminal fistula treated by combined transvenous and transarterial embolisation. Acta Neurochir (Wien) 2008;150:583–588. doi: 10.1007/s00701-008-1496-3. [DOI] [PubMed] [Google Scholar]
- 2.Yang X, Mu S, et al. Treatment of trauma tictrigeminal cavernous fistula by coil embolization and compression of carotid artery. Neurol India. 2007;55:396–398. doi: 10.4103/0028-3886.37100. [DOI] [PubMed] [Google Scholar]
- 3.Hahnel S, Hartmann M, et al. Persistent hypoglossal artery: MRI, MRA and digital subtraction angiometry. Neuroradiology. 2001;43:767–769. doi: 10.1007/s002340100566. [DOI] [PubMed] [Google Scholar]
- 4.Enomoto T, Sato A, Maki Y. Carotid-cavernous sinus fistula caused by rupture of a primitive trigeminal artery aneurysm. Case report. J Neurosurg. 1977;46:373–376. doi: 10.3171/jns.1977.46.3.0373. [DOI] [PubMed] [Google Scholar]
- 5.Tokunaga K, Sugiu K, et al. Persistent primitive trigeminal artery-cavernous sinus fistula with intracerebral hemorrhage: endovascular treatment using detachable coils in a transarterial double-catheter technique. Case report and review of the literature. J Neurosurg. 2004;101:697–699. doi: 10.3171/jns.2004.101.4.0697. [DOI] [PubMed] [Google Scholar]
- 6.Berger MS, Hosobuchi Y. Cavernous sinus fistula caused by intracavernous rupture of a persistent primitive trigeminal artery. Case report. J Neurosurg. 1984;61:391–395. doi: 10.3171/jns.1984.61.2.0391. [DOI] [PubMed] [Google Scholar]
- 7.Hurst RW, Howard RS, et al. Carotid cavernous fistula associated with persistent trigeminal artery: endovascular treatment using coil embolization. Skull Base Surg. 1998;8:225–228. doi: 10.1055/s-2008-1058188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernstein K, Teitelbaum GP, et al. Coil embolization of a trigeminal-cavernous fistula. Am J Neuroradiol. 1998;19:1953–1954. [PMC free article] [PubMed] [Google Scholar]
- 9.Ohshiro S, Inoue T, et al. Branches of the persistent primitive trigeminal artery--an autopsy case. Neurosurgery. 1993;32:144–148. doi: 10.1227/00006123-199301000-00025. [DOI] [PubMed] [Google Scholar]