Summary
Flow diverting stents are emerging as a treatment option for difficult intracranial aneurysms. Current grading scales for assessment of angio- graphic outcomes following aneurysm treatment do not apply to aneurysms treated by flow diversion. We propose a novel grading scale based on the degree of angiographic filling and contrast stasis. This scale will facilitate communication and standardize reporting of outcomes following flow diversion treatments.
Key words: intracranial aneurysm, stent, grading scale
Introduction
In recent years, parent artery reconstruction with flow diverting stents has emerged as a novel method of repairing certain intracranial aneurysms. Low porosity stents, such as the Pipeline Embolization Device (Chestnut medi- cal/eV3) and the Silk stent (BALT), are deployed across the neck of the aneurysm. These devices function to disrupt aneurysm influx and efflux, diverting blood flow along the course of the reconstructed parent artery. Immediately following the placement of these devices, varying degrees of contrast stasis and aneurysm filling are apparent on angiography. In most cases these aneurysms progressively thrombose over the ensuing six to 12 months, however the rate and extent of the thrombosis are difficult to predict 1,2.
In many ways, flow diversion represents a paradigm shift from the current endovascular (endosaccular) approaches to intracranial an- eurysm treatment. Correspondingly, the initial angiographic evaluation and subsequent monitoring of aneurysm closure are fundamentally different. Angiographic outcomes of conventional aneurysm coiling are generally reported using the three-point scale of Roy and Raymond, where aneurysms are designated as complete occlusion, residual aneurysm, or residual neck 3. Unfortunately, this scale is inadequate for describing aneurysms treated with flow diverting stents. Residual or complete filling of the aneurysm is very common immediately after technically successful flow diversion but is not common after technically successful en- dosaccular treatment. A small neck remnant at follow-up is often accepted as adequate treatment after aneurysm coiling, whereas slight filling of an aneurysm treated with a flow diverting stent may be enough to perpetuate continued mass effect, progressive aneurysm growth and in some cases spontaneous rupture. Finally, a simple assessment of the degree of filling does not take into account the dynamic nature of the contrast stasis and its potential role in predicting aneurysm closure over time. To address these issues, we propose a novel grading scale for the assessment of aneurysms treated with flow diversion. This simple scale accounts for both the amount of aneurysm filling and the degree of contrast stasis seen. We hope this scale will standardize the communication of clinical results with flow diversion. We further anticipate that the simultaneous grading of both filling and stasis will facilitate future research and analysis of flow diverting interventions.
Grading Scale
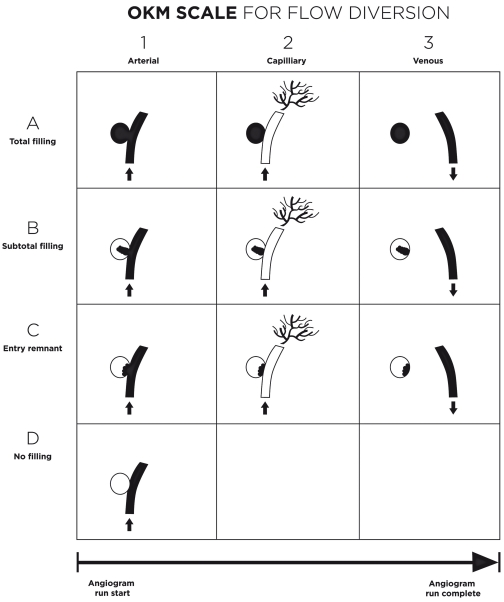
A schematic representation of the grading scale is shown in Figure 1. An angiographic run, extending into the venous phase, is required for determination of the appropriate grade. Two variables are assessed: the volume of contrast filling and the degree of stasis of contrast material. Aneurysm filling is graded as: A - complete (>95%); B - incomplete (5-95%); C - neck remnant (<5%); or D - no filling (0%). The stasis grade is determined by the timing of contrast clearance from the aneurysm sac as defined by the phases of the angiogram: 1 - No stasis (clearance within the arterial phase, prior to the capillary phase); 2 - Moderate stasis (Clearance prior to the venous phase); 3 - Significant stasis (contrast persists in aneurysm into the venous phase and beyond). This creates a total of ten possible grades, with stasis grades coupled to each of the filling grades with the exception of Grade D, no filling. (A1, A2, A3, B1, B2, etc.). Given that many large an- eurysms have stasis on presentation, grades may be assigned to both the pre- and post- treatment angiographic runs. Selected angio- graphic examples of the grading scale are shown in Figures 2 and 3.
Figure 1.
The O'Kelly-Marotta (OKM) grading scale for assessment of aneurysms treated by flow diversion. Each aneurysm is assigned a grade according to the initial degree of filling (A,B,C,D) and the degree of stasis (1,2,3) observed through the angiographic phases (arterial, capillary, venous).
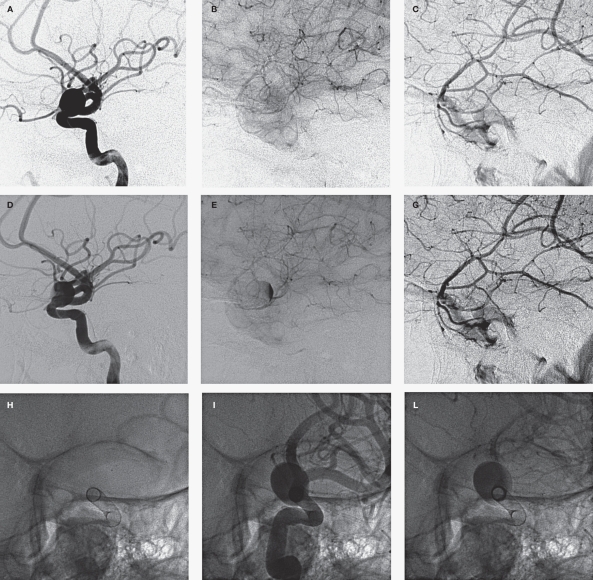
Figure 2.
Selected images of a wide-necked paraophthalmic aneurysm treated with a single flow diverting stent (Pipeline, eV3). The top panel shows the pre-treatment angiogram in the arterial (A), capillary (B) and venous (C) phases. Contrast clears from the aneurysm by the capillary phase (Grade A1). On the post-treatment angiogram (middle panel), the aneurysm continues to fill completely in the arterial phase (D), however contrast lingers into the capillary phase (E), and clears by the venous phase (F) (Grade A2). The subtle stasis is often best appreciated on an oblique projection in line with the long axis of the stent at the level of the aneurysm neck (G). The aneurysm fills completely in the arterial phase (I) but contrast clears from the vessel lumen prior to the aneurysm sac (J).
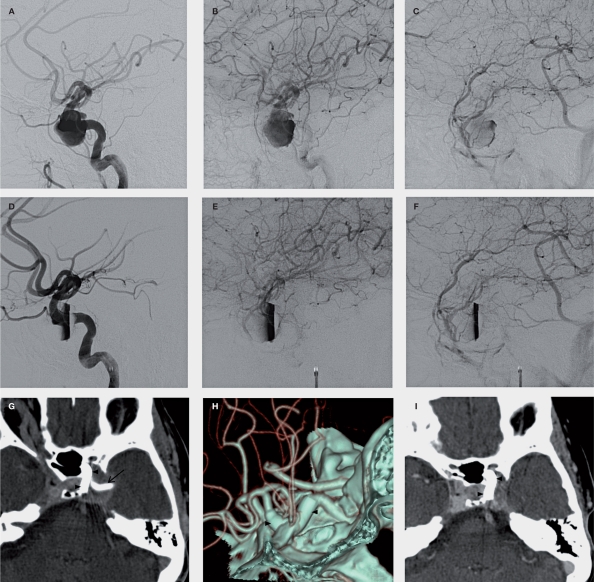
Figure 3.
Pre-treatment, post-treatment and follow-up images of a giant cavernous segment aneurysm treated with a single flow diverting stent (Pipeline, eV3). The top panel shows the pre-treatment angiogram in the arterial (A), capillary (B) and venous (C) phases. The aneurysm fills completely but there is contrast stasis persisting through the venous phase. On the post treatment angiogram (middle panel), there is reduced filling of the aneurysm in the arterial phase (D), with stasis persisting through the capillary (E) and venous phases (F). The reduced filling is also apparent on a CT angiogram performed on postoperative day one (G): the stent is indicated by the arrowheads, filling by the arrow. At 6 months (H,I), the stent (arrowheads) remains in position but there is no filling and the mass effect on the adjacent temporal lobe has decreased.
The aneurysm shown in Figure 2 exemplifies the subtle degree of stasis that is often observed with placement of a single flow diverting stent (Grade A2). This degree of stasis is best appreciated on a 'down the pipe' view as shown in the lower panel (Figure 2). The contrast clears first from the parent vessel lumen, while clearance from the aneurysm is slightly delayed.
The aneurysm shown in Figure 3, underscores the importance of determining a pre- treatment grade. There is stasis on the initial angiographic run, persisting into the venous phase (Grade A3). Following placement of a single flow diverting stent there is reduced filling with significant stasis (Grade B3). Of note, this aneurysm closed relatively quickly on subsequent follow-up assessments. A six month CTA shows no filling and regression of the aneurysm mass effect (Figure 3 lower panel).
Discussion
The appropriate role for flow diversion in the treatment of intracranial aneurysms has yet to be fully established. Early experiences, confined to expert users in selected patient populations, are certainly encouraging. Nevertheless, many questions persist: At what point are an- eurysms treated with flow diversion protected from future subarachnoid hemorrhage? What are the long-term patency rates for the parent vessel and covered branches? How much coverage is required to reliably and safely close a targeted aneurysm? Can the degree of stasis on initial angiographic assessment be used to predict the likelihood and rate of aneurysm closure? What is the significance of a neck remnant in a largely thrombosed aneurysm treated with flow diversion? The answers for many of these questions will come through increased experience and study. However, in order to effectively communicate and interpret such results a standardized means of describing angi- ographic findings is imperative.
We propose the present grading scale to address these objectives. The scale is designed to be simple and is based on recognizable angio- graphic characteristics. The scale adequately discerns the spectrum of expected angiographic outcomes in the pre-treatment, peri-operative and follow-up settings. To establish the validity of this grading scale, several future studies are planned. The inter- and intra-observer reliability will be studied among neuro-interventional- ists. The degree of correlation with quantitative flow analysis will be determined, allowing integration of the insights gained from in vitro and simulated flow experiments with in vivo clinical experience.
Once established this scale will allow standardized outcome reporting from clinical trials and registries, facilitating meta-analysis and data comparison. A reproducible analysis of the angiographic outcomes will be critical for the study of clinically relevant phenomena such as the amount of coverage needed to ultimately ensure aneurysm closure, the expected rate by which aneurysm thrombosis can be expected after flow diversion, parent vessel patency, and the risk of progressive growth or rupture after treatment. As we navigate this new era of an- eurysm treatment, a common language can only facilitate collaborative investigation. It is our hope that this grading scale will provide important assistance in these endeavours.
Acknowledgements and Funding
The authors are grateful to Gyasi Bourne and Laurel Swenson of Canister Creative Inc. for assistance with artwork. This work did not have any specific funding sources.
Note Added in Proof
Drs. O'Kelly, Fiorella, and Marotta have each served as proctors for Pipeline (Chestnut / eV3) cases.
References
- 1.Fiorella D, Kelly ME, Albuquerque FC, et al. Curative reconstruction of a giant midbasilar trunk aneurysm with the pipeline embolization device. Neurosurgery. 2009;64:212–217. doi: 10.1227/01.NEU.0000337576.98984.E4. [DOI] [PubMed] [Google Scholar]
- 2.Lylyk P, Miranda C, Ceratto R, et al. Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: the Buenos Aires experience. Neurosurgery. 2009;64:632–642. doi: 10.1227/01.NEU.0000339109.98070.65. [DOI] [PubMed] [Google Scholar]
- 3.Raymond J, Guilbert F, Weill A, et al. Long-term angi-ographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34:1398–1403. doi: 10.1161/01.STR.0000073841.88563.E9. [DOI] [PubMed] [Google Scholar]