Summary
Treatment of BBAs is currently challenging and remains difficult despite improvement of microsurgical technique and advancement in endovascular technologies. Therapeutic options are reconstructive and deconstructive open surgeries or endovascular procedures. However, there is a lack of consensus about optimal treatment. We report a case of 38-year old woman with subarachnoid hemorrhage due to a ruptured BBA successfully treated with placement of an endovascular flow-diverting stent.
Key words: blood blister-like aneurysm, flow-diverting stent
Introduction
Blood blister-like aneurysms (BBAs) are small, broad-based aneurysms arising at the non-branching sites of the supraclinoid internal carotid artery (ICA). They present treatment challenges due to their small size, fragile walls, lack of aneurysm neck and high intra-operative risk of rupture 1. As several therapeutic strategies have been used including open surgery, endovascular techniques and combined methods, no current gold standard for the treatment of BBAs can be identified.
This paper presents a case of SAH secondary to a ruptured BBA which was treated by endovascular approach using a SILK flow-diverting stent (Balt Extrusion, Montmorency, France). To our knowledge, this is the first reported case utilizing this method for the cure of a ruptured BBA.
Case Report
A 38-year-old woman presented with sudden onset of intense headache and vomiting. Examination revealed hypertension and a Glasgow coma scale (GCS) of 15 without focal neurological deficits. Initial brain computed tomography (CT) revealed a subarachnoid hemorrhage (SAH) grade 3/4 on modified Fisher scale with hydrocephalus. CT angiography showed a 2 mm BBA arising from the lateral wall of the left ICA.
After right frontal external ventricular drain (EVD) insertion for the control of the hydrocephalus and intracranial pressure (ICP) monitoring, the patient was admitted and our standard SAH medical treatment protocol initiated. Various therapeutic options were discussed with the patient including observation, open surgery for clipping and/or wrapping, endovascular treatment consisting of coiling, carotid sacrifice or carotid stenting. Risks and benefits were balanced for all therapeutic options. The final decision was to attempt a reconstructive endovascular procedure with SILK stent placement within the supra-ophthalmic ICA in order to cover the aneurysmal neck and preserve the left carotid artery patency.
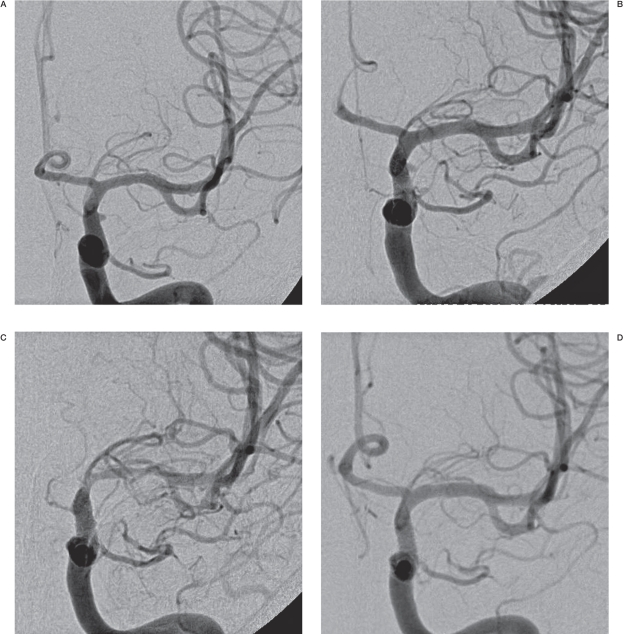
On admission day, the patient underwent cerebral DSA and endovascular treatment under general anesthesia and 600 mg of clopidogrel and 325 mg of acetylsalicylic acid (ASA) were also administered. The DSA confirmed the presence of the 2 mm BBA located on the lateral wall of the left supra-ophthalmic ICA (Figure 1A) and no evidence of other intracranial vascular abnormality or vasospasm.
Figure 1.
Right ICA angiogram (frontal view) shows the BBA (arrowhead) at the time of admission (A) and after placement of the SILK flow-diverting stent (B). Complete Occlusion of the BBA is obtained 18 days after stent placement (C) and maintained 6 months later (D).
The left ICA injection with compression of the right ICA revealed patency of the anterior communicating artery with good cross-flow to the right side. A coaxial system formed by a 6-French long sheath and 6-French guiding catheter was placed into the left carotid artery. When the microcatheter was placed into the left MCA, before stent delivery, the patient was loaded with 10 mg IV ReoPro. A first 4x25 mm flow-diverted SILK stent was satisfactory placed into the supra-ophthalmic segment of the left ICA. Two angiographic controls at 30 minute intervals showed persistent opacification of the BBA, good flow into the left ICA and no evidence of distal thromboembolic projections. A second 4x25 mm SILK stent was placed, overlapping the first one in front of the aneurysm neck. Two more angiographic controls at 20 minute intervals, revealed satisfactory positioning of the stents, with persistent opacification of the BBA, good flow into the left ICA and no distal thromboembolic projections.
Treatment with clopidogrel and ASA was continued for 6 months postoperatively, to prevent stent occlusion and thromboembolic ischemic complications. Angiographic controls were repeated two (Figure 1B), five, 12 and 18 days after stent placement. Occlusion of BBA was demonstrated on the last DSA performed at day 18 (Figure 1C). The course in hospital was complicated by a small left posterior temporoparietal asymptomatic ischemic lesions, hyponatremia requiring 3% NaCl administration and diffuse cerebral vasospasm managed with hypervolemia. The patient was discharged on day 18. DSA studies at 2.5 months and six months (Figure 1D) after treatment demonstrated stable occlusion of the left ICA BBA without evidence of in-stent stenosis or distal thromboembolic complications. At six month follow-up clinic visit, the patient was doing well, had returned to all her previous activities including employment and her neurological examination was normal.
Discussion
Blood blister-like aneurysms (BBAs) account for less than 2% of all intracranial aneurysms 2 and less than 6.6% of ICA aneurysms 1. They consist of focal defects in the non-branching part of the intracranial ICA with very thin walls composed of normal adventitia, but covered with clots and fibrous tissue, and an absence of the remaining arterial wall layers 3. These histological characteristics make them unique entities and therefore, strategies used for the treatment of other types of intracranial aneurysms cannot be applied for BBAs.
Isolated cases of successful endovascular treatment of ruptured BBAs have been reported, using various therapeutic strategies including endosaccular coil embolization with or without stent assistance or stent-in-stent techniques with preservation of the ICA 2,4-7. However, high rates of failure of these treatments have been encountered due to technical difficulties as well as rebleed rates up to 100% have been reported 1,6,8. Various surgical approaches have also been proposed including wrapping of the ICA, aneurysm clipping or ICA ligation or trapping with or without extracranial-intracranial (EC-IC) bypass 1,3,9. However, high rates of intra and post-operative rebleeding have been reported often requiring acute-stage ICA sacrifice which leads to cerebral infarcts during the period of vasospasm and very poor outcome 1,9. Although high flow EC-IC bypass has been proposed as a preventive method for cerebral ischemia following ICA occlusion, it needs to be performed prior to the onset of vasospasm 1 as the preoperative hemodynamic state and viability of corresponding brain area are strong indicators for the success of the EC-IC procedure 10. In conclusion, an optimum treatment of BBAs is currently undetermined and, despite various therapeutic strategies, morbidity and mortality rates as well as the risk of aneurysm regrowth and rebleed remains significant 1,8.
We describe a case of primary reconstructive endovascular stent-within-a-stent technique using two flow-diverting SILK stents for the treatment of a ruptured BBA. Although stent-within-stent techniques have been successfully used to prevent rebleeding and regrowth of BBAs 2, to our knowledge this is the first reported case of cured ruptured BBA with the use of flow-diverting (SILK) stent. While the efficacy of stents, including the SILK flow-diverter, in the treatment of unruptured aneurysms has been demonstrated 11, the major argument against the use of stents in patients with aneurysmal SAH is that it requires antiplatelet therapy 12. Although re-bleeding is a concern, it is believed that the risk of intracerebral hemorrhage in patients undergoing antiplatelet therapy is independent of the preexistence of an SAH 12. This is an even more important issue in the case of flow-diverting devices due to a delayed aneurysm obliteration after device deployment 13,14, a phenomenon also observed in our case.
Acknowledgements
We acknowledge Dr Marshall Wilkinson from the University of Manitoba, for reviewing and helping with editing this manuscript.
References
- 1.Meling TR, Sorteberg A, Bakke SJ, et al. Blood blisterlike aneurysms of the internal carotid artery trunk causing subarachnoid hemorrhage: treatment and outcome. Neurosurgery. 2008;108:662–671. doi: 10.3171/JNS/2008/108/4/0662. [DOI] [PubMed] [Google Scholar]
- 2.Lee BH, Kim BM, Park MS, et al. Reconstructive endovascular treatment of ruptured blood blister-like aneurysm of the internal carotid artery. J Neurosurg. 2009;110:431–436. doi: 10.3171/2008.7.JNS08257. [DOI] [PubMed] [Google Scholar]
- 3.Da Silva JC, Faquini IV, Kitamura MAP, et al. Internal carotid artery blood blister-like aneurysm. Arq Neuropsiquiatr. 2008;66:563–565. doi: 10.1590/s0004-282x2008000400027. [DOI] [PubMed] [Google Scholar]
- 4.McNeely PD, Clarke DB, Baxter B, et al. Endovascular treatment of a "blisterlike" aneurysm of the internal carotid artery. Can J Neurol Sci. 2000;27:247–250. doi: 10.1017/s0317167100000901. [DOI] [PubMed] [Google Scholar]
- 5.Doorenbosch X, Harding M. Primary treatment of a blood-blister-like aneurysm of the internal carotid artery with Guglielmi detachable coil embolization. J Clinical Neuroscience. 2008;15:1276–1279. doi: 10.1016/j.jocn.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 6.Korja M, Rautio R, Valtonen S, et al. Primary treatment of ruptured blood blister-like aneurysms with stent-assisted coil embolization: report of two cases. Acta Radiol. 2008;49:180–183. doi: 10.1080/02841850701675735. [DOI] [PubMed] [Google Scholar]
- 7.Gaughen JR, Jr, Hasan D, Dumont AS, et al. The efficacy of endovascular stenting in the treatment of supraclinoid internal carotid artery blister aneurysms using a stent-in-stent technique. Am J Neuradiol. 2010 doi: 10.3174/ajnr.A2016. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park JH, Park IS, Han DH, et al. Endovascular treatment of blood blister-like aneurysms of the internal carotid artery. J.Neurosurg. 2007;106:812–819. doi: 10.3171/jns.2007.106.5.812. [DOI] [PubMed] [Google Scholar]
- 9.Ogawa A, Suzuki M, Ogasawara K. Aneurysms at non-branching sites in the surpaclinoid portion of the internal carotid artery: internal carotid artery trunk aneurysms. Neurosurgery. 2000;47:578–583. doi: 10.1097/00006123-200009000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Schaller B. Extracranial-intracranial bypass to reduce the risk of ischemic stroke in intracranial aneurysms of the anterior cerebral circulation: a systematic review. J Stroke Cerebrovasc Dis. 2008;17:287–298. doi: 10.1016/j.jstrokecerebrovasdis.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Appelboom G, Kadri K, Hassan F, et al. Infectious aneurysm of the cavernous carotid artery in a child treated with a new-generation of flow-diverting stent graft: case report. Neurosurgery. 2010:E623–624. doi: 10.1227/01.NEU.0000365370.82554.08. [DOI] [PubMed] [Google Scholar]
- 12.Pearl M, Gregg L, Gailloud P. Endovascular treatment of aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am. 2010;21:271–280. doi: 10.1016/j.nec.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Lylyk P, Miranda C, Ceratto R, et al. Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: the Buenos Aires experience. Neurosurgery. 2009;64:632–642. doi: 10.1227/01.NEU.0000339109.98070.65. [DOI] [PubMed] [Google Scholar]
- 14.Szikora I, Berentei Z, Kulcsar Z, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the Pipeline embolization device. Am J Neuradiol. 2010 doi: 10.3174/ajnr.A2023. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]