Summary
We describe a patient with dural arteriovenous fistula (DAVF) treated with Onyx-18 who developed isolated hypoglossal nerve palsy. This is the first case of isolated hypoglossal nerve palsy caused by Onyx-18 embolization. This complication suggests that over embolization with On- yx-18 in the treatment of hypoglossal canal DAVFs should be avoided, and transvenous em- bolization may be safer. Furthermore, pred- nisolone therapy should be carried out in the prophase of nerve palsy.
Key words: dural arteriovenous fistula, intracranial arteriovenous malformations, hypoglossal nerve, dimethyl sulfoxide
Introduction
Dural arteriovenous fistulas (DAVFs) are defined as abnormal connections between an arterial feeder and a dural venous sinus or leptomeningeal vein, with the point of fistulization located within the dural leaflets. They account for 10% to 15% of all intracranial arteriovenous malformations (AVMs) 1. As DVAFs with leptomeningeal venous drainage or an associated venous varix present with hemorrhage or progressive neurologic deficits, aggressive treatment is required. Onyx (ev3, Irvine, CA, USA) embolization is now an established method for treatment of DAVFs 1-3. The literature on complications of Onyx embolization is increasing gradually. Here, we report a case treatment of DAVF using Onyx-18 that led to isolated hypoglossal nerve palsy. To our knowledge, this is the first case of isolated hypoglossal nerve palsy caused by Onyx-18 embolization.
Case Report
A 48-year-old man presented at our hospital complaining of intracranial bruits. The cranial nerve and laboratory examinations were normal. A DVAF was considered, conventional digital subtraction angiography was performed, which showed a Cognard II DVAF in the location of right hypoglossal canal (HC). The DVAF was fed by the meningeal branches of the bilateral ascending pharyngeal arteries, and the right anterior condylar veins within the hypoglossal canal that was the fistulous point mainly drained into the jugular vein. Endovascular treatment was insisted upon by the patient because of the associated intolerable intracranial bruit. Treatment was performed by transarterial approach under general anesthesia using a biplane angiographic unit. Standard coaxial techniques were used. The guide catheter was navigated into the left ascendingtrawt pharyngeal artery. Marathon flow directed catheter (eV3) was subsequently navigated over a Mirage.008 microwire (eV3) to reach as near as possible to the fistula. The microcatheter was flushed with 10 mL of normal saline. The dead space of the microcatheter was subsequently filled with dimethyl sulfoxide (DMSO). Onyx-18 was then injected over two minutes to fill the microcatheter and to replace the DMSO in the dead space. The injection was stopped until unwanted flow into branches of the right ascending pharyngeal artery was observed. The follow-up angiogram showed no residual shunt (Figure 1). The intracranial bruits disappeared immediately after the operation. For the toxicity of DMSO, 10 mg dexamethasone was intravenously injected for three days. On the second day after endovascular treatment, the patient complainted of difficulty moving his tongue to the left. Cranial nerve examination was only significant for a right hypoglossal nerve palsy. The patient was discharged from our hospital four days after treatment without continuative pharmacotherapy. At two months follow-up, the patient's main complaint were difficulty swallowing (dysphagia) and slurred speech (dysarthria). In addition, his tongue deviated toward the right during tongue protrusion, and marked right-sided hemiatrophy was observed (Figure 2).
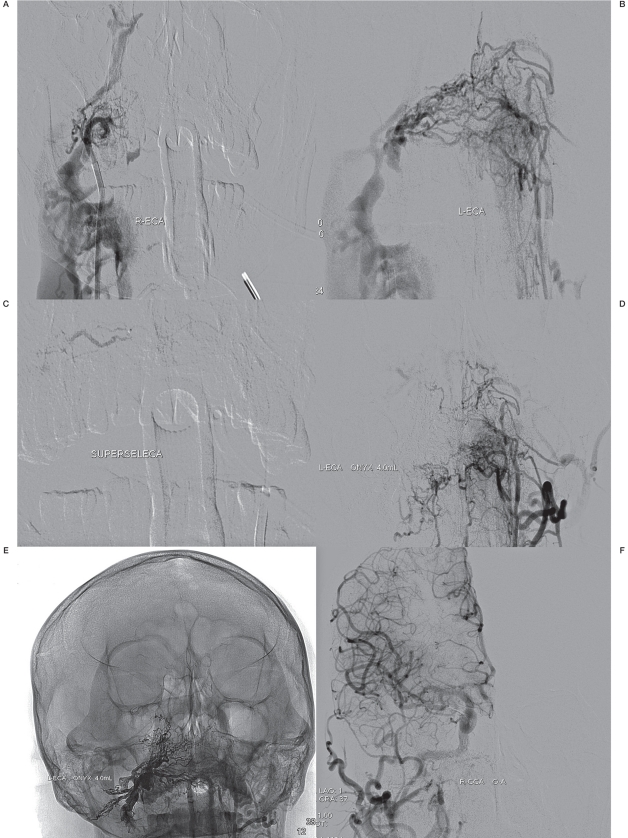
Figure 1.
A) DSA shows a DVAF in the location of right HC ^ which is fed by right ascending pharyngeal artery and drains into the right jugular vein (right external carotid injection). B) The DVAF is also supplied by left ascending pharyngeal artery (left external carotid injection). (C) Superselect angiography shows the fistula. (D) No residue of shunt remains after Onyx injection (left external carotid injection). E) The extension of reflux of Onyx. F) The DVAF is eliminated (right common carotid injection).
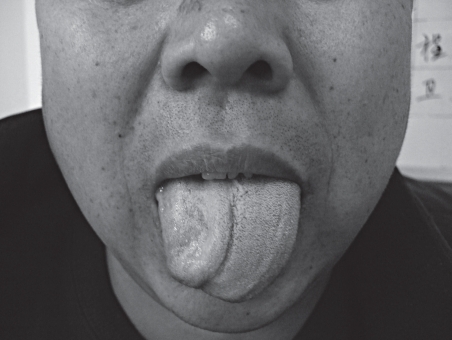
Figure 2.
The patient's tongue deviates toward the right during tongue protrusion, and marked right-sided hemiatrophy is present.
The cranial nerve examation showed right hypoglossal nerve palsy persisted. We telephone the patient at three months follow-up and requested a vocal cord evaluation by an ENT specialist in a local hospital. Vocal cord paralysis was not found, and there was no evidence of vagus nerve dysfunction. Oral Vitamin B12 was used and his prognosis was still at a long follow-up.
Discussion
The hypoglossal nerve is a pure motor nerve that primarily supplies the intrinsic and extrinsic muscles of the tongue. The nucleus of the nerve has a bulbar and spinal extension. The fibers exit between the inferior olivary nucleus and the corticospinal tract of the pyramid. In the medullary cistern, these fibers fuse to form the hypoglossal nerve. The nerve has a short cisternal segment directed anterolaterally and inferiorly. It then enters the hypoglossal canal of the occipital bone. The nerve then courses anteriorly and inferiorly between the internal carotid artery and the internal jugular vein, and finally extends anteriorly and cephalad into the tongue. The hypoglossal canal is found to contain three important structures: the hypoglossal nerve, the meningeal branch of ascending pharyngeal artery and surrounding venous plexus (anterior condylar veins).
The canal lies posteromedial and inferior to the jugular foramen 4. The definition of hypoglossal canal DVAFs was first proposed by Manabe et al. Hypoglossal canal DAVFs are mostly fed by the neuromeningeal branches of the bilateral ascending pharyngeal artery via the jugular foramen and the HC, the occipital artery via the mastoid foramen and the meningeal branches of the vertebral artery via the foramen magnum. The anterior condylar vein within the HC that is the fistulous point mainly drains via an extracranial route into the jugular vein, and often drains via an intraosseous route 5.
Manabe et al. had reported a patient with isolated hypoglossal nerve palsy after endovascular treatment of a hypoglossal canal DAVF with coil 5. The mechanical compression of the coil was considered to be the cause of nerve palsy. Two mechanisms responsible for isolated hypoglossal nerve palsy in our patient were suggested. First, some reflux of Onyx into the branches of right ascending pharyngeal artery were noted during our injection for a complete shunt occlusion. The nerve plasy may be attributed to the interruption of the nutrient vessel (the meningeal branches of the ascending pharyngeal artery) 6,7. Second, this complication might be caused by DMSO which exhibited high local toxicity, causing nerve damage at or near the site of administration 8.
The endovascular treatment methods for DAVFs include transarterial embolization, transvenous embolization and transarterial combined with transvenous embolization. Transarterial approaches which consist of superselective catheterization of the dural branches supplying the DAVF are well established with low mortality and morbidity 1-3. But concerning to hypoglossal canal DAVFs, Manabe et al. presumed the transvenous approach may be even better 5. The hypoglossal nerves were fed by branches of the ascending pharyngeal arteries which also supplied the glossopharyngeal and vagus nerves, and often anastomosed with vessels such as the carotid and vertebral arteries. Over occlusion of the ascending pharyngeal artery might lead to some unexpected complications, since the endovascular surgeon could not exactly control over injection of onyx to prevent its transversal penetration deep into the venous circulation or normal vessels. But because of the tortuosity of venous systems, the microcatheter was placed at the target position with difficultly.
The literature on medication of this complication is lacking, Loro et al. suggested prednisolone was effective for hypoglossal nerve palsy due to trauma 9, this was a reference for our pharmacotherapy. In summary, we should avoid over embolization with Onyx in the treatment of hypoglossal canal DAVFs, and prednisolone should be given in the prophase of nerve palsy.
References
- 1.Stiefel MF, Albuquerque FC, Park MS, et al. Endovascular treatment of intracranial dural arteriovenous fistulae using Onyx: a case series. Neurosurgery. 2009;65(6 Suppl):132–139. doi: 10.1227/01.NEU.0000345949.41138.01. [DOI] [PubMed] [Google Scholar]
- 2.Lv X, Jiang C, Li Y, et al. Embolization of intracranial dural arteriovenous fistulas with Onyx-18. Eur J Radiol. 2010;73(3):664–671. doi: 10.1016/j.ejrad.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Lv X, Jiang C, Zhang J, et al. Complications related to percutaneous transarterial embolization of intracranial dural arteriovenous fistulas in 40 patients. Am J Neuroradiol. 2009;30(3):462–468. doi: 10.3174/ajnr.A1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karasu A, Cansever T, Batay F, et al. The microsurgical anatomy of the hypoglossal canal. Surg Radiol Anat. 2009;31(5):363–367. doi: 10.1007/s00276-008-0455-x. [DOI] [PubMed] [Google Scholar]
- 5.Manabe S, Satoh K, Matsubara S, et al. Head and neck hypervascular lesions: embolization with ethylene vinyl alcohol copolymer-laboratory evaluation in swine and clinical evaluation in humans1. Neuroradiology. 2008;50(8):715–721. [Google Scholar]
- 6.Geibprasert S, Pongpech S, Armstrong D, et al. Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventionalist needs to know. Am J Neuroradiol. 2009;30(8):1459–1468. doi: 10.3174/ajnr.A1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lasjaunias P, Berenstein A, et al. The ascending pharyngeal artery. Vol 1. Berlin-Heidelberg: Springer-Verlag; 2001. Surgical neuroangiog-raphy; pp. 200–224. [Google Scholar]
- 8.Gobin YP, Murayama Y, Milanese K, et al. Head and neck hypervascular lesions: embolization with ethylene vinyl alcohol copolymer--laboratory evaluation in swine and clinical evaluation in humans. Radiology. 2001;221(2):309–317. doi: 10.1148/radiol.2212001140. [DOI] [PubMed] [Google Scholar]
- 9.Loro WA, Owens B. Unilateral hypoglossal nerve injury in a collegiate wrestler: a case report. J Athl Train. 2009;44(5):534–537. doi: 10.4085/1062-6050-44.5.534. [DOI] [PMC free article] [PubMed] [Google Scholar]