Summary
A 69-year-old hypertensive woman with a hyperdynamic, left brachio-basilic dialysis fistula presented with a long history of throbbing in her head, swelling of the left side of the face and two months of right visual loss with gross swelling of the right optic disc.
Tight stenosis of left brachiocephalic vein was found to be causing retrograde flow into the left jugular vein which normalised after dilatation and stenting with resolution of the papillodema.
Key words: brachiocephalic vein stenosis, dialysis fistula
Introduction
Brachiocephalic vein stenosis or thrombotic occlusion can occur in dialysis patients, and creation of an ipsilateral arteriovenous fistula can cause cerebral venous hypertension, retrograde flow in the ipsilateral jugular vein and may result in unilateral facial swelling 1 and pseudotumour cerebri 2-4.
We describe a patient with left brachiocephalic stenosis who developed papillodema and visual loss contralateral to a hyperdynamic left brachio-basilic fistula, several years after complaining of facial swelling and throbbing headache ipsilateral to the fistula.
Case Report
A 69-year-old, hypertensive Afro-Caribbean woman with a seven year history of dialysis dependent renal failure, secondary to microscopic polyangiitis, presented with a two month history of gradually progressive visual loss in the right eye.
In 2001 she had had right central venous catheterisation but no left-sided catheterisations. A left brachio-basilic fistula was fashioned and required several surgical revisions to reduce flow over the subsequent eight years. In 2004 painless left facial swelling and throbbing headache (without visual disturbance) was noted, and balloon venoplasty carried out at that time on a left brachiocephalic stenosis resulted in symptomatic improvement.
On examination there was oedema of the left face with dilated veins over the face and neck. There was slight proptosis of the left eye. Visual acuity was 6/6+4 on the right and 6/9+3 on the left with a grossly swollen right optic disc. The visual field in the right eye was constricted. There were no cranial bruits. The fistula in the left cubital fossa was grossly aneurysmal.
An MRI scan of the brain showed dilated left superior ophthalmic vein and dilated veins over the scalp and bridge of the nose (Figure 1). Cerebral angiogram showed reversal of flow in the left vertebral artery, thought to be secondary to a subclavian steel phenomenon, and the venous phase of the angiogram showed the dilated left superior ophthalmic vein (Figure 2) with failure of the left transverse sinus and left jugular vein to fill, but normal filling on the right.
Figure 1.
T2-weighted MR image shows the dilated left superior ophthalmic vein and dilated veins over bridge of the nose.
Figure 2.
Early venous phase of cerebral angiogram, left carotid injection, showing retrograde flow in enlarged superior ophthalmic vein and to lesser extent in inferior ophthalmic vein.
Arch aortogram showed failure of the left vertebral artery to fill, as well as venous return in the cephalic, axillary and subclavian veins refluxing towards the head in the left internal jugular vein (Figure 3) and crossing through the skull base to exit the skull vault through the right internal jugular vein. Thrombus was also seen in the left internal jugular vein.
Figure 3.
Arch aortogram, late venous phase showing reflux towards the head in the left internal jugular vein with left internal jugular vein thrombus.
A central venogram revealed a mild left subclavian vein stenosis and a completely blocked left brachiocephalic vein (Figure 4) forcing returning blood into the left jugular vein. The stenosed segment of the left brachiocephalic vein was dilated with a balloon, and a stent (Gore Haemobhan, diameter 13 mm, lenth 5 cm) was placed across the narrowing, resulting in an immediate reduction in collateral flow via the neck (Figure 5).
Figure 4.
Central venogram, showing tight stenosis in the most medial aspect of the left brachiocephalic vein.
Figure 5.
Central venogram after stenting of the stenosed segment of the left brachiocephalic vein.
An ultrasound examination following stenting demonstrated an immediate return to normal direction of flow in both the left vertebral artery and left jugular vein. MRI three weeks after the procedure showed reduced distension in the left superior ophthalmic and facial veins (Figures 6A,B). The patient quickly reported a marked improvement in the throbbing headache, intracranial noise and left-sided facial swelling. The papillodema in the right eye settled over the next three months but without improvement in visual acuity which was 6/9+3 on the right and 6/9+1 on the left.
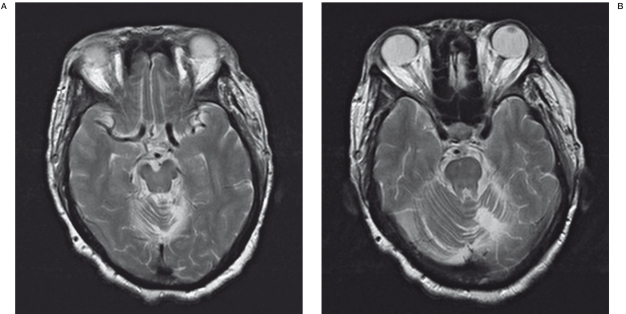
Figure 6.
T2 weighted MR image showing less dilatation in the left superior ophthalmic vein (A) and superficial vessels over the bridge of the nose (B).
Discussion
Brachiocephalic vein stenosis has been reported in dialysis patients much less commonly than subclavian vein stenosis but is associated with retrograde flow in the jugular vein, facial swelling and cerebral venous hypertension 1-4. Central venous stenosis, especially subclavian stenosis, is often related to prior central venous cannulation, although our patient had not had left central venous cannulation. It is interesting that Bommer et al. 1 report left brachiocephalic kinking and stenosis in a patient who had had all central catheters placed on the right hand side, suggesting that this may be explained by the tip of a right-sided catheter becoming displaced to the left causing local damage to the vessel wall resulting in stenosis. In addition, Ashizawa et al. 5 demonstrated brachiocephalic vein stenosis in a patient without prior central venous cannulation suggesting that this was idiopathic. Raised intracranial pressure (CSF pressure was not measured in our patient) would be likely in our patient and would explain papillodema if it was bilateral but it is difficult to explain the marked optic disc swelling contralateral to the obviously congested left orbit although it is likely that ischaemia secondary to venous congestion was the etiology, although possibly bilateral papillodema may have developed in time as described by Cuadra et al. 2. Brachiocephalic vein stenosis is unusual, but in renal patients with a history of subclavian cannulation the patency of the central veins should be checked before creation of a fistula. A high index of suspicion of central vein stenosis should be maintained when symptoms develop in a limb associated with a fistula as the sequelae are serious and largely reversible. Unfortunately vein restenosis is common following stenting, occurring in many patients within the first year 6, but can be addressed by angi-oplasty or surgical procedures to preserve a limb for haemodialysis for as long as possible.
Acknowledgements
The authors would like to acknowlege Dr Allan Thomas, Consultant Neuroradiologist, University Hospitals of Birmingham, UK and Dr Peter Riley, Consultant Interventional Radiologist.
References
- 1.Bommer J, Ritz E. The dialysed lady with one swollen cheek. Nephrol Dial Transplant. 1997;12:2188–2190. doi: 10.1093/ndt/12.10.2188. [DOI] [PubMed] [Google Scholar]
- 2.Cuadra SA, Padberg FT, Turbin RE, et al. P. Cerebral venous hypertension and blindness: A reversible complication. J Vasc Surg. 2005;42:792–5. doi: 10.1016/j.jvs.2005.05.060. [DOI] [PubMed] [Google Scholar]
- 3.Lal SM, Twardowski ZJ, van Stone JC. Benign intracranial hypertension: a complication of subclavian vein catheterisation and arteriovenous fistula. Am J Kid Dis. 1986;8:262–264. doi: 10.1016/s0272-6386(86)80037-3. [DOI] [PubMed] [Google Scholar]
- 4.Molina J, Martinez-Vea A, Riu S, et al. Pseudotumor cerebri: An unusual complication of brachiocephalic vein thrombosis associated with hemodialysis catheters. Am J Kid Dis. 1998;31:E3–E3. doi: 10.1016/s0272-6386(98)70065-4. [DOI] [PubMed] [Google Scholar]
- 5.Ashizawa A, Kimura G, Sanai T, et al. Idiopathic left innominate vein stenosis manifested following the creation of arteriovenous fistula in uremia. Am J Nephrol. 1994;14:142–144. doi: 10.1159/000168703. [DOI] [PubMed] [Google Scholar]
- 6.Maskova J, Komarkova J, Kivanek J. Endovascular treatment of central vein stenoses and/ or occlusions in haemodialysis patients. Cardiovasc Intervent Radiol. 2003;26:27–30. doi: 10.1007/s00270-002-1960-7. [DOI] [PubMed] [Google Scholar]