Summary
This report evaluated the short and midterm results of the safety and effectiveness of the treatment technique with hybrid and non-hybrid Y-configured, dual stent-assisted coil embolization of wide-neck intracranial aneurysms, and reviewed the literature concerning this technique.
Nine patients, eight with unruptured and one with ruptured aneurysms were included in the study. Of aneurysms embolized with a hybrid (with two different stents) and non-hybrid (with two identical stents) technique, three were located in the anterior communicating artery, three at the tip and one at the distal site of basilar artery, and two in the middle cerebral artery. All aneurysms included the orifices of bifurcation vessels. All aneurysms were stented and embolized during the same session. While Neuroform and Enterprise stents were used in the hybrid technique, two Enterprise stents were used in the non-hybrid technique.
Dual Y-stent assisted coil embolization was performed successfully in eight of nine patients (88.9%), including five patients (55.6%) with hybrid and three patients (33.3%) with non-hybrid technique. No procedural complication, no mortality and no minor or major neurological complications were seen during the angiographic or clinical follow-up. When an attempt was made at passing the second stent through the first Enterprise stent, the stent protruded inside the aneurysm in one patient (11.1%).
Hybrid or non-hybrid dual Y-stent-assisted coil embolization in the treatment of ruptured or unruptured wide-neck and complex intracranial aneurysms is a safe and effective method from the viewpoint of short and midterm results.
Key words: intracranial aneurysm, stent, therapeutic embolization
Introduction
Stent-assisted coil embolization or sole stenting has been widely used in the treatment of intracranial aneurysms. Almost every kind of aneurysm, ruptured or unruptured, including blister-like, wide-neck or fusiform complex lesions, can be treated with the endovascular technique, mainly with the help of stent technology, i.e. special intracranial, self-expanding, open and closed-cell nitinol stents with minimal radial force 1-7.
The Neuroform stent (Boston Scientific, Fremont, CA, uSA) is the first self-expanding, open-cell stent designed for intracranial usage. In addition to Neuroform, Enterprise (Codman & Shurtleff, Inc., Raynham, MA, uSA), Solitaire (EV3, MTI, Irvine, CA, uSA) and Leo (Balt, Montmorency, France) stents (closed-cell design) are also produced for aneurysm treatment 1,5,8-10.
Pipeline (PED; Chestnut Medical, Menlo Park, CA, uSA) and Silk (Balt, Montmorency, France) stents are used as flow diverters in the treatment of intracranial fusiform aneurysms or aneurysms with mainly mass effect 7,11,12.
Many reports have been published and many techniques have been described in the treatment of intracranial aneurysms with single, horizontal, double Y-configured or kissing and telescopic (stent in stent) stents 7,13-22.
This report evaluated the short and midterm results of the safety and effectiveness of the treatment technique with hybrid and non-hybrid Y-configured, dual stent-assisted coil embolization of wide-neck intracranial aneurysms and reviewed the literature. This article also presents the largest patient population in the Y-stent-assisted treatment series reported in the literature which was obtained from Pubmed, and the first cases of hybrid Y-configured stent technique.
Materials and Methods
Definition
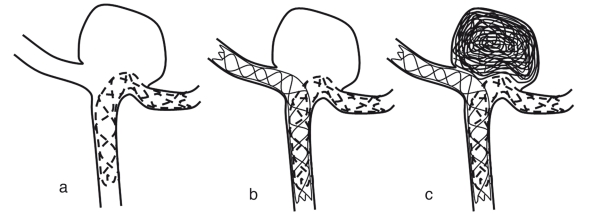
In this study, "hybrid, dual Y-stent-assisted coil embolization" means the use of two different stents (Neuroform3 and Enterprise) and "non-hybrid, dual Y-stent-assisted coil embolization" means the use of two stents of the same type in both cases in Y configuration (two Enterprise stents) (Figure 1).
Figure 1.
A-C Sequential schematic presentation of a wide-neck basilar bifurcation aneurysm embolization with hybrid, dual Y-stent-assisted coiling. After a neuroform stent is placed in the most acutely angled posterior cerebral artery (A), an Enterprise stent is deployed in the other branch (B). Then the aneurysm is coiled (C).
Patient Population
Nine patients, eight with unruptured and one with ruptured aneurysms were included in this study. There were five women and four men aged from 48 to 66 years (Mean: 49). Of aneurysms embolized with hybrid and non-hybrid technique, three were located in the anterior communicating artery (Acom), three at the tip, one at the distal site of the basilar artery (BA), and two in the middle cerebral artery (MCA). All aneurysms included the orifices of bifurcation vessels. Diameters of the aneurysms were from 5 to 14 mm. Of the nine patients, one had a subarachnoid hemorrhage (SAH); one, seizure; one, seizure and headache, and six, headache. One patient (patient no. 1) with a left MCA aneurysm had been operated on two months previously but she could not be clipped (Figure 2).
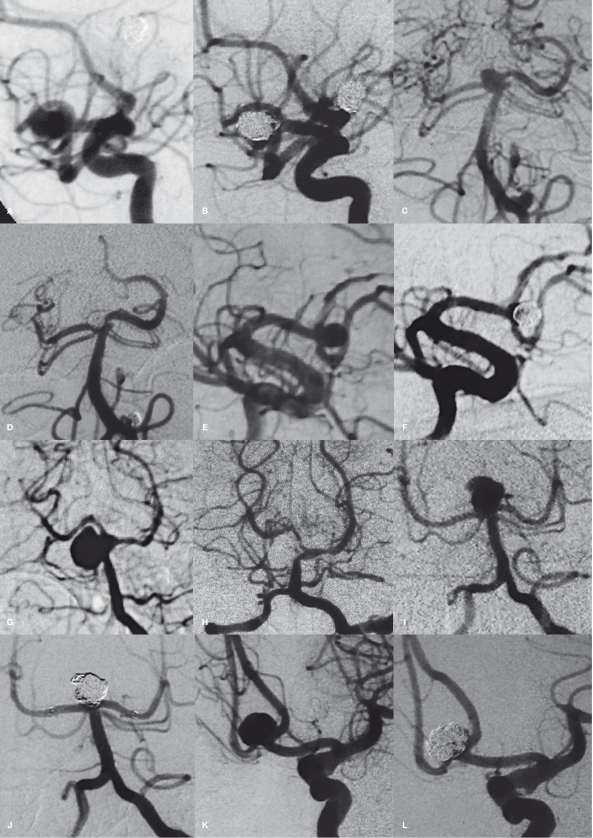
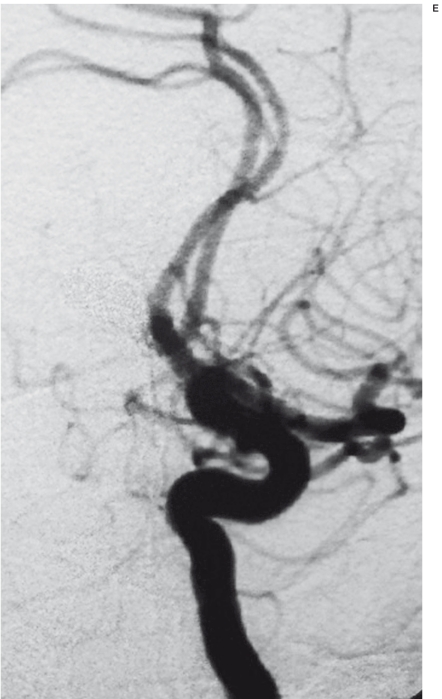
Figure 2.
A-G The patient with the left middle cerebral artery (MCA) aneurysm (patient no. 1) had been operated on 2 months previously and could not be clipped: Digital subtraction angiography shows the wide-neck MCA aneurysm (A). The first Enterprise stent (Neuroform3 stent could not be placed) lies between the inferior truncus and the proximal part of the MCA (black arrows in B). While trying to cross the first stent to deploy the second stent (Enterprise), the first stent protruded into the aneurysm, so proximal and distal markers of the first stent migrated (black arrows show the first and white arrows show the second stent markers in C). Aneurysm was intentionally not packed fully due to the protrusion of the stent into the aneurysm (D). This patient stopped taking the antiaggregant drugs (aspirin and clopidogrel) after 2 months and applied to the hospital because of severe headache and speaking problems. The cranial computed tomography showed acute temporal lobe infarction on the left (not shown). The occlusion of the inferior truncus of the left MCA was seen on angiography (E). Residual filling was also seen in the neck of the aneurysm. On DSA performed in the 11th month (F), the aneurysm was totally closed and there was no restenosis in the stent lying between the proximal part and the superior truncus of the MCA. Magnetic resonance imaging with the FLAIR sequence showed gliotic and cystic changes consistent with chronic infarction of the left temporal and occipital lobes (G) due to the occlusion of the inferior trunk of the MCA.
The patient (patient no. 6) with a seizure had also been treated surgically for an Acom aneurysm three years ago. This patient's aneurysm was also embolized totally using the balloon remodeling technique ten days after partial clipping surgery. Angiography performed three years after the first embolization showed a recurrence of the Acom aneurysm (Figure 3). Another patient (patient No. 3) with left MCA aneurysm, who also had a right MCA aneurysm, was treated with one stent-assisted coiling. Surgical clipping was suggested but the patient rejected the surgical treatment. The patient with SAH (patient no. 5) had a wide-neck BA aneurysm, containing left orifices of superior cerebellar (SCA) and posterior cerebral arteries (PCAs), between the right SCA and PCAs. This patient was embolized 25 days after SAH due to the high risk of surgery. Figure 4 shows all other patients' pre and postembolization angiographic images. Table 1 summarizes the demographic, clinical and angiographic findings, and figure numbers of the patients.
Table 1.
Summary of patients' demographic and clinical findings, and figure numbers of the patients.
| Patient no |
Age/ Sex |
Clinical Findings |
Location | Aneurysm diameter |
Additional aneurysm |
Previous treatment |
Stents (mm) |
Rate of embolization |
Complication | Follow-up Angiographic/ Clinical (Month/ Month) |
Figure |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 48/F | Headache | L MCA | 6×7 mm | Operated (failure) |
Enterprise (4.5x28) & Enterprise (4.5x22) |
Residual filling (intentionally) |
Stent protrusion and thrombosis due to cessation of antiaggregant drugs |
11/22 | 2 | |
| 2 | 60/F | Headache | L MCA | 6×6 mm | R MCA | Neuroform (3x20) & Enterprise (4.5x22) |
Total | 15/21 | 4A,B | ||
| 3 | 54/F | Headache | BT | 5×5 mm | BA L PICA L Pcom |
Neuroform (3x20) & Enterprise (4.5x22) |
Total | 15/20 | 4C,D | ||
| 4 | 56/M | Headache | Acom | 6×7 mm | Enterprise (4.5x22) & Enterprise (4.5x22) |
Total | 16/20 | 4E,F | |||
| 5 | 55/F | SAH | Distal BA | 10x12 mm | Neuroform (3x20) & Enterprise (4.5x22) |
Total | 15/19 | 4G,H | |||
| 6 | 57/M | Seizure/ Recanaliza- tion |
Acom | 6x8 mm | Partially clipped and Coil embolization without residual filling |
Neuroform (3x20) & Enterprise (4.5x22) |
Total | 16/19 | 3 | ||
| 7 | 59/F | Headache | BT | 8x9 mm | LOA | Neuroform (3x20) & Enterprise (4.5x28) |
Total | 15/17 | 4I,J | ||
| 8 | 66/M | Headache | Acom | 7x9 mm | Enterprise (4.5x22) & Enterprise (4.5x22) |
Total | 15/16 | 4K,L | |||
| 9 | 49/M | Headache Seizure |
BT | 14x10 mm | Neuroform (3x20) & Enterprise (4.5x22) |
Total | 6/10 | 4M,N | |||
| SAH: Subarachnoid hemorrhage, L: Left, R: Right, MCA: Middle cerebral artery, Acom: Anterior communicating artery, PICA: Posterior in ferior cerebellar artery, Pcom: Posterior communicating artery, \OA: Ophthalmic artery, BT: Basilar tip, BA: Basilar artery, DSA: Digital subtraction angiography. | |||||||||||
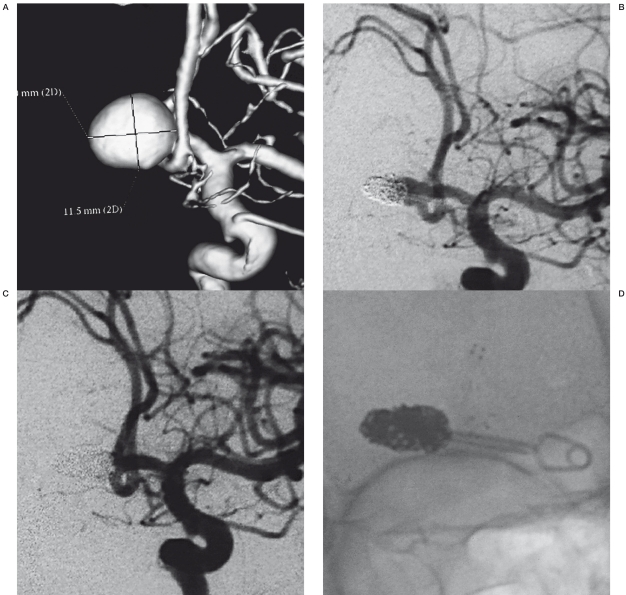
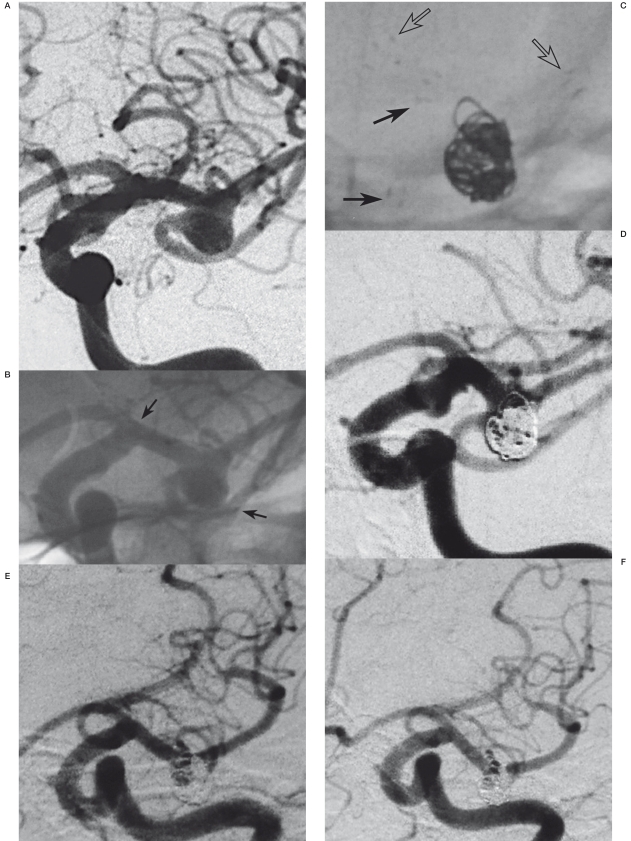
Figure 3.
A-E This patient (patient no. 6), admitted to the hospital because of seizure, was treated surgically for an anterior communicating artery (Acom) aneurysm 3 years previously (A). This patient's aneurysm, due to partial clipping was also totally embolized with the balloon remodeling technique 10 days after the surgery. Angiography performed 3 years after the first embolization showed recurrence of the Acom aneurysm (B). The aneurysm was treated with hybrid Y-stent-assisted coiling (C,D). The aneurysm was totally closed. Angiography performed 4 and 16 (E) months later showed no recurrence or in-stent stenosis.
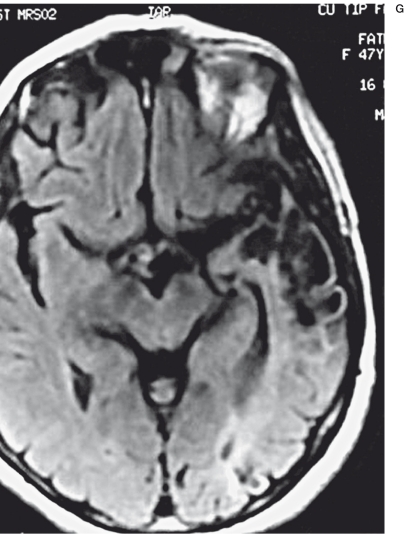
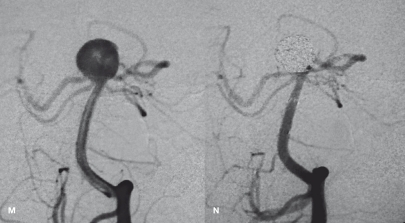
Figure 4.
A-N Pre and postprocedural angiographic images of patient no. 2 (A,B), 3 (C,D), 4 (E,F), 5 (G,H), 7 (I,J), 8 (K,L) and 9 (M,N).
Technique
One day before catheterization, eight of the nine patients were given 150 mg of acetylsalicylic acid (Aspirin; Bayer HealthCare, Germany) and 450 mg (six tablets) of clopidogrel (Plavix; Bristol-Myers Squibb/Sanofi Pharmaceuticals, NY, USA). The ninth patient, the one with a ruptured distal BA aneurysm, tirofiban (Aggrastat, Merck&Co., Inc., NJ) was administered a 0.5 mg intravenously (IV) of as an antiaggregant drug after stenting. Aspirin and loading dose of clopidogrel were administered by nasogastric tube one hour after the embolization After general anesthesia, a 6F 80-90 cm introducer (Arrow, Arrow International Inc., Reading, PA, USA) and a 6F 90 cm guiding catheter (Envoy; Codman & Shurtleff, Inc., Raynham, MA, USA or Guider Soft Tip; Boston Scientific, Fremont, CA, USA) for the internal carotid artery, and a 5F 90 cm shuttle introducer (Cook Medical Inc., IN, USA) for the vertebral artery were inserted through the right femoral access. After the femoral artery access, the serum-activated coagulation time (ACT) was checked and then 7500 IU heparin was administered IV. During the procedure, 1000 IU or more of heparin was administered per hour to obtain an ACT two to three times higher than the baseline value.
Hybrid, dual Y-stent-assisted coil embolization of the eight aneurysms without rupture was planned, first with a Neuroform3 stent and then with an Enterprise stent. In all eight patients, to facilitate the second stent deployment, the first stent was placed in the most acutely angled branch.
The second stent (Enterprise in all patients) was placed in the contralateral bifurcation branch by being passed through the first stent and partially telescoped at the proximal portion. Before deployment of the first stent, bifurcation vessels including aneurysms were catheterized with a microcatheter (Excelsior 10-18; Boston Scientific) and microguide wire (Terumo 0.016 inch, double angled, 180 cm; Terumo Medical Corporation, Tokyo, Japan). After the placement of the microcatheter into the desired position, the microguide wire was retracted and replaced with the exchange microguide wire (Transend Floppy 0.014 inch, 300 cm; Boston Scientific). A Neuroform3 stent (3×20 mm) was advanced and deployed carefully by centering it at the neck of the aneurysm. Then the neuroform3 stent transport shaft was pulled back and the transport microcatheter (Prowler Select Plus) of the Enterprise stent was advanced to the neck of the aneurysm. Then the microguide wire was pulled back. With the help of the microguide wire (terumo, 0.016 inch, double angle), the Prowler Select Plus was advanced through the neuroform3 struts and the microguide wire pulled back again. Then the Enterprise stent was deployed as a second stent. After the placement of the stents, the Prowler Select Plus microcatheter was retracted and the microcatheter excelsior SL-10 (Boston Scientific) was placed inside the aneurysm using a microguide wire (terumo 0.012 inch, 45° angled). All aneurysms were embolized with a combination of Guglielmi (GDC; Boston Scientific), Micrus (Micrus Endovascular Corporation, San Jose, CA, USA) and MicroPlex (MicroVention, Aliso Viejo, CA, USA) detachable bare and hydrogel coated coils.
In three patients, one with MCA (our first case, patient no. 1) and two with Acom aneu- rysms (patient nos. 4 and 8), two Enterprise stents (non-hybrid dual Y-stent-assisted technique) were placed, because the vessel tortuosity prevented applying sufficient force to push the Neuroform3 stent shaft to the desired position. In these three patients, Enterprise stents was easily placed at the necks of the aneurysms using Prowler Select Plus microcatheters.
A plan was made to embolize the ruptured aneurysm (patient no. 5) with the balloon-remodeling technique (Hyperglide 4×20 mm, EV3). But because of coil protrusion and aneurysmal dilation in the left and right orifices of the PCAs, the hybrid technique was applied after coiling.
In two patients, one (patient no. 2) with right MCA bifurcation and one (patient no. 7) with left ophthalmic artery aneurysms, the aneurysms were embolized with stent-assisted coiling during the same sessions. In another (patient no. 3) with basilar tip (BT) aneurysm, the left orificial aneurysm of the left posterior inferior cerebellar artery (PICA) was embolized using the balloon-remodeling technique (l·lyperform 4×7 mm, EV3) during the same session. One month later, the left Pcom aneurysm was treated using only a Silk stent (Bard, France), due to the mass effect of aneurysm, which caused left oculomotor nerve palsy. A small (1.5 mm) aneurysm between the left SCA and PCA was left without coiling after the hybrid Y stenting of the BT aneurysm in this patient. All angiographic and interventional procedures were performed using the General Electric angiographic machine (Advantx, General Electric Medical Systems, Milwaukee, WI, USA).
Follow-up
After embolization, 1000 Iu/h heparin IV infusion was continued for one day in all patients. Low molecular heparin (2 × 0.6 ml) was administered for five to seven days subcutaneously after stopping the IV heparin. A plan was formulated to give acetylsalicylic acid (150 mg/ day) and clopidogrel (75 mg/day) orally for three months, followed by a life-long use of aspirin alone.
Computed tomography (CT) was performed 30 minutes after the embolization and conventional magnetic resonance imaging (MRI) and diffusion MM, one to three days later. After discharge, all patients were controlled clinically. Follow-up first angiograms were performed after three to seven months and second ones 1215 months later.
Results
Dual Y-stent assisted coil embolization was performed successfully in eight of nine patients (88.9%) including six patients (66.7%) with hybrid and two patients (22.2%) with non-hybrid technique. In these eight patients, all aneurysms were closed totally without any residual filling. No procedural complication, no mortality, and no minor or major neurological complications were seen during either the angiographic (mean period: 13.8 months) or clinical (mean period: 15.8) follow-up.
In one patient (11.1%) with a left MCA bifurcation aneurysm (patient no. 1, our first case), a Neuroform3 stent could not be placed as a first stent because of tortuosity. While trying to pass the first Enterprise stent through the first stent, the first protruded into the aneurysm. After placement of the second stent, the aneurysm was partially coiled to prevent occlusion of the inferior truncus (Figure 2). This patient stopped taking the antiaggregant drugs (aspirin and clopidogrel) after two months and presented at the hospital because of severe headache and speech problems. Neurological examination disclosed right hemianopsia, Wernicke aphasia and emotional symptoms. Brain et examination revealed an acute infarction of the left temporal lobe. Antiaggregant treatment was restarted and cerebral digital subtraction angiography (DSA) was performed. The inferior truncus of left MCA was occluded and aneurysm filling was reduced. There was no intimal hyperplasia or stenosis inside the stent lying between the M1 segment and the superior truncus of the MCA. The patient was discharged with minimal emotional symptoms and right hemianopsia. A cerebral DSA performed after 11 months revealed that the aneurysm was almost totally closed with no intimal hyperplasia inside the stent. In the other eight patients, the first cerebral DSAs performed in three to seven months and the second ones in 11-13 months after embolization revealed no recanalization in their aneurysms and no stenosis or hyperplasia inside the proximal (two stents, stent in stent) or distal (one stent) part of the stents. Periodic clinical examination performed between one and 22 months after embolization in these eight patients revealed no neurological complications.
The patient with the ruptured distal BA aneurysm (patient no. 5) had a modified Rankin Scale (mRS) of 5 points before endovascular treatment. Her mRs was 1 point in the 19th month clinical control.
No subarachnoidal or intraparenchymal hemorrhage was seen on the cranial CT performed about 30 minutes after the procedure. No additional lesions were seen on the cerebral MRI performed after one to three days except in one patient with BT aneurysm with SAH who had a asymptomatic small brainstem ischemic lesion on MRI.
Discussion
In the management of wide-neck bifurcation aneurysms, more complex and novel techniques reported by some authors are needed and include remodeling with double-balloon 23, TriSpan neck-bridge device-assisted (Boston Scientfic) 14, horizontal stenting 18,20 and waffle cone technique 19 with one stent, and kissing 14 and Y-configured 13,15-17,21,22 stenting with two stents. The double-balloon remodeling technique is especially suitable in the treatment of ruptured wide-neck bifurcation aneurysms due to the possibility of hazardous re-rupture of aneurysms when anticoagulant and antiaggregant drugs are used. In this technique, two remodeling balloons are placed in the bifurcation vessels and cover the aneurysm neck 23. TriSpan neck-bridge device-assisted coiling was used before the employment of self-expanding, intracranial stents 14. But in recent times it has not been used widely. Most centers have abandoned the use of TriSpan. Horizontal stent-assisted coiling may be an alternative way of Y-stent-assisted coiling of the aneurysm in case it is impossible to place stents in Y configuration through the vertebral artery. In this technique, reported by Wanke et al. 18 in one patient and Siddiqui et al. 20 in eight patients, one stent is placed in the bifurcation of the BT or internal carotid artery terminus through the posterior communicating (Pcom) or Acom arteries and then coiling is performed. In this technique, the Pcom or Acom arteries must be patent and large enough to pass a microcatheter. In Horowitz's waffle cone technique, eight patients were treated using a single Neuroform stent placed partially into the afferent artery of the aneurysm. The portion of the stent protruding into the aneurysm fundus provided neck support for the subsequent successful coiling 19. Henkes et al. combined a kissing stent (two Neuroform2 stents) with a TriSpan (Boston Scientific), in a BT aneurysm before coiling 14. Firstly, they placed two stents side by side into the afferent artery of the aneurysm extending the distal parts of the stents inside the bilateral P1 segments of the PSA. Secondly, they placed the TriSpan in the neck of the aneurysm and coiled.
Dual Y-stent-assisted coil embolization is another option in the treatment of wide-neck, complex bifurcation aneurysms. In a wide-neck bifurcation aneurysm consisting of both bifurcation branches, the deployment of a single stent may not protect the contralateral branch from coil herniation 17. In the literature, this technique was first published by Chow et al. in 2004 13. They performed the technique without any complications in a patient with a wide-neck BT aneurysm that was unruptured and found accidentally. They used two self-expanding Neuroform stents to construct the Y configuration. Thorell et al. published the largest series in the literature, performed on seven patients with BT aneurysms 17. Y-stent-assisted coil embolization was performed mainly in BT aneurysms. Sani et al. performed the technique to treat a wide-neck MCA aneurysm for the first time 15. Lozen et al. also reported a series of cases including five BT aneurysms and one MCA aneurysm 21. While two Neuroform stents were used in all cases reported before Rohde et al., Rohde et al. reported the first case of wide-neck Acom artery aneurysm treated with two Enterprise stents 22. Table 2 summarizes the literature related to Y-stent-assisted coil embolization and our study.
Table 2.
Summary of the literature including Y-stent-assisted coil embolization.
| Author | No. of patients | Location (n) | Stents (n) | Complications (n) | Follow-up (months) |
|---|---|---|---|---|---|
| Chow et al. 13 | 1 | BT | Neuroform & Neuroform |
||
| Perez-Arjona et al. 16 | 3 | BT | Neuroform & Neuroform |
||
| Sani et al. 15 | 1 | MCA | Neuroform & Neuroform |
||
| Thorell et al. 17 | 7 | BT | Neuroform & Neuroform |
Stent migration (1) | 6 |
| Lozen et al. 21 | 6 | BT: 5 MCA: 1 |
Neuroform & Neuroform |
SAH (1) Coil stretch (1) |
36.7 |
| Rohde et al. 22 | 1 | Acom | Enterprise & Enterprise |
||
| Current study | 9 | BT (3) Acom (3) MCA (2) Distal BA (1) |
Enterprise & Enterprise (3) Neurorform & Enterprise (6) |
Stent protrusion and stent thrombosis one month later (1) |
Angiographic: 13.8 Clinical: 15.8 |
| BT: Basilar tip, MCA: Middle cerebral artery, Acom: Anterior communicating artery, SAH: Subarachnoid hemorrhage, BA: Basilar artery. | |||||
In our study, we planned to construct the Y configuration with two different self-expanding intracranial stents in all cases. We preferred Neuroform3 as a first stent, because it is an open-cell stent. When you deploy the Neuroform, its struts act as anchors and stabilize the stent. This way, stent migration is nearly impossible while you manipulate the transport catheter of the second stent to advance it through the interstices of the Neuroform. The reason for choosing the Enterprise as a second stent is that the transport catheter (Prowler Select Plus) of the Enterprise is thinner than the transport catheter of the Neuroform3 stent (2.3 F and 2.8 F respectively). So passing through the first stent struts with the Prowler Select Plus catheter is easier than with the Neuroform transport catheter. In our first case with an unruptured MCA aneurysm and two other cases with unruptured Acom artery aneurysms, we could not place the Neuroform transport catheter in the desired position because of carotid artery tortuosity and the shortness of the Neuroform transform catheter (135 cm). In three of these cases we easily deployed two Enterprise stents because the navigation and tractability of the Prowler Select Plus is easier and it is longer than the transport catheter of the Neuroform stent except one. We described the usage of same stents to configure Y shape in the cases as non-hybrid dual Y-stent-assisted coil embolization. In our first case with an MCA aneurysm, the first Enterprise stent migrated inside the aneurysm when we tried to pass the second stent through the struts of the first. In this case, we did not pack the whole aneurysm intentionally in order to protect the inferior trunk of the MCA from the occlusion. In three other unruptured BT aneurysms, one Acom, MCA, and one ruptured distal BA, we used Neuroform3 as the first and Enterprise as the second stent without any difficulty or any stent migration (hybrid dual Y-stent-assisted coil embolization). After construction of the Y configuration, all aneurysms were coiled without any remnants except for one ruptured BT aneurysm. This aneurysm was coiled with the balloon-remodeling technique and then Y-stenting was performed due to coil protrusion.
Incomplete coiling of wide-neck bifurcation aneurysms may result in recanalization secondary to the hemodynamics of the parent artery and to the high-pressure pulsatile flow directly at the coil mass. The placement of two stents in Y configuration may alter the flow pattern at the aneurysm neck, redirecting the flow toward the bifurcation vessels to potentially reduce the likelihood of recanalization and thromboembolic events. The presence of the stent reduces the risk of coil protrusion into the parent vessel. As the inflow is disturbed, the residence time of the platelets is increased, so the possibility of platelet adhesion on the vessel wall or coils is also increased, thus promoting aneurysm thrombosis. Finally, the stent provides a physical matrix for possible endothelial growth, facilitating the remodeling of both the aneurysm neck and the parent vessel. Multiple stent placements also seem to have an additive effect at reducing wall-shear stress, an advantage to the Y configuration compared to alternative approaches 13,21,24. In Thorell et al.'s series, recanalization was seen in two patients at the sixth and twelfth months and while one needed to be re-treated with embolization, the other did not 17. Lozen et al. also reported a case of recanalization, which did not require retreatment, at the 32nd month. The patient was being followed up and was stable at month 52.6 21. In our cases, during short and mid term follow-ups, we did not encounter any recanalization. When we reviewed the cases reported in the literature, we could see that the dual Y-stent-assisted coil embolization was performed on unruptured wide-neck aneurysms. In case of coiling the aneurysm with the stent, antiaggregant and anticoagulant drugs are required before, during and after the procedure. Although recent articles report the safety of stenting in ruptured aneurysms, especially in wide-neck blister-like and dissecting lesions, the use of stents in the endovascular treatment of the ruptured aneurysms may have devastating consequences in case of aneurysm rupture, aneurysm re-rupture, or parent vessel damage 1,2,4,6,8. Therefore, if possible, stents must not be used in the treatment of the ruptured aneurysms and other treatment options must be sought. In our case of the ruptured distal BA aneurysm, we coiled the aneurysm with the balloon-remodeling technique. But due both to the coil protrusion and to aneurysmal dilation consisting of the left and right orifices of PSAs, two stents with hybrid technique were deployed.
Conclusions
Hybrid or non-hybrid dual Y-stent-assisted coil embolization in the treatment of ruptured or unruptured wide-neck and complex intracranial aneurysms is a safe and effective method in view of short and midterm results in case of high risk of surgical clipping or refusal of surgical treatment.
The selection of the open-cell design for the first stent provides stent stabilization and reduces migration of the stent during insertion of the second stent.
It is important that this method be performed in patients with no contraindication for the administration of anticoagulant and antiaggregant drugs. Even though ours were not of a large group of patients (the largest in the literature) with a sufficient follow-up period, the risk of complications was similar to the conventional stent-assisted treatments. We need further studies to establish the long-term results regarding the safety and effectiveness of this technique for broad application and to obtain sufficient "first hand" experience.
References
- 1.Biondi A, Janardhan V, Katz JM, et al. Neuroform stent-assisted coil embolization of wide-neck intracranial aneurysms: strategies in stent deployment and midterm follow-up. Neurosurgery. 2007;61(3):460–468. doi: 10.1227/01.NEU.0000290890.62201.A9. [DOI] [PubMed] [Google Scholar]
- 2.Ahn JY, Cho JH, Jung JY, et al. Blister-like aneurysms of the supraclinoid internal carotid artery: challenging endovascular treatment with stent-assisted coiling. J Clin Neurosci. 2008;15:1058–1061. doi: 10.1016/j.jocn.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 3.Zenteno MA, Santos-Franco JA, Freitas-Modenesi JM, et al. Use of the sole stenting technique for the management of aneurysms in the posterior circulation in a prospective series of 20 patients. J Neurosurg. 2008;108:1104–1118. doi: 10.3171/JNS/2008/108/6/1104. [DOI] [PubMed] [Google Scholar]
- 4.Wakhloo AK, Mandell J, Gounis MJ, et al. Stent-assisted reconstructive endovascular repair of cranial fusiform atherosclerotic and dissecting aneurysms: longterm clinical and angiographic follow-up. Stroke. 2008;39:3288–3296. doi: 10.1161/STROKEAHA.107.512996. [DOI] [PubMed] [Google Scholar]
- 5.Juszkat R, Nowak S, Wieloch M, et al. Complete obliteration of a basilar artery aneurysm after insertion of a self-expandable Leo stent into the basilar artery without coil embolization. Korean J Radiol. 2008;9:371–374. doi: 10.3348/kjr.2008.9.4.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tähtinen OI, Vanninen RL, Manninen HI, et al. wide-necked intracranial aneurysms: treatment with stentassisted coil embolization during acute (<72 hours) subarachnoid hemorrhage-experience in 61 consecutive patients. Radiology. 2009;253:199–208. doi: 10.1148/radiol.2531081923. [DOI] [PubMed] [Google Scholar]
- 7.Lylyk P, Miranda C, Ceratto R, et al. Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: the Buenos Aires experience. Neurosurgery. 2009;64(4):632–642. doi: 10.1227/01.NEU.0000339109.98070.65. [DOI] [PubMed] [Google Scholar]
- 8.Yavuz K, Geyik S, Pamuk AG, et al. Immediate and midterm follow-up results of using an electrodetachable, fully retrievable SoLo stent system in the endovascular coil occlusion of wide-necked cerebral aneurysms. J Neurosurg. 2007;107:49–55. doi: 10.3171/JNS-07/07/0049. [DOI] [PubMed] [Google Scholar]
- 9.Pumar JM, Lete I, Pardo MI, et al. LEO stent monotherapy for the endovascular reconstruction of fusiform aneurysms of the middle cerebral artery. Am J Neuroradiol. 2008;29:1775–1776. doi: 10.3174/ajnr.A1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lubicz B, François O, Levivier M, et al. Preliminary experience with the enterprise stent for endovascular treatment of complex intracranial aneurysms: potential advantages and limiting characteristics. Neurosurgery. 2008;62:1063–1069. doi: 10.1227/01.neu.0000325868.06764.de. [DOI] [PubMed] [Google Scholar]
- 11.Fiorella D, Kelly ME, Albuquerque FC, et al. Curative reconstruction of a giant midbasilar trunk aneurysm with the pipeline embolization device. Neurosurgery. 2009;64:212–217. doi: 10.1227/01.NEU.0000337576.98984.E4. [DOI] [PubMed] [Google Scholar]
- 12.Appelboom G, Kadri K, Hassan F, et al. Infectious aneurysm of the cavernous carotid artery in a child treated with a new-generation of flow-diverting stent graft: case report. Neurosurgery. 2010;66:E623–4. doi: 10.1227/01.NEU.0000365370.82554.08. discussion E624. [DOI] [PubMed] [Google Scholar]
- 13.Chow MM, Woo HH, Masaryk TJ, et al. A novel endovascular treatment of a wide-necked basilar apex aneurysm by using a Y-configuration, double-stent technique. Am J Neuroradiol. 2004;25:509–512. [PMC free article] [PubMed] [Google Scholar]
- 14.Henkes H, Kirsch M, Mariushi W, et al. Coil treatment of a fusiform upper basilar trunk aneurysm with a combination of "kissing" neuroform stents, TriSpan-, 3D- and fibered coils, and permanent implantation of the microguidewires. Neuroradiology. 2004;46(6):464–468. doi: 10.1007/s00234-004-1192-4. [DOI] [PubMed] [Google Scholar]
- 15.Sani S, Lopes DK. Treatment of a middle cerebral artery bifurcation aneurysm using a double neuroform stent "Y" configuration and coil embolization: technical case report. Neurosurgery. 2005;57(1 Suppl):E209. doi: 10.1227/01.neu.0000163684.75204.cd. [DOI] [PubMed] [Google Scholar]
- 16.Perez-Arjona E, Fessler RD. Basilar artery to bilateral posterior cerebral artery 'Y stenting' for endovascular reconstruction of wide-necked basilar apex aneurysms: report of three cases. Neurol Res. 2004;26(3):276–281. doi: 10.1179/016164104225013969. [DOI] [PubMed] [Google Scholar]
- 17.Thorell WE, Chow MM, Woo HH, et al. Y-configured dual intracranial stent-assisted coil embolization for the treatment of wide-necked basilar tip aneurysms. Neurosurgery. 2004:1035–1040. [PubMed] [Google Scholar]
- 18.Wanke I, Gizewski E, Forsting M. Horizontal stent placement plus coiling in a broad-based basilar-tip aneurysm: an alternative to the Y-stent technique. Neuroradiology. 2006;48:817–820. doi: 10.1007/s00234-006-0128-6. [DOI] [PubMed] [Google Scholar]
- 19.Horowitz M, Levy E, Sauvageau E, et al. Intra/extraaneurysmal stent placement for management of complex and wide-necked-bifurcation aneurysms: eight cases using the waffle cone technique. Neurosurgery. 2006;58(4 Suppl 2):ONS-258-262. doi: 10.1227/01.NEU.0000204713.24945.D2. [DOI] [PubMed] [Google Scholar]
- 20.Siddiqui MA, J Bhattacharya J, Lindsay KW, et al. Horizontal stent-assisted coil embolisation of wide-necked intracranial aneurysms with the Enterprise stent-a case series with early angiographic follow-up. Neuroradiology. 2009;51:411–418. doi: 10.1007/s00234-009-0517-8. [DOI] [PubMed] [Google Scholar]
- 21.Lozen A, Manjila S, Rhiew R, et al. Y-stent-assisted coil embolization for the management of unruptured cerebral aneurysms: report of six cases. Acta Neurochir (Wien) 2009;151:1663–1672. doi: 10.1007/s00701-009-0436-9. [DOI] [PubMed] [Google Scholar]
- 22.Rohde S, Bendszus M, Hartmann M, et al. Treatment of a wide-necked aneurysm of the anterior cerebral artery using two Enterprise stents in "Y"-configuration stenting technique and coil embolization: a technical note. Neuroradiology. 2010;52:231–235. doi: 10.1007/s00234-009-0603-y. [DOI] [PubMed] [Google Scholar]
- 23.Arat A, Cil B. Double-balloon remodeling of wide-necked aneurysms distal to the circle of Willis. Am J Neuroradiol. 2005;26:1768–1771. [PMC free article] [PubMed] [Google Scholar]
- 24.Cantón G, Levy DI, Lasheras JC. Hemodynamic changes due to stent placement in bifurcating intracranial aneurysms. J Neurosurg. 2005;103:146–155. doi: 10.3171/jns.2005.103.1.0146. [DOI] [PubMed] [Google Scholar]