Summary
The endovascular technique is the gold standard treatment in dural arteriovenous fistulas. Due to the limited number of series published it is difficult to create rigid guidelines in terms of the best endovascular treatment approach. Treatment must be tailored to each particular case, but it is important to keep in mind that the possibility of treating a type V dAVF by the transvenous approach should not be discarded. In selected cases the transvenous approach may be helpful to increase the chance of success in the endovascular treatment of type V dAVF.
We describe a patient in whom the first arterial treatment failed to achieve occlusion of the fistulous point with the glue. Clinical symptoms improved due to the diminished flow at the fistula after the first embolization but as soon as collateral arteries were recruited by the fistula, spinal cord venous drainage impairment led to symptoms recurrence. Transvenous access allowed us to close the fistula completely in one only session with a complete disappearance of the pathologically inverted perimedullary venous flow.
Key words: dural arterious fistula, Cognard V, endovascular treatment, transvenous approach
Introduction
Intracranial dural arteriovenous fistulae (DAVF) are a heterogeneous group of lesions characterised by abnormal shunting of blood between the arterial and venous systems within the intracranial dura. Several classification systems have been reported to grade the risks of DAVF, predominantly those devised by Cognard et al 1 and Borden et al 2. It is now generally accepted that the venous drainage pattern of DAVF is the most important factor in predicting the risk of aggressive DAVF symptoms 1. DAVF represent 10%-15% of all intracranial vascular malformations and are considered acquired, probably as a result of venous thrombosis 3. Although they may occur anywhere in the brain dura mater, they more frequently appear in the transverse-sigmoid sinuses (TSS) and in the cavernous sinus (CS) 3. One or multiple dural feeders primarily supply intracranial DAVF through transosseous branches from the external carotid artery (ECA), but DAVF can also be fed by tentorial branches from the internal carotid (ICA) or vertebral arteries (VA).
Intracranial DAVF with spinal venous drainage is an uncommon presentation of this entity and is usually challenging because the presenting symptoms are variable and often related to spinal dysfunction 1. Only a few small series of this type of intracranial DAVF (Cognard classification type V) have been reported 4,5. Intracranial DAVF with spinal perimedullary venous drainage are characterised by slowly progressive myelopathy caused by congestion in the perimedullary venous system, leading to decreased tissue perfusion with oedema and progressive loss of cord function 1,5.
The gold standard for diagnosis is digital subtraction angiography (DSA), which allows us to identify the arterial feeders, the location and flow of the DAVF and also the venous drainage 6,7. In type V DAVF, cerebral angiography is the key to diagnosis, showing spinal venous drainage and enlarged spinal perimedullary veins, which can be followed downward throughout the spinal cord 5. Thrombosis of the involved sinus may also be identified. Hybrid CT angiography is a combination of bone subtraction and masking for bone removal. This new tool allows us to evaluate the DAVF completely, including haemodynamic and anatomical aspects6. Magnetic resonance angiography (MRA) allows the projection images similar to those obtained by radiographic DSA 7. MRI can reveal sinus thrombosis or even parenchymal oedema. DAVF with spinal venous drainage have a pathognomonic appearance on MRI, showing a swollen cervical cord with central myelopathy and enlarged perimedullary veins; these signs can be found in both spinal and intracranial DAVF. MRA is a complementary tool for the identification of DAVF with venous flow-related enhancement 8.
DAVF require treatment aimed at a complete and definitive fistula closure. In general, treatment of such fistulas primarily involves an endovascular approach, and if this fails, surgical or radiosurgical approaches are used 9.
We treated a patient with type V DAVF with transvenous embolization after failed transarterial treatment that allowed us to close the fistula completely in a single session.
Case Report
The patient was a 67-year-old woman with a medical history of intracranial DAVF localised at the upper margin of the right petrosal bone, sCognard classification V. Three months ago the patient attended the emergency department of another hospital with acute clinical spinal cord symptoms. The patient had acute neck pain radiating to the interscapular area, accompanied by weakness in both lower extremities that progressed to the upper extremities, as well as associated acute urinary retention. A cerebral CT scan showed no abnormalities. T2-weighted MRI showed a diffuse intramedullary lesion extending from C1 to C7 associated with serpiginous vascular structures in the posterior portion of the medulla oblongata, suggestive of DAVF.
Cerebral arteriography disclosed a thrombosed right sinus and type V DAVF, which was embolized using a transarterial approach, occluding the afferent artery that arises from the stylomastoid artery branch of the right occipital artery. The procedure ended with the apparent occlusion of the fistula. The patient remained asymptomatic for three months until one week prior to admission to our institution for progressive loss of strength in the upper extremities. During the previous seven days, she had noted progressive left hand clumsiness with subsequent total loss of strength. On clinical examination, the patient was alert and oriented. The pupils were equal and constricted briskly to light; visual fields were full on confrontation; upward and downward gazes were normal. Cranial nerve function was preserved. The patient had tetraparesis with right predominance and the bilateral triceps reflexes were abolished. MRI revealed a large diffuse lesion on the medulla oblongata secondary to an oedema and dilated perimedullary venous system (Figure 1). Angiography of the right ICA showed a thrombosed right transverse sinus (RTS) and right jugular vein (RJV) (Figure 2). Right ECA selective angiographies showed DAVF supplied by transosseous occipital branches (Figure 3), the ascending pharyngeal artery (Figure 4), and the posterior branch of the middle meningeal artery (Figure 5). We knew that the fistula pouch was near the thrombosed RTS (Figure 6A,B).The venous drainage was through the veins surrounding the brainstem, such as the pontomesencephalic, anterior and posterior spinal per- imedullary veins (Figure 7). Due to the failure of the first transarterial approach embolization procedure, we decided to attempt transvenous access. Since the fistula pouch was located in the proximal portion of the thrombosed RTS, we performed a right femoral vein approach navigated through the left jugular vein towards the RTS. We decided to use the left side because the thrombosed segment of the RTS to be reopened was smaller than the right side. The tip of a 6F guiding catheter (Cordis®) was placed into the right sigmoid sinus and then a 4F vertebral catheter (Terumo®) was advanced to the distal part of the RTS. The occluded RTS was penetrated from the distal side of the RTS using an Excelsior 14 microcatheter (Boston®) and Synchro 14 microguidewire (Boston®), and the catheter was navigated to the theoretical site of the fistula pouch. A successful attempt was made and the pouch was completely packed with Axium coils (Ev3®) (3 mm×4 cm, 2 mm×4 cm (2 coils), 2 mm×3 cm) and 33% Glubran® (Figures 8 and 9). Angiography performed immediately after embolization showed no contrast filling of the DAVF (Figure 10A,B). MRI performed nine months after embolization showed complete resolution of the large, diffuse lesion on the medulla oblongata (Figure 11).
Figure 1.
T2-weighted sagittal MRI showed oedema on the medulla oblongata.
Figure 2.
Angiography of the right ICA showing a thrombosed RTS and RJV.
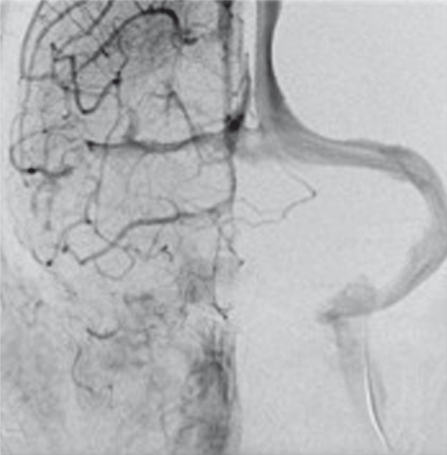
Figure 3.
A selective occipital artery angiogram oblique projection showed tge DAVF.
Figure 4.
A selective ascending pharyngeal artery angiogram lateral projection show the DAVF.
Figure 5.
Internal Maxilar angiogram in lateral projection showed DAVF supplied by middle meningeal artery.
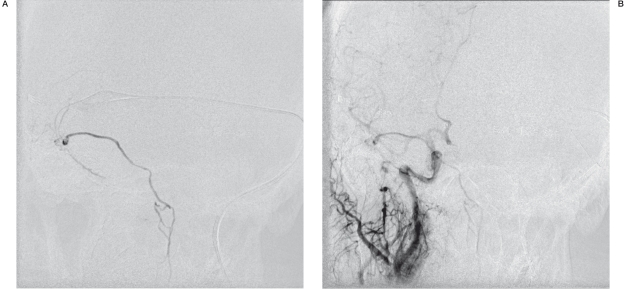
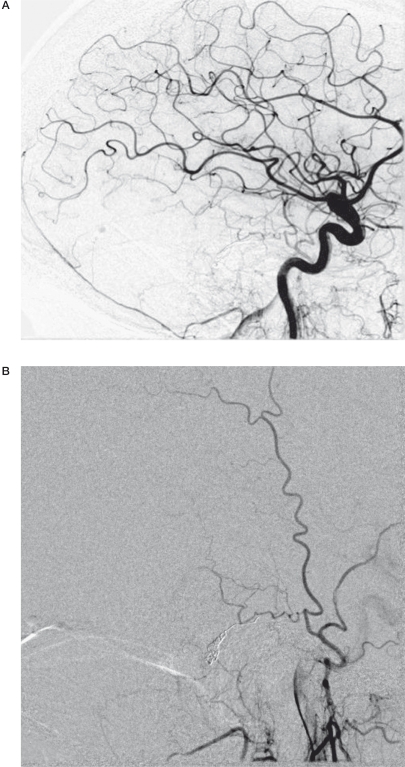
Figure 6.
A) A Selective microcatheter angiogram from DAVF pouch in frontal Towne projection showed the fistula. B) Right CCA angiogram in frontal towne projection showed the DAVF pouch.
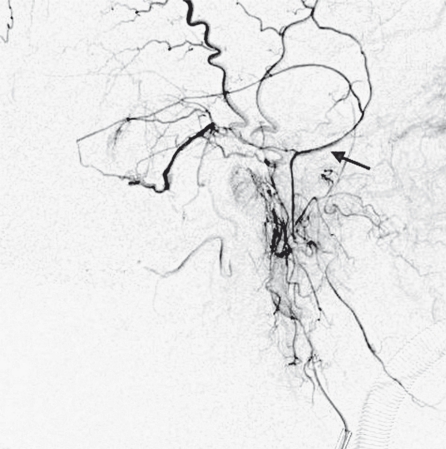
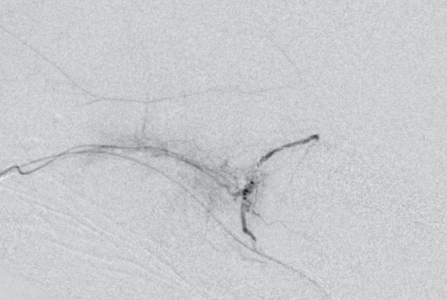
Figure 7.
The venous drainage was through the spinal perimedullary veins.
Figure 8.
A selective microcatheter angiogram in frontal Towne projection showed the completely packed DAVF pouch with Axium coils and Glubran.
Figure 9.
A selective microcatheter angiogram in lateral projection showed the completely packed DAVF pouch with Axium coils and Glubran.
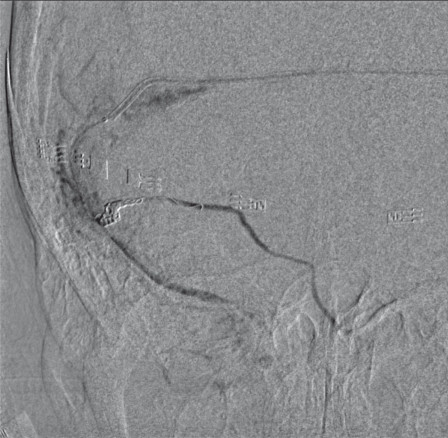
Figure 10.
A,B) Angiography performed immediately after embolization.
Figure 11.
MRI performed 9 months after embolization.
Discussion
The goal of DAVF treatment is to close the fistulous point and subsequently the perimedullary venous drainage to avoid or limit spinal cord damage secondary to the oedema due to venous drainage impairment, in an attempt to reverse clinical symptoms 3,4.
Due to the limited number of series published, it is difficult to create rigid guidelines in terms of the best endovascular treatment approach 1,4,5. The endovascular technique must be tailored to each particular case, but it is important to keep in mind that the possibility of treating a type V DAVF using the transvenous approach should not be discarded.
There is general agreement that endovascular treatment should be attempted first and surgery reserved for those intracranial DAVF with unsuccessful embolization or recurrence 3. The most frequent endovascular approach is through the arterial route, striving to bring the microcatheter as close as possible to the fistula pouch. Some cases have been reported with initially good results but with a high degree of recurrence. An inability to reach the fistula pouch with the embolization material explains many of these treatment failures. A deep understanding of the aetiology of the DAVF due to thrombosis of the venous sinuses and concepts based on anatomical distribution of the veins and sinuses raises the possibility of a transvenous approach, aiming to navigate across the thrombosed sinus and then through the fistulous point to the initial portion of the drainage vein 1. Few cases of this type of approach in type V DAVF have been published 1,4,5. In selected cases the transvenous approach may be helpful to increase the chance of success in the endovascular treatment of type V DAVF.
In the present patient, the main objective was to go through the thrombosed sinus to access the fistula pouch with the intention of closing it and the proximal vein, avoiding hypertension in the perimedullary veins. Another treatment option in the transvenous approach was to reopen the pathological venous sinus with angioplasty with or without stenting to restore the physiological venous drainage with normal flow restoration into the previously dilated perimedullary veins 3.
In our patient, failure in the first treatment was due to too proximal occlusion of the feeding artery, thus not achieving the occlusion of the fistulous point with the glue. Clinical symptoms improved due to the diminished flow to the fistula after the first embolization, but as soon as collateral arteries were recruited by the fistula, spinal cord venous drainage impairment led to the recurrence of symptoms. Transvenous access allowed us to close the fistula completely in a single session, with the pathologically inverted perimedullary venous flow completely disappearing. Finally it is important to have extensive knowledge of the embolization materials (particles, coils, onyx and n-butyl cyanoacrylate) in order to use them correctly depending on the different situations at the time of embolization. Surgical techniques are another treatment option, but thanks to technical development, they are reserved for difficult cases.
References
- 1.Cognard C, Gobin YP, Pierot L, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995;194:671–680. doi: 10.1148/radiology.194.3.7862961. [DOI] [PubMed] [Google Scholar]
- 2.Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995;82:166–179. doi: 10.3171/jns.1995.82.2.0166. [DOI] [PubMed] [Google Scholar]
- 3.Kiyosue H, Hori Y, Okahara M, et al. Treatment of intracranial dural arteriovenous fistulas: current strategies based on location and hemodynamics, and alternative techniques of trans-catheter embolization. Radiographics. 2004;24:1637–1653. doi: 10.1148/rg.246045026. [DOI] [PubMed] [Google Scholar]
- 4.Sugiura Y, Nozaki T, Sato H, et al. Sigmoid sinus dural arteriovenous fistula with spinal venous drainage manifesting as only brainstem-related neurological deficits without myelopathy. Neurol Med Chir (Tokyo) 2009;49:71–76. doi: 10.2176/nmc.49.71. [DOI] [PubMed] [Google Scholar]
- 5.Brunereau L, Gobin YP, Meder J-F, et al. Intracranial dural arteriovenous fistulas with spinal venous drainage: relation between clinical presentation and angiographic findings. Am J Neuroradiol. 1996;17:1549–1554. [PMC free article] [PubMed] [Google Scholar]
- 6.Lee C-W, Huang A, Wang Y-H, et al. Intracranial dural arteriovenous fistulas: diagnosis and evaluation with 64-detector row CT angiography. Radiology. 2010;256:219–228. doi: 10.1148/radiol.10091835. [DOI] [PubMed] [Google Scholar]
- 7.Wetzel SG, Bilecen D, Lyrer P, et al. Cerebral dural arteriovenous fistulas: detection by dynamic MR projection angiography. Am J Radiol. 2000;174:1293–1295. doi: 10.2214/ajr.174.5.1741293. [DOI] [PubMed] [Google Scholar]
- 8.Kwon BJ, Han MH, Kang HS, et al. MR Imaging findings of intracranial dural arteriovenous fistulas: relations with venous drainage patterns. Am J Neuroradiol. 2005;26:2500–2507. [PMC free article] [PubMed] [Google Scholar]
- 9.Cognard C, Januel AC, Silva NA, Jr, et al. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: new management using Onyx. Am J Neuroradiol. 2008;29:235–241. doi: 10.3174/ajnr.A0817. [DOI] [PMC free article] [PubMed] [Google Scholar]