Abstract
Objective
We sought to assess the relationship between patient cost sharing; medication adherence; and clinical, utilization, and economic outcomes.
Methodology:
We conducted a literature review of articles and abstracts published from January 1974 to May 2008. Articles were identified using PubMed, Ovid, medline, Web of Science, and Google Scholar databases. The following terms were used in the search: adherence, compliance, copay, cost sharing, costs, noncompliance, outcomes, hospitalization, utilization, economics, income, and persistence.
Results:
We identified and included 160 articles in the review. Although the types of interventions, measures, and populations studied varied widely, we were able to identify relatively clear relationships between cost sharing, adherence, and outcomes. Of the articles that evaluated the relationship between changes in cost sharing and adherence, 85% showed that an increasing patient share of medication costs was significantly associated with a decrease in adherence. For articles that investigated the relationship between adherence and outcomes, the majority noted that increased adherence was associated with a statistically significant improvement in outcomes.
Conclusion:
Increasing patient cost sharing was associated with declines in medication adherence, which in turn was associated with poorer health outcomes.
Keywords: adherence, cost sharing, copays, outcomes, compliance
INTRODUCTION
Health care spending in the U.S. has climbed to $2.2 trillion annually, up from $2.0 trillion in 2005.1,2 On a per-capita basis, this amounts to $7,400 spent per person per year and to employers’ costs of more than $9,300 for annual family coverage.3 Although these estimates are astonishing, they are not surprising—the growth in health care spending has been surpassing the growth of the overall economy for more than four decades.4 Of great interest, however, are the growth rates within health care service areas. High-growth services comprise the key targets for reform efforts by payers, purchasers, and other cost-conscious stakeholders within the health care system. Although prescription drugs are one of the “lower-ticket” service types (at 10% of total spending), they are one of those target areas.
Spending for drug therapies has increased by 89% since 2000, compared with a rate of only 67% for the “higher-ticket” hospital and physician services, which account for more than half of annual health care expenditures.2 Factors contributing to increased drug spending include not only higher prices for specialty and biotech therapies5 but also greater use of pharmaceuticals for a wider range of conditions and for longer periods to treat chronic illnesses.6 Thus, most efforts to control drug expenditures have targeted drug utilization by curbing demand for costly therapies via changes in drug coverage and in benefit design.
Strategies that have been commonly used to curb drug utilization include higher copayments, co-insurance plans, more restrictive formulary listings, and a move from branded products to less expensive generic brands through mandatory substitution. If these tools are implemented effectively, they can decrease costs by reducing the moral hazard of health insurance and by causing patients to realize the true cost of medications through their higher out-of-pocket expenses.
In theory, these steps should deter the overuse of nonessential therapies and should direct patients toward taking drugs that offer a therapeutic benefit at a lower cost, thus maximizing value. However, obtaining these results hinges on an important assumption—that high-value and low-value drugs can be differentiated and that patients will actively continue to use high-value drugs to receive the therapeutic benefit. If this assumption is met and if the links between uninterrupted medication use and future disease burden and costs are established, a greater value should be attained in the pharmacy benefit, along with, perhaps, a positive return on investment—particularly in conditions for which pharmaceuticals play a crucial role in effective disease management.7
There is a need, therefore, to examine the evidence base for support of these assumptions and presumed associations. Of particular interest is the question of whether cost sharing or other cost-containment techniques that shift the financial burden to patients lead to decreased adherence. If they do, to what extent are changes in adherence based on the degree of change in cost sharing?
A related question, if we assume that cost sharing affects adherence, is whether decreased adherence leads to poorer health outcomes. Although it is generally accepted that decreased adherence results in worse clinical outcomes, greater use of other health services, and higher costs,7 the results have been ambiguous in studies of patients who are not chronically ill.6 Moreover, with the new interest in personalized benefit designs that categorize patients and consider total costs of care, examining the existing body of evidence for these significant linkages has the potential to influence future benefit strategies aimed at achieving maximum value in all patient groups and to replace the “one-size-fits-all” approaches that emphasize cost-containment measures primarily.7,8
Our study sought to address these issues and to inform managed care decision makers who must consider the point at which additional cost shifting to patients adversely affects medication adherence and subsequent outcomes. To meet this objective, we conducted a comprehensive literature review to examine the effects of increased cost sharing on adherence and outcomes in patients with neurological, cardiovascular, mental health, metabolic, and pulmonary disorders. Although previous review articles have assessed aspects of the relationships of interest in earlier time periods, our review focuses on the most recent evidence for four distinct aspects:
whether increased cost sharing leads to decreased adherence
to what extent adherence is changed based on the degree of change in cost sharing
whether increased adherence results in improved clinical, utilization, and economic outcomes, irrespective of cost sharing
whether there was a link between cost sharing and health outcomes for studies in which cost sharing and outcomes were measured simultaneously
Ongoing primary research seeks to optimize value in a more concise and often treatment-specific approach, whereas our goal in summarizing the evidence was to translate valuable insights into lessons learned.
Study Selection
In 1975, a widely cited article by Roemer (“Copayments for ambulatory care: Penny-wise and pound-foolish”) was one of the first to evaluate the effects of cost sharing on the utilization of resources in a cohort of patients while applying statistical techniques to adjust for the critical differences between the cohort and controls.9 For our literature review, we evaluated articles published one year before the Roemer article (1975).
We identified articles and abstracts published from January 1974 to May 2008 using PubMed, Ovid, Medline, Web of Science, and Google Scholar databases. These articles included the following search terms: adherence, compliance, copay, cost sharing, costs, noncompliance, outcomes, hospitalization, utilization, economics, income, and persistence.
From the basket of studies with those terms, articles were excluded if they were published before 1974; did not address a chronic disease state; were not original empirical research; were published in a language other than English; did not relate cost sharing to medication adherence or outcomes; or analyzed study populations located outside the U.S. and Canada.
Study Classification
As a result of heterogeneity in the measurement of adherence and cost sharing, literature addressing the effect of cost sharing is somewhat diffuse. Medication adherence, for instance, is commonly defined in at least five ways, including the medication possession ratio, proportion of days covered, cumulative multiple-refill gap, number of prescriptions, and aggregate days supplied.10,11 Similarly, changes in cost sharing can occur by modifying the patient’s copayment, the rate of co-insurance, the deductible, or the number of formulary tiers. To be as comprehensive as possible, we accepted all of these definitions for the studies included in our assessment.
To examine the relationship between adherence and outcomes, we also included studies not directly linked to cost sharing. With or without the inclusion of a cost-sharing parameter, outcomes were classified into three domains:
Clinical outcomes were related to improvements in symptoms or changes in blood pressure (BP) or glycosylated hemoglobin (HbA1c) levels, for example.
Utilization outcomes included measures related to the use of health services such as emergency department (ED) visits, outpatient visits, hospitalizations, nursing-home admissions, readmissions, and length of stay.
Economic outcomes consisted of total health care costs, including pharmacy and medical costs.
RESULTS
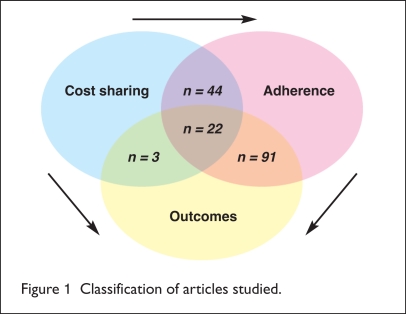
A total of 160 articles9,12–170 met the selection criteria and were included in the assessment; 66 articles (41%) evaluated the effect of cost sharing on medication adherence, and 113 articles (71%) evaluated the effect of adherence on outcomes. As shown in Figure 1, there was some overlap between the two categories of articles, allowing for direct assessment of the effect of cost sharing and outcomes. Of the 66 articles evaluating the effect of cost sharing on adherence, 22 also included outcomes within that assessment.
Figure 1.
Classification of articles studied.
In addition to these 22 articles, three articles evaluated cost sharing and outcomes (but not adherence), bringing the total number of articles evaluating the relationship between cost sharing and outcomes to 25.
Cost Sharing and Medication Adherence
Table 1 provides an overview of the characteristics of the articles assessing patient cost sharing and medication adherence. Most of the articles focused only on the relationship between cost sharing and adherence and did not assess effects on health outcomes; they were retrospective in nature and included data from commercially insured populations.
Table 1.
Characteristics of Articles Investigating Patient Cost-Sharing Amount and Medication Adherence
| Concept studied | |
| Impact of cost sharing on adherence | 44 (67%) |
| Impact of cost sharing on adherence and outcomes | 22 (33%) |
| Study design | |
| Retrospective | 56 (85%) |
| Prospective | 9 (14%) |
| Cross-sectional | 1 (2%) |
| Population studied | |
| Commercially insured | 57 (86%) |
| Medicare, other publicly insured | 9 (14%) |
| Treatment or disease area studied | |
| Cardiovascular | 20 (31%) |
| Diabetes | 5 (7%) |
| Mental health | 3 (4%) |
| Pulmonary | 3 (4%) |
| Arthritis | 2 (3%) |
| Infectious disease | 1 (2%) |
| Gastrointestinal disease | 2 (3%) |
| General | 30 (46%) |
| Adherence: operational definition | |
| Number of filled prescriptions over a set time period | 25 (38%) |
| Medication possession ratio (MPR) | 20 (30%) |
| Combination of number of refills and medication possession ratio | 2 (4%) |
| Patient self-report | 10 (15%) |
| Other (i.e., initiation, discontinuation, elasticity) | 8 (12%) |
| Relationship between cost sharing and adherence | |
| Statistically significant, inverse relationship | 56 (85%) |
| No relationship or no statistically significant relationship | 10 (15%) |
Overall, adherence was most commonly defined as the number of prescriptions filled over a specified time period (37.8%), the medication possession ratio (30.4%), or a combination of these measures (4.4%). In addition, 10 studies12–21 included patient self-reporting as the measure of adherence; the remaining studies used metrics such as initiation and discontinuation. All articles except two22,23 specifically assessed the effect of increased cost sharing on adherence. The remaining two studies assessed the effect of reduced copays for five drug classes23 and the effect of copay reductions on all diabetes medications.22
Of the 66 studies, 56 (85%) demonstrated a statistically significant relationship between increased patient cost sharing and decreased medication adherence.9,12–19,22–26,28–68,78 The remaining 10 studies (15%) demonstrated either limited or nonsignificant findings for the cost-sharing/adherence relationship (Table 1).27,69–77
Quantifying the relationship between changes in copays and patient cost sharing and changes in medication adherence was often complicated by the presence of other interventions during the same study period. For example, many studies included changes in the copay tier (e.g., from tier 2 to tier 3 or higher) along with changes in patient copay amounts. Other studies included a switch from copays to co-insurance along with introduction of a deductible based on the patient’s income status.
Similarly, many studies looked at multiple classes or a wide variety of patient types (e.g., new versus continuing users, different age groups) over long time periods to increase the sample size or to investigate how different characteristics might affect any identified relationship; however, these studies did not provide clear information about the actual changes in patient cost sharing within all patient subgroups to accurately assess the relationship between cost sharing and adherence.
After we excluded studies in which it was not possible to quantify a change in patient cost sharing or in medication adherence, 24 studies remained for further analysis. As shown in Table 2, there was still a wide variety of these articles in terms of populations studied, methods used, and final results. Of the 24 studies included in Table 2, 18 (75%) identified a statistically significant relationship between changes in patient cost sharing and medication adherence, although six studies did not. We could not identify any specific variables that explained the differences in results between these two groups of articles, although it appeared that the six studies with negative findings had tended to have more complex interventions (i.e., changes in cost sharing as well as other changes to benefit design), had targeted more motivated populations or essen tial medications (e.g., therapy for postmyocardial infarction), or had utilized different methodologies for defining adherence (i.e., with a focus on initiation or discontinuation rates vs. medication possession ratios).
Table 2.
Changes in Patient Cost-Sharing Amount and Adherence
| Lead Author | Year of Publication | Medication Classes Studied | Population | Change in Patient Cost-Sharing Amount | Change in Adherence |
|---|---|---|---|---|---|
| Roemer9 | 1975 | All | Medicaid | + $0.50 | −10% |
| Nelson35 | 1984 | All | Medicaid | + $0.50 | −15% |
| Harris30 | 1990 | All | Commercial HMO | + $1.50 | −11% |
| Ellis50 | 2004 | Lipid-lowering | Commercial | + $10.00 | −11% |
| Huskamp54 | 2005 | Antihypertensives, lipid-lowering, proton pump inhibitors | Commercial | + $8.00 | −10% |
| Landsman33 | 2005 | Nine common classes | Commercial | + $5.00 | −5% |
| Roblin57 | 2005 | Diabetes | Commercial | + $10.00 | −19% |
| Schultz45 | 2005 | Lipid-lowering | Commercial | + $15.00 | −10% |
| Bender46 | 2006 | Asthma | Retail pharmacy | + $15.00 | −2% |
| Cole42 | 2006 | ACE inhibitors, beta blockers for CHF | CHF patients receiving Medicare supplemental benefits | + $10.00 | −3% –2% |
| Gibson43 | 2006 | Lipid-lowering | Commercial | + $10.00 | −2% (new users) −3% (continuing users) |
| Goldman44 | 2006 | Lipid-lowering | Commercial | + $10.00 | −8% |
| Kessler32 | 2007 | 10 most common classes | Commercial | + $30.00 | −2% |
| Pedan64 | 2007 | Lipid-lowering | Retail pharmacy | + $10.00 | −2% |
| Zeber40 | 2007 | Schizophrenia | Veterans | + $7.00 | −12% |
| Chernew23 | 2008 | Five medication classes | Commercial | −$12.50 | +3% |
| Colombi63 | 2008 | Diabetes | Commercial | + $10.00 + $20.00 |
−7% −20% |
| Thiebaud61 | 2008 | Lipid-lowering | Pharmacy benefit manager | + $10.00 | −10% |
| Johnson27 | 1997 | 22 medication classes | Managed Medicare | + $3.50 | 0%* |
| Motheral71 | 2001 | Four medication classes | Commercial | + $25.00 | −7%* |
| Motheral72 | 1999 | All medications | Commercial | + $5.00 | +6%* |
| Pilote74 | 2002 | Beta blockers, ACE inhibitors, lipid-lowering, aspirin | Quebec (Canada) health insurance participants, hospitalized for post-myocardial infarction | + $20.00 | 0%* |
| Williams75 | 2007 | Inhaled corticosteroids | Commercial HMO | + $10.00 | −3%* |
| Blais76 | 2001 | Nitrates, antihypertensives, warfarin, benzodiazepines | Quebec (Canada) health insurance participants | + $20.00 | −2%* |
ACE = angiotensin-converting enzyme; CHF = congestive heart failure; HMO = health maintenance organization.
No statistically significant change.
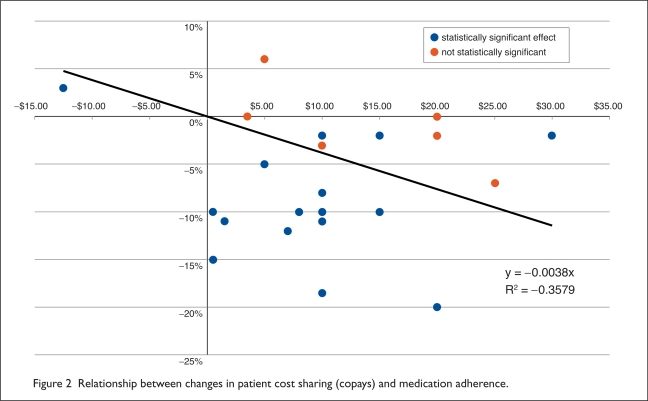
Given the wide variety of intervention types, study populations, and sample sizes, it was a challenge to summarize the studies to provide an estimate of the relationship between changes in patient cost sharing and medication adherence. Figure 2 (see page 48) depicts the results of Table 2 in graphic form, in an attempt to investigate the potential relationship between the two variables. As shown by the linear regression line fitted to the data, for each dollar increase in patient copays, adherence (as measured by these studies) would be expected to decrease by 0.4%. Thus, a $10 change would be expected to result in a 3.8% drop in adherence overall; however, as evidenced by the wide range of results included in the chart, the actual result of such a change might be larger or smaller, depending on the population and intervention affected.
Figure 2.
Relationship between changes in patient cost sharing (copays) and medication adherence.
Medication Adherence and Outcomes
Overall, 91 articles examined the relationship between medication adherence and outcomes (Table 3). Adherence in these studies was usually defined by calculating a medication possession ratio (45.1%) or the number of prescriptions filled over a specified time period (15.4%); however, 10 studies used patient self-reporting as the measure of adherence. Although the design for most studies examining adherence and outcomes was retrospective in nature (59.3%), 30 articles were either prospective studies or randomized clinical trials (33%). Most of the articles (63%) evaluated clinical outcomes (e.g., HbA1c, blood pressure), although a sizable number evaluated resource use or economic outcomes (e.g., medical and pharmacy costs).
Table 3.
Characteristics of Articles Investigating Medication Adherence and Treatment Outcomes
| No. of Articles | |
|---|---|
| Study design | |
| Retrospective | 54 (59%) |
| Prospective | 27 (30%) |
| Cross-sectional | 10 (11%) |
| Treatment or disease area studied | |
| Cardiovascular | 39 (43%)* |
| Diabetes | 18 (20%) |
| Mental health | 26 (29%) |
| Pulmonary | 14 (15%) |
| Type of treatment outcome studied | |
| Clinical outcomes | 57 (63%) |
| Resource use | 13 (14%) |
| Economic outcomes | 21 (23%) |
| Adherence: operational definition | |
| Medication possession ratio | 41 (45%) |
| Number of prescription refills in set time period | 14 (15%) |
| Patient self-report | 10 (11%) |
| Other | 26 (29%) |
Percentages may add up to more than 100% because of overlap of articles.
Table 4 presents an overview of the findings, stratified by disease state and type of treatment outcomes studied. Of the 57 articles exploring adherence and clinical outcomes, 49 (86%) found a positive relationship (increased adherence = improved outcome), one study (2%) found an inverse relationship, and seven studies (12%) did not detect any relationship.
Table 4.
Impact of Medication Adherence Changes on Treatment Outcomes, by Outcome Type and Disease Area Studied
| Clinical Outcomes | Resource Utilization | Economic Outcomes | ||||
|---|---|---|---|---|---|---|
| Total No. of Articles | Percentage With Positive Significant Relationship | Total No. of Articles | Percentage With Positive Significant Relationship | Total No. of Articles | Percentage With Positive Significant Relationship | |
| Diabetes | 10 | 80% | 6 | 100% | 7 | 86% |
| Hypertension | 11 | 73% | 3 | 100% | 3 | 67% |
| Coronary artery disease | 12 | 83% | 4 | 75% | 2 | 100% |
| Depression | 3 | 100% | 2 | 100% | 8 | 38% |
| Schizophrenia | 4 | 100% | 7 | 86% | 3 | 67% |
| Asthma or COPD | 9 | 67% | 10 | 70% | 1 | 100% |
| Postmyocardial infarction | 9 | 100% | 1 | 100% | — | — |
| Bipolar disorder | 4 | 75% | 2 | 50% | 1 | 100% |
| Congestive heart failure | 4 | 75% | 2 | 50% | 1 | 100% |
| Seizure disorder | 1 | 100% | — | — | — | — |
COPD = chronic obstructive pulmonary disease.
Similar trends were observed in articles addressing the relationship between adherence and utilization or economic outcomes. Most of the articles reported a positive relationship (improved adherence = improved outcomes); a few articles detected a negative relationship. Within utilization outcomes, 81% were significantly positive, 3% were significantly negative, and 16% were neutral. Within economic outcomes, 57% were significantly positive, 14% were significantly negative, and 29% were neutral.
We did not identify any other obvious traits that distinguished between studies that found or did not find a positive relationship between adherence and outcomes, and no differences existed with respect to the article’s publication year, sample size, operational definitions, or research methodology. As in any study of health care resource utilization and outcomes, it is likely that a number of unmeasured effects might have affected some analyses more than others; however, given that most studies revealed similar results, the relationship between adherence and outcomes does appear to be measurable.
Cost Sharing and Outcomes
Twenty-five studies directly assessed the association between cost sharing and outcomes.9,12,16–18,20–22,24–27,40–45,63,69–71,74,75,79 All studies except three20,21,79 included an assessment of medication adherence. The majority of studies (14 of 25, or 56%) examined more than one therapeutic class, whereas seven studies assessed cardiovascular treatments,17,18,42–45, 74 two evaluated diabetes treatment,16,63 one covered arthritis,41 and one examined asthma.75 We examined the effect of cost sharing for these therapies for a wide array of non-medication outcomes, including medical costs, adverse events, self-reported health status, and symptoms, as well as ED visits, outpatient visits, office visits, preventive services, hospitalizations, and nursing-home admissions.
Overall, 19 of 25 studies (76%) indicated that increased patient cost sharing adversely affected outcomes. The remaining six studies indicated that an increase in cost sharing did not affect medical utilization or the number of medical visits27,69–71,74,75 or costs.27,43,70 A study by Kephart et al.39 indicated that increased patient cost sharing was associated with increased hospital and ED admissions, with no effect on total costs.
In the evaluation of the six studies that demonstrated no effect on outcomes, five found that adherence was not significantly affected by an increase in cost sharing.69–71,74,75 Given the hypothesis that the effect of cost sharing on outcomes is mediated through adherence, it is conceivable that outcomes should not be affected in these studies, because adherence was not affected. However, Johnson et al.27 found that an increase in copays adversely affected adherence without any consistent negative impact on medical care utilization (i.e., office and ED visits and hospitalizations) or non-drug medical care expenditures resulting from copay increases. In the Johnson study, initial periods of increased cost sharing in one population were associated with a negative effect on medical care utilization; however, subsequent increases showed no effect.
DISCUSSION
Our literature review evaluated the relationship between patient cost sharing, medication adherence, and outcomes in terms of four aspects:
whether more cost sharing results in less adherence
to what extent adherence is changed according to the degree of change in cost sharing
whether increased adherence leads to improved clinical, utilization, and economic outcomes, irrespective of patient cost sharing
whether there is a relationship between cost sharing and outcomes for studies in which cost sharing and outcomes were measured simultaneously
Approximately 85% of studies that examined changes in patient cost sharing revealed that increasing cost sharing had a negative effect on adherence. When analyzing the effect of cost sharing on adherence in studies involving changes in cost sharing and adherence estimates, we noted a wide variation in measured effects, possibly a result of differences in underlying populations, methods, and operational definitions. However, the overall trend was an inverse relationship; for all increases in cost sharing, an expected decrease in adherence could be expected.
When studies assessing adherence and outcomes were evaluated, irrespective of cost sharing, the preponderance of evidence supported a significant positive relationship between changes in adherence and changes in treatment outcomes, irrespective of type of outcome (clinical, resource use, or economic) or disease state (cardiovascular, respiratory, or mental health).
It still needs to be determined, as Roehmer et al. asked, whether increasing cost sharing is “penny-wise and pound-foolish.”9 Our study and similar earlier reviews highlight the fact that increasing cost sharing decreases adherence and adversely affects outcomes. Yet the underlying premise of this strategy—overall cost reduction—has been neither supported nor refuted. Almost half of the studies included in the assessment showed a beneficial effect on economic outcomes, although, by far, it was in this domain that the literature was the most sparse.
To resolve this question, we recommend future studies that can assess reductions in pharmacy costs against the potential increased expense resulting from the additional use of health care resources and total medical costs. Research should also continue to evaluate when and how increased patient cost sharing is beneficial and when it is deleterious, as a one-size-fits-all approach is usually not the right solution. For example, the result of increased cost sharing for a “silent” condition such as diabetes may differ greatly from that for a symptomatic condition, such as chronic obstructive pulmonary disease (COPD). Basic economic theory leads us to believe that a patient’s income and the number of medications being filled, and paid for, can also have a substantial effect.
Our review indicates that a broad approach is generally not supported by the literature; further, success is more likely if we can develop better cost-sharing strategies to ensure that patients will receive the best value for the drugs that they buy and if we can capitalize on established relationships between out-of-pocket costs, adherence, and outcomes. Indeed, approaching benefit design using a scalpel, rather than an ax, may result in increased value not only for the pharmacy benefit but also for the wide range of coverage for health care services.
STUDY LIMITATIONS
As with most types of studies, literature reviews are not without limitations. Publication bias may exist when only a few studies that show no effect among the relationships of interest are available. The articles identified in this review covered a wide range of patient populations, interventions, and methodologies. In many instances, the effect of changes in patient cost sharing was heavily intertwined with other interventions that were introduced at the same time—the result of conducting research in a real-world setting. This situation often inhibits the ability to directly quantify the effect of increased copays on adherence.
The relationship between cost sharing and medication adherence can be affected by other factors, such as the patient’s underlying disease state. For example, patients being treated for symptomatic conditions are more likely to remain more adherent, even with changes in cost sharing, than patients with less apparent or less severe symptoms. Although some articles attempted to address this difference by categorizing treatments, neither the categories nor the methods were consistent for all articles.
Despite these limitations, our review of the available literature, as well as the general trend of the results observed, suggests that managed care decision makers should carefully consider the implications of increased cost sharing in each subgroup within their specific populations.
CONCLUSION
With health care spending projected to exceed 20% of the U.S. gross domestic product by 2018,4 with more than 75% of all employees subject to a tier 3 or tier 4 pharmacy benefit,3 and with more than 40% of employers stating that they are likely to raise employees’ out-of-pocket costs for prescription drugs in 2012, our findings have particular relevance. Health care decision makers are undoubtedly planning to continue increasing the level of patient cost sharing for prescription drugs to slow the rising costs of health care; however, this approach may be shortsighted and counterproductive because increases in medical utilization attributable to poorer outcomes may outweigh the savings from lower prescription drug use, particularly when results for the total cost of care are evaluated over long periods of time.7
Footnotes
Disclosure: GlaxoSmithKline provided funding for this literature review. Dr. Eaddy and Dr. O’Day are employees of Xcenda, a consultant of GlaxoSmithKline, which sponsored the study from which the data in the manuscript were derived. Dr. Cook, Dr. Burch, and Dr. Cantrell report that they have no financial or commercial relationships in regard to this article.
REFERENCES
- 1.Caitlin A, Cowan C, Heffler S, Washington B. National health spending in 2005: The slowdown continues. Health Aff (Millwood) 2007;26:142–153. doi: 10.1377/hlthaff.26.1.142. [DOI] [PubMed] [Google Scholar]
- 2.Henry J, Kaiser Family Foundation . Mar, 2009. Health care costs: A primer. Available at: www.kff.org/insurance/7670.cfm. Accessed August 30, 2011. [Google Scholar]
- 3.Henry J, Kaiser Family Foundation and Health Research and Educational Trust . Employer Health Benefits: 2008 Summary of Findings. Available at: ehbs.kff.org/images/abstract/7791/pdf. Accessed August 30, 2011. [Google Scholar]
- 4.Henry J, Kaiser Family Foundation . Fact sheet. Mar, 2009. Trends in healthcare costs and spending. Available at: www.kff.org/insurance/7692.cfm. Accessed August 30, 2011. [Google Scholar]
- 5.Bach PB. Limits on Medicare’s ability to control rising spending on cancer drugs. JAMA. 2009;360:626–633. doi: 10.1056/NEJMhpr0807774. [DOI] [PubMed] [Google Scholar]
- 6.Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: Associations with medication and medical utilization and spending and health. JAMA. 2007;298:61–69. doi: 10.1001/jama.298.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hom D, Mahoney J, Wells K, Lednar W. Leading employers share strategies for managing promising, high-cost biotech medications. Am J Manag Care. 2008;14:S264–S268. [PubMed] [Google Scholar]
- 8.Hodge B, Martin M. Benefit design critical to protecting out-of-pocket costs for employees. Am J Manag Care. 2008;14:S246–S251. [PubMed] [Google Scholar]
- 9.Roemer MI, Hopkins CE, Carr L, Gartside F. Copayments for ambulatory care: Penny-wise and pound-foolish. Med Care. 1975;13:457–466. doi: 10.1097/00005650-197506000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Sikka R, Xia F, Aubert RE. Estimating medication adherence using administrative claims data. Am J Manag Care. 2005;11:449–457. [PubMed] [Google Scholar]
- 11.Hess LM, Raebel MA, Conner DA, Malone DC. Measurement of adherence in pharmacy administrative databases: A proposal for standard definitions and preferred measures. Ann Pharmacother. 2006;40:1280–1288. doi: 10.1345/aph.1H018. [DOI] [PubMed] [Google Scholar]
- 12.Mojtabai R, Olfson M. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Aff (Millwood) 2003;22:220–229. doi: 10.1377/hlthaff.22.4.220. [DOI] [PubMed] [Google Scholar]
- 13.Stuart B, James G. Ability to pay and the decision to medicate. Med Care. 1998;36:202–211. doi: 10.1097/00005650-199802000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Tseng CW, Brook RH, Keeler E, et al. Cost-lowering strategies used by Medicare beneficiaries who exceed drug benefit caps and have a gap in drug coverage. JAMA. 2004;292:952–960. doi: 10.1001/jama.292.8.952. [DOI] [PubMed] [Google Scholar]
- 15.Reed M, Brand R, Newhouse JP, et al. Coping with prescription drug cost sharing: Knowledge, adherence, and financial burden. Health Serv Res. 2008;43:785–797. doi: 10.1111/j.1475-6773.2007.00797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Piette JD, Wagner TH. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care. 2004;42:102–109. doi: 10.1097/01.mlr.0000108742.26446.17. [DOI] [PubMed] [Google Scholar]
- 17.Rahimi AR, Spertus JA, Reid KJ, et al. Financial barriers to health-care and outcomes after acute myocardial infarction. JAMA. 2007;297:1063–1072. doi: 10.1001/jama.297.10.1063. [DOI] [PubMed] [Google Scholar]
- 18.Schoen MD, DiDomenico RJ, Connor SE, et al. Impact of the cost of prescription drugs on clinical outcomes and indigent patients with heart disease. Pharmacotherapy. 2001;31:1455–1463. doi: 10.1592/phco.21.20.1455.34473. [DOI] [PubMed] [Google Scholar]
- 19.Piette JD, Heisler M, Wagner TH. Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care. 2004;27:384–391. doi: 10.2337/diacare.27.2.384. [DOI] [PubMed] [Google Scholar]
- 20.Carlson MJ, DeVoe J, Wright BJ. Short-term impacts of coverage loss in a Medicaid population: Early results from a prospective cohort study of the Oregon Health Plan. Ann Fam Med. 2006;4:391–398. doi: 10.1370/afm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heisler M, Langa KM, Eby EL, et al. The health effects of restricting prescription medication use because of cost. Med Care. 2004;42:626–634. doi: 10.1097/01.mlr.0000129352.36733.cc. [DOI] [PubMed] [Google Scholar]
- 22.Mahoney JJ. Reducing patient drug acquisition costs can lower diabetes health claims. Am J Manag Care. 2005;11:S170–S176. [PubMed] [Google Scholar]
- 23.Chernew ME, Shah MR, Wegh A, et al. Impact of decreasing co-payments on medication adherence within a disease management environment. Health Aff (Millwood) 2008;27:103–112. doi: 10.1377/hlthaff.27.1.103. [DOI] [PubMed] [Google Scholar]
- 24.Christian-Herman J, Emons M, George D. Effects of generic-only drug coverage in a Medicare HMO. Health Aff (Millwood) Sep 29, 2004. Web exclusive. Available at: http://content.healthaffairs.org/content/early/2004/09/29/hlthaff.w4.455.citation. Accessed August 30, 2011. [DOI] [PubMed]
- 25.Hsu J, Price M, Huang J, et al. Unintended consequences of caps on Medicare drug benefits. N Engl J Med. 2006;354:2349–2359. doi: 10.1056/NEJMsa054436. [DOI] [PubMed] [Google Scholar]
- 26.Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285:421–429. doi: 10.1001/jama.285.4.421. [DOI] [PubMed] [Google Scholar]
- 27.Johnson RE, Goodman MJ, Hornbrook MC, Eldredge MB. The effect of increased prescription drug cost-sharing on medical care utilization and expenses of elderly health maintenance organization members. Med Care. 1997;35:1119–1131. doi: 10.1097/00005650-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Artz MB, Hadsall RS, Schondelmeyer SW. Impact of generosity level of outpatient prescription drug coverage on prescription drug events and expenditure among older persons. Am J Public Health. 2002;92:1257–1263. doi: 10.2105/ajph.92.8.1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldman DP, Joyce GF, Escarce JJ, et al. Pharmacy benefits and the use of drugs by the chronically ill. JAMA. 2004;291:2344–2350. doi: 10.1001/jama.291.19.2344. [DOI] [PubMed] [Google Scholar]
- 30.Harris BL, Stergachis A, Ried LD. The effect of drug co-payments on utilization and cost of pharmaceuticals in a health maintenance organization. Med Care. 1990;28:907–917. doi: 10.1097/00005650-199010000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Hillman AL, Pauly MV, Escarce JJ, et al. Financial incentives and drug spending in managed care. Health Aff (Millwood) 1999;2:189–200. doi: 10.1377/hlthaff.18.2.189. [DOI] [PubMed] [Google Scholar]
- 32.Kessler RC, Cantrell CR, Berglund P, Sokol M. The effects of copayments on medication adherence during the first two years of prescription drug treatment. J Occup Environ Med. 2007;49:597–609. doi: 10.1097/JOM.0b013e318057772b. [DOI] [PubMed] [Google Scholar]
- 33.Landsman PB, Yu W, Liu X, et al. Impact of 3-tier pharmacy benefit design and increased consumer cost-sharing on drug utilization. Am J Manag Care. 2005;11:621–628. [PubMed] [Google Scholar]
- 34.Nair KV, Wolfe P, Valuck RJ, et al. Effects of a 3-tier pharmacy benefit design on the prescription purchasing behavior of individuals with chronic disease. J Manag Care Pharm. 2003;9:123–133. doi: 10.18553/jmcp.2003.9.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nelson AA, Reeder CE, Dickson WM. The effect of a Medicaid drug copayment program on the utilization and cost of prescription services. Med Care. 1984;22:724–736. doi: 10.1097/00005650-198408000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Shrank WH, Hoang T, Ettner SL, et al. The implications of choice: Prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditions. Arch Intern Med. 2006;166:332–337. doi: 10.1001/archinte.166.3.332. [DOI] [PubMed] [Google Scholar]
- 37.Thomas CP, Wallack SS, Lee S, Ritter GA. Impact of health plan design and management on retirees’ prescription drug use and spending, 2001. Health Aff (Millwood) Dec 4, 2002. Web exclusive. Available at: http://content.healthaffairs.org/content/early/2002/12/04/hlthaff.w2.408.citation. Accessed August 30, 2011. [DOI] [PubMed]
- 38.Gilman BH, Kautter J. Impact of multi-tiered copayments on the use and cost of prescription drugs among Medicare beneficiaries. Health Serv Res. 2008;43:478–495. doi: 10.1111/j.1475-6773.2007.00774.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kephart G, Skedgel C, Sketris I, et al. Effect of copayments on drug use in the presence of annual payment limits. Am J Manag Care. 2007;13:328–334. [PubMed] [Google Scholar]
- 40.Zeber JE, Grazier KL, Valenstein M, et al. Effect of a medication copayment increase in veterans with schizophrenia. Am J Manag Care. 2007;13:335–346. [PubMed] [Google Scholar]
- 41.Anis AH, Guh DP, Lacaille D, et al. When patients have to pay a share of drug costs: Effects on frequency of physician visits, hospital admissions and filling of prescriptions. Can Med Assoc J. 2005;173:1335–1340. doi: 10.1503/cmaj.045146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cole JA, Norman H, Weatherby LB, Walker AM. Drug copayment and adherence in chronic heart failure: Effect on cost and outcomes. Pharmacother. 2006;26:1157–1164. doi: 10.1592/phco.26.8.1157. [DOI] [PubMed] [Google Scholar]
- 43.Gibson TB, Mark TL, Axelsen K, et al. Impact of statin copayments on adherence and medical care utilization and expenditures. Am J Manag Care. 2006;12 (Spec. No. SP11–19). [PubMed] [Google Scholar]
- 44.Goldman DP, Joyce GF, Karaca-Mandic P. Varying pharmacy benefits with clinical status: The case of cholesterol-lowering therapy. Am J Manag Care. 2006;12:21–28. [PubMed] [Google Scholar]
- 45.Schultz JS, O’Donnell JC, McDonough KL, et al. Determinants of compliance with statin therapy and low-density lipoprotein cholesterol goal attainment in a managed care population. Am J Manag Care. 2005;11:306–312. [PubMed] [Google Scholar]
- 46.Bender BG, Pedan A, Varasteh LT. Adherence and persistence with fluticasone proprionate/salmeterol combination therapy. J Allergy Clin Immunol. 2006;118:899–904. doi: 10.1016/j.jaci.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 47.Blais L, Couture J, Rahme E, LeLorier J. Impact of a cost sharing drug insurance plan on drug utilization among individuals receiving social assistance. Health Policy. 2003;64:163–172. doi: 10.1016/s0168-8510(02)00158-6. [DOI] [PubMed] [Google Scholar]
- 48.Briesacher B, Kamal-Bahl S, Hochberg M, et al. Three-tiered co-payment drug coverage and use of nonsteroidal anti-inflammatory drugs. Arch Intern Med. 2004;164:1679–1684. doi: 10.1001/archinte.164.15.1679. [DOI] [PubMed] [Google Scholar]
- 49.Dormuth CR, Glynn RJ, Neumann P, et al. Impact of two sequential drug cost-sharing policies on the use of inhaled medications in older patients with chronic obstructive pulmonary disease or asthma. Clin Ther. 2006;28:964–978. doi: 10.1016/j.clinthera.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 50.Ellis JJ, Erickson SR, Stevenson JG, et al. Suboptimal statin adherence on discontinuation in primary and secondary prevention populations. J Gen Intern Med. 2004;19:638–645. doi: 10.1111/j.1525-1497.2004.30516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Foxman B, Valdez RB, Lohr KN, et al. The effect of cost-sharing on the use of antibiotics in ambulatory care: Results from a population-based randomized controlled trial. J Chron Dis. 1987;40:429–437. doi: 10.1016/0021-9681(87)90176-7. [DOI] [PubMed] [Google Scholar]
- 52.Gibson TB, Mark TL, McGuigan KA, et al. The effects of prescription drug copayments on statin adherence. Am J Manag Care. 2005;11:730–740. [PubMed] [Google Scholar]
- 53.Huskamp HA, Deverka PA, Epstein AM, et al. The effect of incentive-based formularies on prescription-drug utilization and spending. N Engl J Med. 2003;349:2224–2232. doi: 10.1056/NEJMsa030954. [DOI] [PubMed] [Google Scholar]
- 54.Huskamp HA, Deverka PA, Epstein AM, et al. Impact of 3-tier formularies on drug treatment of attention-deficit/hyperactivity disorder in children. Arch Gen Psychiatry. 2005;62:435–441. doi: 10.1001/archpsyc.62.4.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kamal-Bahl S, Briesacher B. How do incentive-based formularies influence drug selection and spending for hypertension? Health Aff (Millwood) 2004;23:227–236. doi: 10.1377/hlthaff.23.1.227. [DOI] [PubMed] [Google Scholar]
- 56.Rector TS, Finch MD, Danzon PM, et al. Effect of tiered prescription copayments on the use of preferred brand medications. Med Care. 2003;41:398–406. doi: 10.1097/01.MLR.0000053022.47132.82. [DOI] [PubMed] [Google Scholar]
- 57.Roblin DW, Platt R, Goodman MJ, et al. Effect of increased cost-sharing on oral hypoglycemic use in five managed care organizations. Med Care. 2005;43:951–959. doi: 10.1097/01.mlr.0000178216.23514.b7. [DOI] [PubMed] [Google Scholar]
- 58.Schneeweiss S, Maclure M, Soumerai SB. Prescription duration after drug copay changes in older people: Methodological aspects. J Am Geriatr Soc. 2002;50:521–525. doi: 10.1046/j.1532-5415.2002.50120.x. [DOI] [PubMed] [Google Scholar]
- 59.Schneeweiss S, Patrick AR, Maclure M, et al. Adherence to statin therapy under drug cost sharing in patients with and without acute myocardial infarction: A population-based natural experiment. Circulation. 2007;115:2128–2135. doi: 10.1161/CIRCULATIONAHA.106.665992. [DOI] [PubMed] [Google Scholar]
- 60.Taira DB, Wong KS, Frech-Tamas F, Chung RS. Copayment level and compliance with antihypertensive medication: Analysis and policy implications for managed care. Am J Manag Care. 2006;12:678–683. [PubMed] [Google Scholar]
- 61.Thiebaud P, Patel BV, Nichol MB. The demand for statin: The effect of copay on utilization and compliance. Health Econ. 2008;17:83–97. doi: 10.1002/hec.1245. [DOI] [PubMed] [Google Scholar]
- 62.Briesacher BA, Limcangco MR, Frech-Tamas F. New-user persistence with antihypertensives and prescription drug cost-sharing. J Clin Hypertens. 2007;9:831–836. doi: 10.1111/j.1524-6175.2007.06651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Colombi AM, Yu-Isenberg K, Priest J. The effects of health plan copayments on adherence to oral diabetes medication and health resource utilization. J Occup Environ Med. 2008;50:535–541. doi: 10.1097/JOM.0b013e31816ed011. [DOI] [PubMed] [Google Scholar]
- 64.Pedan A, Varasteh L, Schneeweiss S. Analysis of factors associated with statin adherence in a hierarchical model considering physician, pharmacy, patient, and prescription characteristics. J Manag Care Pharm. 2007;13:487–496. doi: 10.18553/jmcp.2007.13.6.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schneeweiss S, Patrick AR, Maclure M, et al. Adherence to beta-blocker therapy under drug cost-sharing in patients with and without acute myocardial infarction. Am J Manag Care. 2007;13:445–452. [PMC free article] [PubMed] [Google Scholar]
- 66.Ungar WJ, Kozyrskyj A, Paterson M, Ahmad F. Effect of cost-sharing on use of asthma medication in children. Arch Pediatr Adolesc Med. 2008;162:104–110. doi: 10.1001/archpediatrics.2007.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ye X, Gross CR, Schommer J, et al. Association between copayment and adherence to statin treatment initiated after coronary heart disease hospitalization: A longitudinal, retrospective, cohort study. Clin Ther. 2007;29:2748–2757. doi: 10.1016/j.clinthera.2007.12.022. [DOI] [PubMed] [Google Scholar]
- 68.Ye X, Gross CR, Schommer J, et al. Initiation of statins after hospitalization for coronary heart disease. J Manag Care Pharm. 2007;13:385–396. doi: 10.18553/jmcp.2007.13.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fairman KA, Motheral BR, Henderson RR. Retrospective, long-term follow-up study of the effect of a three-tier prescription drug copayment system on pharmaceutical and other medical utilization and costs. Clin Ther. 2003;25:3147–3161. doi: 10.1016/s0149-2918(03)90099-3. [DOI] [PubMed] [Google Scholar]
- 70.Johnson RE, Goodman MJ, Hornbrook MC, Eldredge MB. The impact of increasing patient prescription drug cost sharing on therapeutic classes of drugs received and on the health status of elderly HMO members. Health Serv Res. 1997;32:103–121. [PMC free article] [PubMed] [Google Scholar]
- 71.Motheral B, Fairman KA. Effect of a three-tier prescription copay on pharmaceutical and other medical utilization. Med Care. 2001;39:1293–1304. doi: 10.1097/00005650-200112000-00005. [DOI] [PubMed] [Google Scholar]
- 72.Motheral BR, Henderson R. The effect of a copay increase on pharmaceutical utilization, expenditures, and treatment continuation. Am J Manag Care. 1999;5:1383–1394. [PubMed] [Google Scholar]
- 73.Huskamp HA, Deverka PA, Landrum MB, et al. The effect of three-tier formulary adoption on medication continuation and spending among elderly retirees. Health Serv Res. 2007;42:1926–1942. doi: 10.1111/j.1475-6773.2007.00722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pilote L, Beck C, Richard H, Eisenberg MJ. The effects of cost-sharing on essential drug prescriptions, utilization of medical care, and outcomes after acute myocardial infarction in elderly patients. Can Med Assoc J. 2002;67:246–252. [PMC free article] [PubMed] [Google Scholar]
- 75.Williams LK, Joseph CL, Peterson EL, et al. Race-ethnicity, crime, and other factors associated with adherence to inhaled corticosteroids. J Allergy Clin Immunol. 2007;119:168–175. doi: 10.1016/j.jaci.2006.09.029. [DOI] [PubMed] [Google Scholar]
- 76.Blais L, Boucher JM, Couture J, et al. Impact of a cost-sharing drug insurance plan on drug utilization among older people. J Am Geriatr Soc. 2001;49:410–414. doi: 10.1046/j.1532-5415.2001.49084.x. [DOI] [PubMed] [Google Scholar]
- 77.LaFleur J, Thompson CJ, Joish VN, et al. Adherence and persistence with single-dosage form extended-release niacin/lovastatin compared with statins alone or in combination with extended-release niacin. Ann Pharmacother. 2006;40:1274–1279. doi: 10.1345/aph.1G646. [DOI] [PubMed] [Google Scholar]
- 78.Brixner DI, Joish VN, Odera GM, et al. Effects of benefit design change across 5 disease states. Am J Manag Care. 2007;13:370–376. [PubMed] [Google Scholar]
- 79.Cecil WT, Barnes J, Shea T, Coulter S. Relationship of the use and costs of physician office visits and prescription drugs to travel distance and increases in member cost share. J Manag Care Pharm. 2006;12:665–676. doi: 10.18553/jmcp.2006.12.8.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Andrade SE, Saperia GM, Berger ML, Platt R. Effectiveness of antihyperlipidemic drug management in clinical practice. Clin Ther. 1999;21:1973–1987. doi: 10.1016/S0149-2918(00)86743-0. [DOI] [PubMed] [Google Scholar]
- 81.Asher-Svanum A, Faires DE, Zhu B, et al. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry. 2006;67:453–460. doi: 10.4088/jcp.v67n0317. [DOI] [PubMed] [Google Scholar]
- 82.Ascher-Svanum H, Nyhuis AW, Faries DE, et al. Clinical, functional, and economic ramifications of early nonresponse to antipsychotics in the naturalistic treatment of schizophrenia. Schizophrenia Bull. 2008;34(6):1163–1171. doi: 10.1093/schbul/sbm134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Batal HA, Krantz MJ, Dale RA, et al. Impact of prescription size on statin adherence and cholesterol levels. BMC Health Serv Res. 2007;7:175. doi: 10.1186/1472-6963-7-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bauman LJ, Wright E, Leickly FE, et al. Relationship of adherence to pediatric asthma morbidity among inner-city children. Pediatrics. 2002;110(1):e6–e7. doi: 10.1542/peds.110.1.e6. [DOI] [PubMed] [Google Scholar]
- 85.Bouchard MH, Dragomir A, Blais L, et al. Impact of adherence to statins on coronary artery disease in primary prevention. Br J Clin Pharmacol. 2007;63:698–708. doi: 10.1111/j.1365-2125.2006.02828.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bramley TJ, Gerbino PP, Nightengale BS, Frech-Tamas F. Relationship of blood pressure control to adherence with antihypertensive monotherapy in 13 managed care organizations. J Manag Care Pharm. 2006;12:239–245. doi: 10.18553/jmcp.2006.12.3.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bunting BA, Cranor CW. The Asheville Project: Long-term clinical, humanistic, and economic outcomes of a community-based medication therapy management program for asthma. J Am Pharm Assoc. 2006;46:133–138. doi: 10.1331/154434506776180658. [DOI] [PubMed] [Google Scholar]
- 88.Burton WN, Chen C, Conti DJ, et al. The association of anti-depressant medication adherence with employee disability absences. Am J Manag Care. 2007;13:105–112. [PubMed] [Google Scholar]
- 89.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: Impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 90.Cramer JA, Glassman M, Rienzi V. The relationship between poor medication compliance and seizures. Epilepsy Behav. 2002;3:338–342. doi: 10.1016/s1525-5050(02)00037-9. [DOI] [PubMed] [Google Scholar]
- 91.DelBello MP, Hanseman D, Adler CM, et al. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry. 2007;164:582–590. doi: 10.1176/ajp.2007.164.4.582. [DOI] [PubMed] [Google Scholar]
- 92.Dunayevich E, Ascher-Svanum H, Zhao F, et al. Longer time to antipsychotic treatment discontinuation for any cause is associated with better functional outcomes for patients with schizophrenia, schizophreniform disorder, or schizoaffective disorder. J Clin Psych. 2007;68:1163–1171. doi: 10.4088/jcp.v68n0801. [DOI] [PubMed] [Google Scholar]
- 93.Fung V, Huang J, Brand R, et al. Hypertension treatment in a Medicare population: Adherence and systolic blood pressure control. Clin Ther. 2007;29:972–984. doi: 10.1016/j.clinthera.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 94.Gallagher JE, Viscoli CM, Horwitz RI. The relationship of treatment adherence to the risk of death after myocardial infarction in women. JAMA. 1993;270:742–744. [PubMed] [Google Scholar]
- 95.Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: The Heart and Soul Study. Arch Intern Med. 2007;167:1798–1803. doi: 10.1001/archinte.167.16.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Glynn RJ, Buring JE, Manson JE, et al. Adherence to aspirin in the prevention of myocardial infarction. Arch Intern Med. 1994;154:2649–2657. doi: 10.1001/archinte.1994.00420230032005. [DOI] [PubMed] [Google Scholar]
- 97.Ho P, Fihn S, Wang L, et al. Clopidogrel and long-term outcomes after stent implantation for acute coronary syndrome. Am Heart J. 2007;154:846–851. doi: 10.1016/j.ahj.2007.08.028. [DOI] [PubMed] [Google Scholar]
- 98.Ho PM, Magid DJ, Shetterly SM, et al. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008;155:772–779. doi: 10.1016/j.ahj.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 99.Ho PM, Magid DJ, Shetterly SM, et al. Importance of therapy intensification and medication nonadherence for blood pressure control in patients with coronary disease. Arch Intern Med. 2008;168:271–276. doi: 10.1001/archinternmed.2007.72. [DOI] [PubMed] [Google Scholar]
- 100.Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication non-adherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 101.Ho PM, Spertus JA, Masoudi FA, et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. 2006;166:1842–1847. doi: 10.1001/archinte.166.17.1842. [DOI] [PubMed] [Google Scholar]
- 102.Horwitz RI, Viscoli CM, Berkman L, et al. Treatment adherence and risk of death after myocardial infarction. Lancet. 1990;336:542–545. doi: 10.1016/0140-6736(90)92095-y. [DOI] [PubMed] [Google Scholar]
- 103.Jackevicius CA, Li P, Tu JV. Prevalence, predictors, and outcomes of primary nonadherence after acute myocardial infarction. Circulation. 2008;117:1028–1036. doi: 10.1161/CIRCULATIONAHA.107.706820. [DOI] [PubMed] [Google Scholar]
- 104.Keck PE, McElroy SL, Strakowski SM, et al. 12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J Psychiatry. 1998;155:646–652. doi: 10.1176/ajp.155.5.646. [DOI] [PubMed] [Google Scholar]
- 105.Kimmel SE, Chen Z, Price M, et al. The influence of patient adherence on anticoagulation control with warfarin: Results from the International Normalized Ratio Adherence and Genetics (IN-RANGE) Study. Arch Intern Med. 2007;167:229–235. doi: 10.1001/archinte.167.3.229. [DOI] [PubMed] [Google Scholar]
- 106.Krapek K, King K, Warren SS, et al. Medication adherence and associated hemoglobin A1c in type 2 diabetes. Ann Pharmacother. 2004;38:1357–1362. doi: 10.1345/aph.1D612. [DOI] [PubMed] [Google Scholar]
- 107.Lawrence DB, Ragucci KR, Long LB, et al. Relationship of oral antihyperglycemic (sulfonylurea or metformin) medication adherence and hemoglobin A1c goal attainment for HMO patients enrolled in diabetes management program. J Manag Care Pharm. 2006;12:466–471. doi: 10.18553/jmcp.2006.12.6.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lee JY, Kusek JW, Greene PG, et al. Assessing medication adherence by pill count and electronic monitoring in the African American Study of Kidney Disease and Hypertension (AASK) pilot study. Am J Hypertens. 1996;9(8, part 1):719–725. doi: 10.1016/0895-7061(96)00056-8. [DOI] [PubMed] [Google Scholar]
- 109.Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol. JAMA. 2006;296:2563–2571. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]
- 110.Melfi CA, Chawla AJ, Croghan TW, et al. The effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depression. Arch Gen Psychiatry. 1998;55:1128–1132. doi: 10.1001/archpsyc.55.12.1128. [DOI] [PubMed] [Google Scholar]
- 111.Milgrom H, Bender B, Ackerson L, et al. Noncompliance and treatment failure in children with asthma. J Allergy Clin Immunol. 1996;98(6, part 1):1051–1057. doi: 10.1016/s0091-6749(96)80190-4. [DOI] [PubMed] [Google Scholar]
- 112.Parris ES, Lawrence DB, Mohn LA, Long LB. Adherence to statin therapy and LDL cholesterol goal attainment by patients with diabetes and dyslipidemia. Diabetes Care. 2005;28:595–599. doi: 10.2337/diacare.28.3.595. [DOI] [PubMed] [Google Scholar]
- 113.Pladevall M, Williams LK, Potts LA, et al. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27:2800–2805. doi: 10.2337/diacare.27.12.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Psaty BM, Koepsell TD, Wagner EH, et al. The relative risk of incident coronary heart disease associated with recent use of beta-blockers. JAMA. 1990;263:1653–1657. [PubMed] [Google Scholar]
- 115.Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007;297:177–186. doi: 10.1001/jama.297.2.177. [DOI] [PubMed] [Google Scholar]
- 116.Rhee MK, Slocum W, Ziemer DC, et al. Patient adherence improved glycemic control. Diabetes Educ. 2005;31:240–250. doi: 10.1177/0145721705274927. [DOI] [PubMed] [Google Scholar]
- 117.Robinson DG, Woerner MG, Alvir JMAJ, et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999;56:241–247. doi: 10.1001/archpsyc.56.3.241. [DOI] [PubMed] [Google Scholar]
- 118.Schatz M, Zeiger RS, Vollmer WM, et al. The controller-to-total asthma medication ratio is associated with patient-centered as well as utilization outcomes. Chest. 2006;130:43–50. doi: 10.1378/chest.130.1.43. [DOI] [PubMed] [Google Scholar]
- 119.Schectman JM, Nadkarni MM, Voss JD. The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care. 2002;25:1015–1021. doi: 10.2337/diacare.25.6.1015. [DOI] [PubMed] [Google Scholar]
- 120.Schneider PJ, Murphy JE, Pedersen CA. Impact of medication packaging on adherence and treatment outcomes in older ambulatory patients. J Am Pharm Assoc. 2008;48:58–63. doi: 10.1331/JAPhA.2008.07040. [DOI] [PubMed] [Google Scholar]
- 121.Sood N, Treglia M, Obenchain RL, et al. Determinants of anti-depressant treatment outcome. Am J Manag Care. 2000;6:1327–1336. [PubMed] [Google Scholar]
- 122.Stern L, Berman J, Lumry W, et al. Medication compliance and disease exacerbation in patients with asthma: A retrospective study of managed care data. Ann Allergy Asthma Immunol. 2006;97:402–408. doi: 10.1016/S1081-1206(10)60808-3. [DOI] [PubMed] [Google Scholar]
- 123.Strakowski SM, Keck PE, McElroy SL, et al. Twelve-month outcome after a first hospitalization for affective psychosis. Arch Gen Psychiatry. 1998;55:49–55. doi: 10.1001/archpsyc.55.1.49. [DOI] [PubMed] [Google Scholar]
- 124.Sublett JL, Pollard SJ, Kadlec GJ, Karibo JM. Non-compliance in asthmatic children: A study of theophylline levels in a pediatric emergency room population. Ann Allergy Asthma Immunol. 1979;43:95–97. [PubMed] [Google Scholar]
- 125.Walker E, Molitch M, Kramer MK, et al. Adherence to preventive medications: Predictors and outcomes in the diabetes prevention program. Diabetes Care. 2006;29:1997–2002. doi: 10.2337/dc06-0454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wei L, MacDonald TM, Watson AD, Murphy MJ. Effectiveness of two statin prescribing strategies with respect to adherence and cardiovascular outcomes: Observational study. Pharmacoepidemiol Drug Saf. 2007;16:385–392. doi: 10.1002/pds.1297. [DOI] [PubMed] [Google Scholar]
- 127.Wu JR, Moser DK, Chung ML, Lennie TA. Objectively measured, but not self-reported, medication adherence independently predicts event-free survival in patients with heart failure. J Card Fail. 2008;14:203–210. doi: 10.1016/j.cardfail.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang Q, Safford M, Miller D, et al. Short-term statin exposure is associated with reduced all-cause mortality in persons with diabetes. Med Care. 2007;45:308–314. doi: 10.1097/01.mlr.0000250227.94196.f0. [DOI] [PubMed] [Google Scholar]
- 129.Blackburn DF, Dobson RT, Blackburn JL, Wilson TW. Cardiovascular morbidity associated with nonadherence to statin therapy. Pharmacotherapy. 2005;25:1035–1043. doi: 10.1592/phco.2005.25.8.1035. [DOI] [PubMed] [Google Scholar]
- 130.Choo PW, Rand CS, Inui TS, et al. A pharmacodynamic assessment of the impact of antihypertensive non-adherence on blood pressure control. Pharmacoepidemiol Drug Saf. 2000;9:557–563. doi: 10.1002/pds.539. [DOI] [PubMed] [Google Scholar]
- 131.Fan VS, Bryson CL, Curtis JR, et al. Inhaled drug therapy in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2003;168:1488–1494. doi: 10.1164/rccm.200301-019OC. [DOI] [PubMed] [Google Scholar]
- 132.Grant RW, Devita NG, Singer DE, Meigs JB. Polypharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care. 2003;26:1408–1412. doi: 10.2337/diacare.26.5.1408. [DOI] [PubMed] [Google Scholar]
- 133.Rand C, Bilderback MS, Schiller K, et al. Adherence with montelukast or fluticasone in a long-term clinical trial: Results from the Miami Asthma Montelukast versus Inhaled Corticosteroid Trial [MIAMI] J Allergy Clin Immunol. 2007;119:916–923. doi: 10.1016/j.jaci.2006.12.664. [DOI] [PubMed] [Google Scholar]
- 134.Rothman RL, Mulvaney S, Elasy TA, et al. Self-management behaviors, racial disparities, and glycemic control among adolescents with type 2 diabetes. Pediatrics. 2008;121:e912–e919. doi: 10.1542/peds.2007-1484. [DOI] [PubMed] [Google Scholar]
- 135.Turner J, Wright E, Mendella L, Anthonisen N. Predictors of patient adherence to long-term home nebulizer therapy for COPD. Chest. 1995;108:394–400. doi: 10.1378/chest.108.2.394. [DOI] [PubMed] [Google Scholar]
- 136.Sajatovic M, Valenstein M, Blow F, et al. Treatment adherence with lithium and anticonvulsant medications among patients with bipolar disorder. Psychiatr Serv. 2007;58:855–863. doi: 10.1176/ps.2007.58.6.855. [DOI] [PubMed] [Google Scholar]
- 137.Balkrishnan R, Christensen DB. Inhaled corticosteroid use and associated outcomes in elderly patients with moderate to severe chronic pulmonary disease. Clin Ther. 2000;22:452–469. doi: 10.1016/S0149-2918(00)89013-X. [DOI] [PubMed] [Google Scholar]
- 138.Camargo CA, Jr, Ramachandran S, Ryskina KL, et al. Association between common asthma therapies and recurrent asthma exacerbations in children enrolled in a state Medicaid plan. Am J Health Syst Pharm. 2007;64:1054–1061. doi: 10.2146/ajhp060256. [DOI] [PubMed] [Google Scholar]
- 139.Gilmer TP, Dolder CR, Lacro JP, et al. Adherence to treatment with antipsychotic medication and healthcare costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry. 2004;161:692–699. doi: 10.1176/appi.ajp.161.4.692. [DOI] [PubMed] [Google Scholar]
- 140.Hepke KL, Martus MT, Share DA. Costs and utilization associated with pharmaceutical adherence in a diabetic population. Am J Manag Care. 2004;10(part 2):144–151. [PubMed] [Google Scholar]
- 141.Lau DT, Nau DP. Oral antihyperglycemic medication non-adherence and subsequent hospitalization among individuals with type 2 diabetes. Diabetes Care. 2004;27:2149–2153. doi: 10.2337/diacare.27.9.2149. [DOI] [PubMed] [Google Scholar]
- 142.Lee WC, Balu S, Cobden D, et al. Medication adherence and associated health–economic impact among patients with type 2 diabetes mellitus converting to insulin pen therapy: An analysis of third party managed claims data. Clin Ther. 2006;28:1712–1725. doi: 10.1016/j.clinthera.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 143.Maronde RF, Chan LS, Larsen FJ, et al. Underutilization of anti-hypertensive drugs and associated hospitalization. Med Care. 1998;27:1159–1166. doi: 10.1097/00005650-198912000-00007. [DOI] [PubMed] [Google Scholar]
- 144.Murray MD, Young J, Hoke S, et al. Pharmacist intervention to improve medication adherence in heart failure. Ann Intern Med. 2007;146:714–725. doi: 10.7326/0003-4819-146-10-200705150-00005. [DOI] [PubMed] [Google Scholar]
- 145.Olfson M, Mechanic D, Hansell S, et al. Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatr Serv. 2000;51:216–222. doi: 10.1176/appi.ps.51.2.216. [DOI] [PubMed] [Google Scholar]
- 146.Sclar DA, Robison LM, Skaer TL, et al. Antidepressant pharmacotherapy: Economic outcomes in a health maintenance organization. Clin Ther. 1994;16:715–730. doi: 10.1016/s0011-393x(05)80275-9. [DOI] [PubMed] [Google Scholar]
- 147.Scott J, Pope M. Self-reported adherence to treatment with mood stabilizers, plasma levels, and psychiatric hospitalization. Am J Psychiatry. 2002;159:1927–1929. doi: 10.1176/appi.ajp.159.11.1927. [DOI] [PubMed] [Google Scholar]
- 148.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 149.Suissa S, Ernst P, Kezouh A. Regular use of inhaled corticosteroids and the long-term prevention of hospitalization for asthma. Thorax. 2002;57:880–884. doi: 10.1136/thorax.57.10.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Svarstad BL, Shireman TI, Sweeney JK. Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatr Serv. 2001;52:805–811. doi: 10.1176/appi.ps.52.6.805. [DOI] [PubMed] [Google Scholar]
- 151.Valenstein M, Copeland LA, Blow FC, et al. Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Med Care. 2002;40:630–639. doi: 10.1097/00005650-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 152.Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatr Serv. 2004;55:886–891. doi: 10.1176/appi.ps.55.8.886. [DOI] [PubMed] [Google Scholar]
- 153.White TJ, Vanderplas A, Ory C, et al. Economic impact of patient adherence with antidepressant therapy within a managed care organization. Dis Manag Health Outcomes. 2003;11:817–822. [Google Scholar]
- 154.Williams LK, Pladevall M, Xi H, et al. Relationship between adherence to inhaled corticosteroids and poor outcomes among adults with asthma. J Allergy Clin Immunol. 2004;114:1288–1293. doi: 10.1016/j.jaci.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 155.Yang Z, Olomu A, Corser W, et al. Outpatient medication use and health outcomes in post-acute coronary syndrome patients. Am J Manag Care. 2006;12:581–587. [PubMed] [Google Scholar]
- 156.Rich MW, Gray DB, Beckham V, et al. Effect of a multidisciplinary intervention on medication compliance in elderly patients with congestive heart failure. Am J Med. 1996;101:270–276. doi: 10.1016/s0002-9343(96)00172-6. [DOI] [PubMed] [Google Scholar]
- 157.Weissman EM, Dellenbaugh C. Impact of splitting risperidone tablets on medication adherence and on clinical outcomes for patients with schizophrenia. Psychiatr Serv. 2007;58:201–206. doi: 10.1176/ps.2007.58.2.201. [DOI] [PubMed] [Google Scholar]
- 158.Wood PR, Casey R, Kolski GB, McCormick MC. Compliance with oral theophylline therapy in asthmatic children. Ann Allergy Asthma Immunol. 1985;54:400–404. [PubMed] [Google Scholar]
- 159.Balkrishnan R, Rajagopalan R, Camacho FT, et al. Prediction of medication adherence and associated healthcare costs in an older population with type 2 diabetes mellitus: A longitudinal cohort study. Clin Ther. 2003;25:2958–2971. doi: 10.1016/s0149-2918(03)80347-8. [DOI] [PubMed] [Google Scholar]
- 160.Becker MA, Young MS, Ochshorn E, Diamond RJ. The relationship of antipsychotic medication class and adherence with treatment outcomes and costs for Florida Medicaid beneficiaries with schizophrenia. Adm Policy Ment Health. 2007;34:307–314. doi: 10.1007/s10488-006-0108-5. [DOI] [PubMed] [Google Scholar]
- 161.Katon W, Cantrell CR, Sokol MC, et al. Impact of antidepressant drug adherence on comorbid medication use and resource utilization. Arch Intern Med. 2005;165:2497–2503. doi: 10.1001/archinte.165.21.2497. [DOI] [PubMed] [Google Scholar]
- 162.Rizzo JA, Simons WR. Variations in compliance among hypertensive patients by drug class: Implications for health care costs. Clin Ther. 1997;19:1446–1457. doi: 10.1016/s0149-2918(97)80018-5. [DOI] [PubMed] [Google Scholar]
- 163.Shenolikar RA, Balkrishnan R, Camacho FT, et al. Comparison of medication adherence and associated health care costs after introduction of pioglitazone treatment in African Americans vs. all other races in patients with type 2 diabetes mellitus: A retrospective data analysis. Clin Ther. 2006;28:1199–1207. doi: 10.1016/j.clinthera.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 164.Thompson D, Buesching D, Gregor KJ, Oster G. Patterns of anti-depressant use and their relation to costs of care. Am J Manag Care. 1996;2:1239–1246. [Google Scholar]
- 165.Cantrell R, Eaddy MT, Shah MB, et al. Methods for evaluating patient adherence to antidepressant therapy: A real-world comparison of adherence and economic outcomes. Med Care. 2006;44:300–303. doi: 10.1097/01.mlr.0000204287.82701.9b. [DOI] [PubMed] [Google Scholar]
- 166.Eaddy MT, Druss BG, Sarnes MW, et al. Relationship of total health care charges to selective serotonin reuptake inhibitor utilization patterns including the length of antidepressant therapy: Results from a managed care administrative claims database. J Manag Care Pharm. 2005;11:145–150. doi: 10.18553/jmcp.2005.11.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Hepke KL, Martus MT, Share DA. Costs and utilization associated with pharmaceutical adherence in a diabetic population. Am J Manag Care. 2004;10(part 2):144–151. [PubMed] [Google Scholar]
- 168.Stein MB, Cantrell CR, Sokol MC, Eaddy MT, Shah MB. Anti-depressant adherence and medical resource use among managed care patients with anxiety disorders. Psychiatr Serv. 2006;57:673–680. doi: 10.1176/ps.2006.57.5.673. [DOI] [PubMed] [Google Scholar]
- 169.Dickson M, Plauschinat C. Compliance with antihypertensive therapy in the elderly: A comparison of fixed-dose combination amlodipine/benazepril versus component-based free-combination therapy. Am J Cardiovasc Drugs. 2008;8:45–50. doi: 10.2165/00129784-200808010-00006. [DOI] [PubMed] [Google Scholar]
- 170.Robinson RL, Long SR, Chang S, et al. Higher costs and therapeutic factors associated with adherence to NCQA HEDIS anti-depressant medication management measures: Analysis of administrative claims. J Manag Care Pharm. 2006;12:43–54. doi: 10.18553/jmcp.2006.12.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]