Abstract
While some avian retroviruses have been shown to induce gliomas in animal models, human herpesviruses, specifically, the most extensively studied cytomegalovirus, and the much less studied roseolovirus HHV-6, and Herpes simplex viruses 1 and 2, currently attract more and more attention as possible contributing or initiating factors in the development of human brain tumors. The aim of this review is to summarize and highlight the most provoking findings indicating a potential causative link between brain tumors, specifically malignant gliomas, and viruses in the context of the concepts of viral oncomodulation and the tumor stem cell origin.
Keywords: Gliomas, Brain tumors, Viruses, Herpesviruses, Retroviruses, Oncomodulation, Progenitors, Stem cells
Introduction
Malignant gliomas are histologically heterogeneous and invasive brain tumors that are associated with a disproportionally high mortality rate [1]. With no specific pathogenetic mechanisms identified by now for the majority of gliomas except for the exposure to the ionizing radiation and gene polymorphisms that affect detoxification, DNA repair and cell cycle regulation, the attention of researchers has recently been drawn to the possible infectious etiology of brain tumors. In this review we discuss the role of retroviruses in animal models of glioma and the possible impact of some human herpes viruses on the initiation and formation of brain tumors. While nowadays the role of stem cells as the major players in tumorigenes is widely discussed, we put together the relatively scarce data on the interactions of herpes viruses with local neural stem/progenitor cells as well as non-transformed astrocytes and glioma cells. Such interactions may potentially cause on-cotransformation, or influence various intracellular signaling pathways that will predispose cells to oncogenic changes, or further drive the formation or aggravation of the existing malignant phenotype with negative implications for the therapy of gliomas.
Retroviruses in animal models of brain tumors
Since the end of 1960s Rous sarcoma virus (RSV) and its closely related avian sarcoma leukosis virus (ASLV) were used in experimental animal models for induction of brain tumors [2–9] with morphological similarity to human gliomas [9, 10]. Both RSV and ASLV belong to the group of retroviruses, type C. While RSV and ASLV induce neurogenic tumors in many species, the naturally occurring fowl glioma has also been shown to be caused by the specific strain of a subgroup A of ASLV [11–13]. This strain could induce gliomas after injection in ovo, although the virus had the broad tissue tropism similar to other ASLV [14–17]. It had previously been reported that both cell cultures derived from chemically induced gliomas in Sprague-Dawley rats [18] and hydrocortisone-hypersensitive variant of rat glioma C6 cells line [19] also produced the so-called C-type viral particles, the morphologically similar group of enveloped RNA virus particles with an electron dense central nucleoid that is associated with certain cancers, such as sarcomas and leukemias. The particles were produced only in response to the treatment of cells with glucocorticoids. The latter are known to enhance the production of B type mouse mammary tumor virus (MMTV), and to exert immunosuppressive effects in vivo. The particles demonstrated reverse-transcriptase activity, yet poor transforming efficiency [19]. Steroids are regularly used to reduce cerebral edema in glioma. They might activate the production of retroviral-like particles in human glioma cells, but additional studies are required to determine if this was the case.
Sequences bearing homology to retroviral elements are inherent constituents of the human genome. They include endogenous retroviruses (often defective and non-infectious), LTR-, and poly-A (non-LTR) retrotransposons, which can amplify themselves, retroposons (retrotranscripts), the repetitive DNA fragments, which in contrast to retrotransposons do not encode Reverse Transcriptase, and other so-called retroelements [20]. Retroelements are known primarily as mobile DNA species integrated at various positions in the genomes of their host species. Many of them, such as for example, human LINE-1 (L1) retroelements, are considered to be essential for the regulation of mammalian gene expression [21, 22] and embryonic development [23, 24]. Of special interest are the findings that human L1 retroelementss are abundant in the brain as compared to other tissues, undergo transpositions in cultured human neural stem cells [25], and are controlled by the same factors that are involved in neuronal development [26]. Importantly, retroelements might be involved in mutagenesis and cancer initiation [27, 28]. As an example, the random amplified polymorphic DNA (RAPD) analysis of tissue obtained from the highly malignant human glioblastoma multiforme in comparison with genomic DNA from the normal human tissues revealed the loss of a 443 bp long DNA fragment that had 91% homology with fragments of three retroposons belonging to the human endogenous retrovirus HERV-K, which resembles MMTV. Interestingly, the altered fragment spanned a GC rich region, the polypurine tract, the steroid hormone responsive element and the enhancer core of these retroposon sequences [29]. In addition, several stretches of this altered sequence were also present in inverted repeats of human XRCC1 gene, which is involved in the efficient repair of DNA single-strand breaks, and of the BRCA2 tumor suppressor gene, which, in turn, plays an important role in the error-free repair of DNA double-strand breaks. Therefore, the regions of tumor suppressor genes harboring retroviral elements may be subjected to mutations, rearrangements, increased frequency of recombination, and other events resulting in genomic instability and neoplasia.
Herpesviruses and oncomodulation
Herpesviruses are a large family of DNA viruses that can cause latent or lytic infections. The classification of human herpesviruses is shown in Table 1. Epstein-Barr virus (EBV) and Kaposi’s sarcoma-associated herpes virus (KSHV) are proven to play an important role in the development of various cancers (EBV—in Burkitt’s and Hodgkin’n lymphomas, nasopharyngeal carcinoma, KSHV—in Kaposi’s sarcoma and primary effusion lymphoma), notably—often in immunocompromised patients. Other herpesviruses have also been suspected to be linked with various tumors, brain tumors being studied most intensely, even though the direct role of most of herpesviruses in tumori-genesis has not been proven yet.
Table 1.
Classification of human herpesviruses [229]
| Virus | Type | Subfamily | Diseases |
|---|---|---|---|
| Herpes simplex virus-1 (HSV-1) | HHV-1 | α (alpha) | Oral and/or genital herpes, herpes encephalitis in patients with gliomas, herpes infections in immunocompromised patients |
| Herpes simplex virus-2 (HSV-2) | HHV-2 | α | Oral and/or genital herpes (predominantly genital), other herpes simplex infections |
| Varicella zoster virus (VZV) | HHV-3 | α | Chickenpox and shingles, infections in immunocompromised patients |
| Epstein-Barr virus (EBV), lymphocryptovirus | HHV-4 | γ (gamma) | Infectious mononucleosis, Burkitt’s lymphoma, CNS lymphoma in AIDS patients, post-transplant lymphoproliferative syndrome (PTLD), nasopharyngeal carcinoma, HIV-associated hairy leukoplakia |
| Cytomegalovirus (CMV) | HHV-5 | β (beta) | Infectious mononucleosis-like syndrome, retinitis, infections in immunocompromised patients |
| Roseolovirus, Herpes lymphotropic virus | HHV-6 | β | Sixth disease (roseola infantum or exanthem subitum) |
| Roseolovirus | HHV-7 | β | Analogously to HHV-6 Sixth disease (roseola infantum or exanthem subitum) |
| Kaposi’s sarcoma-associated herpesvirus (KSHV), a type of rhadinovirus | HHV-8 | γ | Kaposi’s sarcoma, primary effusion lymphoma, some types of multicentricCastleman’s disease |
With this regard, the concept of “oncomodulation” has emerged [30, 31]. Oncomodulation is defined as the ability of viral proteins and non-coding RNAs to promote oncogenic processes without direct oncotransformation but through disturbances in various intracellular signaling pathways. They may include interference with the activity of tumor suppressor genes, enhancement of cell proliferation, motility and invasiveness, inhibition of apoptosis and cellular senescence, shift from the precise to error-prone DNA damage repair pathways, immune evasion, selection of the malignant phenotype, epigenetic changes, which in turn, may also regulate virus latency and reactivation [32], and aberrant angiogenesis. As the growing number of evidences suggests that tumors originate from local stem/progenitor cells, deregulation of cell differentiation can also be viewed as the sign of tumor-promoting activity.
We will review the human cytomegalovirus (HCMV), by now one of relatively better studied herpesviruses, which spectrum of activities may be considered as a prototype for oncomodulation, and compare its pro-oncogenic properties with those of human herpes simplex virus 1 and 2 (HSV) and herpes lymphotropic virus (HHV-6) (Table 2).
Table 2.
Selected pro-oncogenic properties of HCMV, HSV and HHV-6
| HCMV | HHV-6 | HSV-1 and -2 | |
|---|---|---|---|
| Detection in the tumors | Brain tumors, breast cancer, colon cancer, cervix cancer, prostate carcinoma, EBV-negative Hodgkin’s lymphoma | Brain tumors, lymphomas and leukemias, cervical cancer | Malignant and benign thyroid tumors |
| Cellular entry receptor | PDGFR alpha | CD46 | Nectin-1 and-2, HSV entry mediator A |
| Distribution of cellular entry receptors | Various cell types including astrocytes and neural stem/progenitor cells, | Various cell types including astrocytes and neural stem/progenitor cells | Various cell types including neurons, ependymal cells, oligodendrocytes, astrocytes. Neural stem/progenitor cells (?) |
| Expression of the cellular entry receptors in gliomas | Yes | Yes | Yesa |
| Influence on cell cycle progression | Differs between the transformed and primary cells, probably depends on P53 status | (?) | (?) |
| Pro- and anti-apoptotic activity | Anti-apoptotic effect. Pro-apoptotic effect related to blocking cell cycle progression (?) | (?) | Differs between the cancer cells and normal cells. Pro- apoptotic in the lytic, and anti-apoptotic in the latent phase |
| Cellular senescence | Upregulation of telomerase | Integration into telomeres. Elongation of telomeres (?) | Upregulation of telomerase |
| Cellular differentiation | Inhibition of cell differentiation, reactivation in differentiated cells (?) | (?) | (?) |
| Transactivation in the absence of wild type p53 | Yes | (?) | Yes |
| DNA-damage | Yes | (?) | (?) |
| Mutagenesis of cellular genomic DNA | Yes (?) | (?) | (?) |
| Dependence on histone deacetilase inhibition | Yes | Yes | Yes |
| Immunomodulation | Yes | Yes | Yes |
| Cell migration, invasion, angiogenesis | Enhancement | (?) | (?) |
Author’s data (unpublished)
Pro-oncogenic properties of HCMV
Human cytomegalovirus (HCMV) is a widespread human virus that has been mainly known to cause disease in immunocompromised patients [33, 34]. The virus is believed to persist mainly in myeloid cells but may be reactivated and infect different tissues in immunocompromised or cancer patients due to cancer-related immunosupression and chemo- and radiation therapy, inflammation and stress [32, 35–41]. By now HCMV has been the most intensely studied virus for its possible link with various tumors, including brain tumors. The HCMV genome encodes more than 200 proteins, and their expression occurs in three sequential stages after infection: immediate early (IE), early (E), and late (L). These proteins have multiple biological activities that interfere with physiological functions in infected cells [42].
HCMV presence in human brain tumors
A possible relationship between HCMV and cancers had been prompted in the early 1970s by the finding of increased anti-HCMV antibody titers in patients with cervical carcinoma [43]. Recently by employing highly sensitive techniques, HCMV has been found in tumor cells of more than 90% of patients with breast cancer, colon cancer, cervix cancer, prostate carcinoma, and EBV-negative Hodgkin’s lymphoma [30, 32, 44, 45]. The presence of HCMV genomic sequences as well as its proteins expression has also been detected in malignant gliomas of various grades [46–49]. In nearly 80% of patients with brain tumors HCMV DNA was also detected in the peripheral blood suggesting either systemic reactivation or viral shedding from tumor cells to the periphery [50, 51]. Moreover, those patients, who had a low viral load, lived twice as long compared to patients with high levels of infection [52]. The non-structural HCMV 72 kDa immediate early (IE) 1 protein (IE72), also known as UL123, is one of the first HCMV antigens expressed in an infected cell. IE72 could be detected in about 16–90%, and pp65 protein—in about 50% of the cases in brain tumors [52, 53]. Both proteins could be detected by immunohistochemical methods. It has been reported that vaccination with autologous dendritic cells as adjunctive therapy in malignant gliomas once resulted in an extremely robust anti-HCMV-specific CD8+ T-cell response to pp65 [54]. It is noteworthy that non-cancer cells even in the vicinity of tumors appear to be HCMV negative.
HCMV and neural precursors
The adult human brain maintains a population of progenitor cells in the subventricular zone (SVZ), the largest germinal center in the brain and source of local stem/progenitor cells within the walls of the lateral ventricle [55]. Most gliomas have been shown to contact the walls of the lateral ventricle [52]. Cells in the SVZ and ventricular zone appear to be the primary targets for the HCMV in connection with congenital HCMV infection [56–58]. Analogously to the observations that it interferes with differentiation of myeloid cells into the macrophages and dendritic cells, HCMV has been reported to inhibit both neuronal [59] and astrocyte differentiation as indicated by downregulation of glial fibrillary acidic protein [57, 60, 61]. In transgenic mice expressing gene-reporters driven by the HCMV IE enhancer/promoter its activity was strongly induced in reactive astrocytes in response to a neocortical stab lesion [58]. Neural progenitors and primary cultures of differentiated human astrocytes appear to be the most permissive for HCMV infection [59, 62], and support productive replication of HCMV [62–64]. However, susceptibility to HCMV infection declines following differentiation of neural precursors into neurons [64, 65], and in immortalized astrocytic cell lines susceptibility to HCMV varies from complete resistance to partial expression of viral genes [59, 66]. The cell and tissue specificity of HCMV depends on the presence and activity of SP1 cell transcription factor. SP1 together with HCMV 86-kDa IE2 protein (IE86) forms a complex that binds to an inverted-repeat element of HCMV UL54 (polymerase) promoter [67], thus activating replication of the virus.
Platelet derived growth factor (PDGF) and its receptors (PDGFR) are essential to the self-renewal of neural stem cells. In vitro studies demonstrated that PDGF signaling results in inhibition of their differentiation into neurons, astrocytes and oligodendrocytes, and has a growth promoting effect in the neural progenitor cell population [68]. Many human gliomas express markers of glial progenitors, in particular, PDGFR alpha, which expression as well as phosphorylation correlates with malignant histology in pediatric gliomas [69]. In turn, PDGF ligands are powerful mitogens for both glioma cells and adult glial progenitors [70]. Infusion, or retroviral-mediated delivery of PDGF B ligand into the lateral ventricles resulted in massive expansion of both infected and uninfected glial progenitors with the characteristic for gliomas cellular atypia and pleyomorphism [52]. Interestingly PDGFR alpha is activated by HCMV and absolutely required for HCMV internalization, activation of downstream signaling and production of infectious virus [71]. However it was reported that in smooth muscle cells HCMV downregulates expression of PDGFR alpha and beta [72]. It is not clear whether HCMV binding to PDGF receptor may mimic the action of PDGF ligands, or if HCMV exploits this opportunity to maintain its replication. Nevertheless, efficient HCMV infection, or even expression of some of its proteins even out of the whole virus context significantly alters multiple pathways related to cell cycle, apoptosis, DNA repair, cell invasion, angiogenesis and host immune response (see “HCMV and cell cycle” Section).
HCMV and cell cycle
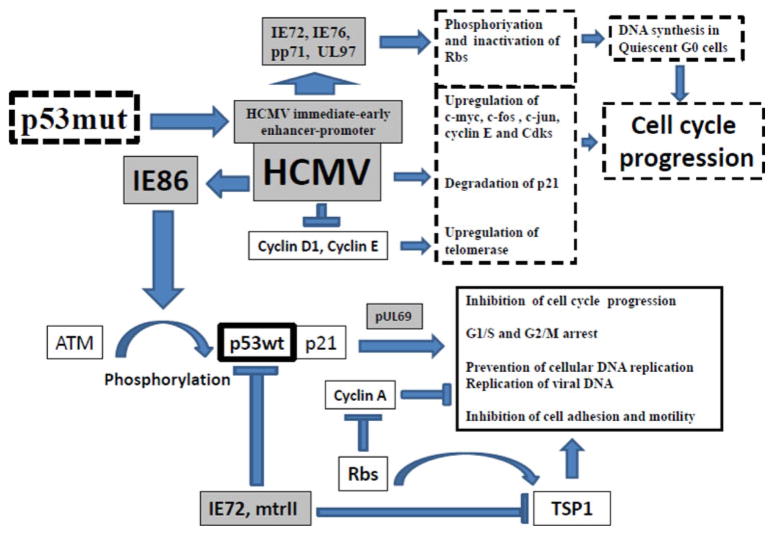
Stem cells in vivo represent quiescent (G0) cell pool that intermittently gives rise to tissue-specific progenitors with robust proliferative potential, the so-called transiently amplifying (TA) cells, that, in turn, eventually become terminally differentiated [73]. The retinoblastoma tumor suppressor protein (pRb) is responsible for transcriptional repression of cyclin A, a positive regulatory component of kinases required for the progression through S phase and for the transition between the G2 and M phases of the cell division cycle [74]. IE72, IE76, pp71, and UL97 HCMV proteins are able to interact, phosphorylate and inactivate proteins of Rb family (Rbs) that includes pRb, p107 and p130. In addition, binding of pp71 to Rbs induces DNA synthesis in quiescent G0 cells [75, 76]. These changes may prompt resting in G0 phase local progenitors to generate the pool of TA with their following massive expansion. The levels of the protooncogenes c-myc, c-fos and c-jun, as well as of cyclin E and Cdks are rapidly upregulated following infection of cells by HCMV [77], and the p21waf1 protein, which arrests cells in the G1 phase, becomes degraded [78]. HCMV chemokine receptor US28 also enhances cell proliferation [79, 80]. However, HCMV may block cell cycle progression as well [30, 32]. The controversy of the existing data could probably be explained by the status of p53 protein in the cell lines used for experiments. Specifically, in some glioma cell lines, p53 is mutated and therefore acts oppositely to its wild type counterpart by failing to transactivate its usual target genes with anti-oncogenic activities, but instead de-repressing or transactivating a plethora of protooncogenes [81, 82]. In addition, mutated p53 activates some viral promoters, in particular, the human cytomegalovirus major immediate-early promoter-enhancer, the long terminal repeat promoters of Rous sarcoma virus, and human T-cell lymphotropic virus type I [83]. In normal permissive cells, HCMV-encoded regulatory proteins induce cell cycle arrest in both the G1/S and G2/M check-points [84, 85] and prevent cellular DNA replication while enabling replication of viral DNA [86, 87]. In HCMV-infected cells, cyclins A and D1 are inhibited, and IE86 may induce cell cycle arrest by activating an ataxia telangiectasia mutated gene–dependent phosphorylation of p53 at Ser15. These events result in p53 accumulation and activation, leading to a p53-and p21-dependent inhibition of cell cycle progression [88], but only in cells with intact p53. In normal fibroblasts expressing wild-type p53, HCMV IE1-72 protein cannot drive cells out of quiescence, whereas IE1-72 can induce S phase and delay cell cycle exit in p53-deficient cells [30]. Other virus regulatory proteins, for example the pUL69, contribute to HCMV-induced cell cycle arrest [86]. In T89G glioblastoma cells with disrupted p53 signaling, persistent HCMV infection did not induce cell cycle arrest and virus antigen-positive cells continued to divide [51]. In turn, p53, may be downregulated by IE72, or inactivated by mtrII protein encoded within the morphological transforming region II (mtrII) of HCMV strain Towne [89]. Another tumor suppressor gene thrombospondin-1 (TSP-1) is down-regulated by IE72. TSP-1 is involved in the inhibition of cell growth, adhesion and motility, and is upregulated by Rbs [52, 61]. Again these results were obtained with U373 malignant glioma cell line, which harbors the p53 mutant (R273H), and it is not clear whether down-regulation of aberrant p53 has pro- or anti-tumor consequences. The putative effects of HCMV on the cell cycle are summarized in Fig. 1.
Fig. 1.
HCMV and cell cycle: shadowed boxes depict HCMV transcriptional elements and proteins
HCMV and cellular senescence
HCMV induces constitutive expression and activation of human telomerase reverse transcriptase (hTERT) both in several malignant glioma cell lines and in normal fibroblasts. HCMV-mediated transactivation of the hTERT gene is also dependent on the presence of Sp1-binding sites in the hTERT promoter and accompanied by increases in Sp1 binding, acetylation of histone H3, and a reduction in histone deacetylases (HDAC-1 and -2) binding at the hTERT promoter, which is consistent with local chromatin remodeling at the sites of active transcription [42]. Telomerase is commonly activated in cancer cells of both viral and nonviral origin, and hTERT activation is sufficient to immortalize normal diploid cells [31]. In addition, hTERT promotes cancer cell growth and shifts the balance toward DNA repair instead of apoptosis, thus potentially rendering tumors chemo- and radioresistant. Ectopic expression of only IE72, out of the roughly 200 different HCMV gene products, was sufficient to reproduce the viral effects on hTERT promoter activation [42]. IE72 is a promiscuous transcriptional activator of numerous viral and host cell genes. It interacts with several common cellular transcription factors including CTF1, E2Fs, and Sp1 and targets histone deacetylases (HDACs) to promote histone acetylation [90].
HCMV and DNA damage
HCMV has been demonstrated to induce chromosomal damage [91, 92], by both randomly distributed chromatid breaks at low frequencies, and site-specific chromosome 1 double-strand breaks (DSB) at positions 1q42 and 1q21 [93]. The chromosomal breaks were predominantly chromatid breaks rather than chromosome breaks, which is explained by the experimental settings when a large proportion of cells were in S or G2/M phases of the cell cycle. Eukaryotic cells repair DSB primarily by two mechanisms: homologous recombination (HR) and nonhomologous end-joining (NHEJ). HR uses a DNA molecule with significant length of sequence homology (undamaged sister chromatid or homologous chromosome as a DNA template) to prime the repair DNA synthesis. In contrast, NHEJ, and relatively less studied microhomology-mediated end joining (MMEJ) are both the error-prone joining of DNA ends without the requirement for sequence homology. NHEJ plays an especially important role in DSB repair during the G1 phase of the cell cycle when no sister chromatid is available. Since HCMV may block cell cycle progression in G1 phase, the prevalence of NHEJ may result in mutations and translocations therefore increasing genetic instability. The possible targets residing near 1q42 include the ADPRT locus involved in DNA repair and replication [94], whose deletion has been connected to the development of glioblastoma [95], and breast cancer tumor suppressor gene, which is located at 1q21–31 [96]. HCMV virion binding and/or entry was necessary and sufficient to induce chromosomal damage even in the absence of de novo viral gene expression. Therefore, neural progenitors could be infected with HCMV, incur chromosomal damage and pass this damage on to daughter cells that might become origins of the tumors.
HCMV and mutagenesis
It has been reported that HCMV IE72 and IE86 proteins are mutagenic and can cooperate with the adenovirus E1A protein to transform primary baby rat kidney (BRK) cells [97]. In addition, stable cell lines transformed by HCMV were shown to harbor an activating mutation in both alleles in H-Ras, the proto-oncogene, related to the development of certain types of cancers [98]. Since HCMV proteins and DNA were not present in cell lines derived from the transformed BRK foci, it is not clear whether the mutations in H-Ras result from direct mutagenic activity, or HCMV acted as a selector for the mutant phenotypes.
It is noteworthy that persistent HCMV infection of a number of tumor cell lines including glioblastomas appears to be dependent on selection of the novel slowly growing virus strains with mutations/deletions in the coding sequences of viral regulatory proteins [99–101]. The subculturing of virus-containing tumor tissues, as well as HCMV-transformed human embryo cells results in the loss of HCMV [84, 85, 102]. It appears that the consistent presence of HCMV in tumors in vivo may also be dependent on the tumor microenvironment, in particular, hypoxia that is characteristic for all solid tumors including gliomas, and has been reported to influence replication of some viruses [103–111].
Other pro-oncogenic properties of HCMV
Other activities of HCMV include inhibition of cancer cell apoptosis and immunogenecity, enhancement of cell migration, invasion, adhesion to the endothelium, and angiogenesis (reviewed in [30, 32, 52]. Those properties of HCMV also appear to have variable effects in normal cells and in cancer cells. HCMV infection stimulates invasiveness of gliomas [51, 79, 80, 112]. Human glioblastoma cells expressing US28, a chemokine receptor of HCMV, exhibited increased malignancy after injection in nude mice. In contrast, US28 induced apoptosis in nontumorigenic human cells [80]. It appears that expression of HCMV products even out of the context of the whole virus can induce significant changes in the cellular signaling network.
In conclusion, HCMV presence in the tumors may induce the shift toward more malignant phenotype. Therefore, HCMV may represent a therapeutic target, and in experimental models it has been shown that general antiviral therapeutic strategies or inhibition of HCMV IE genes expression has counteracted and reverted HCMV-induced malignant changes and chemoresistance [31, 52].
HHV-6
HHV-6 (Roseolovirus, herpes lymphotropic virus) was first isolated in 1986 from AIDS patients and patients with other lymphoproliferative disorders [113]. HHV-6 uses CD46 cell surface molecule, which is expressed in all nucleated cells, as its cellular entry receptor [114]. Such broad tropism combined with immunological and molecular evidence of HHV-6 infection in individuals raised the question of the pathogenicity of this virus in some diseases [113, 115]. HHV-6 has been linked with several CNS diseases including enecephalitis in non-immuno-compromised patients as well as digestive problems in immunosupressed patients, severe maternal-fetal infections, but most important—with hematological malignancies [116–118]. Below we briefly review some features of HHV-6 that associate it with brain tumors.
HHV-6 presence in human brain tumors
A number of reports described the finding of HHV-6 sequences and proteins in adult and pediatric brain tumors by various techniques including PCR, in situ hybridization, and immunohistochemistry [119–125]. Other studies demonstrated HHV-6 DNA sequences in non-pathological brain tissues as well, though at lower levels [117]. It is not clear whether detection of HHV-6 can be explained by primary infection or reactivation due to the tumor-induced dysfunctions of immune surveillance mechanisms and enhanced glial cell proliferation [120].
HHV-6 and neural precursors
HHV-6 has been shown to infect human mature oligodendrocytes and astrocytes in vitro and in vivo [126, 127]. Two viral variants (HHV-6A and HHV-6B) may elicit different infection patterns: HHV-6A results in productive lytic infection while HHV-6B is associated with a non-productive (apparently latent) infection. [127]. It appears that HHV-6 can infect glial precursors as well and shift their differentiation toward oligodendrocytes [128]. Various medulloblastoma cell lines as well as clinical specimens obtained from brain tumors also express CD46 [129].
Apoptosis and cell cycle
It has been reported that HHV-6 infection of human oligodendrocytes and their immediate precursors induce apoptosis via caspase-independent pathways [130]. However, it is not clear which viral variant was used in the experiments. The opposite results were obtained with glial precursors, which infection with both HHV-6A and HHV-6B resulted in alterations in cell morphology and impairment of cell replication but not cell death. Infected cells demonstrated cell cycle arrest in G1/S phase, downregulation of the glial progenitor cell marker A2B5 and a corresponding increase in the oligodendrocyte differentiation marker [128]. It is not clear whether the HHV-6-induced cell cycle arrest is irreversible. One of the unique features of HHV-6 is its ability to stably integrate into the telomeres of chromosomes during latency and vertically transmit through the germ-line [131–134]. Reactivation of the integrated HHV-6 genome can be achieved in the presence of histone deacetylase inhibitor [132]. It was suggested that HHV-6 genome may serve as an initial template for telomere elongation [114], and therefore counteract apoptosis and enhance cell proliferation during the latency.
Tumor-initiating properties
HHV-6 DNA and specifically its ORF-1 gene can transform human epidermal keratinocytes and NIH 3T3 cells in vitro. Moreover, cells expressing ORF-1 protein produce fibrosarcomas when injected into nude mice. The ORF-1 protein binds and inactivates p53, and another HHV-6 gene product U95 binds to nuclear factor-kappa B (NF-kB), which deregulation has been postulated to contribute to cancer [118, 135].
HHV-6 and immunomodulation
Like other herpesviruses HHV-6 expresses a number of proteins that counteract host’s immune system and allow HHV-6 to escape immune surveillance, especially during the latency [114, 136]. HHV-6 upregulates interleukin-10, inhibits IFN-gamma, and in general the immune disturbances induced by HHV-6 appears to be a shift from a Th-1 to a Th-2 type cytokine profile [137]. HHV-6 reactivation is usually accompanied by reactivation of other herpesviruses, such as HCMV and EBV [138–142], as well as in HIV-infected individuals (HHV-6 has been proposed as a potential co-factor in AIDS progression) [114, 143], and in cancer patients [144].
HSV-1 AND -2
Herpes simplex viruses cause a lytic infection in epithelial cells. HSV-1 can be transmitted through skin contact during outbreaks. HSV-2 is a primarily sexually transmitted human infection. Both HSV- 1 and HSV-2 can persist in the nerve cells in a latent state, in which the viral genome persists in a nonintegrated form without causing disease in an immune-competent host [145]. Since 1960s HSV-1 and HSV-2 were intensely studied for their possible association with cancers, specifically—head and neck and cervical cancers [146, 147]. Of interest is the recent discovery of HSV-1 and -2 DNA in malignant and benign thyroid tumors. During tumor progression, thyroid cells acquire increased susceptibility to HSV due to activation of mitogenic signaling in cancer cells and increased expression of nectin-1, the receptor that is necessary for HSV-1 cellular entry [148].
Virtually all neurons, ependymal cells, choroid plexus epithelial cells, meningothelial cells, vascular endothelial cells, as well as many oligodendrocytes, astrocytes, and vascular smooth muscle cells express nectin-1 [149–152], However, reports on the presence of HSV-1 DNA in brain tumors are contradictory [123, 153, 154]. This may be explained both by the differences in the sensitivity of the used techniques and by the presence of only the fragments of the viral DNA. It was reported earlier by several laboratories that in a small fraction of permissive cells a portion of the viral genome is either damaged or missing [155–158], and only a fragment of HSV-2 DNA may be enough to induce tumorigenic transformation [159–162].
Both HSV-1 and-2 induce apoptosis in infected cells at the early stage of infection. However, it is well established that apoptosis in HSV-infected cell is blocked at later stages, especially during the latency, via cooperation of multiple viral gene products and cellular factors [163–166]. Interestingly the cells demonstrated different levels of sensitivity to HSV-1-induced apoptosis. For example, human cancer cells display an exquisite sensitivity to HSV-1-induced apoptosis [164]. However, apoptosis is significantly delayed during the infection of astrocytes [167]. It appears that primary cells are generally resistant to HSV-1-dependent apoptosis [164]. The anti-apoptotic activity of HSV, which is linked to the so-called Latency Associated Transcript, may explain the above described findings of HSV DNA in thyroid tumors as well as the ability of the fragments of viral DNA to induce oncogenic transformation. One may speculate that, for example, in case of genotoxic stress latent HSV infections may shift the balance from apoptosis towards error-prone DNA repair, which is associated with genomic instability and cancer.
In addition, HSV-1 vectors genetically engineered for cancer gene therapy (both replication-competent and deletion mutants) were found to upregulate the promoters of human telomerase reverse transcriptase as well as other cancer-linked promoters (tyrosinase and probasin) in both tumor and non-tumor cells, and such activity was attributed to VP16, ICP4 and especially ICP0 viral gene products [168].
As mentioned above, herpes infections and herpes-associated cancers appear to be linked with immunodeficiency. Dissemination of herpes zoster [169–177] as well as reactivation of HSV-1 [178–184] have been reported in cancer patients who were subjected to chemo- and radiotherapy. However, the mechanisms of reactivation remain unknown. There are a number of clinical reports on the cases of HSV-1 encephalitis in patients with gliomas who received radiotherapy [185–187]. In tumor cells and skin fibroblasts, HSV-1 can be reactivated by both ultraviolet [188–190] and ionizing radiation [191, 192]. In turn, HSV-1 may render infected cells more radiosensitive through the expression of the immediate-early protein ICP0, which downregulates DNA-dependent protein kinase and delays repair of DNA double-strand breaks [193]. Rat glioma C6-derived cell line may become more susceptible to HSV-1 upon the treatment with glucocorticoids [194–197]. HSV-2 can be reactivated from those C6-BU-1 cells by superinfection with murine cytomegalovirus (MCMV), but not with UV-irradiated MCMV or human cytomegalovirus.
Interestingly, HCMV may also be reactivated during space flights [198, 199], which is explained by stress, but also may be related to the low dose ionizing radiation. Other similarities between HSV-1 and HCMV include: (i) upregulation of hTERT [168]; (ii) transactivation of HSV-1 UL9 by mutant p53 [83]; (iii) interplay of both HCMV and HSV-1 with gamma interferon and tumor necrosis factor alpha in the process of reactivation from the latency [32, 190, 200, 201]; (iv) dependence of HCMV, HHV-6 and HSV-1 replication on the inhibition of histone de-acetylation [90, 202, 203] (for example, HCMV cannot replicate in human teratocarcinoma cells because they express histone deacetylase-3 [202]); (v) contribution to both pro- and anti-apoptotic processes [204]: in mouse peritoneal macrophages [205] and neurons [206] productive HSV-1 and HSV-2 infection results in virus multiplication and cell death, whereas in cervical cancer cell lines HSV-2 boosts DNA synthesis in G1 and S phases of cell cycle [207]; (vi) inhibition of immune response via downregulation of MHC class 1 in infected glioma cell line [208]. HSV-2-transformed murine tumors cell lines may inhibit immune response through expression of TGF-beta [209].
Other herpesviruses
A cohort of epidemiological studies reported a correlation between the presence of antibodies against various herpesviruses and onsets and survival rates in cervical and head and neck cancers [210–222], and inverse correlation between the anti-HHV-3 immunoglobulins and the onset of gliomas [223, 224].
EBV was detected in a significant number of samples obtained from patients with pilocytic astrocytoma, a non-malignant glioma [123]. However, EBV, which is known for its link with primary brain lymphomas [225, 226], has not been associated with malignant gliomas before.
Conclusions
While herpesviruses are widespread among the human population, pre-existing conditions, such as mutations of tumor suppressor proteins, fluctuations in microRNA profiles, or other biomarkers may explain why some infected individuals are at higher risk to develop brain tumors as well as other cancers. The ability of herpesviruses and possibly other viruses to contribute to tumorigenesis may vary and is apparently dependent on the heterogeneity of cell populations within normal tissues. The experimental paradigms of pathogenesis of brain tumors that include the use of glial stem/progenitors appear to be the most interesting in revealing the oncogenic potential of latent viruses, most of all, herpesviruses, which remain “the usual suspects” and are kept in the spotlight of modern cancer research. The availability of well-characterized cell lines obtained from human gliomas [227, 228] with the properties of cancer stem cells (expression of stem cell markers, multipotency and ability to initiate brain tumors after being transplanted to immunocompromised animals) allows researchers to explore the interactions between the viruses and cancer stem cells with regard to the possible impacts on the clinical outcome and efficiency of currently used therapeutic approaches. Finally, targeting herpesviruses cellular entry receptors on tumor cells may one day become a part of the complex anti-tumor therapy.
Acknowledgments
We thank Chris Letson for reading and correcting the manuscript. Supported by NIH RO1 NS045209 (R. A-bounader) and NIH R01 CA134843 (R. Abounader).
Contributor Information
Alexander Kofman, Department of Microbiology, University of Virginia, P.O. Box 800168, Charlottesville, VA 22908, USA.
Lucasz Marcinkiewicz, Department of Microbiology, University of Virginia, P.O. Box 800168, Charlottesville, VA 22908, USA.
Evan Dupart, Department of Microbiology, University of Virginia, P.O. Box 800168, Charlottesville, VA 22908, USA.
Anton Lyshchev, St. Petersburg State Department of Health, Laboratory of Molecular Genetics, Hospital #31, Pr. Dinamo 3, St. Petersburg 197110, Russia.
Boris Martynov, S.M.Kirov Medical Academy, Pr. Dinamo 3, St. Petersburg 197110, Russia.
Anatolii Ryndin, Clinical Diagnostic Center, Pr. Dinamo 3, St. Petersburg 197110, Russia.
Elena Kotelevskaya, St. Petersburg State Department of Health, Laboratory of Molecular Genetics, Hospital #31, Pr. Dinamo 3, St. Petersburg 197110, Russia.
Jay Brown, Department of Microbiology, University of Virginia, P.O. Box 800168, Charlottesville, VA 22908, USA.
David Schiff, Department of Cancer Center, University of Virginia, Charlottesville, VA, USA.
Roger Abounader, Email: RA6U@virginia.edu, Department of Microbiology, University of Virginia, P.O. Box 800168, Charlottesville, VA 22908, USA. Department of Cancer Center, University of Virginia, Charlottesville, VA, USA.
References
- 1.Wen PY, Kesari S. Malignant gliomas in adults. N Engl J Med. 2008;359:492–507. doi: 10.1056/NEJMra0708126. [DOI] [PubMed] [Google Scholar]
- 2.Sakamoto K, Hoshino H, Kiuchi Y, Nakano G, Nagamachi Y. Potential usefulness of a cultured glioma cell line induced by Rous sarcoma virus in B10. A mouse as an immunotherapy model. Jpn J Exp Med. 1989;59:173–180. [PubMed] [Google Scholar]
- 3.Nakamura O, Hojo S, Takakura K, Nagashima K, Ishizaki R. Schmidt Ruppin-D-ASV-induced primary rat brain tumor model for therapeutic screening. No To Shinkei. 1982;34:691–697. [PubMed] [Google Scholar]
- 4.Rabotti GF. Gliomas induced in mammals by Rous sarcoma virus (RSV) (author’s transl) Neurochirurgie. 1981;27:247–249. [PubMed] [Google Scholar]
- 5.Kumanishi T, Ikuta F, Yamamoto T. Brain tumors induced by Rous sarcoma virus, Schmidt-Ruppin strain. 3. Morphology of brain tumors induced in adult mice. J Natl Cancer Inst. 1973;50:95–109. doi: 10.1093/jnci/50.1.95. [DOI] [PubMed] [Google Scholar]
- 6.Bigner DD, Odom GL, Mahaley MS, Jr, Day ED. Brain tumors induced in dogs by the Schmidt-Ruppin strain of Rous sarcoma virus. Neuropathological and immunological observations. J Neuropathol Exp Neurol. 1969;28:648–680. doi: 10.1097/00005072-196910000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Mahaley MS, Jr, Aronin PA, Michael AJ, Bigner D. Prevention of glioma induction in rats by simultaneous intra-cerebral inoculation of avian sarcoma virus plus bacillus Calmette-Guerin cell-wall preparation. Surg Neurol. 1983;19:453–455. doi: 10.1016/0090-3019(83)90145-3. [DOI] [PubMed] [Google Scholar]
- 8.Lee YS, Wikstrand CJ, Bigner DD. Glioma-associated antigens defined by monoclonal antibodies against an avian sarcoma virus-induced rat astrocytoma. J Neuroimmunol. 1986;13:183–202. doi: 10.1016/0165-5728(86)90064-0. [DOI] [PubMed] [Google Scholar]
- 9.Britt RH, Lyons BE, Eng LF, Bigner SH, Bigner DD. Immunohistochemical study of glial fibrillary acidic protein in avian sarcoma virus-induced gliomas in dogs. J Neurooncol. 1985;3:53–59. doi: 10.1007/BF00165172. [DOI] [PubMed] [Google Scholar]
- 10.Haguenau F. Comparative ultrastructure of human gliomas and experimental gliomas induced by Rous sarcoma virus (RSV) (author’s transl) Neurochirurgie. 1981;27:251–253. [PubMed] [Google Scholar]
- 11.Iwata N, Ochiai K, Hayashi K, Ohashi K, Umemura T. Avian retrovirus infection causes naturally occurring glioma: isolation and transmission of a virus from so-called fowl glioma. Avian Pathol. 2002;31:193–199. doi: 10.1080/03079450120118702. [DOI] [PubMed] [Google Scholar]
- 12.Hatai H, Ochiai K, Nagakura K, Imanishi S, Ochi A, Kozakura R, Ono M, Goryo M, Ohashi K, Umemura T. A recombinant avian leukosis virus associated with fowl glioma in layer chickens in Japan. Avian Pathol. 2008;37:127–137. doi: 10.1080/03079450801898815. [DOI] [PubMed] [Google Scholar]
- 13.Hatai H, Ochiai K, Murakami M, Imanishi S, Tomioka Y, Toyoda T, Ohashi K, Umemura T. Prevalence of fowl glioma-inducing virus in chickens of zoological gardens in Japan and nucleotide variation in the env gene. J Vet Med Sci. 2008;70:469–474. doi: 10.1292/jvms.70.469. [DOI] [PubMed] [Google Scholar]
- 14.Tomioka Y, Ochiai K, Ohashi K, Kimura T, Umemura T. In ovo infection with an avian leukosis virus causing fowl glioma: viral distribution and pathogenesis. Avian Pathol. 2003;32:617–624. doi: 10.1080/03079450310001610640. [DOI] [PubMed] [Google Scholar]
- 15.Toyoda T, Ochiai K, Hatai H, Murakami M, Ono E, Kimura T, Umemura T. Cerebellar hypoplasia associated with an avian leukosis virus inducing fowl glioma. Vet Pathol. 2006;43:294–301. doi: 10.1354/vp.43-3-294. [DOI] [PubMed] [Google Scholar]
- 16.Hatai H, Ochiai K, Tomioka Y, Toyoda T, Hayashi K, Anada M, Kato M, Toda A, Ohashi K, Ono E, Kimura T, Umemura T. Nested polymerase chain reaction for detection of the avian leukosis virus causing so-called fowl glioma. Avian Pathol. 2005;34:473–479. doi: 10.1080/03079450500368086. [DOI] [PubMed] [Google Scholar]
- 17.Tomioka Y, Ochiai K, Ohashi K, Ono E, Toyoda T, Kimura T, Umemura T. Genome sequence analysis of the avian retrovirus causing so-called fowl glioma and the promoter activity of the long terminal repeat. J Gen Virol. 2004;85:647–652. doi: 10.1099/vir.0.79778-0. [DOI] [PubMed] [Google Scholar]
- 18.Anzil AP, Stavrou D, Blizinger K. Type-C viral particles in cell cultures of chemically induced glioma in Sprague-Dawley rats. Vopr Onkol. 1978;24:30–32. [PubMed] [Google Scholar]
- 19.Armelin MC, Garrido J, Armelin HA. RNA tumor virus production accompanies the transformed phenotype change induced by hydrocortisone hormone in rat glioma cells. Cell Biol Int Rep. 1983;7:689–696. doi: 10.1016/0309-1651(83)90197-2. [DOI] [PubMed] [Google Scholar]
- 20.Boeke JD, Stoye JP. Retrotransposons, endogenous retroviruses, and the evolution of retroelements. In: Coffin JM, Hughes SH, Varmus HE, editors. Retroviruses. Cold Spring Harbor; New York: 1997. [PubMed] [Google Scholar]
- 21.Han JS, Boeke JD. LINE-1 retrotransposons: modulators of quantity and quality of mammalian gene expression? Bioessays. 2005;27:775–784. doi: 10.1002/bies.20257. [DOI] [PubMed] [Google Scholar]
- 22.Shapiro JA. Retrotransposons and regulatory suites. Bioessays. 2005;27:122–125. doi: 10.1002/bies.20192. [DOI] [PubMed] [Google Scholar]
- 23.Beraldi R, Pittoggi C, Sciamanna I, Mattei E, Spadafora C. Expression of LINE-1 retroposons is essential for murine preimplantation development. Mol Reprod Dev. 2006;73:279–287. doi: 10.1002/mrd.20423. [DOI] [PubMed] [Google Scholar]
- 24.Svoboda P, Stein P, Anger M, Bernstein E, Hannon GJ, Schultz RM. RNAi and expression of retrotransposons MuERV-L and IAP in preimplantation mouse embryos. Dev Biol. 2004;269:276–285. doi: 10.1016/j.ydbio.2004.01.028. [DOI] [PubMed] [Google Scholar]
- 25.Coufal NG, Garcia-Perez JL, Peng GE, Yeo GW, Mu Y, Lovci MT, Morell M, O’Shea KS, Moran JV, Gage FH. L1 retrotransposition in human neural progenitor cells. Nature. 2009;460:1127–1131. doi: 10.1038/nature08248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuwabara T, Hsieh J, Muotri A, Yeo G, Warashina M, Lie DC, Moore L, Nakashima K, Asashima M, Gage FH. Wnt-mediated activation of NeuroD1 and retro-elements during adult neurogenesis. Nat Neurosci. 2009;12:1097–1105. doi: 10.1038/nn.2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Konkel MK, Batzer MA. A mobile threat to genome stability: The impact of non-LTR retrotransposons upon the human genome. Semin Cancer Biol. 2010;20:211–221. doi: 10.1016/j.semcancer.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilkins AS. The enemy within: an epigenetic role of retrotransposons in cancer initiation. Bioessays. 2010;32:856–865. doi: 10.1002/bies.201000008. [DOI] [PubMed] [Google Scholar]
- 29.Misra A, Chosdol K, Sarkar C, Mahapatra AK, Sinha S. Alteration of a sequence with homology to human endogenous retrovirus (HERV-K) in primary human glioma: implications for viral repeat mediated rearrangement. Mutat Res. 2001;484:53–59. doi: 10.1016/s0027-5107(01)00240-8. [DOI] [PubMed] [Google Scholar]
- 30.Michaelis M, Doerr HW, Cinatl J. The story of human cytomegalovirus and cancer: increasing evidence and open questions. Neoplasia. 2009;11:1–9. doi: 10.1593/neo.81178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cinatl J, Jr, Nevels M, Paulus C, Michaelis M. Activation of telomerase in glioma cells by human cytomegalovirus: another piece of the puzzle. J Natl Cancer Inst. 2009;101:441–443. doi: 10.1093/jnci/djp047. [DOI] [PubMed] [Google Scholar]
- 32.Soderberg-Naucler C. Does cytomegalovirus play a causative role in the development of various inflammatory diseases and cancer? J Intern Med. 2006;259:219–246. doi: 10.1111/j.1365-2796.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- 33.Soderberg-Naucler C. HCMV microinfections in inflammatory diseases and cancer. J Clin Virol. 2008;41:218–223. doi: 10.1016/j.jcv.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 34.Soderberg-Naucler C. Human cytomegalovirus persists in its host and attacks and avoids elimination by the immune system. Crit Rev Immunol. 2006;26:231–264. doi: 10.1615/critrevimmunol.v26.i3.30. [DOI] [PubMed] [Google Scholar]
- 35.Gredmark-Russ S, Dzabic M, Rahbar A, Wanhainen A, Bjorck M, Larsson E, Michel JB, Soderberg-Naucler C. Active cytomegalovirus infection in aortic smooth muscle cells from patients with abdominal aortic aneurysm. J Mol Med. 2009;87:347–356. doi: 10.1007/s00109-008-0413-4. [DOI] [PubMed] [Google Scholar]
- 36.Cinatl J, Jr, Nevels M, Paulus C, Michaelis M. Activation of telomerase in glioma cells by human cytomegalovirus: another piece of the puzzle. J Natl Cancer Inst. 2009;101:441–443. doi: 10.1093/jnci/djp047. [DOI] [PubMed] [Google Scholar]
- 37.Varani S, Mastroianni A, Frascaroli G, Tammik C, Rahbar A, Christensson M, Rossini G, Landini MP, Soderberg-Naucler C. Generalized Wegener’s granulomatosis in an immuno-competent adult after cytomegalovirus mononucleosis and bacterial urinary tract infection. Arthritis Rheum. 2009;60:1558–1562. doi: 10.1002/art.24487. [DOI] [PubMed] [Google Scholar]
- 38.Varani S, Frascaroli G, Landini MP, Soderberg-Naucler C. Human cytomegalovirus targets different subsets of antigen-presenting cells with pathological consequences for host immunity: implications for immunosuppression, chronic inflammation and autoimmunity. Rev Med Virol. 2009;19:131–145. doi: 10.1002/rmv.609. [DOI] [PubMed] [Google Scholar]
- 39.Cederarv M, Soderberg-Naucler C, Odeberg J. HCMV infection of PDCs deviates the NK cell response into cytokine-producing cells unable to perform cytotoxicity. Immunobiology. 2009;214:331–341. doi: 10.1016/j.imbio.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 40.Gredmark S, Jonasson L, Van Gosliga D, Ernerudh J, Soderberg-Naucler C. Active cytomegalovirus replication in patients with coronary disease. Scand Cardiovasc J. 2007;41:230–234. doi: 10.1080/14017430701383755. [DOI] [PubMed] [Google Scholar]
- 41.Larsson S, Soderberg-Naucler C, Wang FZ, Moller E. Cytomegalovirus DNA can be detected in peripheral blood mononuclear cells from all seropositive and most seronegative healthy blood donors over time. Transfusion. 1998;38:271–278. doi: 10.1046/j.1537-2995.1998.38398222871.x. [DOI] [PubMed] [Google Scholar]
- 42.Straat K, Liu C, Rahbar A, Zhu Q, Liu L, Wolmer-Solberg N, Lou F, Liu Z, Shen J, Jia J, Kyo S, Bjorkholm M, Sjoberg J, Soderberg-Naucler C, Xu D. Activation of telomerase by human cytomegalovirus. J Natl Cancer Inst. 2009;101:488–497. doi: 10.1093/jnci/djp031. [DOI] [PubMed] [Google Scholar]
- 43.Fuccillo DA, Sever JL, Moder FL, Chen TC, Catalano LW, Johnson LD. Cytomegalovirus antibody in patients with carcinoma of the uterine cervix. Obstet Gynecol. 1971;38:599–601. doi: 10.1097/00006250-197110000-00016. [DOI] [PubMed] [Google Scholar]
- 44.Harkins L, Volk AL, Samanta M, Mikolaenko I, Britt WJ, Bland KI, Cobbs CS. Specific localisation of human cytomegalovirus nucleic acids and proteins in human colorectal cancer. Lancet. 2002;360:1557–1563. doi: 10.1016/S0140-6736(02)11524-8. [DOI] [PubMed] [Google Scholar]
- 45.Samanta M, Harkins L, Klemm K, Britt WJ, Cobbs CS. High prevalence of human cytomegalovirus in prostatic intraepithelial neoplasia and prostatic carcinoma. J Urol. 2003;170:998–1002. doi: 10.1097/01.ju.0000080263.46164.97. [DOI] [PubMed] [Google Scholar]
- 46.Cobbs CS, Harkins L, Samanta M, Gillespie GY, Bharara S, King PH, Nabors LB, Cobbs CG, Britt WJ. Human cytomegalovirus infection and expression in human malignant glioma. Cancer Res. 2002;62:3347–3350. [PubMed] [Google Scholar]
- 47.Scheurer ME, El-Zein R, Bondy ML, Harkins L, Cobbs CS. RE: “Lack of association of herpesviruses with brain tumors”. J Neurovirol. 2007;13:85. doi: 10.1080/13550280601164325. author reply 86–87. [DOI] [PubMed] [Google Scholar]
- 48.Miller G. Brain cancer. A viral link to glioblastoma? Science. 2009;323:30–31. doi: 10.1126/science.323.5910.30. [DOI] [PubMed] [Google Scholar]
- 49.Scheurer ME, Bondy ML, Aldape KD, Albrecht T, El-Zein R. Detection of human cytomegalovirus in different histological types of gliomas. Acta Neuropathol. 2008;116:79–86. doi: 10.1007/s00401-008-0359-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mitchell DA, Xie W, Schmittling R, Learn C, Friedman A, McLendon RE, Sampson JH. Sensitive detection of human cytomegalovirus in tumors and peripheral blood of patients diagnosed with glioblastoma. Neuro Oncol. 2008;10:10–18. doi: 10.1215/15228517-2007-035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Luo MH, Fortunato EA. Long-term infection and shedding of human cytomegalovirus in T98G glioblastoma cells. J Virol. 2007;81:10424–10436. doi: 10.1128/JVI.00866-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barami K. Oncomodulatory mechanisms of human cytomegalovirus in gliomas. J Clin Neurosci. 2010;17:819–823. doi: 10.1016/j.jocn.2009.10.040. [DOI] [PubMed] [Google Scholar]
- 53.Lucas KG, Bao L, Bruggeman R, Dunham K, Specht C. The detection of CMV pp65 and IE1 in glioblastoma multiforme. J Neurooncol. 2011;103:231–238. doi: 10.1007/s11060-010-0383-6. [DOI] [PubMed] [Google Scholar]
- 54.Prins RM, Cloughesy TF, Liau LM. Cytomegalovirus immunity after vaccination with autologous glioblastoma lysate. N Engl J Med. 2008;359:539–541. doi: 10.1056/NEJMc0804818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Seri B, Herrera DG, Gritti A, Ferron S, Collado L, Vescovi A, Garcia-Verdugo JM, Alvarez-Buylla A. Composition and organization of the SCZ: a large germinal layer containing neural stem cells in the adult mammalian brain. Cereb Cortex. 2006;16(Suppl 1):i103–i111. doi: 10.1093/cercor/bhk027. [DOI] [PubMed] [Google Scholar]
- 56.Perlman JM, Argyle C. Lethal cytomegalovirus infection in preterm infants: clinical, radiological, and neuropathological findings. Ann Neurol. 1992;31:64–68. doi: 10.1002/ana.410310112. [DOI] [PubMed] [Google Scholar]
- 57.Odeberg J, Wolmer N, Falci S, Westgren M, Sundtrom E, Seiger A, Soderberg-Naucler C. Late human cytomegalovirus (HCMV) proteins inhibit differentiation of human neural precursor cells into astrocytes. J Neurosci Res. 2007;85:583–593. doi: 10.1002/jnr.21144. [DOI] [PubMed] [Google Scholar]
- 58.Fritschy JM, Brandner S, Aguzzi A, Koedood M, Luscher B, Mitchell PJ. Brain cell type specificity and gliosis-induced activation of the human cytomegalovirus immediate-early promoter in transgenic mice. J Neurosci. 1996;16:2275–2282. doi: 10.1523/JNEUROSCI.16-07-02275.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Odeberg J, Wolmer N, Falci S, Westgren M, Seiger A, Soderberg-Naucler C. Human cytomegalovirus inhibits neuronal differentiation and induces apoptosis in human neural precursor cells. J Virol. 2006;80:8929–8939. doi: 10.1128/JVI.00676-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Koh K, Lee K, Ahn JH, Kim S. Human cytomegalovirus infection downregulates the expression of glial fibrillary acidic protein in human glioblastoma U373MG cells: identification of viral genes and protein domains involved. J Gen Virol. 2009;90:954–962. doi: 10.1099/vir.0.006486-0. [DOI] [PubMed] [Google Scholar]
- 61.Lee K, Jeon K, Kim JM, Kim VN, Choi DH, Kim SU, Kim S. Downregulation of GFAP, TSP-1, and p53 in human glioblastoma cell line, U373MG, by IE1 protein from human cytomegalovirus. Glia. 2005;51:1–12. doi: 10.1002/glia.20179. [DOI] [PubMed] [Google Scholar]
- 62.McCarthy M, Wood C, Fedoseyeva L, Whittemore SR. Media components influence viral gene expression assays in human fetal astrocyte cultures. J Neurovirol. 1995;1:275–285. doi: 10.3109/13550289509114024. [DOI] [PubMed] [Google Scholar]
- 63.Cheeran MC, Hu S, Gekker G, Lokensgard JR. Decreased cytomegalovirus expression following proinflammatory cytokine treatment of primary human astrocytes. J Immunol. 2000;164:926–933. doi: 10.4049/jimmunol.164.2.926. [DOI] [PubMed] [Google Scholar]
- 64.Lokensgard JR, Cheeran MC, Gekker G, Hu S, Chao CC, Peterson PK. Human cytomegalovirus replication and modulation of apoptosis in astrocytes. J Hum Virol. 1999;2:91–101. [PubMed] [Google Scholar]
- 65.Cheeran MC, Hu S, Ni HT, Sheng W, Palmquist JM, Peterson PK, Lokensgard JR. Neural precursor cell susceptibility to human cytomegalovirus diverges along glial or neuronal differentiation pathways. J Neurosci Res. 2005;82:839–850. doi: 10.1002/jnr.20682. [DOI] [PubMed] [Google Scholar]
- 66.Wolff D, Sinzger C, Drescher P, Jahn G, Plachter B. Reduced levels of IE2 gene expression and shutdown of early and late viral genes during latent infection of the glioblastoma cell line U138-MG with selectable recombinants of human cytomegalovirus. Virology. 1994;204:101–113. doi: 10.1006/viro.1994.1514. [DOI] [PubMed] [Google Scholar]
- 67.Wu J, O’Neill J, Barbosa MS. Transcription factor Sp1 mediates cell-specific trans-activation of the human cytomegalovirus DNA polymerase gene promoter by immediate-early protein IE86 in glioblastoma U373MG cells. J Virol. 1998;72:236–244. doi: 10.1128/jvi.72.1.236-244.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Erlandsson A, Brannvall K, Gustafsdottir S, Westermark B, Forsberg-Nilsson K. Autocrine/paracrine platelet-derived growth factor regulates proliferation of neural progenitor cells. Cancer Res. 2006;66:8042–8048. doi: 10.1158/0008-5472.CAN-06-0900. [DOI] [PubMed] [Google Scholar]
- 69.Thorarinsdottir HK, Santi M, McCarter R, Rushing EJ, Cornelison R, Jales A, MacDonald TJ. Protein expression of platelet-derived growth factor receptor correlates with malignant histology and PTEN with survival in childhood gliomas. Clin Cancer Res. 2008;14:3386–3394. doi: 10.1158/1078-0432.CCR-07-1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Assanah M, Lochhead R, Ogden A, Bruce J, Goldman J, Canoll P. Glial progenitors in adult white matter are driven to form malignant gliomas by platelet-derived growth factor-expressing retroviruses. J Neurosci. 2006;26:6781–6790. doi: 10.1523/JNEUROSCI.0514-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Soroceanu L, Akhavan A, Cobbs CS. Platelet-derived growth factor-alpha receptor activation is required for human cytomegalovirus infection. Nature. 2008;455:391–395. doi: 10.1038/nature07209. [DOI] [PubMed] [Google Scholar]
- 72.Gredmark S, Straat K, Homman-Loudiyi M, Kannisto K, Soderberg-Naucler C. Human cytomegalovirus down-regulates expression of receptors for platelet-derived growth factor by smooth muscle cells. J Virol. 2007;81:5112–5120. doi: 10.1128/JVI.02197-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kuwahara R, Kofman AV, Landis CS, Swenson ES, Barendswaard E, Theise ND. The hepatic stem cell niche: identification by label-retaining cell assay. Hepatology. 2008;47:1994–2002. doi: 10.1002/hep.22218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Philips A, Huet X, Plet A, Le Cam L, Vie A, Blanchard JM. The retinoblastoma protein is essential for cyclin A repression in quiescent cells. Oncogene. 1998;16:1373–1381. doi: 10.1038/sj.onc.1201655. [DOI] [PubMed] [Google Scholar]
- 75.Kalejta RF, Shenk T. Proteasome-dependent, ubiquitin-independent degradation of the Rb family of tumor suppressors by the human cytomegalovirus pp71 protein. Proc Natl Acad Sci USA. 2003;100:3263–3268. doi: 10.1073/pnas.0538058100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kalejta RF, Bechtel JT, Shenk T. Human cytomegalovirus pp71 stimulates cell cycle progression by inducing the proteasome-dependent degradation of the retinoblastoma family of tumor suppressors. Mol Cell Biol. 2003;23:1885–1895. doi: 10.1128/MCB.23.6.1885-1895.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Boldogh I, AbuBakar S, Albrecht T. Activation of proto-oncogenes: an immediate early event in human cytomegalovirus infection. Science. 1990;247:561–564. doi: 10.1126/science.1689075. [DOI] [PubMed] [Google Scholar]
- 78.Spiller OB, Borysiewicz LK, Morgan BP. Development of a model for cytomegalovirus infection of oligodendrocytes. J Gen Virol. 1997;78(Pt 12):3349–3356. doi: 10.1099/0022-1317-78-12-3349. [DOI] [PubMed] [Google Scholar]
- 79.Cobbs CS, Soroceanu L, Denham S, Zhang W, Kraus MH. Modulation of oncogenic phenotype in human glioma cells by cytomegalovirus IE1-mediated mitogenicity. Cancer Res. 2008;68:724–730. doi: 10.1158/0008-5472.CAN-07-2291. [DOI] [PubMed] [Google Scholar]
- 80.Maussang D, Verzijl D, van Walsum M, Leurs R, Holl J, Pleskoff O, Michel D, van Dongen GA, Smit MJ. Human cytomegalovirus-encoded chemokine receptor US28 promotes tumorigenesis. Proc Natl Acad Sci USA. 2006;103:13068–13073. doi: 10.1073/pnas.0604433103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Menendez D, Inga A, Resnick MA. The expanding universe of p53 targets. Nat Rev Cancer. 2009;9:724–737. doi: 10.1038/nrc2730. [DOI] [PubMed] [Google Scholar]
- 82.Weisz L, Oren M, Rotter V. Transcription regulation by mutant p53. Oncogene. 2007;26:2202–2211. doi: 10.1038/sj.onc.1210294. [DOI] [PubMed] [Google Scholar]
- 83.Deb S, Jackson CT, Subler MA, Martin DW. Modulation of cellular and viral promoters by mutant human p53 proteins found in tumor cells. J Virol. 1992;66:6164–6170. doi: 10.1128/jvi.66.10.6164-6170.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cinatl J, Scholz M, Kotchetkov R, Vogel JU, Doerr HW. Molecular mechanisms of the modulatory effects of HCMV infection in tumor cell biology. Trends Mol Med. 2004;10:19–23. doi: 10.1016/j.molmed.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 85.Cinatl J, Jr, Vogel JU, Kotchetkov R, Wilhelm Doerr H. Oncomodulatory signals by regulatory proteins encoded by human cytomegalovirus: a novel role for viral infection in tumor progression. FEMS Microbiol Rev. 2004;28:59–77. doi: 10.1016/j.femsre.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 86.Castillo JP, Kowalik TF. HCMV infection: modulating the cell cycle and cell death. Int Rev Immunol. 2004;23:113–139. doi: 10.1080/08830180490265565. [DOI] [PubMed] [Google Scholar]
- 87.Sanchez V, Spector DH. Subversion of cell cycle regulatory pathways. Curr Top Microbiol Immunol. 2008;325:243–262. doi: 10.1007/978-3-540-77349-8_14. [DOI] [PubMed] [Google Scholar]
- 88.Song YJ, Stinski MF. Inhibition of cell division by the human cytomegalovirus IE86 protein: role of the p53 pathway or cyclin-dependent kinase 1/cyclin B1. J Virol. 2005;79:2597–2603. doi: 10.1128/JVI.79.4.2597-2603.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Muralidhar S, Doniger J, Mendelson E, Araujo JC, Kashanchi F, Azumi N, Brady JN, Rosenthal LJ. Human cytomegalo-virus mtrII oncoprotein binds to p53 and down-regulates p53-activated transcription. J Virol. 1996;70:8691–8700. doi: 10.1128/jvi.70.12.8691-8700.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nevels M, Paulus C, Shenk T. Human cytomegalovirus immediate-early 1 protein facilitates viral replication by antagonizing histone deacetylation. Proc Natl Acad Sci USA. 2004;101:17234–17239. doi: 10.1073/pnas.0407933101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hartmann M, Brunnemann H. Chromosome aberrations in cytomegalovirus-infected human diploid cell culture. Acta Virol. 1972;16:176. [PubMed] [Google Scholar]
- 92.Fortunato EA, Spector DH. Viral induction of site-specific chromosome damage. Rev Med Virol. 2003;13:21–37. doi: 10.1002/rmv.368. [DOI] [PubMed] [Google Scholar]
- 93.Fortunato EA, Dell’Aquila ML, Spector DH. Specific chromosome 1 breaks induced by human cytomegalovirus. Proc Natl Acad Sci USA. 2000;97:853–858. doi: 10.1073/pnas.97.2.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Baumgartner M, Schneider R, Auer B, Herzog H, Schweiger M, Hirsch-Kauffmann M. Fluorescence in situ mapping of the human nuclear NAD + ADP-ribosyltransferase gene (AD-PRT) and two secondary sites to human chromosomal bands 1q42, 13q34, and 14q24. Cytogenet Cell Genet. 1992;61:172–174. doi: 10.1159/000133400. [DOI] [PubMed] [Google Scholar]
- 95.Li YS, Ramsay DA, Fan YS, Armstrong RF, Del Maestro RF. Cytogenetic evidence that a tumor suppressor gene in the long arm of chromosome 1 contributes to glioma growth. Cancer Genet Cytogenet. 1995;84:46–50. doi: 10.1016/0165-4608(95)00065-8. [DOI] [PubMed] [Google Scholar]
- 96.Bieche I, Champeme MH, Lidereau R. Loss and gain of distinct regions of chromosome 1q in primary breast cancer. Clin Cancer Res. 1995;1:123–127. [PubMed] [Google Scholar]
- 97.Shen Y, Zhu H, Shenk T. Human cytomagalovirus IE1 and IE2 proteins are mutagenic and mediate “hit-and-run” oncogenic transformation in cooperation with the adenovirus E1A proteins. Proc Natl Acad Sci U S A. 1997;94:3341–3345. doi: 10.1073/pnas.94.7.3341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Boldogh I, Huang ES, Rady P, Arany I, Tyring S, Albrecht T. Alteration in the coding potential and expression of H-ras in human cytomegalovirus-transformed cells. Intervirology. 1994;37:321–329. doi: 10.1159/000150396. [DOI] [PubMed] [Google Scholar]
- 99.Dolan A, Cunningham C, Hector RD, Hassan-Walker AF, Lee L, Addison C, Dargan DJ, McGeoch DJ, Gatherer D, Emery VC, Griffiths PD, Sinzger C, McSharry BP, Wilkinson GW, Davison AJ. Genetic content of wild-type human cytomegalovirus. J Gen Virol. 2004;85:1301–1312. doi: 10.1099/vir.0.79888-0. [DOI] [PubMed] [Google Scholar]
- 100.Hahn G, Revello MG, Patrone M, Percivalle E, Campanini G, Sarasini A, Wagner M, Gallina A, Milanesi G, Koszinowski U, Baldanti F, Gerna G. Human cytomegalovirus UL131–128 genes are indispensable for virus growth in endothelial cells and virus transfer to leukocytes. J Virol. 2004;78:10023–10033. doi: 10.1128/JVI.78.18.10023-10033.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gerna G, Percivalle E, Lilleri D, Lozza L, Fornara C, Hahn G, Baldanti F, Revello MG. Dendritic-cell infection by human cytomegalovirus is restricted to strains carrying functional UL131–128 genes and mediates efficient viral antigen presentation to CD8+ T cells. J Gen Virol. 2005;86:275–284. doi: 10.1099/vir.0.80474-0. [DOI] [PubMed] [Google Scholar]
- 102.Geder L, Laychock AM, Gorodecki J, Rapp F. Alterations in biological properties of different lines of cytomegalorivus-transformed human embryo lung cells following in vitro cultivation. IARC Sci Publ. 1978;24:591–601. [PubMed] [Google Scholar]
- 103.Washington AT, Singh G, Aiyar A. Diametrically opposed effects of hypoxia and oxidative stress on two viral transactivators. Virol J. 2010;7:93. doi: 10.1186/1743-422X-7-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pipiya T, Sauthoff H, Huang YQ, Chang B, Cheng J, Heitner S, Chen S, Rom WN, Hay JG. Hypoxia reduces adenoviral replication in cancer cells by downregulation of viral protein expression. Gene Ther. 2005;12:911–917. doi: 10.1038/sj.gt.3302459. [DOI] [PubMed] [Google Scholar]
- 105.Haque M, Davis DA, Wang V, Widmer I, Yarchoan R. Kaposi’s sarcoma-associated herpesvirus (human herpesvirus 8) contains hypoxia response elements: relevance to lytic induction by hypoxia. J Virol. 2003;77:6761–6768. doi: 10.1128/JVI.77.12.6761-6768.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Davis DA, Rinderknecht AS, Zoeteweij JP, Aoki Y, Read-Connole EL, Tosato G, Blauvelt A, Yarchoan R. Hypoxia induces lytic replication of Kaposi sarcoma-associated herpes-virus. Blood. 2001;97:3244–3250. doi: 10.1182/blood.v97.10.3244. [DOI] [PubMed] [Google Scholar]
- 107.Pina-Oviedo S, Khalili K, Del Valle L. Hypoxia inducible factor-1 alpha activation of the JCV promoter: role in the pathogenesis of progressive multifocal leukoencephalopathy. Acta Neuropathol. 2009;118:235–247. doi: 10.1007/s00401-009-0533-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Nakamura M, Bodily JM, Beglin M, Kyo S, Inoue M, Laimins LA. Hypoxia-specific stabilization of HIF-1alpha by human papillomaviruses. Virology. 2009;387:442–448. doi: 10.1016/j.virol.2009.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fasullo M, Burch AD, Britton A. Hypoxia enhances the replication of oncolytic herpes simplex virus in p53- breast cancer cells. Cell Cycle. 2009;8:2194–2197. doi: 10.4161/cc.8.14.8934. [DOI] [PubMed] [Google Scholar]
- 110.Haeberle HA, Durrstein C, Rosenberger P, Hosakote YM, Kuhlicke J, Kempf VA, Garofalo RP, Eltzschig HK. Oxygen-independent stabilization of hypoxia inducible factor (HIF)-1 during RSV infection. PLoS One. 2008;3:e3352. doi: 10.1371/journal.pone.0003352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jiang JH, Wang N, Li A, Liao WT, Pan ZG, Mai SJ, Li DJ, Zeng MS, Wen JM, Zeng YX. Hypoxia can contribute to the induction of the Epstein-Barr virus (EBV) lytic cycle. J Clin Virol. 2006;37:98–103. doi: 10.1016/j.jcv.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 112.Cobbs CS, Soroceanu L, Denham S, Zhang W, Britt WJ, Pieper R, Kraus MH. Human cytomegalovirus induces cellular tyrosine kinase signaling and promotes glioma cell invasiveness. J Neurooncol. 2007;85:271–280. doi: 10.1007/s11060-007-9423-2. [DOI] [PubMed] [Google Scholar]
- 113.Ablashi DV, Josephs SF, Buchbinder A, Hellman K, Nakamura S, Llana T, Lusso P, Kaplan M, Dahlberg J, Memon S, et al. Human B-lymphotropic virus (human herpesvirus-6) J Virol Methods. 1988;21:29–48. doi: 10.1016/0166-0934(88)90050-x. [DOI] [PubMed] [Google Scholar]
- 114.Flamand L, Komaroff AL, Arbuckle JH, Medveczky PG, Ablashi DV. Review, part 1: Human herpesvirus-6-basic biology, diagnostic testing, and antiviral efficacy. J Med Virol. 2010;82:1560–1568. doi: 10.1002/jmv.21839. [DOI] [PubMed] [Google Scholar]
- 115.Tang H, Mori Y. Human herpesvirus-6 entry into host cells. Future Microbiol. 2010;5:1015–1023. doi: 10.2217/fmb.10.61. [DOI] [PubMed] [Google Scholar]
- 116.Revest M, Minjolle S, Veyer D, Lagathu G, Michelet C, Colimon R. Detection of HHV-6 in over a thousand samples: New types of infection revealed by an analysis of positive results. J Clin Virol. 2011;51:20–24. doi: 10.1016/j.jcv.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 117.Yao K, Crawford JR, Komaroff AL, Ablashi DV, Jacobson S. Review part 2: Human herpesvirus-6 in central nervous system diseases. J Med Virol. 2010;82:1669–1678. doi: 10.1002/jmv.21861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ablashi DV, Devin CL, Yoshikawa T, Lautenschlager I, Luppi M, Kuhl U, Komaroff AL. Review Part 3: Human herpesvirus-6 in multiple non-neurological diseases. J Med Virol. 2010;82:1903–1910. doi: 10.1002/jmv.21860. [DOI] [PubMed] [Google Scholar]
- 119.Chan PK, Ng HK, Cheng AF. Detection of human herpesviruses 6 and 7 genomic sequences in brain tumours. J Clin Pathol. 1999;52:620–623. doi: 10.1136/jcp.52.8.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Crawford JR, Santi MR, Thorarinsdottir HK, Cornelison R, Rushing EJ, Zhang H, Yao K, Jacobson S, Macdonald TJ. Detection of human herpesvirus-6 variants in pediatric brain tumors: association of viral antigen in low grade gliomas. J Clin Virol. 2009;46:37–42. doi: 10.1016/j.jcv.2009.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cuomo L, Trivedi P, Cardillo MR, Gagliardi FM, Vecchione A, Caruso R, Calogero A, Frati L, Faggioni A, Ragona G. Human herpesvirus 6 infection in neoplastic and normal brain tissue. J Med Virol. 2001;63:45–51. [PubMed] [Google Scholar]
- 122.Luppi M, Barozzi P, Maiorana A, Marasca R, Trovato R, Fano R, Ceccherini-Nelli L, Torelli G. Human herpesvirus-6: a survey of presence and distribution of genomic sequences in normal brain and neuroglial tumors. J Med Virol. 1995;47:105–111. doi: 10.1002/jmv.1890470119. [DOI] [PubMed] [Google Scholar]
- 123.Neves AM, Thompson G, Carvalheira J, Trindade JC, Rueff J, Caetano JM, Casey JW, Hermouet S. Detection and quantitative analysis of human herpesvirus in pilocytic astrocytoma. Brain Res. 2008;1221:108–114. doi: 10.1016/j.brainres.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 124.Rantala H, Mannonen L, Ahtiluoto S, Linnavuori K, Herva R, Vaheri A, Koskiniemi M. Human herpesvirus-6 associated encephalitis with subsequent infantile spasms and cerebellar astrocytoma. Dev Med Child Neurol. 2000;42:418–421. doi: 10.1017/s0012162200000773. [DOI] [PubMed] [Google Scholar]
- 125.Stodberg T, Deniz Y, Esteitie N, Jacobsson B, Mousavi-Jazi M, Dahl H, Zweygberg WB, Grillner L, Linde A. A case of diffuse leptomeningeal oligodendrogliomatosis associated with HHV-6 variant A. Neuropediatrics. 2002;33:266–270. doi: 10.1055/s-2002-36739. [DOI] [PubMed] [Google Scholar]
- 126.Albright AV, Lavi E, Black JB, Goldberg S, O’Connor MJ, Gonzalez-Scarano F. The effect of human herpesvirus-6 (HHV-6) on cultured human neural cells: oligodendrocytes and microglia. J Neurovirol. 1998;4:486–494. doi: 10.3109/13550289809113493. [DOI] [PubMed] [Google Scholar]
- 127.Donati D, Martinelli E, Cassiani-Ingoni R, Ahlqvist J, Hou J, Major EO, Jacobson S. Variant-specific tropism of human herpesvirus 6 in human astrocytes. J Virol. 2005;79:9439–9448. doi: 10.1128/JVI.79.15.9439-9448.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dietrich J, Blumberg BM, Roshal M, Baker JV, Hurley SD, Mayer-Proschel M, Mock DJ. Infection with an endemic human herpesvirus disrupts critical glial precursor cell properties. J Neurosci. 2004;24:4875–4883. doi: 10.1523/JNEUROSCI.5584-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Studebaker AW, Kreofsky CR, Pierson CR, Russell SJ, Galanis E, Raffel C. Treatment of medulloblastoma with a modified measles virus. Neuro Oncol. 2010;12:1034–1042. doi: 10.1093/neuonc/noq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kong H, Baerbig Q, Duncan L, Shepel N, Mayne M. Human herpesvirus type 6 indirectly enhances oligodendrocyte cell death. J Neurovirol. 2003;9:539–550. doi: 10.1080/13550280390241241. [DOI] [PubMed] [Google Scholar]
- 131.Strenger V, Urban C, Schwinger W, Nacheva EP, Aberle SW. Transmission of chromosomally integrated HHV-6 by bone marrow transplantation. Pediatr Blood Cancer. 2011;56:171. doi: 10.1002/pbc.22828. [DOI] [PubMed] [Google Scholar]
- 132.Arbuckle JH, Medveczky PG. The molecular biology of human herpesvirus-6 latency and telomere integration. Microbes Infect. 2011 doi: 10.1016/j.micinf.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Strenger V, Aberle SW, Wendelin G, Pfurtscheller K, Nacheva EP, Zobel G, Nagel B. Chromosomal integration of the HHV-6 genome as a possible cause of HHV-6 detection in cardiac tissues. J Clin Pathol. 2010;63:1129–1130. doi: 10.1136/jcp.2010.079277. [DOI] [PubMed] [Google Scholar]
- 134.Lohi O, Arola M, Lautenschlager I, Nacheva EP, Vettenranta K. A high circulating copy number of HHV-6 due to chromosomal integration in a child with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2010;55:1236–1238. doi: 10.1002/pbc.22671. [DOI] [PubMed] [Google Scholar]
- 135.Doniger J, Muralidhar S, Rosenthal LJ. Human cytomegalovirus and human herpesvirus 6 genes that transform and transactivate. Clin Microbiol Rev. 1999;12:367–382. doi: 10.1128/cmr.12.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lusso P. HHV-6 and the immune system: mechanisms of immunomodulation and viral escape. J Clin Virol. 2006;37(Suppl 1):4–10. doi: 10.1016/S1386-6532(06)70004-X. [DOI] [PubMed] [Google Scholar]
- 137.Arena A, Liberto MC, Iannello D, Capozza AB, Foca A. Altered cytokine production after human herpes virus type 6 infection. New Microbiol. 1999;22:293–300. [PubMed] [Google Scholar]
- 138.Watanabe H, Tohyama M, Kamijima M, Nakajima T, Yoshida T, Hashimoto K, Iijima M. Occupational trichloroethylene hypersensitivity syndrome with human herpesvirus-6 and cytomegalovirus reactivation. Dermatology. 2010;221:17–22. doi: 10.1159/000290775. [DOI] [PubMed] [Google Scholar]
- 139.Cameron B, Flamand L, Juwana H, Middeldorp J, Naing Z, Rawlinson W, Ablashi D, Lloyd A. Serological and virological investigation of the role of the herpesviruses EBV, CMV and HHV-6 in post-infective fatigue syndrome. J Med Virol. 2010;82:1684–1688. doi: 10.1002/jmv.21873. [DOI] [PubMed] [Google Scholar]
- 140.Clark DA, Emery VC, Griffiths PD. Cytomegalovirus, human herpesvirus-6, and human herpesvirus-7 in hematological patients. Semin Hematol. 2003;40:154–162. doi: 10.1053/shem.2003.50015. [DOI] [PubMed] [Google Scholar]
- 141.Michalek J, Horvath R. High incidence of Epstein-Barr virus, cytomegalovirus and human herpesvirus 6 infections in children with cancer. BMC Pediatr. 2002;2:1. doi: 10.1186/1471-2431-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Leach CT, Pollock BH, McClain KL, Parmley RT, Murphy SB, Jenson HB. Human herpesvirus 6 and cytomegalovirus infections in children with human immunodeficiency virus infection and cancer. Pediatr Infect Dis J. 2002;21:125–132. doi: 10.1097/00006454-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 143.Hillyer CD, Lankford KV, Roback JD, Gillespie TW, Silberstein LE. Transfusion of the HIV-seropositive patient: immunomodulation, viral reactivation, and limiting exposure to EBV (HHV-4), CMV (HHV-5), and HHV-6, 7, and 8. Transfus Med Rev. 1999;13:1–17. doi: 10.1016/s0887-7963(99)80084-4. [DOI] [PubMed] [Google Scholar]
- 144.Michalek J, Horvath R, Benedik J, Hrstkova H. Human herpesvirus-6 infection in children with cancer. Pediatr Hematol Oncol. 1999;16:423–430. doi: 10.1080/088800199276976. [DOI] [PubMed] [Google Scholar]
- 145.Knipe DM, Cliffe A. Chromatin control of herpes simplex virus lytic and latent infection. Nat Rev Microbiol. 2008;6:211–221. doi: 10.1038/nrmicro1794. [DOI] [PubMed] [Google Scholar]
- 146.Jones C. Cervical cancer: is herpes simplex virus type II a cofactor? Clin Microbiol Rev. 1995;8:549–556. doi: 10.1128/cmr.8.4.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Parker TM, Smith EM, Ritchie JM, Haugen TH, Vonka V, Turek LP, Hamsikova E. Head and neck cancer associated with herpes simplex virus 1 and 2 and other risk factors. Oral Oncol. 2006;42:288–296. doi: 10.1016/j.oraloncology.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 148.Jensen K, Patel A, Larin A, Hoperia V, Saji M, Bauer A, Yim K, Hemming V, Vasko V. Human herpes simplex viruses in benign and malignant thyroid tumours. J Pathol. 2010;221:193–200. doi: 10.1002/path.2701. [DOI] [PubMed] [Google Scholar]
- 149.Prandovszky E, Horvath S, Gellert L, Kovacs SK, Janka Z, Toldi J, Shukla D, Valyi-Nagy T. Nectin-1 (HveC) is expressed at high levels in neural subtypes that regulate radial migration of cortical and cerebellar neurons of the developing human and murine brain. J Neurovirol. 2008;14:164–172. doi: 10.1080/13550280801898672. [DOI] [PubMed] [Google Scholar]
- 150.Guzman G, Oh S, Shukla D, Engelhard HH, Valyi-Nagy T. Expression of entry receptor nectin-1 of herpes simplex virus 1 and/or herpes simplex virus 2 in normal and neoplastic human nervous system tissues. Acta Virol. 2006;50:59–66. [PubMed] [Google Scholar]
- 151.Shukla D, Scanlan PM, Tiwari V, Sheth V, Clement C, Guzman-Hartman G, Dermody TS, Valyi-Nagy T. Expression of nectin-1 in normal and herpes simplex virus type 1-infected murine brain. Appl Immunohistochem Mol Morphol. 2006;14:341–347. doi: 10.1097/00129039-200609000-00014. [DOI] [PubMed] [Google Scholar]
- 152.Horvath S, Prandovszky E, Kis Z, Krummenacher C, Eisenberg RJ, Cohen GH, Janka Z, Toldi J. Spatiotemporal changes of the herpes simplex virus entry receptor nectin-1 in murine brain during postnatal development. J Neurovirol. 2006;12:161–170. doi: 10.1080/13550280600760594. [DOI] [PubMed] [Google Scholar]
- 153.Chauvin C, Suh M, Remy C, Benabid AL. Failure to detect viral genomic sequences of three viruses (herpes simplex, simian virus 40 and adenovirus) in human and rat brain tumors. Ital J Neurol Sci. 1990;11:347–357. doi: 10.1007/BF02335937. [DOI] [PubMed] [Google Scholar]
- 154.Ochsner F. Contamination of a glioma by the herpes virus. Schweiz Arch Neurol Neurochir Psychiatr. 1981;129:19–30. [PubMed] [Google Scholar]
- 155.Frenkel N, Locker H, Cox B, Roizman B, Rapp F. Herpes simplex virus DNA in transformed cells: sequence complexity in five hamster cell lines and one derived hamster tumor. J Virol. 1976;18:885–893. doi: 10.1128/jvi.18.3.885-893.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Aurelian L. Persistence and expression of the herpes simplex virus type 2 genome in cervical tumor cells. Cancer Res. 1974;34:1126–1135. [PubMed] [Google Scholar]
- 157.Roizman B, Frenkel N. The transcription and state of herpes simplex virus DNA in productive infection and in human cervical cancer tissue. Cancer Res. 1973;33:1402–1416. [PubMed] [Google Scholar]
- 158.Frenkel N, Roizman B, Cassai E, Nahmias A. A DNA fragment of Herpes simplex 2 and its transcription in human cervical cancer tissue. Proc Natl Acad Sci USA. 1972;69:3784–3789. doi: 10.1073/pnas.69.12.3784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kessous-Elbaz A, Pelletier M, Cohen EA, Langelier Y. Retention and expression of the left end subfragment of the herpes simplex virus type 2 BglII N DNA fragment do not correlate with tumorigenic conversion of NIH 3T3 cells. J Gen Virol. 1989;70(Pt 8):2171–2177. doi: 10.1099/0022-1317-70-8-2171. [DOI] [PubMed] [Google Scholar]
- 160.Trimble JJ, Gay H, Docherty JJ. Characterization of the tumor-associated 38-kd protein of herpes simplex virus type 2. J Reprod Med. 1986;31:399–409. [PubMed] [Google Scholar]
- 161.Manservigi R, Cassai E, Deiss LP, Di Luca D, Segala V, Frenkel N. Sequences homologous to two separate transforming regions of herpes simplex virus DNA are linked in two human genital tumors. Virology. 1986;155:192–201. doi: 10.1016/0042-6822(86)90179-0. [DOI] [PubMed] [Google Scholar]
- 162.Iwasaka T, Smith C, Aurelian L, Ts’o PO. The cervical tumor-associated antigen (ICP-10/AG-4) is encoded by the transforming region of the genome of herpes simplex virus type 2. Jpn J Cancer Res. 1985;76:946–958. [PubMed] [Google Scholar]
- 163.Jiang X, Chentoufi AA, Hsiang C, Carpenter D, Osorio N, Benmohamed L, Fraser NW, Jones C, Wechsler SL. The herpes simplex virus type 1 latency-associated transcript can protect neuron-derived C1300 and Neuro2A cells from granzyme B-induced apoptosis and CD8 T-cell killing. J Virol. 2011;85:2325–2332. doi: 10.1128/JVI.01791-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Nguyen ML, Blaho JA. Apoptosis during herpes simplex virus infection. Adv Virus Res. 2007;69:67–97. doi: 10.1016/S0065-3527(06)69002-7. [DOI] [PubMed] [Google Scholar]
- 165.Thompson RL, Sawtell NM. HSV latency-associated transcript and neuronal apoptosis. Science. 2000;289:1651. [PubMed] [Google Scholar]
- 166.Perng GC, Jones C, Ciacci-Zanella J, Stone M, Henderson G, Yukht A, Slanina SM, Hofman FM, Ghiasi H, Nesburn AB, Wechsler SL. Virus-induced neuronal apoptosis blocked by the herpes simplex virus latency-associated transcript. Science. 2000;287:1500–1503. doi: 10.1126/science.287.5457.1500. [DOI] [PubMed] [Google Scholar]
- 167.Aravalli RN, Hu S, Rowen TN, Gekker G, Lokensgard JR. Differential apoptotic signaling in primary glial cells infected with herpes simplex virus 1. J Neurovirol. 2006;12:501–510. doi: 10.1080/13550280601064921. [DOI] [PubMed] [Google Scholar]
- 168.Yang CT, Song J, Bu X, Cong YS, Bacchetti S, Rennie P, Jia WW. Herpes simplex virus type-1 infection upregulates cellular promoters and telomerase activity in both tumor and nontumor human cells. Gene Ther. 2003;10:1494–1502. doi: 10.1038/sj.gt.3302005. [DOI] [PubMed] [Google Scholar]
- 169.Hughes BA, Kimmel DW, Aksamit AJ. Herpes zoster-associated meningoencephalitis in patients with systemic cancer. Mayo Clin Proc. 1993;68:652–655. doi: 10.1016/s0025-6196(12)60600-4. [DOI] [PubMed] [Google Scholar]
- 170.Maiche AG, Kajanti MJ, Pyrhonen S. Simultaneous disseminated herpes zoster and bacterial infection in cancer patients. Acta Oncol. 1992;31:681–683. doi: 10.3109/02841869209083855. [DOI] [PubMed] [Google Scholar]
- 171.Affronti M, Malta R, Di Rosa S, Maggio AM, Vassallo L, Occhino C, Scardavi M, Renda M, Scarpinati P. Thoracic herpes zoster treated with intravenous Acyclovir in three cancer patients. J Chemother. 1989;1:1304. [PubMed] [Google Scholar]
- 172.Winston DJ, Eron LJ, Ho M, Pazin G, Kessler H, Pottage JC, Jr, Gallagher J, Sartiano G, Ho WG, Champlin RE, et al. Recombinant interferon alpha-2a for treatment of herpes zoster in immunosuppressed patients with cancer. Am J Med. 1988;85:147–151. doi: 10.1016/s0002-9343(88)80333-4. [DOI] [PubMed] [Google Scholar]
- 173.Riegelman R. Cancer and herpes zoster. N Engl J Med. 1982;307:1706–1707. [PubMed] [Google Scholar]
- 174.Feldman S, Novak R, Malone W. Case report—Herpes zoster affecting three noncontiguous dermatomes in a child with cancer. J Tenn Med Assoc. 1979;72:664–666. [PubMed] [Google Scholar]
- 175.Feldman S, Hughes WT, Kim HY. Herpes zoster in children with cancer. Am J Dis Child. 1973;126:178–184. doi: 10.1001/archpedi.1973.02110190156009. [DOI] [PubMed] [Google Scholar]
- 176.Yoo KH, Park JH, Kim BJ, Kim MN, Song KY. Herpes zoster duplex bilateralis in a patient with breast cancer. Cancer Res Treat. 2009;41:50–52. doi: 10.4143/crt.2009.41.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Parikh PM, Davison SP. Herpes zoster after reconstruction for head and neck cancer. Plast Reconstr Surg. 2008;122:211e–213e. doi: 10.1097/PRS.0b013e31818dc04d. [DOI] [PubMed] [Google Scholar]
- 178.Djuric M, Jankovic L, Jovanovic T, Pavlica D, Brkic S, Knezevic A, Markovic D, Milasin J. Prevalence of oral herpes simplex virus reactivation in cancer patients: a comparison of different techniques of viral detection. J Oral Pathol Med. 2009;38:167–173. doi: 10.1111/j.1600-0714.2008.00684.x. [DOI] [PubMed] [Google Scholar]
- 179.Aisenberg GM, Torres HA, Tarrand J, Safdar A, Bodey G, Chemaly RF. Herpes simplex virus lower respiratory tract infection in patients with solid tumors. Cancer. 2009;115:199–206. doi: 10.1002/cncr.24011. [DOI] [PubMed] [Google Scholar]
- 180.Gundling F, Rohrbach H, Nerlich A, Schepp W. Herpes simplex virus esophagitis in an immunodeficient patient with non-small-cell lung cancer following a disseminated herpes zoster infection. Endoscopy. 2008;40(Suppl 2):157–158. doi: 10.1055/s-2007-995380. [DOI] [PubMed] [Google Scholar]
- 181.Grimm B, Padberg B, Ruhstaller T, Fleisch F, von Moos R. Fatal herpes simplex virus hepatitis in a patient with esophageal cancer under radiochemotherapy. Onkologie. 2008;31:620–622. doi: 10.1159/000162283. [DOI] [PubMed] [Google Scholar]
- 182.Ramphal R, Grant RM, Dzolganovski B, Constantin J, Tellier R, Allen U, Weitzman S, Matlow A, Petric M, Sung L. Herpes simplex virus in febrile neutropenic children undergoing chemotherapy for cancer: a prospective cohort study. Pediatr Infect Dis J. 2007;26:700–704. doi: 10.1097/INF.0b013e31805cdc11. [DOI] [PubMed] [Google Scholar]
- 183.Montgomery MT, Redding SW, LeMaistre CF. The incidence of oral herpes simplex virus infection in patients undergoing cancer chemotherapy. Oral Surg Oral Med Oral Pathol. 1986;61:238–242. [Google Scholar]
- 184.Berg JW. Esophageal herpes: a complication of cancer therapy. Cancer. 1955;8:731–740. doi: 10.1002/1097-0142(1955)8:4<731::aid-cncr2820080416>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 185.Spacca B, Mallucci C, Riordan A, Appleton R, Thorp N, Pizer B. HSV encephalitis in a child with brain stem glioma: a rare complication of therapy. Case report and review of the neurosurgical literature. Childs Nerv Syst. 2007;23:1347–1350. doi: 10.1007/s00381-007-0389-3. [DOI] [PubMed] [Google Scholar]
- 186.Bataller L, Dalmau J. Herpes simplex encephalitis in a patient with cancer. J Neurooncol. 2006;78:211. doi: 10.1007/s11060-005-9089-6. [DOI] [PubMed] [Google Scholar]
- 187.Krieger D, Wendtland B, Bruckmann H. Herpes simplex encephalitis following irradiation of a brain stem glioma. Nervenarzt. 1988;59:50–54. [PubMed] [Google Scholar]
- 188.Coppey J, Menezes S. Enhanced reactivation of ultraviolet-damaged herpes virus in ultraviolet pretreated skin fibroblasts of cancer prone donors. Carcinogenesis. 1981;2:787–793. doi: 10.1093/carcin/2.8.787. [DOI] [PubMed] [Google Scholar]
- 189.Lytle CD, Benane SG, Bockstahler LE. Ultraviolet-enhanced reactivation of Herpes virus in human tumor cells. Photochem Photobiol. 1974;20:91–94. doi: 10.1111/j.1751-1097.1974.tb06554.x. [DOI] [PubMed] [Google Scholar]
- 190.Minami M, Kita M, Yan XQ, Yamamoto T, Iida T, Sekikawa K, Iwakura Y, Imanishi J. Role of IFN-gamma and tumor necrosis factor-alpha in herpes simplex virus type 1 infection. J Interferon Cytokine Res. 2002;22:671–676. doi: 10.1089/10799900260100150. [DOI] [PubMed] [Google Scholar]
- 191.Mezhir JJ, Advani SJ, Smith KD, Darga TE, Poon AP, Schmidt H, Posner MC, Roizman B, Weichselbaum RR. Ionizing radiation activates late herpes simplex virus 1 promoters via the p38 pathway in tumors treated with oncolytic viruses. Cancer Res. 2005;65:9479–9484. doi: 10.1158/0008-5472.CAN-05-1927. [DOI] [PubMed] [Google Scholar]
- 192.Advani SJ, Sibley GS, Song PY, Hallahan DE, Kataoka Y, Roizman B, Weichselbaum RR. Enhancement of replication of genetically engineered herpes simplex viruses by ionizing radiation: a new paradigm for destruction of therapeutically intractable tumors. Gene Ther. 1998;5:160–165. doi: 10.1038/sj.gt.3300546. [DOI] [PubMed] [Google Scholar]
- 193.Hadjipanayis CG, DeLuca NA. Inhibition of DNA repair by a herpes simplex virus vector enhances the radiosensitivity of human glioblastoma cells. Cancer Res. 2005;65:5310–5316. doi: 10.1158/0008-5472.CAN-04-3793. [DOI] [PubMed] [Google Scholar]
- 194.Sakihama K, Eizuru Y, Minamishima Y. Differential susceptibility of a rat glioma cell line and its clones to herpes simplex virus types 1 and 2. Acta Virol. 1991;35:127–134. [PubMed] [Google Scholar]
- 195.Smith CA, Lancz GJ. Abortive infection of neural cells by herpes simplex virus type 2. Arch Virol. 1982;74:311–323. doi: 10.1007/BF01314164. [DOI] [PubMed] [Google Scholar]
- 196.Ando T, Arai H. Stimulation of herpes simplex type I infection of C6 cells by trypsin-EDTA. J Gen Virol. 1980;48:319–328. doi: 10.1099/0022-1317-48-2-319. [DOI] [PubMed] [Google Scholar]
- 197.Adler R, Glorioso JC, Levine M. Infection by herpes simplex virus and cells of nervous system origin: characterization of a non-permissive interaction. J Gen Virol. 1978;39:9–20. doi: 10.1099/0022-1317-39-1-9. [DOI] [PubMed] [Google Scholar]
- 198.Stowe RP, Mehta SK, Ferrando AA, Feeback DL, Pierson DL. Immune responses and latent herpesvirus reactivation in spaceflight. Aviat Space Environ Med. 2001;72:884–891. [PubMed] [Google Scholar]
- 199.Mehta SK, Stowe RP, Feiveson AH, Tyring SK, Pierson DL. Reactivation and shedding of cytomegalovirus in astronauts during spaceflight. J Infect Dis. 2000;182:1761–1764. doi: 10.1086/317624. [DOI] [PubMed] [Google Scholar]
- 200.Preston CM, Harman AN, Nicholl MJ. Activation of interferon response factor-3 in human cells infected with herpes simplex virus type 1 or human cytomegalovirus. J Virol. 2001;75:8909–8916. doi: 10.1128/JVI.75.19.8909-8916.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Heise MT, Virgin HWt. The T-cell-independent role of gamma interferon and tumor necrosis factor alpha in macrophage activation during murine cytomegalovirus and herpes simplex virus infections. J Virol. 1995;69:904–909. doi: 10.1128/jvi.69.2.904-909.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Murphy JC, Fischle W, Verdin E, Sinclair JH. Control of cytomegalovirus lytic gene expression by histone acetylation. EMBO J. 2002;21:1112–1120. doi: 10.1093/emboj/21.5.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Pinnoji RC, Bedadala GR, George B, Holland TC, Hill JM, Hsia SC. Repressor element-1 silencing transcription factor/neuronal restrictive silencer factor (REST/NRSF) can regulate HSV-1 immediate-early transcription via histone modification. Virol J. 2007;4:56. doi: 10.1186/1743-422X-4-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Nguyen ML, Kraft RM, Blaho JA. Susceptibility of cancer cells to herpes simplex virus-dependent apoptosis. J Gen Virol. 2007;88:1866–1875. doi: 10.1099/vir.0.82868-0. [DOI] [PubMed] [Google Scholar]
- 205.Fleck M, Mountz JD, Hsu HC, Wu J, Edwards CK, 3rd, Kern ER. Herpes simplex virus type 2 infection induced apoptosis in peritoneal macrophages independent of Fas and tumor necrosis factor-receptor signaling. Viral Immunol. 1999;12:263–275. doi: 10.1089/vim.1999.12.263. [DOI] [PubMed] [Google Scholar]
- 206.Watanabe D, Honda T, Nishio K, Tomita Y, Sugiura Y, Nishiyama Y. Corneal infection of herpes simplex virus type 2–induced neuronal apoptosis in the brain stem of mice with expression of tumor suppressor gene (p53) and transcription factors. Acta Neuropathol. 2000;100:647–653. doi: 10.1007/s004010000240. [DOI] [PubMed] [Google Scholar]
- 207.Kulomaa P, Paavonen J, Lehtinen M. Herpes simplex virus induces unscheduled DNA synthesis in virus-infected cervical cancer cell lines. Res Virol. 1992;143:351–359. doi: 10.1016/s0923-2516(06)80123-8. [DOI] [PubMed] [Google Scholar]
- 208.Song GY, DeJong G, Jia W. Cell surface expression of MHC molecules in glioma cells infected with herpes simplex virus type-1. J Neuroimmunol. 1999;93:1–7. doi: 10.1016/s0165-5728(98)00167-2. [DOI] [PubMed] [Google Scholar]
- 209.Das MR, Gridley DS, Kettering JD. Suppression of immune responses by herpes virus type 2-transformed murine tumor cells. Immunol Lett. 1991;30:37–45. doi: 10.1016/0165-2478(91)90087-q. [DOI] [PubMed] [Google Scholar]
- 210.Lakshmi N, Kumar AG, Anand T, Reddy BK. Sero-prevalence of herpes simplex virus type-2 among cancer cervix patients. Indian J Cancer. 1993;30:189–191. [PubMed] [Google Scholar]
- 211.Larsson PA, Edstrom S, Westin T, Nordkvist A, Hirsch JM, Vahlne A. Reactivity against herpes simplex virus in patients with head and neck cancer. Int J Cancer. 1991;49:14–18. doi: 10.1002/ijc.2910490104. [DOI] [PubMed] [Google Scholar]
- 212.Davis JM, La Thangue NB, Taylor DL, Latchman DS, Anderson M, Tyms AS. Cellular polypeptides overexpressed after herpes simplex infection permit virus subtyping and may help diagnose cervical cancer. Genitourin Med. 1988;64:321–326. doi: 10.1136/sti.64.5.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.te Velde ER, Aurelian L. Antibodies to the herpes simplex virus type-2-induced tumor-associated antigen AG-4 as markers of recurrence in cervical cancer. Tumour Biol. 1987;8:26–33. doi: 10.1159/000217488. [DOI] [PubMed] [Google Scholar]
- 214.Stoian M, Suru M, Zaharia O, Hozoc M, Nastac E, Fleshler BA. Possible relation between viruses and oromaxillofacial tumors. I. Demonstration of herpes antigens and anti-herpes antibodies. Virologie. 1987;38:25–34. [PubMed] [Google Scholar]
- 215.Teglbjaerg CS, Feldborg R, Norrild B. Immunological reactivity of human sera with individual herpes simplex proteins: a comparative study of sera from patients with preinvasive or invasive cervical cancer and from controls. J Med Virol. 1986;18:169–180. doi: 10.1002/jmv.1890180209. [DOI] [PubMed] [Google Scholar]
- 216.Shillitoe EJ, Greenspan D, Greenspan JS, Silverman S., Jr Five-year survival of patients with oral cancer and its association with antibody to herpes simplex virus. Cancer. 1986;58:2256–2259. doi: 10.1002/1097-0142(19861115)58:10<2256::aid-cncr2820581016>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 217.Shillitoe EJ. Measured levels of antibody to the herpes simplex virus in patients with oral cancer and controls. J Dent Res. 1985;64:944. doi: 10.1177/00220345850640062001. [DOI] [PubMed] [Google Scholar]
- 218.Vass-Sorensen M, Abeler V, Berle E, Pedersen B, Davy M, Thorsby E, Norrild B. Prevalence of antibodies to herpes simplex virus and frequency of HLA antigens in patients with preinvasive and invasive cervical cancer. Gynecol Oncol. 1984;18:349–358. doi: 10.1016/0090-8258(84)90047-7. [DOI] [PubMed] [Google Scholar]
- 219.Shillitoe EJ, Greenspan D, Greenspan JS, Silverman S., Jr Antibody to early and late antigens of herpes simplex virus type 1 in patients with oral cancer. Cancer. 1984;54:266–273. doi: 10.1002/1097-0142(19840715)54:2<266::aid-cncr2820540214>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 220.Kumari TV, Harikumar T, Prabha B, Sasidharan VK, Vasudevan DM. Detection of antibodies against herpes simplex virus in patients with oral cancer. Indian J Cancer. 1984;21:137–140. [PubMed] [Google Scholar]
- 221.Chiphangwi JD. Antibodies to membrane antigens of herpes simplex virus type-2 infected cells and HSV-2 specific antibodies in patients with cervical cancer in Malawi. IARC Sci Publ. 1984;63:465–470. [PubMed] [Google Scholar]
- 222.Wentz WB, Heggie AD, Anthony DD, Reagan JW. Effect of prior immunization on induction of cervical cancer in mice by herpes simplex virus type 2. Science. 1983;222:1128–1129. doi: 10.1126/science.6316503. [DOI] [PubMed] [Google Scholar]
- 223.Wrensch M, Weinberg A, Wiencke J, Miike R, Sison J, Wiemels J, Barger G, DeLorenze G, Aldape K, Kelsey K. History of chickenpox and shingles and prevalence of antibodies to varicella-zoster virus and three other herpesviruses among adults with glioma and controls. Am J Epidemiol. 2005;161:929–938. doi: 10.1093/aje/kwi119. [DOI] [PubMed] [Google Scholar]
- 224.Wrensch M, Weinberg A, Wiencke J, Miike R, Barger G, Kelsey K. Prevalence of antibodies to four herpesviruses among adults with glioma and controls. Am J Epidemiol. 2001;154:161–165. doi: 10.1093/aje/154.2.161. [DOI] [PubMed] [Google Scholar]
- 225.Shimura T, Sugisaki Y, Fukino K, Node Y, Teramoto A, Kawamoto M. Detection of Epstein-Barr virus DNA and expression of CD30 antigen in primary anaplastic diffuse large B-cell lymphoma of the brain. Brain Tumor Pathol. 2001;18:161–165. doi: 10.1007/BF02479431. [DOI] [PubMed] [Google Scholar]
- 226.Murphy JK. Epstein-Barr virus and primary brain lymphomas. Am J Clin Pathol. 1999;112:881–882. doi: 10.1093/ajcp/112.6.881. [DOI] [PubMed] [Google Scholar]
- 227.Lee J, Kotliarova S, Kotliarov Y, Li A, Su Q, Donin NM, Pastorino S, Purow BW, Christopher N, Zhang W, Park JK, Fine HA. Tumor stem cells derived from glioblastomas cultured in bFGF and EGF more closely mirror the phenotype and genotype of primary tumors than do serum-cultured cell lines. Cancer Cell. 2006;9:391–403. doi: 10.1016/j.ccr.2006.03.030. [DOI] [PubMed] [Google Scholar]
- 228.Gürsel DB, Beyene RT, Hofstetter C, Greenfield JP, Souweidane MM, Kaplitt M, Arango-Lievano M, Howard B, Boockvar JA. Optimization of glioblastoma multiforme stem cell isolation, transfection, and transduction. J Neuro Oncol. 2011 doi: 10.1007/s11060-011-0528-2. [DOI] [PubMed] [Google Scholar]
- 229.Ryan K. Sherris Medical Microbiology. 4. McGraw Hill; New York: 2004. [Google Scholar]