Abstract
Background: The food supply and dietary preferences have changed in recent decades.
Objective: We studied time- and age-related individual and population-wide changes in a dietary quality score and food groups during 1985–2006.
Design: The Coronary Artery Risk Development in Young Adults (CARDIA) study of 5115 black and white men and women [aged 18–30 y at year 0 (1985–1986)] assessed diet at examinations at study years 0, 7 (1992–1993), and 20 (2005–2006). The dietary quality score, which was validated by its inverse association with cardiovascular disease risk, summed 46 food groups rated by investigators as positive or negative on the basis of hypothesized health effects. We used repeated-measures regression to estimate time-specific mean diet scores and servings per day of food groups.
Results: In 2652 participants with all 3 diet assessments, the mean (±SD) dietary quality score increased from 64.1 ± 13.0 at year 0 to 71.1 ± 12.6 at year 20, which was mostly attributable to increased age. However, the secular trend, which was estimated from differences of dietary quality scores across time at a fixed age (age-matched time trend) decreased. The diet score was higher in whites than in blacks and in women than in men and increased with education, but demographic gaps in the score narrowed over 20 y. There tended to be increases in positively rated food groups and decreases in negatively rated food groups, which were generally similar in direction across demographic groups.
Conclusions: The CARDIA study showed many age-related, desirable changes in food intake over 20 y of observation, despite a secular trend toward a lower diet quality. Nevertheless, demographic disparities in diet persist.
INTRODUCTION
Food availability, supply, and environment changed considerably between 1985 and 2006. There have been a variety of international dietary recommendations for reducing risk of ischemic heart disease. Recently, recommendations have begun to emphasize particular food groups, which may be easier for the population to implement. The 1985 US Dietary Guidelines (1) encouraged increased intakes of fruit and vegetables; however, in the 2010 US Dietary Guidelines (2), food-group recommendations have been extended and advise a shift in food intake to a more plant-based diet that emphasizes fruit, vegetables, legumes, whole grains, nuts, and seeds. In addition, increased intakes of seafood and low-fat dairy products and consumption of only moderate amounts of lean meats, poultry, and eggs were likewise recommended (2). Recommendations are ultimately intended to guide the public to a healthful diet; compared with nutrient recommendations, food recommendations have been more stable and may be easier for the population to implement. However, more information is needed about whether earlier recommendations correspond to actual changes in dietary intakes in the general population and whether changes are different in sociodemographic groups.
Some data suggested that diet quality has improved over recent decades despite population-wide weight gain, but secular trends and age effects were not distinguished (3). Because people age from young adulthood to middle age, they tend to improve their diet (4–6). In contrast, one study reported an unfavorable secular diet quality trend and a lower proportion of the population who met the national recommended nutrient and food intakes in 2 cross-sectional studies in 2000 and 2005 (7). Some reports of trends in food-group and nutrient intakes have focused on differentials by sex (3, 8), race, or education (9). The Coronary Artery Risk Development in Young Adults (CARDIA) study reported that the Keys score, which is a measure of the tendency of diet to alter serum cholesterol, tended to decrease in young adult between 1985–1986 and 1992–1993, which was similar for black and white men and women and concordant with a secular trend toward lower serum cholesterol, despite increasing obesity (10). These studies documented demographic differences in diet that did not narrow over time (8–10). Furthermore, during the last few decades, major societal changes in the food environment have occurred. Fast-food availability and consumption has increased greatly (11), and restaurant portion sizes have increased (12). The production and availability of processed foods, including boxed or packaged and frozen foods, increased (13).
We used an a priori diet score that has been validated as a measure of dietary quality in that it is a predictor of myocardial infarction (14), diabetes (15), and variables that are apparently on the causal pathway for clinical cardiovascular disease (16, 17). The a priori diet-quality score is novel in that it is based on a priori reasoning and solely on foods consumed rather than on nutrients.
In light of the societal influences mentioned, we compared CARDIA diet data between 1985–1986 and 2005–2006. We hypothesized that a secular trend toward a worse overall a priori diet quality exists but that certain improvements in dietary quality, such as an increased intake of phytochemical-rich plant food and decreased intake of red meat, would be evident and consistent with recent dietary recommendations. In addition, we hypothesized that these improvements in dietary quality would be age related and more common among certain sociodemographic strata, such as higher education, white race, and female sex (ie, that demographic gaps would widen over 20 y).
SUBJECTS AND METHODS
Study sample
The CARDIA study is a multicenter, longitudinal investigation of the evolution of ischemic heart disease risk starting in young adulthood (18). The CARDIA study began in 1985–1986 with 5115 black and white adults aged 18–30 y from 4 metropolitan areas (Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA). Study participants were sampled to obtain roughly equal numbers of blacks (51.5%) and whites (48.5%), men (45.5%) and women (54.5%), ages 18–24 y (44.9%) and 25–30 y (55.1%), and with a high school education or less (39.7%) or more than a high school education (60.3%). Among 6 follow-up examinations were those in 1992–1993 (year 7) and 2005–2006 (year 20). A majority of the surviving cohort membership has been examined at each of the follow-up examinations (81% of subjects at year 7 and 72% of subjects at year 20); 87% of subjects have attended ≥2 examinations at years 0, 7, and 20, and 63% of subjects attended all 3 examinations.
Participants who attended a clinic but had no dietary data (n = 4, 143, and 406 at years 0, 7, and 20, respectively) or an implausibly high or low energy intake (<800 or >8000 kcal/d for men; <600 or >6000 kcal/d for women; n = 128, 94, and 54 at years 0, 7, and 20, respectively) were excluded from analysis. After exclusion, there were 4983, 3849, and 3089 participants with diet measured at years 0, 7, and 20, respectively, and 2652 participants who completed the diet assessment at all 3 examinations. Findings differed little between all available participants and the cohort of 2652 people with complete data. The CARDIA study was approved by the institutional review board of each field center; each study participant provided informed written consent.
Other baseline measurements
Standard questionnaires were used to obtain self-reported demographic and behavioral information. Sex, race, date of birth, education, and cigarette smoking were ascertained by a structured interview or self-administered questionnaire at each examination. Self-reported smoking status was classified as never, former, or current smoker. Height and weight were measured at each examination and recorded to the nearest 0.5 cm and 0.2 kg, respectively. BMI was defined as weight (in kg) divided by height squared (in m2). A physical activity score was derived from the CARDIA Physical Activity History, which is a simplified version of the Minnesota Leisure Time Physical Activity Questionnaire (19), at each examination. Educational status was quantified as years attained as reported at each examination (Table 1) or as the maximum (at any visit) reported number of years of schooling completed in stratification (Table 2).
TABLE 1.
Demographic, behavioral, and dietary characteristics of participants in the CARDIA study, 1985–1986 to 2005–20061
| Year 0 | Year 7 | Year 20 | P-trend | |
| Age (y) | 25.2 ± 3.52 | 32.2 ± 3.5 | 45.3 ± 3.6 | — |
| Women (%) | 57 | — | — | — |
| White (%) | 57 | — | — | — |
| Center (%) | ||||
| Birmingham | 24 | — | — | — |
| Chicago | 25 | — | — | — |
| Minneapolis | 25 | — | — | — |
| Oakland | 25 | — | — | — |
| Education attained (y) | 14.2 ± 2.2 | 14.9 ± 2.5 | 15.2 ± 2.6 | <0.0001 |
| BMI (kg/m2) | 24.4 ± 4.8 | 26.5 ± 5.8 | 29.4 ± 7.2 | <0.0001 |
| Waist circumference (cm ) | 77.4 ± 11.2 | 83.4 ± 13.7 | 91.7 ± 15.3 | <0.0001 |
| Physical activity (exercise units) | 419.8 ± 291.6 | 336.9 ± 267.3 | 336.2 ± 265.5 | <0.0001 |
| Current smoker (%) | 24.3 | 22.7 | 17.3 | <0.0001 |
| Dietary variables | ||||
| Mean total energy (kcal/d) | 2681.4 ± 1222.0 | 2694.4 ± 1157.0 | 2296.1± 999.4 | <0.0001 |
| Total carbohydrates (percentage of energy) | 45.9 ± 7.2 | 49.7 ± 8.1 | 47.0 ± 9.6 | 0.04 |
| Total protein (percentage of energy) | 14.9 ± 2.6 | 14.8 ± 2.7 | 15.6 ± 3.6 | <0.0001 |
| Total fat (percentage of energy) | 37.6 ± 5.9 | 34.9 ± 6.8 | 36.4 ± 8.4 | <0.0001 |
| Saturated fat | 14.1 ± 2.9 | 12.1 ± 3 | 11.5 ± 3.1 | <0.0001 |
| Monounsaturated fat | 13.9 ± 2.5 | 12.9 ± 2.9 | 13.9 ± 4 | 0.003 |
| Polyunsaturated fat | 6.9 ± 2 | 7.1 ± 2.2 | 8.1 ± 3.6 | <0.0001 |
| Fast food (visits/wk) | 1.9 ± 2.2 | 1.9 ± 2.4 | 1.6 ± 2.2 | <0.0001 |
| Eats breakfast (times/wk) | Not asked | 4.2 ± 2.6 | 4.8 ± 2.4 | <0.0001 |
n = 2652 participants with dietary assessment at CARDIA years 0, 7, and 20. P-trend values were based on repeated-measures regression models with time modeled as a continuous variable. CARDIA, Coronary Artery Risk Development in Young Adults.
Mean ± SD (all such values).
TABLE 2.
Changes in the a priori diet score during the CARDIA study, 1985–1986 to 2005–2006 (n = 2652)1
| n | Year 0 | Year 7 | Year 20 | P-trend | Adjusted change2 | |
| A priori diet score | 2652 | 64.1 ± 13.03 | 67.5 ± 12.1 | 71.1 ± 12.6 | <0.0001 | 6.8 (6.4–7.3) |
| Sex, race | ||||||
| Female, white | 797 | 71.6 ± 12.6 | 73.7 ± 10.9 | 77.6 ± 11.7 | <0.0001 | 5.9 (5.2–6.7) |
| Male, white | 717 | 66.6 ± 11.8 | 69.4 ± 11.2 | 72.6 ± 11.8 | <0.0001 | 5.8 (4.9–6.6) |
| Female, black | 713 | 57.9 ± 10.4 | 62.7 ± 10.7 | 66.7 ± 11.1 | <0.0001 | 8.6 (7.8–9.5) |
| Male, black | 425 | 56.2 ± 10.2 | 60.4 ± 10.8 | 63.8 ± 11.3 | <0.0001 | 7.3 (6.2–8.4) |
| Education4 | ||||||
| High school | 369 | 57.3 ± 11.0 | 60.6 ± 11.8 | 64.4 ± 12.3 | <0.0001 | 6.9 (5.7–8.0) |
| Some college | 787 | 59.9 ± 11.7 | 64.1 ± 11.3 | 67.6 ± 11.4 | <0.0001 | 7.5 (6.7–8.3) |
| College | 662 | 66.1 ± 13.0 | 69.4 ± 11.3 | 72.9 ± 12.5 | <0.0001 | 6.7 (5.8–7.6) |
| Postcollege | 834 | 69.4 ± 12.4 | 72.2 ± 11.2 | 76.0 ± 11.5 | <0.0001 | 6.5 (5.7–7.2) |
P-trend values and adjusted mean changes were based on repeated-measures regression models adjusted for sex, race, center, age, and total energy (kcal/d). CARDIA, Coronary Artery Risk Development in Young Adults.
Values are means; 95% CI in parentheses.
Mean ± SD (all such values).
Maximum attained during follow-up.
Dietary assessment and food-group creation
Diet was assessed at years 0, 7, and 20 by using an interviewer-administered CARDIA Diet History (20). Interviewers asked open-ended questions about dietary consumption in the past month within 100 food categories that referenced 1609 separate food items during years 0 and 7 and many more at year 20. The diet assessment methods were maintained across examinations; despite the increase in the number of food items reported, which was a reflection of the changing food supply. In addition, fast-food restaurant use (visits/wk) was queried at each examination and eating breakfast (d/wk) was queried at years 7 and 20.
Foods were assigned in one of 166 food groups by using the food-grouping system devised by the University of Minnesota Nutrition Coordinating Center. Food-group intake was assessed as servings per day of constituent foods. We excluded 6 infant-product food groups (not relevant), unsweetened water (collected at year 20 only), and nongrain flour (rarely consumed). In addition, we collapsed these 158 food groups into 46 food groups, which, in turn, were based on considerations of similar nutrient characteristics, hypothesized biologic effects, and comparability to food groups defined in previous studies (9).
Description of the a priori dietary pattern score
We created a dietary pattern score from the 46 foods groups as done in previous studies (14–17). The a priori score was created by classifying foods groups according to investigator ratings that matched those established in the initial use of the a priori score (14) as beneficial (n = 20), adverse (n = 13), or neutral (n = 13) in terms of hypothesized health effects. See Table 1 under “Supplemental data” in the online issue for details about the investigator ratings of food groups and the CARDIA a priori assignment. Food groups considered beneficial or adverse with respect to health effects were categorized into quintiles of consumption, and study participants received a score of 0–4 for each of the 46 food groups, depending on their amount of consumption. In food groups with large subsets of nonconsumers, nonconsumers were coded 0 and consumers were split into quartiles with scores from 1 to 4 to ensure variability across 5 levels of consumption. The a priori dietary pattern score was the sum of category scores 0–4 for the positively rated food groups plus scores in reverse order (4–0) for negatively rated food groups. Food groups that were considered neutral did not contribute to the overall a priori dietary pattern score. The theoretical maximum score was 132. It was assumed that a higher a priori dietary pattern score indicated better diet quality. A one-unit change in the score was a change of one category (usually one quintile) of one food group in the presumed positive direction. To assess the change in the overall dietary pattern, we scaled the score according to baseline parameters. Specifically, we used the cutoffs of food group categories as determined at year 0, which were then applied to dietary data of years 0, 7, and 20.
A baseline reliability study of nutrient consumption from the diet history showed that sex- and energy-adjusted 1-mo test-retest correlations were lower for blacks (0.27–0.58) than for whites (0.54–0.82). Correlations between mean nutrient intakes from the diet history and 7 random 24-h dietary recalls ranged from 0.50 to 0.86 for white men to 0.20–0.53 for black women, with the exception of carbohydrates in black women, r = 0.04 (21). Despite the suggestion that the diet history was less reliable in blacks than in whites, the correlations for the a priori diet score tracking over time were high in both races. In blacks, the correlation between years 0 and 7 was 0.51, between years 7 and 20 was 0.52, and between years 0 and 20 was 0.43. These correlations were slightly lower than the corresponding correlations in whites (ie, 0.62, 0.61, and 0.57, respectively). The diet score tracked over time more highly than did the direct questions about fast food (0.30, 0.27, 0.18, respectively) and breakfast eating (0.46 between years 7 and 20); in each case, the tracking was somewhat higher in whites than in blacks.
Statistical analysis
We based most analyses on the cohort of 2652 people with complete data. We used the personal computer version (9.2) of the Statistical Analysis System (SAS Institute Inc) for all analyses. A longitudinal analysis was conducted by using the 3 repeated measures of the dietary pattern score modeled as the outcome variable in a mixed model (SAS PROC MIXED, n = 2652; SAS Institute Inc). We examined several regression models with different levels of adjustment. The model included participant sex (male or female sex), study center (Birmingham, Chicago, Minneapolis, or Oakland), race (white or black), total energy intake (kcal/d), age at year 0 (continuous), and time (continuous or discrete, depending on the model). Sensitivity models also included BMI (continuous). SAS PROC MIXED (SAS Institute Inc) with time modeled as a continuous variable was used to obtain the P-trend. Interactions with race, sex, and maximum achieved education were analyzed by using product terms (eg, time × race). To separate secular trends from age effects, we plotted unadjusted means and 95% CIs and included all available participants (n = 4983). A mixed model was also used to estimate the a priori diet score at ages 20 and 50 y by following the linear equation that linked the a priori diet score to age within each examination (12). In this model, the dependent variable was the repeated a priori diet score, and independent variables were the current age (continuous) and year of examination (0, 7, or 20). The model was repeated with adjustment for race, sex, and time-dependent energy intakes. Statistical significance was considered to be met at P < 0.05.
To study changes in food groups over time, we computed mean servings per day for each food group and time point. We assessed the P-trend in a mixed model by using time as a continuous variable. We examined demographic interactions by noting the race × sex or education (high school degree or less compared with any college) interaction with P < 0.0011 (Bonferroni adjusted for 46 food-group comparisons). For race and sex, we hierarchically deleted nonsignificant interaction terms (ie, we first examined a model with race × time, sex × time, and race × sex × time terms). If the race × sex × time term had a P value ≥0.0011, we deleted it and examined lower-order interactions.
RESULTS
Sample characteristics
Characteristics of the study participants for each survey are shown in Table 1. Years of education attained increased significantly over 20 y, as did BMI and waist circumference. Physical activity decreased between years 0 and 7, whereas current smoking decreased over 20 y. Total energy intake decreased between years 7 and 20. Carbohydrate intake increased between years 0 and 7 but decreased between years 7 and 20. Protein intake increased between years 7 and 20. Total fat intake decreased between years 0 and 7 but rebounded by year 20, whereas changes in saturated and polyunsaturated fats were monotonically decreasing and increasing, respectively. Participants reported visiting fast-food restaurants, on average, almost twice per week, which decreased to 1.6 times/wk at year 20. Participants reported eating breakfast 4.2 times/wk at year 7, which increased to 4.8 times/wk at year 20.
Trends in the diet-quality score
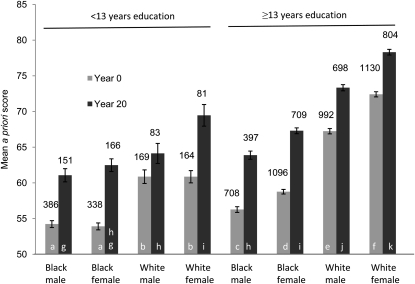
The unadjusted mean (±SD) a priori dietary pattern score in the 2652 participants whose diet was assessed on all occasions was 64.1 ± 13.0, 67.5 ± 12.1, and 71.1 ± 12.6 at years 0, 7, and 20, respectively (Table 2). Participants who did not attend all examinations or who otherwise had missing dietary data at any time point showed significantly lower scores [corresponding values: 61.0 ± 12.8 (n = 2331), 65.4 ± 12.4 (n = 1197), and 66.8 ± 13.2 (n = 437); P < 0.0001]. The dietary pattern score varied by demographic group and was higher in whites than in blacks and in women than in men. The score was also higher with greater educational attainment. In contrast, changes over time were most positive in groups that initially had lower scores. There was a larger increase in the dietary pattern score in blacks (8 units) than in whites (6 units) (P < 0.0001), and the increase in the score was less with increased educational attainment. Adjustment for sex, race, center, education, age, and total energy intake had little effect on the unadjusted means. Further adjustment for BMI did not change the outcomes. The variability in score over race, sex, education, and time was substantial. For example, the unadjusted score in participants whose diet was assessed on all occasions was 54.6 ± 9.8 in year 0 in 109 black men who had no education past high school, which increased at year 20 to 61.0 ± 11.3 (P < 0.0001) compared with 72.5 ± 12.3 in year 0 in 726 white women who had more than a college education, which increased at year 20 to 78.3 ± 11.3 (P < 0.0001) (Figure 1).
FIGURE 1.
Unadjusted mean (95% CI) a priori diet score according to race, sex, and educational groups; all available diet records: n = 4983 at year 0 (1985–1986) and 3089 at year 20 (2005–2006). Bars with different letters differed significantly from one another (P < 0.05) in pairwise comparisons. The race, sex, and education comparison was done separately for years 0 and 20.
Aging compared with secular trends
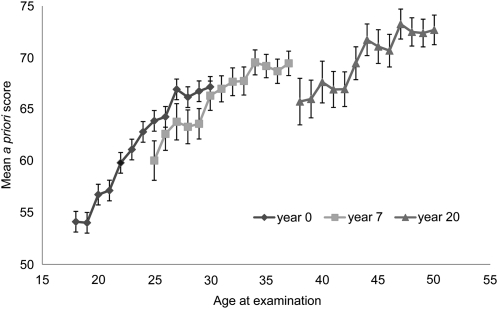
As shown in Figure 2, a large part of the change in the a priori diet score was attributable to the increasing age of the sample. On the basis of repeated-measures regression analysis with adjustment for race, sex, maximum achieved education, and time-dependent energy intake, the increase in the score with age was greatest in the earliest examination (when the participants were youngest) at 0.87 ± 0.043 units/y of age observed at year 0, 0.47 ± 0.047 units/y of age observed at year 7, and 0.38 ± 0.051 units/y of age observed at year 20 (P < 0.0001 for the time × age interaction).
FIGURE 2.
Mean (95% CI) a priori diet score according to current age and year of examination. Adjusted for sex, race, center, age, and total energy (kcal/d); all available diet records: n = 4962 at year 0 (1985–1986), 3803 at year 7 (1992–1993), and 3057 at year 20 (2005–2006).
The secular trend (the average vertical distance between examination-specific curves shown in Figure 2; the so-called age-matched time trend) was negative throughout the study. Between years 0 and 7, people aged 25–30 y in 1992–1993 had a slightly lower mean diet score than did people aged 25–30 y in 1985–1986. Although there were no overlapping ages observed at both years 7 and 20, extrapolation of the curves in Figure 2, with adjustment for race, sex, maximum achieved education, and time-dependent energy intake, suggested a mean a priori diet score of 78.7 at age 50 y if the age pattern at year 0 had been followed, of 68.8 if the age pattern at year 7 had been followed, and of 65.8 if the age pattern at year 20 had been followed. Although a linear age pattern appears to fit the data in Figure 2 well, we did not have sufficient age range in any examination to completely exclude curvature in the association of the diet-pattern score with age.
Changes in food groups
Change in selected food groups over 20 y that corresponded to changes in dietary pattern scores is shown in Table 3. Changes were more prominent and generally more consistent in negatively rated food groups than in neutrally or positively rated food groups, which were generally in a direction consistent with the philosophy of the a priori diet score. Of the 46 food groups studied, 43 food groups showed a significant trend over 20 y; however, these trends did not always display a monotonic trend over 20 y. Decreases of ≥0.5 servings/d occurred in intakes of butter, regular red meat, whole-fat dairy and soft drinks in the negatively rated food groups. Increases of ≥0.35 servings/d were seen in intakes of seeds and nuts, green vegetables, soy products, and oil in the positively rated food groups. Several substantial changes occurred in neutrally rated food groups as follows: intakes of refined grains decreased by 1.0 serving/d, whereas intakes of sugar substitutes and diet soft drinks increased by ≥0.26 servings/d. (See Table 2 under “Supplemental data” in the online issue for a complete analysis of changes in all 46 food groups that composed the dietary score.)
TABLE 3.
Changes in food groups grouped according to their rating in the a priori diet score in the CARDIA study, 1985–1986 to 2005–2006 (n = 2652)1
| Food group | Year 0 | Year 7 | Year 20 | Change in servings/d from years 20 to 02 | Percentage change3 | P-trend |
| Servings/d | Servings/d | Servings/d | ||||
| Positively rated | ||||||
| Oil | 1.46 ± 0.024 | 3.25 ± 0.05 | 2.75 ± 0.12 | 1.29 | 88 | <0.0001 |
| Soy products | 0.23 ± 0.01 | 0.63 ± 0.03 | 0.79 ± 0.04 | 0.56 | 243 | <0.0001 |
| Green vegetables | 0.37 ± 0.01 | 0.54 ± 0.01 | 0.79 ± 0.02 | 0.42 | 114 | <0.0001 |
| Seeds, nuts | 0.80 ± 0.03 | 0.76 ± 0.04 | 1.15 ± 0.04 | 0.35 | 44 | <0.0001 |
| Fruit | 1.43 ± 0.02 | 1.66 ± 0.03 | 1.67 ± 0.03 | 0.24 | 17 | <0.0001 |
| Poultry | 1.24 ± 0.02 | 1.47 ± 0.02 | 1.45 ± 0.03 | 0.21 | 17 | <0.0001 |
| Low-fat dairy | 1.16 ± 0.02 | 1.37 ± 0.03 | 1.30 ± 0.03 | 0.14 | 12 | <0.0001 |
| Whole grains | 1.52 ± 0.02 | 1.89 ± 0.03 | 1.61 ± 0.03 | 0.09 | 6 | <0.0001 |
| Negatively rated | ||||||
| Salty snacks | 0.04 ± 0.00 | 0.20 ± 0.01 | 0.24 ± 0.01 | 0.20 | 500 | <0.0001 |
| Processed meats | 0.90 ± 0.02 | 0.81 ± 0.02 | 0.92 ± 0.02 | 0.02 | 2 | <0.0001 |
| Fried potatoes | 0.36 ± 0.01 | 0.29 ± 0.01 | 0.18 ± 0.01 | −0.18 | −50 | <0.0001 |
| Sweet breads | 1.00 ± 0.02 | 0.90 ± 0.02 | 0.77 ± 0.02 | −0.23 | −23 | 0.3676 |
| Soft drinks | 1.60 ± 0.03 | 1.41 ± 0.03 | 0.95 ± 0.04 | −0.65 | −41 | <0.0001 |
| High-fat dairy | 2.07 ± 0.03 | 1.46 ± 0.03 | 1.18 ± 0.03 | −0.89 | −43 | <0.0001 |
| Regular red meat | 2.37 ± 0.04 | 2.03 ± 0.03 | 1.40 ± 0.03 | −0.97 | −41 | <0.0001 |
| Butter | 4.78 ± 0.07 | 3.88 ± 0.07 | 2.11 ± 0.06 | −2.67 | −56 | <0.0001 |
| Neutrally rated | ||||||
| Sugar substitutes | 0.06 ± 0.01 | 0.13 ± 0.01 | 0.66 ± 0.05 | 0.60 | 1000 | <0.0001 |
| Diet soft drinks | 0.38 ± 0.02 | 0.72 ± 0.02 | 0.64 ± 0.03 | 0.26 | 68 | <0.0001 |
| Nonfried potatoes | 0.42 ± 0.01 | 0.54 ± 0.01 | 0.29 ± 0.01 | −0.13 | −31 | <0.0001 |
| Refined grains | 4.55 ± 0.05 | 5.30 ± 0.06 | 3.55 ± 0.05 | −1.00 | −22 | 0.0005 |
P-trend values were based on repeated-measures regression models adjusted for sex, race, center, age, and total energy (kcal/d). CARDIA, Coronary Artery Risk Development in Young Adults.
All values are means.
(Year 20 – year 0) ÷ year 0.
Mean ± SE (all such values).
Differences in food-group time trends over 20 y between demographic groups tended to be concordant in direction. However, a few food groups showed changes in opposite directions. Whole-grain food consumption increased in white women (+0.29 servings/d) and showed very little change in all other demographic groups. The consumption of soft drinks increased in men (+0.48 servings/d) but decreased in women (−0.08 servings/d). Processed-meat consumption increased in whites (+0.23 servings/d) and in higher-educated people (+0.12 servings/d) and decreased in blacks (−0.16 servings/d) and lower-educated people (−0.25 servings/d).There was a substantially larger decrease in butter consumption in blacks (−3.5 servings/d) than in whites (−1.7 servings/d) and in lower-educated people (−4.3 servings/d) than in people with high education (−2.2 servings/d). (See Tables 3–4 under “Supplemental data” in the online issue for a complete analysis of changes in all 46 food groups that composed the dietary score by race and sex and education.)
The frequency of visits to fast-food restaurants was inversely related to the diet score (age-, race-, and sex-adjusted r = −0.22 at year 0, −0.30 at year 7, and −0.32 at year 20). Corresponding correlations of frequency of eating breakfast with diet score were r = 0.14 at year 7 and 0.18 at year 20.
DISCUSSION
Over 20 y of follow-up of a cohort of black and white Americans aged from young adulthood to middle age, we observed significant and positive changes in a measure of diet quality. In particular, consumption of plant foods, poultry, and low-fat dairy increased, whereas the consumption of many foods that could be considered health adverse, including fried potatoes, soft drinks, high fat dairy, and red meat, decreased. The consumption of sugar substitutes and diet soft drinks increased. Our data suggested that aging played a major role in diet-quality improvement over the course of follow-up because the diet-quality score increased across age within each examination. However, as hypothesized, the age-matched time trend suggested a secular trend of a decreased diet quality from 1985–1986 to 1992–1993 to 2005–2006 in the population from which the CARDIA sample was drawn. Specifically, on the basis of the slope over age of the diet-quality score in 1985–1986, we estimated that a 50-y-old would have a mean diet-quality score of 78.7, but the observation of 50-y olds in 2005–2006 estimated their diet-quality score to be 65.8. Thus, our data imply that individuals attained improvements in dietary quality despite aspects of the food supply and food choices that applied population wide and became less desirable as decades passed.
Improvements in the overall diet quality were apparent in all demographic groups. Although the diet score at year 0 was lower in men, blacks, and subjects with lower educational attainment, those groups tended to show greater increases in the diet score during follow-up. Thus, the substantial demographic gap in diet quality observed at baseline persisted at year 20, but the differences narrowed. Changes in specific food groups generally supported a change in the direction of improved diet quality.
Few studies have examined longitudinal trends in diet quality through adulthood. The 1946 British Birth Cohort of women aged 36 y, who were followed until age 53 y, showed a significantly increased consumption of a dietary pattern derived from principal component analysis (22), which was consistent with our findings of an increased diet-quality score over adulthood. The British Birth Cohort dietary pattern was characterized by a high consumption of fruit, vegetables, and dairy and a deceased consumption of a dietary pattern of meat, potatoes, and sweets. Men seemed to follow similar dietary principles. Because this study covered only a single year of age at each examination, it could not separate age from period effects. In the National Longitudinal Study of Adolescent Health cohort, between 1994 and 2002, as participants aged from between 12–19 to 18–26 y, fast-food consumption significantly declined, whereas breakfast consumption increased (23); no separation of age from period effects was presented. Two studies from Europe also showed that, as people aged from adolescence to adulthood, they changed their diet in the direction of dietary recommendations (3, 8). These studies documented changes over a variety of age ranges, although improvements after adolescence may weaken with increasing age. Our serial cross-sectional data (Figure 2) showed the largest improvement in diet quality per year of age during 1985–1986 (CARDIA year 0) when our participants were 18–30 y old. It is possible that this result indicated an important period of settling in to a stable dietary pattern. We observed a continuing improvement in diet quality in subsequent surveys through age 50 y, albeit at a slower rate than in younger adulthood. It is possible that this trend eventually reverses.
Strengths of our study included the thorough dietary assessment on repeated occasions in a large population-based cohort. The dietary assessment was comprehensive. Although reliability may be have been slightly lower in blacks than in whites, the a priori diet score showed a high level of tracking and expected correlation in both races with other dietary characteristics, including other diet pattern scores, visits to fast-food restaurants, and the frequency of breakfast eating. Although the a priori diet score had an element of subjectivity because it is based on the informed opinions of 4 nutrition scientists, excellent, although not complete, agreement about how to rate the food groups existed across investigators. Ratings were mostly, but not always, in line with official recommendations. The score has functioned well in validity testing. There were also limitations of our study. It is possible that CARDIA participants were particularly aware of their dietary intake because of general study participation and the interviewer-administered dietary history assessments, which resulted in improvements of their diet. However such an intervention seems unlikely because the investigators had little contact with the participants, and the dietary emphasis was largely during the 3 dietary assessments, which were 7 and 13 y apart. To examine population-wide secular trends, we used a method that examined the mean dietary score at a fixed age, which was achieved at different calendar times (age-matched time trend) (10). Consistent with our prior hypothesis and other evidence (6–8), there was a secular decline in diet quality, especially after 1992–1993. Nevertheless, our method should be interpreted with caution for 3 reasons. The method depended on specific ages overlapping between different periods (which did not occur between years 7 and 20), our cohort design represented the underlying population less and less well because there was attrition from our sample, and we could not fully account for the possible curvature in the diet score and age association. As in any observational study, residual confounding could not be ruled out.
During the past decades, dietary recommendations have tended to shift from nutrients to an overall dietary pattern, with emphasis on varied consumption and with specific attention to certain food groups (eg, consumption of red and processed meats, fruit and vegetables, and whole-grain foods). The a priori diet score is in line with many dietary guidelines. The improved diet quality with increased age likely resulted from the attention of CARDIA participants to dietary guidelines. At the same time, our suggestion that diet quality in the population at large worsened between 1985–1986 and 2005–2006 is worthy of note. In addition, different demographic sectors have diets of different quality. In a time of a high supply of nonnutrient-dense foods, the person who wishes to improve his or her diet quality may be working at cross-purposes with the general culture. Increasing the desirability of and access to fruit, vegetables, whole grains without added sugars, salt, solid fats, or extra calories, especially in demographic groups with lower a priori diet scores, could help improve these trends.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—FPCS: conceptualization, statistical analysis, interpretation, and writing of the manuscript text; KAM: conceptualization, interpretation, and writing and review of the manuscript; LMS: conceptualization, review of the manuscript, and director of the CARDIA Diet Center; JMS, LVH, and LH: review of the manuscript; DK: conceptualization, interpretation, and review of the manuscript; DRJ: securement of funding, collection of data, conceptualization, statistical analysis, interpretation, and writing and review of the manuscript text. None of the authors had a conflict of interest.
REFERENCES
- 1.Dietary Guidelines Advisory Committee. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 1985, to the Secretary of Agriculture and the Secretary of Health and Human Services. Washington, DC: US Department of Agriculture, Agricultural Research Service, 1985. Available from: http://www.cnpp.usda.gov/Publications/DietaryGuidelines/1985/1985CommitteeReport.pdf (cited 31 January 2011)
- 2.Dietary Guidelines Advisory Committee. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010, to the Secretary of Agriculture and the Secretary of Health and Human Services. Washington, DC: US Department of Agriculture, Agricultural Research Service, 2010. Available from: http://www.cnpp.usda.gov/DGAs2010-DGACReport.htm (cited 31 January 2011)
- 3.Bertheke Post G, de Vente W, Kemper HC, Twisk JW. Longitudinal trends in and tracking of energy and nutrient intake over 20 years in a Dutch cohort of men and women between 13 and 33 years of age: The Amsterdam Growth and Health Longitudinal Study. Br J Nutr 2001;85:375–85 [DOI] [PubMed] [Google Scholar]
- 4.Hu FB, Rimm EB, Stampfer MJ, Ascherio A, Spiegelman D, Willett WC. Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr 2000;72:912–21 [DOI] [PubMed] [Google Scholar]
- 5.Wang H, Steffen LM, Jacobs DR, Zhou X, Blackburn H, Berger AK, Filion KB, Luepker RV. Trends in cardiovascular risk factor levels in the Minnesota Heart Survey (1980-2002) as compared with the National Health and Nutrition Examination Survey (1976-2002): a partial explanation for Minnesota's low cardiovascular disease mortality? Am J Epidemiol 2011;173:526–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pelucchi C, Galeone C, Negri E, La Vecchia C. Trends in adherence to the Mediterranean diet in an Italian population between 1991 and 2006. Eur J Clin Nutr 2010;64:1052–6 [DOI] [PubMed] [Google Scholar]
- 7.Valdés J, Grau M, Subirana I, Marrugat J, Covas MI, Schröder H. Secular trends in energy intake and diet quality in a Mediterranean population. Ann Nutr Metab 2009;54:177–83 [DOI] [PubMed] [Google Scholar]
- 8.Lake AA, Mathers JC, Rugg-Gunn AJ, Adamson AJ. Longitudinal change in food habits between adolescence (11-12 years) and adulthood (32-33 years): The ASH30 study. J Public Health (Oxf) 2006;28:10–6 [DOI] [PubMed] [Google Scholar]
- 9.Kant AK, Graubard BI, Kumanyika SK. Trends in black-white differentials in dietary intakes of U.S. adults, 1971-2002. Am J Prev Med 2007;32:264–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacobs DR, Jr, Hannan PJ, Wallace D, Liu K, Williams OD, Lewis CE. Interpreting age, period and cohort effects in plasma lipids and serum insulin using repeated measures regression analysis: the CARDIA Study. Stat Med 1999;18:655–79 [DOI] [PubMed] [Google Scholar]
- 11.Nielsen SJ, Siega-Riz AM, Popkin BM. Trends in food locations and sources among adolescents and young adults. Prev Med 2002;35:107–13 [DOI] [PubMed] [Google Scholar]
- 12.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977-1998. JAMA 2003;289:450–3 [DOI] [PubMed] [Google Scholar]
- 13.Du H, Feskens E. Dietary determinants of obesity. Acta Cardiol 2010;65:377–86 [DOI] [PubMed] [Google Scholar]
- 14.Lockheart MS, Steffen LM, Rebnord HM, Fimreite RL, Ringstad J, Thelle DS, Pedersen JI, Jacobs DR., Jr Dietary patterns, food groups and myocardial infarction: a case-control study. Br J Nutr 2007;98:380–7 [DOI] [PubMed] [Google Scholar]
- 15.Nettleton JA, Steffen LM, Ni H, Liu K, Jacobs DR., Jr Dietary patterns and risk of incident type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 2008;31:1777–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nettleton JA, Schulze MB, Jiang R, Jenny NS, Burke GL, Jacobs DR., Jr A priori-defined dietary patterns and markers of cardiovascular disease risk in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 2008;88:185–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacobs DR, Jr, Sluik D, Rokling-Andersen MH, Anderssen SA, Drevon CA. Association of 1-y changes in diet pattern with cardiovascular disease risk factors and adipokines: results from the 1-y randomized Oslo Diet and Exercise Study. Am J Clin Nutr 2009;89:509–17 [DOI] [PubMed] [Google Scholar]
- 18.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988;41:1105–16 [DOI] [PubMed] [Google Scholar]
- 19.Jacobs DR, Jr, Hahn LP, Haskell WL, Pirie P, Sidney S. Validity and reliability of a short physical activity history: CARDIA and the Minnesota Heart Health Program. J Cardiopulm Rehabil 1989;9:448–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McDonald A, Van Horn L, Slattery M, Hilner J, Bragg C, Caan B, Jacobs D, Jr, Liu K, Hubert H, Gernhofer N, et al. The CARDIA dietary history: development, implementation, and evaluation. J Am Diet Assoc 1991;91:1104–12 [PubMed] [Google Scholar]
- 21.Liu K, Slattery M, Jacobs D, Jr, Cutter G, McDonald A, Van Horn L, Hilner JE, Caan B, Bragg C, Dyer A, et al. A study of the reliability and comparative validity of the CARDIA dietary history. Ethn Dis 1994;4:15–27 [PubMed] [Google Scholar]
- 22.Mishra GD, McNaughton SA, Bramwell GD, Wadsworth ME. Longitudinal changes in dietary patterns during adult life. Br J Nutr 2006;96:735–44 [PubMed] [Google Scholar]
- 23.Harris KM, Gordon-Larsen P, Chantala K, Udry JR. Longitudinal trends in race/ethnic disparities in leading health indicators from adolescence to young adulthood. Arch Pediatr Adolesc Med 2006;160:74–81 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.