Abstract
Objective
The purpose of this study was to measure geographic variations in the availability and use of chiropractic under Medicare.
Methods
A cross-sectional design was employed to analyze a large nationally representative sample of Medicare data. Data from a 20% representative sample of all paid Medicare Part B fee for service claims for 2007 were merged with files containing beneficiary and provider data. The sample was restricted to adults aged 65–99. Measures of chiropractic availability and use were described and selectively mapped by state. Geographic variations were quantified. Spearmans’s test was used to evaluate for correlation between chiropractic availability and use.
Results
The average number of doctors of chiropractic (DC) by state was 1,135; average DC per 1,000 beneficiaries was 2.5 (SD 1.1). The average number of chiropractic users by state was 34,502 (SD 30,844); average chiropractic users per 1,000 beneficiaries was 76 (SD 41). Chiropractic availability by state varied six-fold and chiropractic use varied nearly thirty-fold. Availability was strongly correlated with use (Spearman's rho 0.86, p<.001). Expenditures per DC were highest in the upper Midwest and lowest in the far west; expenditures per user were highest in New England and New York, and lowest in the West.
Conclusion
Chiropractic availability and use by older adults under Medicare predominated in rural states in the north central US. Expenditures were higher in the East and Midwest, and lower in the far West. Chiropractic availability and use by state were highly correlated. Future analyses should employ small area analysis and statistical modeling to identify factors predictive of chiropractic use.
MeSH terms: Chiropractic, Aged, Medicare
Introduction
Chiropractic services are covered under the Medicare system in the United States (US), but the scope of covered services is tightly restricted. The chiropractic profession wants the Department of Health and Human Services to make chiropractic care more accessible to Medicare beneficiaries by expanding the scope of allowable chiropractic services, but chiropractic has been described as “a significant vulnerability” for Medicare, due to ongoing concerns about the cost of unnecessary services.1 Furthermore, a demonstration project conducted by Medicare to determine the effect of expanding allowable services concluded that expansion would increase overall costs to Medicare.2 Considerable uncertainty surrounds the question of whether the scope of allowable chiropractic services should be expanded under the Medicare program.
Little is known about the availability and use of chiropractic care currently provided under Medicare. Government reports on chiropractic use under Medicare have focused for the most part upon identifying and controlling the provision of unnecessary services, with limited and inconsistent evaluation of chiropractic use overall.1, 3–6 Other studies of chiropractic use under Medicare were limited to analysis of procedure rates,7 or to relatively small samples of survey respondents.8, 9 Recent national studies on chiropractic utilization and expenditures and on the supply and demand of chiropractic did not focus specifically on the Medicare beneficiary population.10, 11 Few studies have measured geographic variations in chiropractic care, and no nationally representative study has been conducted on geographic variations in the availability and use of chiropractic under Medicare. Evaluation of the availability and use of chiropractic under Medicare will inform chiropractic organizations, policy makers and other stakeholders.
To evaluate these characteristics, availability and use may be measured in various terms; for example, measures of availability may include third party coverage, affordability, distance to point of service, clinic hours, and allowed scope of practice. Chiropractic availability can be measured as the ratio of Doctors of Chiropractic (DC) to potential chiropractic users, use can be measured as the ratio of chiropractic users to potential users, and costs can be measured as allowed charges and payments for chiropractic services. This investigation analyzed a large nationally representative sample of Medicare data to measure chiropractic availability and use for older US adults using the above parameters. This study generated and selected measures that were mapped to illustrate geographic variations.
Methods
Design and Sampling
A cross-sectional design was employed to analyze Medicare data. Claims data from the Medicare Carrier File for 2007 were merged on unique beneficary identifier with beneficiary data from the Medicare Denominator File for 2007. The resultant file was susequently merged on unique provider identifier with data from the Medicare Provider UPIN File. The Carrier File provided a 20% representative sample (randomly generated based upon the last two digits of the the social security number portion of the claim number) of all paid Medicare Part B fee for service claims for chiropractic care. The study sample was restricted to adults aged 65–99 (living as of January 1st of each year), for the year 2007, and to claims records for services provided by chiropractic physicians practicing within the 50 US states and the District of Columbia. For the sake of simplicity, in this paper the District of Columbia is considered to be a state. Chiropractic claims were identified by provider specialty code 35. Excluded from the analysis were records for unallowed claims and duplicate claims for the same patient, provider, procedure and date of service. To reduce the likelihood of individual identification, Medicare beneficiaries older than 99 were excluded. The data used in this study were obtained under a data user agreement with The Centers for Medicare and Medicaid Services. The research plan was reviewed and approved by the Committee for the Protection of Human Subjects, Dartmouth College, Hanover NH. The data were tabulated in EXCEL 2007 (Microsoft Corp, Redmond, WA) and analyzed in EXCEL and STATA 11 (Statacorp, College Station, TX). Data mapping was performed with ArcMap 10.0 (ESRI, Redlands, CA).
Analysis
Medicare claims administration is handled by regional carriers known as Medicare Administrative Contractors (MACs). A MAC is assigned to each of the 15 Medicare administrative contractor jurisdictions (MACJs), which are typically comprised of a block of 3–4 contiguous states. The claims data were aggregated primarily to the state level, and secondarily to the MACJ, using the current coinfiguration of jurisdictions. The data were analyzed using the state as the geographic unit of analysis for availability and use, and the MACJ as the unit of analysis for costs. Data fields with fewer than 11 observations were suppressed to reduce the likelihood of individual identification. Results of analysis of the 20% sample were multiplied by a factor of five to generate 100% estimates. Descriptive statistics for chiropractic availability (defined as Medicare-servicing chiropractors per 1,000 Medicare Part B beneficiaries) and chiropractic users (defined as Medicare beneficiaries with at least one paid claim for chiropractic care on a date-of-service in 2007) were generated. Selected measures of chiropractic availability, use and cost were mapped to illustrate geographic variations, and geographic variations were quantified by coefficient of variation (CV), extremal ratio (ER) and interquartile ratio (IR).12 Spearmans’s test was used to evaluate for correlation between chiropractic availability and use.
Results
Availability
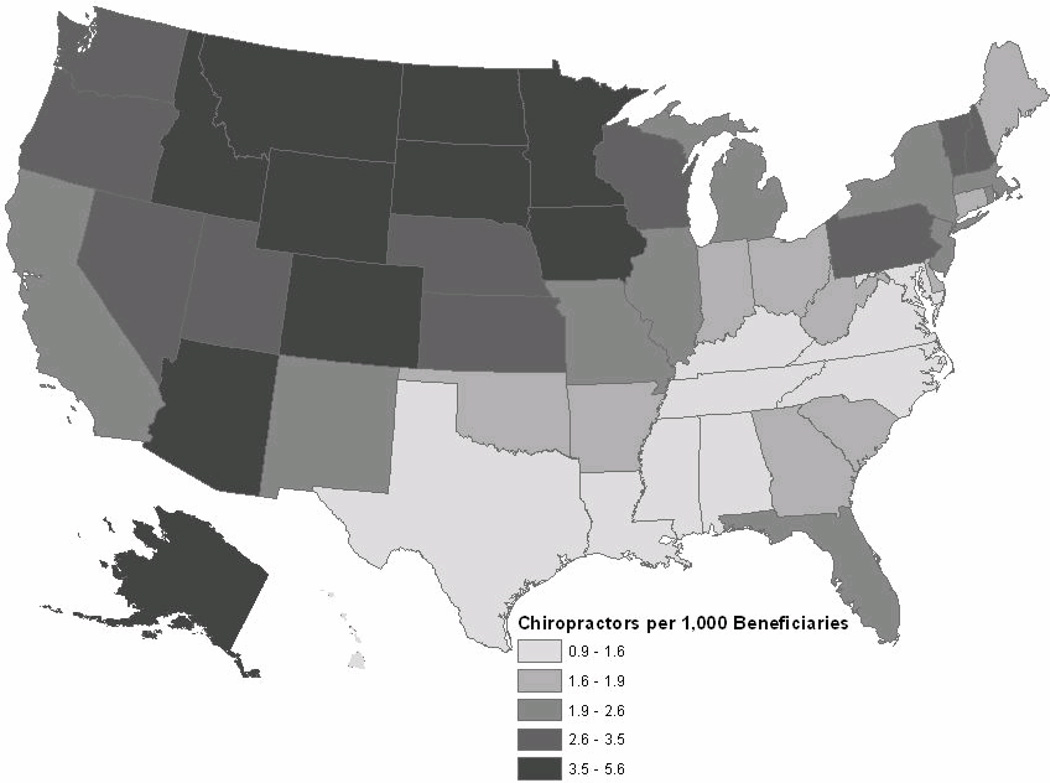
Nationally, the total number of chiroractors in 2007 was 57,912. The number of DCs per state ranged from 40 in the District of Columbia to 4,507 in California (mean 1,135; standard deviation (SD) 1,065).[Table 1] The average number of DCs per 1,000 beneficiaries ranged from 0.9 in Mississippi to 5.6 in South Dakota (mean 2.5; SD 1.1). Figure 1 illustrates variation by state in quintiles of chiropractic physicians per 1,000 beneficiaries. Chiropractic availability to the Medicare beneficary population was highest in the North and West, with a large block of greater availability in the northern plains and mountain states, and lowest in the South and Hawaii. Chiropractic availability by state varied six-fold overall (CV 0.44; ER 6.02; IR 1.97).
Table 1.
Availability of DCs under Medicare and Use of Chiropractic by Medicare part B Beneficiaries, 2007
| State | DCs | Users* | State | DCs | Users* |
|---|---|---|---|---|---|
| Alabama | 614 | 24,735 | Montana | 387 | 12,310 |
| Alaska | 192 | 2,860 | Nebraska | 559 | 24,580 |
| Arizona | 1,674 | 39,270 | Nevada | 500 | 10,160 |
| Arkansas | 519 | 21,355 | New Hampshire | 440 | 9,630 |
| California | 4,507 | 111,170 | New Jersey | 2,156 | 55,560 |
| Colorado | 997 | 23,030 | New Mexico | 363 | 12,275 |
| Connecticut | 657 | 13,155 | New York | 3,353 | 90,235 |
| Delaware | 197 | 5,520 | North Carolina | 1,251 | 46,090 |
| District of Columbia | 40 | 295 | North Dakota | 378 | 15,820 |
| Florida | 4,406 | 110,685 | Ohio | 2,125 | 81,155 |
| Georgia | 1,248 | 35,320 | Oklahoma | 697 | 25,765 |
| Hawaii | 114 | 1,955 | Oregon | 782 | 17,565 |
| Idaho | 457 | 12,115 | Pennsylvania | 2,866 | 78,840 |
| Illinois | 3063 | 99,855 | Rhode Island | 186 | 3,235 |
| Indiana | 1,176 | 43,010 | South Carolina | 774 | 24,815 |
| Iowa | 1,427 | 67,600 | South Dakota | 550 | 19,935 |
| Kansas | 957 | 42,315 | Tennessee | 895 | 30,190 |
| Kentucky | 708 | 26,860 | Texas | 2,573 | 96,165 |
| Louisiana | 378 | 11,980 | Utah | 419 | 10,965 |
| Maine | 338 | 11,175 | Vermont | 204 | 5,235 |
| Maryland | 596 | 13,770 | Virginia | 909 | 26,885 |
| Massachusetts | 1,199 | 28,685 | Washington | 1,668 | 50,055 |
| Michigan | 2,473 | 85,470 | West Virginia | 328 | 8,560 |
| Minnesota | 1,820 | 49,515 | Wisconsin | 1,846 | 57,240 |
| Mississippi | 270 | 9,420 | Wyoming | 236 | 5,520 |
| Missouri | 1,440 | 49,710 | Total | 57,912 | 1,759,615 |
100% estimates extrapolated from 20% representative sample
Figure 1.
Variation by State of Chiropractic Providers per 1,000 Part B Medicare Beneficiaries, 2007
Use
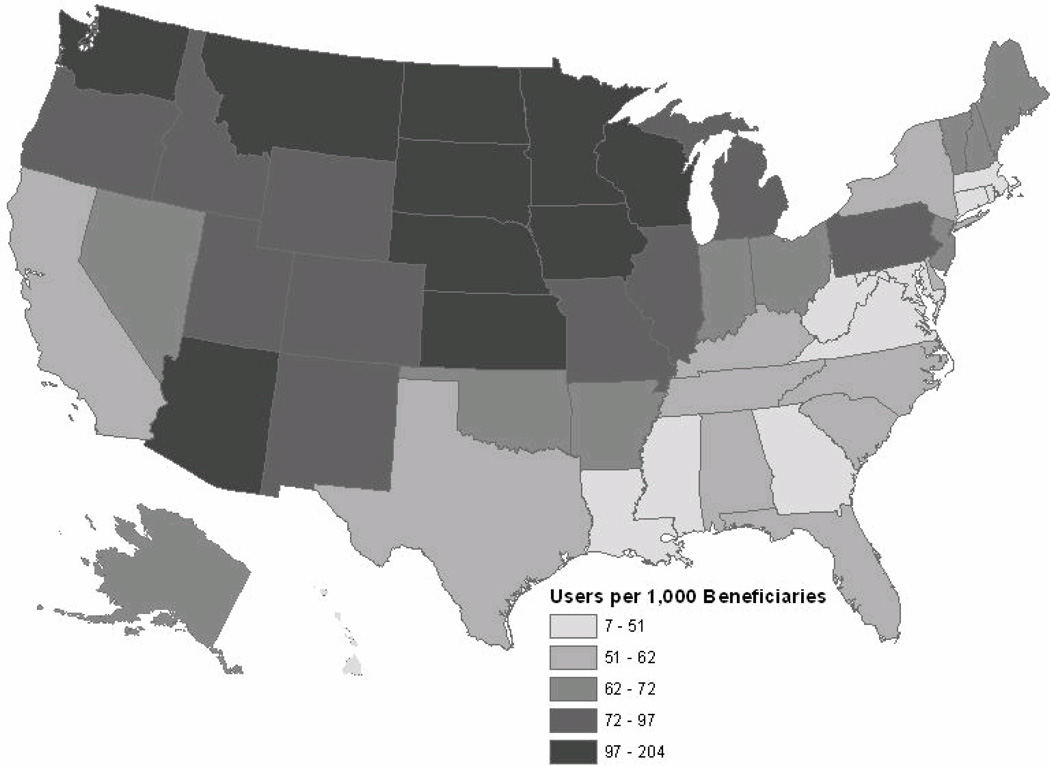
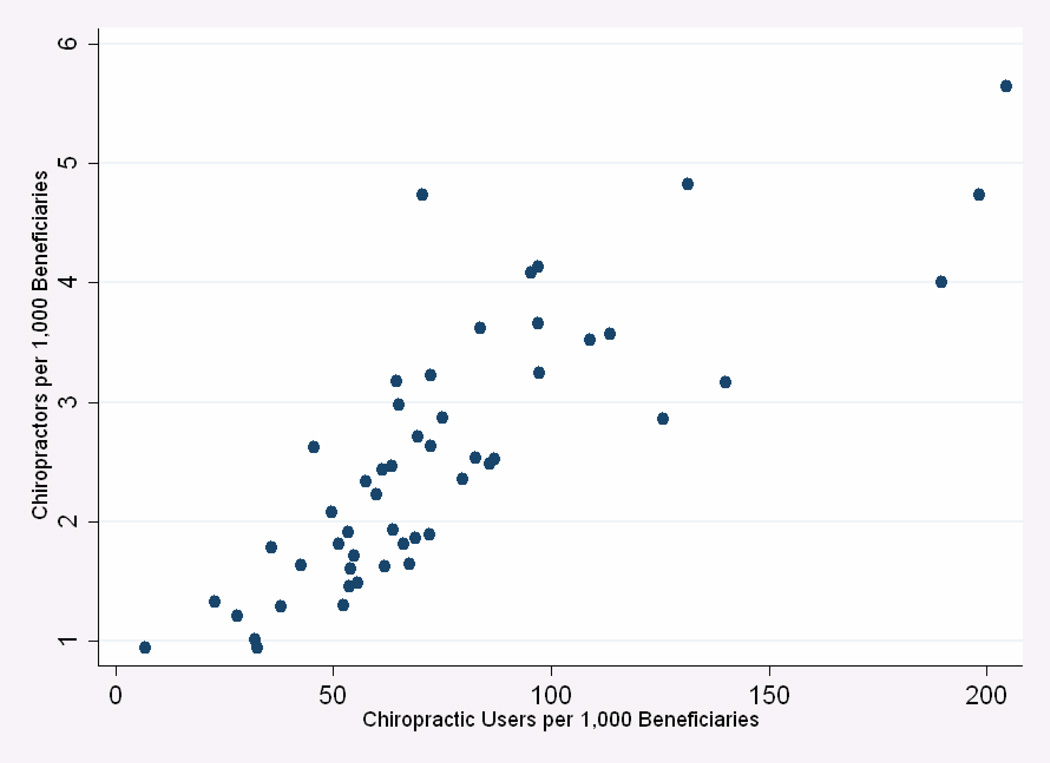
The estimated national total of Medicare beneficiaries who were chiroractic users in 2007 was 1,759,615. By state, the estimated number of chiropractic users ranged from 295 in the District of Columbia to 111,170 in California (mean 34,502; SD 30,844). After California, the states with the greatest number of both DCs and users were Florida, New York and Illinois. Chiropractic users per 1,000 beneficiaries ranged from seven in the District of Columbia to 204 in South Dakota (mean 76; SD 41). Figure 2 illustrates variation by state in quintiles of chiropractic users per 1,000 beneficiaries. Users were more highly concentrated in the northern and western United States, with a large block of higher use in the northern plains and prairie states. States with the lowest rates of use were in the Southeast, southern New England and Hawaii. Chiropractic use by state varied nearly thirty-fold (CV 0.54; ER 29.36; IR 1.63). When analyzed by state, the number of users per thousand beneficiaries was strongly correlated with DCs per 1,000 beneficiaries (Spearman's rho 0.86, p<.001).[Figure 3]
Figure 2.
Variation by State of Chiropractic Users per 1,000 Part B Medicare Beneficiaries, 2007
Figure 3.
Correlation by State between Availability of DCs and Chiropractic Users, per 1,000 Part B Medicare Beneficiaries, 2007
Each chiropractic physician provided care to an average of 30 Medicare beneficiaries in 2007. The average number of users per DC ranged from seven in the District of Columbia to 47 in Iowa (mean 30; SD 8). The states with the largest average numbers of users per DC were the rural heartland states of Iowa, Kansas, Nebraska and North Dakota. In most of the large urbanized states, the average number of users per DC was below the mean of 30.
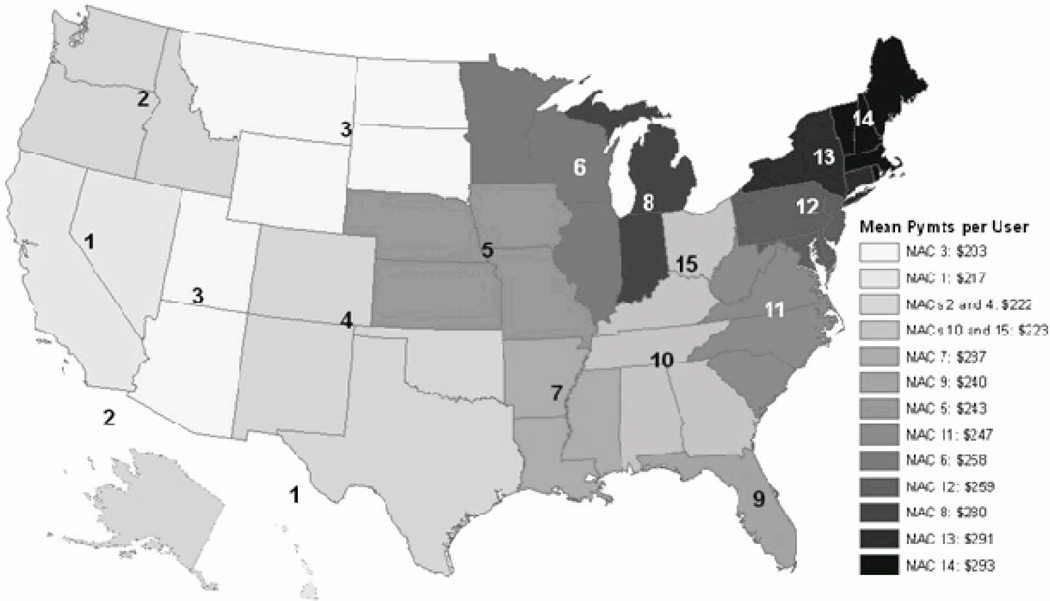
Cost
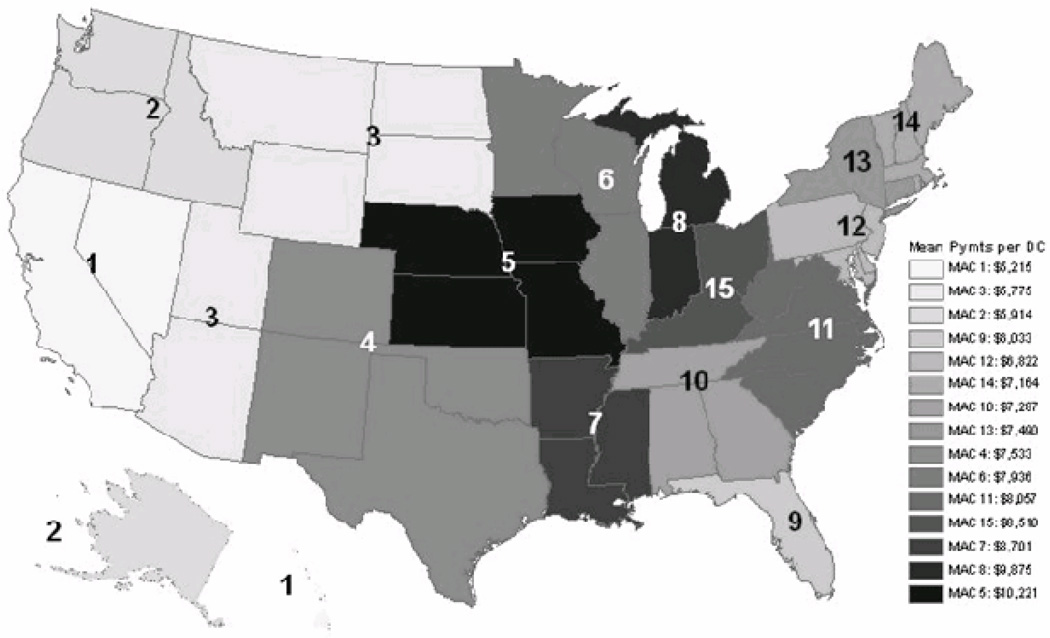
Total allowed charges by MACJ ranged from $14 million in MACJ seven (Arkansas, Louisiana and Mississippi) to $73 million in MACJ six (Illinois, Minnesota and Wisconsin). Total payments ranged from $10 million to $53 million.[Table 2] Average payment per procedure ranged from $20.57 in MACJ fifteen (Kentucky and Ohio) to $24.97 in MACJ twelve (Delaware, District of Columbia, Maryland, New Jersey, Pennsylvania). Average allowed charges per DC ranged from $7,000 in MACJ one (California, Hawaii and Nevada) to $14,000 in MACJ five (Iowa, Kansas, Missouri and Nebraska). Average payments per DC ranged from $5,000 to $10,000.[Figure 4] Average allowed charges per chiropractic user ranged from $279 in MACJ three (Arizona, Montana, North Dakota, South Dakota, Utah and Wyoming) to $395 in MACJ fourteen (Maine, Massachusetts, New Hampshire, Rhode Island, Vermont). Average payments per user ranged from $203 to $293.[Figure 5] Overall variation in cost (measured as average payment per procedure) was relatively low (CV 0.06; ER 1.21; IR 1.12) compared to variations in availability and use
Table 2.
Payments for Chiropractic Services Provided under Medicare Part B, by Medicare Administrative Contractor Jurisdiction (MACJ), 2007
| MACJ | Included States | Allowed Charges |
Paym ents: total |
per DC* | per User** | per Procedure*** |
|---|---|---|---|---|---|---|
| 1 | California, Hawaii, Nevada | $36,026,770 | $26,705,261 | $5,215 | $217 | $24.18 |
| 2 | Alaska, Idaho, Oregon, Arizona, Montana, North | $25,168,897 | $18,327,498 | $5,914 | $222 | $21.96 |
| 3 | Dakota, Colorado, New Mexico, | $28,979,164 | $21,043,210 | $5,775 | $203 | $21.61 |
| 4 | Oklahoma, | $47,751,776 | $34,878,862 | $7,533 | $222 | $22.11 |
| 5 | Iowa, Kansas, Missouri, | $61,853,193 | $44,797,921 | $10,221 | $243 | $22.21 |
| 6 | Illinois, Minnesota, Wisconsin | $73,327,324 | $53,400,669 | $7,936 | $258 | $21.47 |
| 7 | Arkansas, Louisiana, Mississippi | $13,879,919 | $10,153,692 | $8,701 | $237 | $21.31 |
| 8 | Indiana, Michigan | $49,195,356 | $36,032,193 | $9,875 | $280 | $23.65 |
| 9 | Florida | $35,265,383 | $26,579,733 | $6,033 | $240 | $23.80 |
| 10 | Alabama, Georgia, Tennessee North Carolina, South Carolina, | $27,366,132 | $20,091,167 | $7,287 | $223 | $22.07 |
| 11 | Virginia, West Virginia Delaware, District of Columbia, Maryland, New Jersey, | $35,542,845 | $26,282,532 | $8,057 | $247 | $22.42 |
| 12 | Pennsylvania | $53,457,411 | $39,940,327 | $6,822 | $259 | $24.97 |
| 13 | Connecticut, New York Maine, Massachusetts, New Hamp- | $39,772,086 | $30,036,049 | $7,490 | $291 | $24.43 |
| 14 | $22,880,054 | $16,956,394 | $7,164 | $293 | $24.27 | |
| 15 | Kentucky, Ohio | $32,947,279 | $24,110,031 | $8,510 | $223 | $20.57 |
Average Medicare payment per DC was calculated by dividing total payments for chiropractic services in the Medicare administrative contractor jurisdictions (MACJ) by the number of Medicare-servicing DCs in that MACJ.
Average Medicare payment per chiropractic user was calculated by dividing total payments for chiropractic services in the MAJC by the number of Part B Medicare Beneficiaries who used chiropractic services in that MACJ.
Average Medicare payment per procedure was calculated by dividing total payments for chiropractic services in the MACJ by the number of chiropractic procedures allowed in that MACJ.
Figure 4.
Regional Variations in Expenditures per Chiropractic Physician, 2007. The map illustrates the current Medicare administrative contractor jurisdictions (MACJ) for the 50 US states and the District of Columbia. Not all 2007 claims were administered by MACJ as depicted. Average Medicare payment per DC was calculated by dividing total payments for chiropractic services in the MACJ by the number of Medicare-servicing DCs in that MACJ.
Figure 5.
Regional Variations in Expenditures per Chiropractic User, 2007. The map illustrates the current Medicare administrative contractor jurisdictions (MACJ) for the 50 US states and the District of Columbia. Not all 2007 claims were administered by MACJ as depicted. Average Medicare payment per chiropractic user was calculated by dividing total payments for chiropractic services in the MAJC by the number of Part B Medicare Beneficiaries who used chiropractic services in that MACJ.
Discussion
Summary of Findings
In general, the most populous and urbanized states were found to have the most DCs. However, the ratio of DCs to potential chiropractic users is a more specific indicator of availability than the absolute number of DCs. Measured as a ratio of DCs to beneficiaries, the chiropractic availablility to aged Medicare beneficiaries was higher in rural states. Among the states the average availability was 2.5 DCs per 1,000 Medicare beneficiaries. Chiropractic care was generally more available to Medicare beneficiaries in the North and West, and less available in the Southeast.
As with the number of DCs, absolute numbers of older adult chiropractic users were found in the most highly populated areas, but higher proportions of users predominated in the northern and western United States, especially the northern plains and prairie states. States with lower proportions of users were located mostly in the South and East. By state, chiropractic users averaged 76 per 1,000 Medicare beneficiaries. Expenditures per DC were highest in the upper Midwest and lowest in the far west; expenditures per user were highest in New England and New York, and lowest in the West. Expenditures per procedure were highest in the Northeast and lowest in the South. Chiropractic use among older US adults was strongly correlated with availability.
Comparison with Findings of Previous Studies
Cherkin and Mootz reported that in 1995 the states with the lowest DC to population ratios included the District of Columbia, Louisiana, Maryland and Mississippi.13 The results of this analysis show the the same four states with the lowest availability to the Medicare beneficiary population. Cherkin and Mootz reported the highest DC to population ratios for Arizona, Colorado, and Hawaii, but the Dakotas and Minnesota top the list in availability to Medicare beneficaries. Arizona also had relatively high availability to the Medicare population, but relative availability in Hawaii was low.
The supply of 2.39 DCs for every 10,000 US adults reported by Davis and colleagues for 2004 10 was equivalent to an availability ratio of 2.7 DCs per 1,000 Medicare beneficiaries in 2004,14 close to the average availability of 2.5 DCs per 1,000 Medicare beneficiaries reported here for 2007. Grier and Lepnurm attempted to model an ideal DC: population ratio based upon the prevalence of musculoskeletal problems in the general population, and arrived at an ideal ratio of 1 DC per every 2,588 persons, or 0.38 DCs per 1,000.15 By that standard, the average availability ratio reported here of 2.5 DCs per 1,000 beneficiaries would be excessive for the Medicare population but suboptimal as a supply ratio for the general population. However, given current trends in the supply of US DCs, as the population ages and an increasing share of the burden of musculoskeletal problems is borne by older adults, the chiropractic availability ratio for Medicare beneficiaries is likely to decrease.10
Wolinsky and colleagues estimated the rate of use of chiropractic among Medicare beneficiaries to be 4.6%.9 Foster and colleagues reported in 2001 that 11% of US adults over age 65 used chiropractic.16 Based upon an analysis of claims data from 2001 the US Dept of Health and Human Services estimated a rate of 6% chiropractic usage among Medicare beneficiaries.1 Evans and colleagues reported that among a subset of survey respondents 65 years of age and older, 8.7% had used chiropractic or osteopathic manipulation within the past 12 months.17 In the present study, when analyzed by state, the number of chiropractic users averaged 76 beneficiaries per 1,000, or 7.6% of beneficiaries. Conversion to an average user rate weighted by the Medicare beneficiary population in each state yields a national rate of use of 6.9%. Both weighted and unweighted average rates are in line with previous estimates cited above. The Centers for Medicare and Medicaid Services has reported allowed charges for chiropractic services in 2007 totaling $703 million, approximately 20% higher than the totals we report here.18 CMS however does not disclose the methods used to generate this statistic. If the beneficiary population included individuals younger than 65 years or residents outside the 50 US states, or if the included claims were not restricted by provider specialty code and CPT code range, higher estimates would be expected.
Implications
Although Medicare is a federal program and Medicare claims are handled by regional administrative contractors, chiropractic practice is licensed and regulated by the states, so analysis of chiropractic use by state can be informative from a policy point of view. Information on availability of chiropractic services by state may aid planning for resource allocation, and may help DCs to decide where to locate their practices. Chiropractic was founded in Iowa and most of the early development of the chiropractic profession took place there and in surrounding states. By several measures, chiropractic appears to maintain its strongest presence in Iowa and nearby states such as Kansas, Nebraska, Minnesota and the Dakotas. Doctors of chiropractic tend to locate their practices in the more populous states, but those in many of the more sparsely populated states appear to have busier practices on average, at least with regard to older adults. Perhaps the most striking finding reported here is the low cost of chiropractic care under Medicare. By MACJ, Medicare’s average expenditure in 2007 was $21–25 per chiropractic procedure. Under Medicare, payment per chiropractic procedure is equivalent to payment per chiropractic office visit, because Medicare allows only one procedure per visit.
This investigation is the first nationally representative study of geographic variations in the availability and use of chiropractic services under Medicare. In 1973 Wennberg published the first in a series of studies that described unexplained geographic variations in medical care.19 Since then, numerous reports have been published on variations in the distribution and use of medical services.20–24 Such variations are likely to be unwarranted if they cannot be explained on the basis of differences in illness rates or patient preferences and characteristics.20, 25 To explain variations in medical care, health care services may be categorized as necessary, preference- sensitive, or supply-sensitive.26 These categories may also prove useful in evaluations of the clinical appropriateness of chiropractic care.27 Necessary care is treatment that has been proven to be effective and safe. When the best treatment choice is not clear-cut (as in the care of non-specific low back pain), care is considered to be preference- sensitive, and choice of treatment should be based upon patient preferences and a well-informed shared decision-making process.28 Shannon and colleagues have argued that patient beliefs and preferences should play a more prominent role in clinical decision making about integrative medicine.29 Supply-Sensitive Care is governed by the local supply of health care providers, and the availability of facilities and services: the greater the supply, the higher the rate of use, irrespective of necessity or patient preference.26
The phenomenon of supply sensitive care is likely widespread in fee for service payment systems, due to ubiquitous provider self interest. The high degree of correlation between chiropractic availability and use reported here suggests the possibility that chiropractic care for older adults may be supply sensitive in certain areas. However, an effect-cause relationship is also possible: DCs are likely to establish practices in areas where demand for their services is expected to be higher. Furthermore, local health care markets (geographic areas within which patient populations use clinical services) tend not to be determined by political boundaries.30–32 Patients cross municipal, county and even state lines to use clinical services, and large metropolitan areas often contain multiple local health care markets. Thus, significant local variations were likely smoothed over in our state-level analysis. Identification of supply sensitivity in chiropractic care is challenging, in part because the appropriate use of chiropractic care overall has not been determined.27 The challenge is compounded for chiropractic under Medicare, which limits the scope of reimbursable chiropractic practice to spinal manipulation only. The chiropractic profession has argued that expansion of allowable services will allow Medicare beneficiaries to benefit from the full scope chiropractic practice, but Medicare is limited to evaluating the appropriateness of chiropractic care through the narrow lens of practices restricted to spinal manipulation.27 Future analyses of geographic variations in chiropractic availability and use should be performed employing a smaller unit of geographic analysis more likely to reflect actual patterns of use.30 Statistical modeling at the individual level would facilitate determination of factors predictive of chiropractic use among Medicare beneficiaries.
Limitations
This study analyzed only Medicare Part B fee for service claims in 2007, exclusive of claims for expanded chiropractic services provided under a demonstration project that was conducted from 2005 to 2007.2 Inferences drawn from the results are applicable only to US Medicare beneficiaries aged 65–99, and cannot be generalized to populations that are younger, outside the US, or not covered by Medicare. The conclusions cannot be generalized to chiropractic practice in general, because Medicare restricts overage of chiropractic services to spinal manipulation. No predictive modeling was performed to analyze for causation. Reported averages are unweighted, except as noted. The validity of the results of claims-based research may have been limited by inaccurate entry of information on claim forms. US states typically contain multiple local health care markets, so aggregation of data to the state level likely obscured localized variations in use. Chiropractic availability as reported here is a measure of provider availability that is specific to the beneficiary population; this measure should not be misinterpreted as a population-based measure of provider supply.
Allowable charges under Medicare are determined by MACJ, so analysis of costs by region is more appropriate than by state. However, not all 2007 claims were administered by MACJ as depicted in Table 2 and Figure 3. In 2006 CMS began to reconfigure the distribution of MACJs, and reconfiguration continued through 2007. 33 Allowable charges vary by MACJ, are reviewed annually, and may change more than once per year. These ongoing administrative changes make it difficult to compare costs from year to year, or between administrative jurisdictions. The cost data were analyzed using the current congfiguration of MACJs as the geographic units of analysis.33 Finally, cost analysis was not a primary focus of this study. Cost issues such as the cost-effectiveness of care, the resource-based evaluation of services, geographic variations in the cost-of-living, and other economic factors were not addressed in this paper, and would be worthy of future investigation.
Conclusions
Chiropractic availability and use by older adults under Medicare predominate in rural states in the North Central US. Medicare expenditures for chiropractic care were generally higher in the Northeast and Midwest, and lower in the South and West. Chiropractic availability and use by state are highly correlated under Medicare. Future analyses should employ small area analysis and statistical modeling at the individual level to identify factors predictive of chiropractic use in older adults.
This study provides the most comprehensive information available to date on geographic variations in the availability and use of chiropractic under Medicare.
An understanding of the availability of chiropractic care may aid planning for resource allocation, and may help doctors of chiropractic to decide where to locate their practices.
Knowledge of chiropractic availability, utilization and cost will inform decision making by chiropractic organizations, federal policy makers and other stakeholders with regard to the current administration and potential future expansion of chiropractic coverage under Medicare.
Acknowledgments
FUNDING SOURCES AND CONFLICTS OF INTEREST
This study was directly funded under a research career development grant from the National Center for Complementary and Alternative Medicine. Grant Number: 5K01AT005092-03.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No conflicts of interest were reported for this study.
Contributor Information
James M. Whedon, The Dartmouth Institute for Health Policy & Clinical Practice.
Yunjie Song, The Dartmouth Institute for Health Policy & Clinical Practice.
References
- 1.Office of Inspector General. Chiropractic Services in the Medicare Program: Patient Vulnerability Analysis. Washington, D.C: Department of Health and Human Services; 2005. [Google Scholar]
- 2.Stason WB, Ritter G, Shepard DS, et al. Final Report: Evaluation of the Demonstration of Expanded Coverage of Chiropractic Services under Medicare. Waltham, MA: Brandeis University; 2010. May 12, [Google Scholar]
- 3.Office of Inspector General. Chiropractic Services under Medicare. Washington, D.C: Office of Analysis and Inspections, Department of Health and Human Services; 1986. [Google Scholar]
- 4.Office of Inspector General. Chiropractic Care: Controls Used by Medicare, Medicaid, and Other Payers. Washington, D.C: Department of Health and Human Services; 1998. [Google Scholar]
- 5.Office of Inspector General. Utilization Parameters for Chiropractic Treatments. Washington, D.C: Department of Health and Human Services; 1999. [Google Scholar]
- 6.Office of Inspector General. Inappropriate Medicare Payments for Chiropractic Services. Washington, DC: Department of Health and Human Service; 2009. [Google Scholar]
- 7.Whedon JM, Davis MA. Medicare part B claims for chiropractic spinal manipulation, 1998 to 2004. J Manipulative Physiol Ther. 2010;33(8):558–561. doi: 10.1016/j.jmpt.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weigel P, Hockenberry JM, Bentler SE, et al. A longitudinal study of chiropractic use among older adults in the United States. Chiropr Osteopat. 2010;18(34):34. doi: 10.1186/1746-1340-18-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolinsky F, Liu L, Miller T, et al. The use of chiropractors by older adults in the United States. Chiropr Osteopat. 2007 Sep 6;15(12) doi: 10.1186/1746-1340-15-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davis MA, Davis AM, Luan J, Weeks WB. The supply and demand of chiropractors in the United States from 1996 to 2005. Alternative Therapies in Health & Medicine. 2009;15(3):36–40. [PubMed] [Google Scholar]
- 11.Davis MA, Sirovich B, Weeks W. Utilization and expenditures on chiropractic care in the United States from 1997 to 2006. Health Services Research. 2010;45(3):748–761. doi: 10.1111/j.1475-6773.2009.01067.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wennberg JE, Fisher ES, Stukel TA, Skinner JS, Sharp SM, Bronner KK. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. BMJ. 2004;328(7440):607. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cherkin DC, Mootz RD. Chiropractic in the United States: Training, Practice, and Research. Seattle, WA: The Agency for Health Care Policy and Research; 1997. [Google Scholar]
- 14.Medicare Part B FFS beneficiaries in 2004 totaled 27, 075 (100% estimate extrapolated from unpublished 20% representative sample, CMS), , Total US population in 2004 was 293, 739 (US Census Bureau), , Beneficiaries/population = 27, 075/293,045,739 =0.09 = 9%, , 0.09 X 10000 US Adults = 900 US Adults, 2.39 / 900 = 0.0027 or 2.7 per 1000 Medicare beneficiaries.
- 15.Grier AR, Lepnurm R. Modeling a chiropractor:population ratio. J Manipulative Physiol Ther. 1995;7(18):464–470. [PubMed] [Google Scholar]
- 16.Foster DF, Phillips RS, Hamel MB, Eisenberg DM. Alternative medicine use in older Americans. J Am Geriatr Soc. 2000 Dec;48(12):1560–1565. doi: 10.1111/j.1532-5415.2000.tb03864.x. [DOI] [PubMed] [Google Scholar]
- 17.Marion Willard Evans MW, Jr, Ndetan H, Hawk C. Use of Chiropractic or Osteopathic Manipulation by Adults Aged 50 and Older: An Analysis of Data from the 2007 National Health Interview Survey. Topics in Integrative Health Care. 2010;1(2) [Google Scholar]
- 18.Centers for Medicare and Medicaid Services. Medicare Utilization for Part B. [Accessed July 23, 2010];Medicare Fee for Service for Parts A & B. [ https://www.cms.gov/MedicareFeeforSvcPartsAB/04_MedicareUtilizationforPartB.asp#TopOfPage.
- 19.Wennberg J, Gittelsohn Small area variations in health care delivery. Science. 1973;182(117):1102–1108. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- 20.Fisher ES. Research Agenda and Findings. [Accessed July 21, 2009];Dartmouth Atlas of Health Care. [ http://www.dartmouthatlas.org/agenda.shtm.
- 21.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003 Feb 18;138(4):288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 22.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003 Feb 18;138(4):273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 23.Wennberg JE, Brownlee S, Fisher ES, Skinner JS, Weinstein JM. An agenda for change. Improving quality and curbing health care spending: opportunities for the congress and the Obama administration. Lebanon, NH: The Dartmouth Institute for Health Policy and Clinical Practice; 2008. [PubMed] [Google Scholar]
- 24.Wennberg JE, Cooper MM. The Quality of Medical Care in the United States: A Report on the Medicare Program. Chicago: American Health Association Press; 1999. [PubMed] [Google Scholar]
- 25.Sutherland JM, Fisher ES, Skinner JS. Getting past denial--the high cost of health care in the United States. N Engl J Med. 2009 Sep 24;361(13):1227–1230. doi: 10.1056/NEJMp0907172. [DOI] [PubMed] [Google Scholar]
- 26.John Wennberg. Tracking Medicine: A Researcher's Quest to Understand Health Care. New York, NY: Oxford university press; 2010. [Google Scholar]
- 27.Whedon JM, Davis MA, Phillips RB. Implications and Limitations of Appropriateness Studies for Chiropractic. Journal of Chiropractic Humanities. 2010 November; doi: 10.1016/j.echu.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wennberg JE. Medical Technology Leadership Forum. San Francisco, CA: 2008. Evidence-Based Medicine: Vehicle to Value and Efficiency? [Google Scholar]
- 29.Shannon S, Weil A, Kaplan BJ. Medical decision making in integrative medicine. Alternative and Complementary Therapies. 2011;17(2):84–91. [Google Scholar]
- 30.Goodman DC, Mick SS, Bott D, et al. Primary care service areas: a new tool for the evaluation of primary care services. Health Serv Res. 2003 Feb;38(1 Pt 1):287–309. doi: 10.1111/1475-6773.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goody B. Defining rural hospital markets. Health Serv Res. 1993 Jun;28(2):183–200. [PMC free article] [PubMed] [Google Scholar]
- 32.Zwanziger J, Mukamel DB, Indridason I. Use of resident-origin data to define nursing home market boundaries. Inquiry. 2002 Spring;39(1):56–66. doi: 10.5034/inquiryjrnl_39.1.56. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Medicare & Medicaid Services. [Accessed March 10, 2011];Medicare Contracting Reform: A/B MAC Jurisdictions. https://www.cms.gov/MedicareContractingReform/05_PartAandPartBMACJurisdictions.asp#TopOfPage.