Abstract
Objectives
The aim of this study was to investigate whether a medium to high degree of total physical activity and indoor physical activity were associated with reduced all-cause and cardiovascular mortality among elderly Korean women.
Methods
A prospective cohort study was done to evaluate the association between physical activity and mortality. The cohort was made up of elderly (≥65 years of age) subjects. Baseline information was collected with a self-administered questionnaire and linked to death certificates retrieved from a database. Cox proportional hazard models were used to estimate the hazard ratios (HRs) with 95% confidence interval (CI) levels.
Results
Women who did not suffer from stroke, cancer, or ischemic heart disease were followed for a median of 8 years (n=5079). A total of 1798 all-cause deaths were recorded, of which 607 (33.8%) were due to cardiovascular disease. The group with the highest level of total physical activity and indoor physical activity was significantly associated to a reduced all-cause mortality (HR, 0.60; 95% CI, 0.51 to 0.71 and HR, 0.58; 95% CI, 0.50 to 0.67, respectively) compared to the group with the lowest level of total physical activity and indoor physical activity. Additionally, the group with the highest level of total physical activity and indoor physical activity was significantly associated to a lower cardiovascular disease mortality (HR, 0.53; 95% CI, 0.40 to 0.71 and HR, 0.51; 95% CI, 0.39 to 0.67, respectively) compared to the group with the lowest level of total physical activity and indoor physical activity.
Conclusions
Our study showed that regular indoor physical activity among elderly Korean women has healthy benefits.
Keywords: Cardiovascular diseases, Exercise, Indoor physical activity, Mortality
INTRODUCTION
The health benefits of regular physical activity on coronary heart disease, stroke, and premature death are well recognized [1,2]. Although many studies have shown the positive effects of physical activity on health [3,4], the associations between domain-specific physical activities (e.g., leisure time, household, transportation, and occupation), and all-cause or cardiovascular disease mortality remains unclear, especially for domestic physical activity [5-8]. Some studies have shown a relationship between domestic physical activity and mortality [5-8] while other studies failed to show any associations to known cardiovascular disease risk factors and cardiovascular diseases [8-10].
The elderly (aged 65 and older) are a fast growing age group in Korea [11]. Although many studies have shown the relationship between physical activity and mortality, relatively few studies have focused on this age group. Particularly, elderly women use important energy for indoor physical activities, such as household activities and activities associated with domestic responsibilities. The prevalence of achieving recommended levels of physical activity was determined in one cross-sectional study, in women aged 60 to 79 from the UK [9]. This study showed that 66.7% of the participants were 'active' at the recommended levels when domestic activities were included while this proportion decreased to 21% after excluding domestic activities. It is important that the health benefits of domestic physical activity is completely understood so elderly women receive accurate recommendations from healthcare providers for other types of activity. Thus, more studies on the independent effects of domestic physical activities of the elderly, especially for older women, are necessary.
The aim of this study was to investigate whether medium or high total physical activity and indoor physical activity are associated with reduced all-cause and cardiovascular disease mortality among elderly Korean women. In addition, we examined the association between mortality and the subtypes of indoor physical activities, such as cleaning house, doing the laundry by hand, and kitchen working.
METHODS
I. Study Population
The Korean Elderly Pharmacoepidemiologic Cohort (KEPEC) was a dynamic cohort made up of a geriatric population aged 65 and older that were beneficiaries of the Korean Medical Insurance Corporation and lived in Busan between 1993 and 1998. A detailed description of the design and some results of the study can be found elsewhere [12]. The data on risk factors and confounders were collected by a self-administered questionnaire mailed in 1996. The questionnaires were sent to 16 524 elderly people in KEPEC. After 3 mailing trials, 9026 participants replied, and the response rate was 54.6%. The cause of death was determined by linking the information to the death certificates obtained from the database of the Korea National Statistical Office.
Of the 6063 eligible female respondents, individuals with incomplete data for exposure (physical activity, n=67), or co-variables (n=581) were sequentially excluded from the analyses. Women with stroke (n=219), cancer (n=99), or ischemic heart disease (n=46) at baseline were also excluded since these conditions can modify physical activity. Thus, 5079 elderly women were available for the final analyses.
Ethical approval was granted by the Seoul National University College of Medicine and Seoul National University Hospital Institutional Review Board (C-1105-090-363).
II. Data Collection
A. Physical activity
The definition of domestic physical activity varies from study to study. Some studies define domestic physical activity as heavy housework and heavy/gardening/do-it-yourself activities [8,10]. However, other studies have defined as household activity or nonexercise physical activity [5,6]. The results could change due to the various definitions; therefore, there needs to be a consensus on the definition for domestic physical activity. We asked participants about their physical activity focusing on their indoor and outdoor activity taking into consideration their age and defined these as 'indoor physical activity' or 'outdoor physical activity'.
Questions on physical activity asked about the frequency of the participants' activities for outdoor activities and indoor activities. Total physical activities were sum of the nine subtype of outdoor activities (e.g., strolling, cycling, mineral spring visiting, running, climbing, playing gate ball, playing golf, playing tennis, etc.) and seven subtype of indoor activities (e.g., gardening, cleaning house, doing the laundry by hand, child care, kitchen working, stretching, etc.) The questionnaire used 5 categorical variables ranging from 'none or rarely' to 'daily' as an answer scale. To classify the level of physical activity, the frequency of daily episodes for each activity was calculated. When we were calculating the frequency score, the answer of 'none or rarely' was regarded as 0 episodes, '1-2 number of frequency a month' as 0.05 episodes, 'once in a week' as 0.14 episodes, 'once in 2-3 days' as 0.4 episodes and 'daily' as 1 episodes. Each subtypes of total and type (outdoor or indoor) of physical activities were summed producing a scoring system of 0-16 (total physical activity), 0-9 (outdoor physical activity) and 0-7 (indoor physical activity). Then, the total physical activities and type (outdoor or indoor) of physical activities were converted into 3 categories. The bottom of the 3 categories was defined by no participation (0 episodes). Excluding the bottom category, the remaining 2 categories were divided by the median of the daily number of episodes for physical activity [8]. The medium category was defined as being equal to or below the median, and the high category was defined as being over the median. The subtypes of the indoor physical activities were converted into 3 categories. The 'none' category had no episodes of indoor physical activity; the 'irregular' category fell between the 'none' and 'regular' category, and the 'regular' category consisted of episodes of various subtypes of indoor physical activities being done on a daily basis.
A study was done to determine the reliability of the questionnaire. Weighted kappa-value for categorical variables and Pearson correlation coefficients for continuous variables were used to measure the reliability. Additionally, the reliability coefficients of most items were over 0.6 in the self-self responses. Some of the items on the physical activities were found to be somewhat less reliable under 0.6 (for example; strolling, 0.33-0.57; gardening, 0.28-0.53). However, the reliability coefficients of 'cleaning house' and 'kitchen working' were over 0.6. In addition, women had a higher validity for items related to physical activities than that of the men [13].
B. Covariates
For the baseline, information on the demographic characteristics of the subjects, self-reported health, self-reported limitations in activity, disease (hypertension and diabetes mellitus), history of drug use, smoking status, drinking status, alcohol consumption, body mass index (BMI), and religious belief was obtained by a self-administered questionnaire. Self-reported health was categorized as bad, average, and good. The smoking and drinking status were classified according to 3 categories: never, ex-, and current. BMI was calculated as weight in kilograms divided by the height in square meters.
III. Outcome
All data were linked to death certificates from the database of the National Statistical Office of Korea. Among thirteen-digit sequence numbers in the social security number, twelve-digits were used to link between questionnaire responses and death certificates. Any subject with errors found in the merging process was excluded them from the study. The cause of death was coded according to the International Classification of Diseases, tenth revision. The main outcome measures were all-cause mortality and cardiovascular disease mortality. Diagnoses for cardiovascular disease death were coded I01-99 from the International Classification of Diseases, tenth revision.
IV. Statistical Analysis
The means and standard deviations or the frequencies and percentages of the general characteristics according to the categories for total physical activity were calculated. ANOVA or Pearson's chi-squared tests were used to explore the associations between the variables when appropriate.
The Cox proportional hazards model was used to investigate the association between physical activity and death due to any cause or death due to cardiovascular disease. The person-months were calculated as the sum of the follow-up time from the date the questionnaire was completed to the date of death or the date of censoring (the end date of the follow-up, 31 December 2004). For the subjects who did not indicate when the questionnaire was completed, the median date of reporting period was entered (30 November 1996). The number of events (all-cause mortality and cardiovascular disease mortality) and person-months were calculated according to the total physical activity and the type (outdoor or indoor) of physical activity. The proportional hazard assumptions for the different levels of total physical activity were examined by inspecting log-minus-log survival plots. Subjects categorized in the 'the bottom level of physical activity' were designated as the reference group in each domain. The following covariates were considered as potential confounders: age, self-reported health, self-reported limitation of activity, hypertension, diabetes mellitus, smoking status, drinking status, BMI, and religion. After univariable analyses, the final model included covariates that correlated with both exposure and outcome variables with p-values less than 0.2. The age adjusted hazard ratios (HRs) and multivariate adjusted hazard ratios (HRs) and their 95% confidence intervals (CIs) were calculated by total and type of physical activity. Tests for linear trends were done by entering the category of physical activity as continuous parameters.
Sensitivity analyses were run after excluding the all-cause mortality that had occurred in the first 2 years of follow-up or after excluding participants who reported their health as 'bad' or reported limited activity when considering the characteristics of the elderly age group.
All tests were two-sided significance levels with a p-value less than 0.05 and all analyses were done with SAS version 9.2 (SAS Inc., Cary, NC, USA).
RESULTS
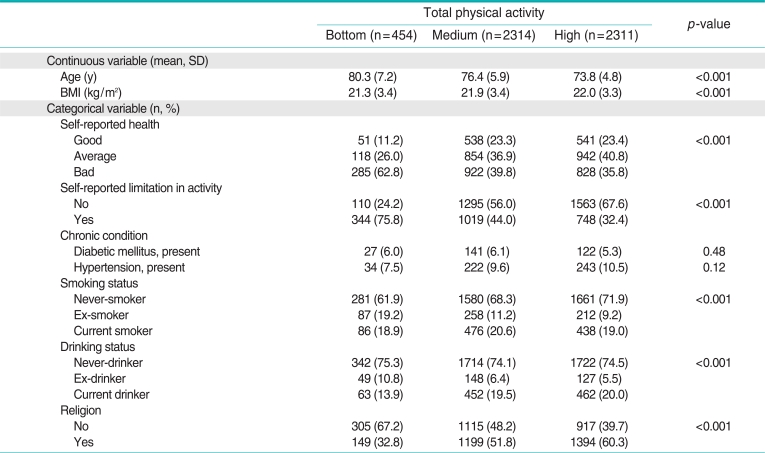
The baseline characteristics of the participants stratified by the total physical activity are presented in Table 1. During a median follow-up of 8 years, 1798 women died, of which 607 (33.8%) deaths were due to cardiovascular diseases. A higher level of total physical activity was associated with younger age, better health (self-reported), less limited activity (self-reported), lower smoking and drinking status, a higher body mass index, and belief in religion. All-cause death and lower cardiovascular disease death were lower for the high category of total physical activity. The subjects' status for hypertension and diabetes was similar in the three groups.
Table 1.
Baseline characteristics among women aged 65 and older in Korean Elderly Pharmacoepidemiologic Cohort
Analyses were performed by using ANOVA for continuous variables and chi-square test for categorical variables.
BMI, body mass index.
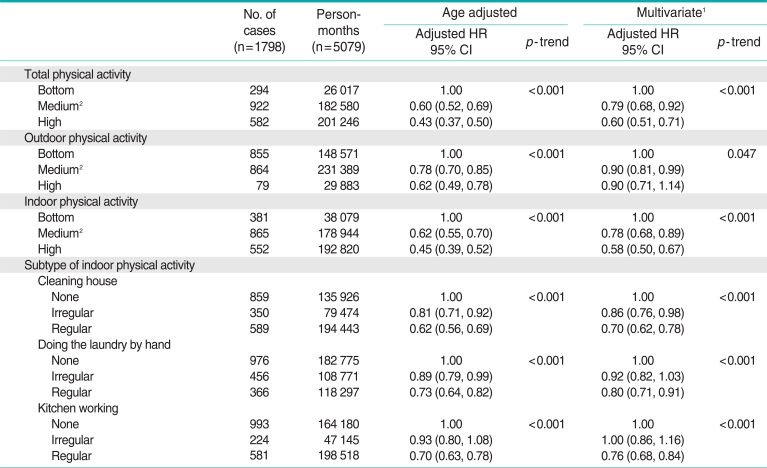
Table 2 presents the age and multivariate adjusted all-cause mortality according to the total physical activity and to the type of physical activity. Compared to the bottom category of physical activity, the high category of total physical activity and indoor physical activity had a significant reduction in risk for all-cause mortality (HR, 0.60; 95% CI, 0.51 to 0.71 and HR, 0.58; 95% CI, 0.50 to 0.67, respectively). Outdoor physical activity was inversely associated with the age adjusted all-cause mortality, but adjustments for covariates attenuated the association. Daily performance of each indoor physical activity such as cleaning house, doing the laundry by hand, and kitchen working was significantly associated with a lower all-cause mortality.
Table 2.
Cox regression models for physical activity levels and all-cause mortality among women aged 65 and older
CI, confidence interval; HR, hazard ratio.
1Adjusted for age, self-reported health, self-reported limitation in activity, smoking status, drinking status, body mass index, religion and other types of physical activity.
2The medium category is defined as equal to or below the median (median of total, outdoor, indoor physical activity was 2.04, 1.00, and 1.94 number of episodes/day, respectively).
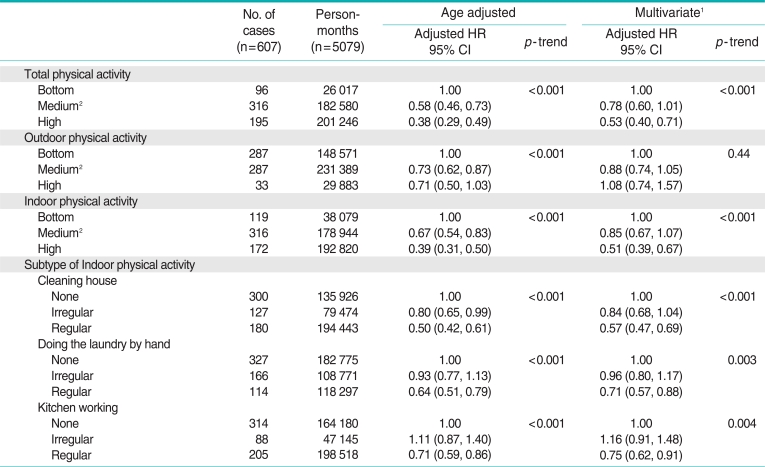
Table 3 presents the age and multivariate adjusted cardiovascular disease mortality according to the total physical activity and to the type of physical activity. The high category of the total physical activity and indoor physical activity were significantly associated with lower cardiovascular disease mortality compared to the bottom category of physical activity (HR, 0.53; 95% CI, 0.40 to 0.71 and HR, 0.51; 95% CI, 0.39 to 0.67, respectively). Outdoor physical activity was not inversely associated with cardiovascular disease mortality. Daily indoor physical activity such as cleaning house, doing the laundry by hand, and kitchen working was significantly associated with lower cardiovascular disease mortality.
Table 3.
Cox regression models for physical activity levels and cardiovascular disease mortality among women aged 65 and older
CI, confidence interval; HR, hazard ratio.
1Adjusted for age, self-reported health, self-reported limitation in activity, hypertension, smoking status, drinking status, body mass index, religion and other types of physical activity.
2The medium category is defined as equal to or below the median (median of total, outdoor, indoor physical activity was 2.04, 1.00, and 1.94 number of episodes/day, respectively).
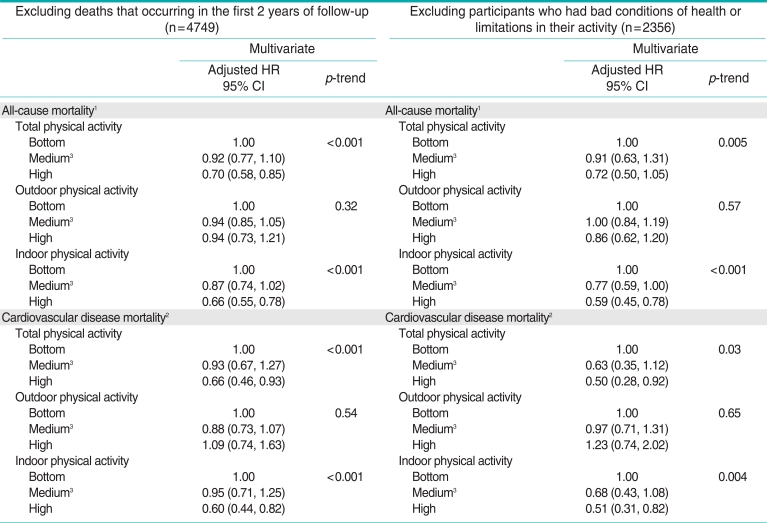
Sensitivity analyses were done with 2 different methods. After excluding the participants with bad health conditions or limited activity, a statistically significant association between physical activity and reduced all-cause and cardiovascular disease mortality risk was found (Table 4). When deaths occurring in the first 2 years of follow-up were excluded, the reported association did not change.
Table 4.
Two different methods for the sensitivity analysis among women aged 65 and older
CI, confidence interval; HR, hazard ratio.
1Adjusted for age, self-reported health, self-reported limitation in activity, smoking status, drinking status, body mass index, religion and other types of physical activity.
2Adjusted for age, self-reported health, self-reported limitation in activity, hypertension, smoking status, drinking status, BMI, religion and other types of physical activity.
3The medium category is defined as equal to or below the median (median of the total, outdoor, and indoor physical activity was 2.04, 1.00, and 1.94 number of episodes/day, respectively).
DISCUSSION
In this study, we observed in women aged 65 or older that both higher levels of total physical activity and indoor physical activity were associated with lower all-cause mortality and cardiovascular disease mortality. This inverse trend was apparent after adjusting for confounders. These associations were similar for each subtype of indoor physical activity.
These findings are in agreement with previous reports that physical activity was associated with lower all-cause mortality. Many cohort studies have shown coincident results about the health-enhancing effects of physical activity [3-6,14]. However, it is difficult to find an independent effect of indoor physical activity among elderly women. A Chinese study found a reduction in the risk of mortality in a comparison of reduced nonexercise activity; the study showed a decrease in mortality risk of approximately 20% to 35% as the nonexercise activity increased [6]. However, the study participants were women aged 40 to 70; the elderly represented only a small proportion of the study. In addition, household activity was analyzed as part of the nonexercise activity; it was not easy to disentangle its single effects. A recent study showed that light household activity was related to lower all-cause mortality; however, the dose-response relationship was not clear [5]. The various domains of physical activity and the different classifications of physical activity levels lead to diverse results. We found that higher levels of physical activities were associated with a greater reduced mortality among the elderly, and the results did not change after adjusting for confounders and for the subgroup analyses.
In previous cross-sectional studies [9,10], domestic physical activity was not associated with cardiovascular disease risk factors such as BMI, high density lipoprotein cholesterol, and resting pulse among women living in England. One study that looked at the independent effects of domestic physical activity on cardiovascular disease events did not show any associations [8]. This Scottish Health Survey showed that intense domestic physical activity was unrelated to risks for cardiovascular disease events after restricting the analysis to those 60 years and older, for whom domestic activity might be important part of physical activity. However, others have found that leisure time physical activity might be associated with decreased cardiovascular disease mortality [15,16]. Likewise, in a study on middle-aged men and women in Finland, moderate and high levels of leisure time and occupational physical activity were associated with reduced cardiovascular disease mortality [4]. Although these were prospective cohort studies, leisure time physical activity was the main exposure variable of interest and the benefit of domestic physical activity was less clear. In addition, we focused specifically on indoor physical activity.
Physical activity had numerous beneficial physiological effects. Physical activity could increase the level of baseline cardiorespiratory fitness, prevent or delay a cardiac event, improve recovery, and slow the rate of decline for physical capacity. The health benefits of physical activity on the metabolic, endocrine, and immune systems were also considerable [17]. Moreover, physical activity positively affects the mental health of individuals [18]. The health benefits of physical activity acts through many pathways, which affect cardiovascular disease. One possible explanation regarding the mechanism for the beneficial effects on cardiovascular disease mortality is that regular physical activity might reduce the blood viscosity, increase the blood flow and therefore, reduce the risk of thrombosis and ischemia. This hypothesis is in accordance with some studies reporting that there are significant inverse effects of physical activity on several hemostatic and inflammatory variables [19,20] and on blood pressure [21]. Another possible hypothesis is that high physical activity might reduce the risk of mortality that is related to adiposity [22]. Long-term exercise may be associated with a decrease in the atherogenic activity of blood mononuclear cells [23].
The association between 'walking or cycling to and from work', which was usually classified as domestic physical activity in other studies, and cardiovascular disease mortality was not statistically significant after adjusting for other domains of physical activity in the Finland study [4]. It is less clear what contributions domestic activity has on cardiovascular disease mortality among the elderly. In contrast to earlier studies, our study found that higher levels of indoor physical activity were associated with reduced cardiovascular disease mortality among elderly women. Higher levels of indoor physical activity lowered blood pressure and reduced blood viscosity based on the hemostatic variables. Additionally, this complex effect reduced cardiovascular disease mortality in the long term.
One of the strengths of this study was that we controlled for confounders. The evaluation of important covariates at baseline allowed for the adjustment of risk factors related to the all-cause and cardiovascular disease mortality. Furthermore, 2 different domains of physical activity were assessed to investigate their independent effects.
Besides these strengths, this study has certain limitations. We used self-reported information on recent physical activity. Self-reporting measures have an inherent measurement error. A systematic reporting error and misclassification due to proxy responses, no responses, and missing variables may influence our results. Moreover, there could be potential misclassifications due to a lower validity for the measure of total physical activity and the type of physical activity. We also acknowledge that this study includes our inability to rule out the possible effects of unmeasured confounders. To minimize the potential bias, we excluded from the analyses women who reported major diseases at baseline. It is difficult to establish whether poor health is a consequence of a low level physical activity. Considering reverse causation, we included major health conditions in our model. In addition, we had consistent results from the sensitivity analysis using participants with good health. Physical activity was assessed only at baseline, and this may have affected the results. A decrease in the level of physical activity could be caused by age, socioeconomic status, and disease, and this change might dilute the association between physical activity and mortality approximately 24% to 59% [24].
In this large, prospective study, higher levels of total physical activity and indoor physical activity in women were associated with lower all-cause mortality and cardiovascular disease mortality. These findings support evidence that physical activity is beneficial for elderly women. Further studies are needed to establish the health benefits of each type of indoor physical activity so that a specific group-based recommendation can be provided based on solid evidence.
Footnotes
The authors have no conflicts of interest with the material presented in this paper.
This article is available at http://jpmph.org/.
References
- 1.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 2.Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morgan K, Clarke D. Customary physical activity and survival in later life: a study in Nottingham, UK. J Epidemiol Community Health. 1997;51(5):490–493. doi: 10.1136/jech.51.5.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barengo NC, Hu G, Lakka TA, Pekkarinen H, Nissinen A, Tuomilehto J. Low physical activity as a predictor for total and cardiovascular disease mortality in middle-aged men and women in Finland. Eur Heart J. 2004;25(24):2204–2211. doi: 10.1016/j.ehj.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 5.Autenrieth CS, Baumert J, Baumeister SE, Fischer B, Peters A, Doring A, et al. Association between domains of physical activity and all-cause, cardiovascular and cancer mortality. Eur J Epidemiol. 2011;26(2):91–99. doi: 10.1007/s10654-010-9517-6. [DOI] [PubMed] [Google Scholar]
- 6.Matthews CE, Jurj AL, Shu XO, Li HL, Yang G, Li Q, et al. Influence of exercise, walking, cycling, and overall nonexercise physical activity on mortality in Chinese women. Am J Epidemiol. 2007;165(12):1343–1350. doi: 10.1093/aje/kwm088. [DOI] [PubMed] [Google Scholar]
- 7.Woodcock J, Franco OH, Orsini N, Roberts I. Non-vigorous physical activity and all-cause mortality: systematic review and meta-analysis of cohort studies. Int J Epidemiol. 2011;40(1):121–138. doi: 10.1093/ije/dyq104. [DOI] [PubMed] [Google Scholar]
- 8.Stamatakis E, Hamer M, Lawlor DA. Physical activity, mortality, and cardiovascular disease: is domestic physical activity beneficial? The Scottish Health Survey: 1995, 1998, and 2003. Am J Epidemiol. 2009;169(10):1191–1200. doi: 10.1093/aje/kwp042. [DOI] [PubMed] [Google Scholar]
- 9.Lawlor DA, Taylor M, Bedford C, Ebrahim S. Is housework good for health? Levels of physical activity and factors associated with activity in elderly women. Results from the British Women's Heart and Health Study. J Epidemiol Community Health. 2002;56(6):473–478. doi: 10.1136/jech.56.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stamatakis E, Hillsdon M, Primatesta P. Domestic physical activity in relationship to multiple CVD risk factors. Am J Prev Med. 2007;32(4):320–327. doi: 10.1016/j.amepre.2006.12.020. [DOI] [PubMed] [Google Scholar]
- 11.Korea National Statistical Office. Population projections for Korea: 2005-2050. [cited 2011 Jul 31]. Available from: http://lib1.kostat.go.kr/search/media/img/CAT000000044245?metsno=000000001741&fileid=M000000001741_FILE000002. (Korean)
- 12.Park BJ, Cho YK, Kim SA. Construction of the Korea Elderly Pharmacoepidemiologic Cohort: drug utilization review of cephalosporins in geriatric inpatients. Pharmacoepidemiol Drug Saf. 2001;10(6):487–492. doi: 10.1002/pds.665. [DOI] [PubMed] [Google Scholar]
- 13.Park BJ, Kim DS, Koo HW, Bae JM. Reliability and validity study of a life style questionnaire for elderly people. Korean J Prev Med. 1998;31(1):49–58. (Korean) [Google Scholar]
- 14.Hrobonova E, Breeze E, Fletcher AE. Higher levels and intensity of physical activity are associated with reduced mortality among community dwelling older people. J Aging Res. 2011. 10.4061/2011/651931. [DOI] [PMC free article] [PubMed]
- 15.Haapanen N, Miilunpalo S, Vuori I, Oja P, Pasanen M. Characteristics of leisure time physical activity associated with decreased risk of premature all-cause and cardiovascular disease mortality in middle-aged men. Am J Epidemiol. 1996;143(9):870–880. doi: 10.1093/oxfordjournals.aje.a008830. [DOI] [PubMed] [Google Scholar]
- 16.Yu S, Yarnell JW, Sweetnam PM, Murray L Caerphilly study. What level of physical activity protects against premature cardiovascular death? The Caerphilly study. Heart. 2003;89(5):502–506. doi: 10.1136/heart.89.5.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Physical activity and health: a report of the surgeon general. U.S. Department of Health and Human Services. [cited 2011 Dec 9]. Available from: http://www.cdc.gov/nccdphp/sgr/pdf/sgrfull.pdf.
- 18.Paluska SA, Schwenk TL. Physical activity and mental health: current concepts. Sports Med. 2000;29(3):167–180. doi: 10.2165/00007256-200029030-00003. [DOI] [PubMed] [Google Scholar]
- 19.Wannamethee SG, Lowe GD, Whincup PH, Rumley A, Walker M, Lennon L. Physical activity and hemostatic and inflammatory variables in elderly men. Circulation. 2002;105(15):1785–1790. doi: 10.1161/hc1502.107117. [DOI] [PubMed] [Google Scholar]
- 20.Geffken DF, Cushman M, Burke GL, Polak JF, Sakkinen PA, Tracy RP. Association between physical activity and markers of inflammation in a healthy elderly population. Am J Epidemiol. 2001;153(3):242–250. doi: 10.1093/aje/153.3.242. [DOI] [PubMed] [Google Scholar]
- 21.Vatten LJ, Nilsen TI, Holmen J. Combined effect of blood pressure and physical activity on cardiovascular mortality. J Hypertens. 2006;24(10):1939–1946. doi: 10.1097/01.hjh.0000244941.49793.f9. [DOI] [PubMed] [Google Scholar]
- 22.Koster A, Harris TB, Moore SC, Schatzkin A, Hollenbeck AR, van Eijk JT, et al. Joint associations of adiposity and physical activity with mortality: the National Institutes of Health-AARP Diet and Health Study. Am J Epidemiol. 2009;169(11):1344–1351. doi: 10.1093/aje/kwp053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith JK, Dykes R, Douglas JE, Krishnaswamy G, Berk S. Long-term exercise and atherogenic activity of blood mononuclear cells in persons at risk of developing ischemic heart disease. JAMA. 1999;281(18):1722–1727. doi: 10.1001/jama.281.18.1722. [DOI] [PubMed] [Google Scholar]
- 24.Andersen LB. Relative risk of mortality in the physically inactive is underestimated because of real changes in exposure level during follow-up. Am J Epidemiol. 2004;160(2):189–195. doi: 10.1093/aje/kwh195. [DOI] [PubMed] [Google Scholar]