Abstract
Purpose
Leiomyosarcoma (LMS) of the inferior vena cava (IVC) is a rare primary soft tissue sarcoma. Few reports have detailed the tumor features, treatment strategies, and long-term outcomes in IVC LMS patients. The present report describes the treatment and long-term outcomes of six patients with IVC LMS.
Methods
We reviewed six consecutive cases of IVC LMS treated at the University of Ulsan College of Medicine, Asan Medical Center from August 1998 to June 2010.
Results
The patients comprised five females and one male, and had a median age of 44 years (range, 25 to 64 years). All tumors were suprarenal. The tumors were located between the hepatic and renal veins (i.e., middle segment; n = 5 [83%]), or above the hepatic veins (i.e., upper segment; n = 1 [17%]). Prosthetic IVC replacement using polytetrafluoroethylene grafts was performed in five patients, and the remaining patient underwent only tumor resection and IVC ligation. There were no intraoperative or postoperative deaths. The mean tumor size was 9.3 cm (range, 5 to 20 cm), and five of the six tumors were high grade. The mean follow-up period was 80 months (range, 6 to 118 months). The median survival period was 94 months. Recurrence occurred in all patients. Distant recurrence resulted in three patients undergoing lung resection and three patients undergoing thigh muscle resection.
Conclusion
IVC LMS is a rare but serious disease. Although surgical resection combined with chemoradiotherapy was not completely curative, it resulted in long-term patient survival, even in patients with advanced tumors.
Keywords: Leiomyosacrcoma, Adjuvant therapy, Inferior vena cava
INTRODUCTION
Leiomyosarcoma of the inferior vena cava (IVC) can be a fatal disease. Although leiomyosarcoma is the most common primary malignancy of the IVC, it is a rare condition, with fewer than 300 cases reported, and most studies are limited to single case reports or compilations of case series. As a result, there is inadequate information regarding IVC leiomyosarcoma prognostic factors due to the lack of data regarding tumor characteristics, treatment strategies and long-term outcomes.
En bloc tumor resection is the only treatment option that can provide long-term survival for IVC leiomyosarcoma patients. According to the international register established by Mingoli et al. [1], the 5- and 10-year actuarial malignancy-free survival rates after wide surgical resection are very low. Debate continues regarding the optimal management of the IVC after tumor resection, with primary repair, ligation and IVC reconstruction all having been utilized with varying success. The efficacy of adjuvant therapy (chemotherapy or radiotherapy) has not been established. In addition, no study has clearly addressed the management of recurrent disease.
The present study describes the treatment of six IVC leiomyosarcoma patients in our center. All patients underwent surgical resection and adjuvant therapy. Patients were followed for up to 118 months. We analyzed treatment regimens, tumor pathology, recurrence and outcomes in these patients.
METHODS
The present study reviewed six cases of IVC leiomyosarcoma treated at the Asan Medical Center between August 1999 and June 2010. Clinical and pathologic data, surgical management, and outcomes were assessed. The study was approved by our institutional review board.
IVC segments were defined as follows: upper segment = from the right atrium to the hepatic veins, middle segment = below the hepatic veins to the renal veins, and lower segment = below the renal veins to the bifurcation of the IVC. Symptom assessment was based on a review of the relevant medical records. Operative notes and pathology reports were used to collect data regarding the tumor, the organs resected en bloc, and post-resection IVC management.
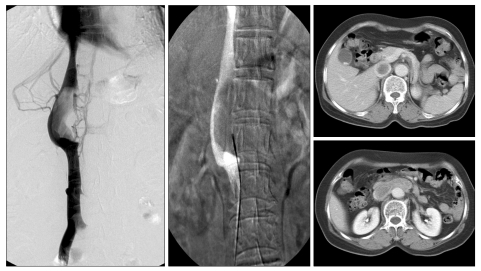
All patients underwent contrast-enhanced computed tomography (CT) scans of the abdomen and pelvis to assess tumor resectability. The degree of caval obstruction and development of collateral vein circulation was evaluated using cavography in four patients. Venographic biopsies were performed in four patients (Fig. 1).
Fig. 1.
Preoperative leiomyosarcoma (LMS) evaluation. LMS were preoperatively assessed using venography computed tomography scan, and venographic biopsy.
Patient survival data were obtained from medical records. Overall survival rates were calculated from the date of surgery to the date of death or last contact. Disease-free survival rates were calculated from the date of the first operation to the date of first recurrence. Disease-specific survival was estimated using the Kaplan-Meier life table.
Case 1
This patient is a female at her age 55. She came to the hospital with a repetitive abdominal pain having started three weeks ago. She did not have any underlying disease. In an abdominal ultrasonography at our hospital, a 7-cm abdomen-pelvis tumor was found, and it was thought to originate from the IVC.
The patient got the resection of her IVC and left renal vein. Then using polytetrafluoroethylene (PTFE), an IVC replacement was operated, and an interposition was carried out on the left renal vein to reconstruct it, and there was no resection of another accompanying organ.
The tumor was located in the middle segment, which was 7 cm. Pathologically the resection margin was secured to be negative. In a pathologic report, it was at a histological high grade; however, there was no necrosis, and the mitotic rate was good (<3/10 HPF).
After the surgery, 5-cycle chemotherapy was carried out with adjuvant therapy, and the regimen of chemotherapy was a combination of dacarbazine, doxorubicin and cyclophosphamide.
In the 76th month after the first surgery, a metastatic recurrence took place on the right lung, so a right middle lobectomy was performed, and a year after, it recurred on the right thigh muscle, so a wide excision, and chemotherapy and radiotherapy with isofamide/cisplatin were performed again and then the patient survives stably without any special relapse until now.
Case 2
This patient is a female at her age 25. She visited another general hospital with an abdominal pain for four months and was diagnosed malignancy through a biopsy, and came to our hospital for a further evaluation and treatment. The size of the tumor was 9 cm, located in the middle segment of IVC. Since the IVC and left renal vein were involved, the IVC and left renal vein got resection during surgery. Then the IVC was replaced using a PTFE graft; however, since the left renal vein has sufficient collateral flow toward the gonadal vein, a ligation only was carried out. Negative resection margin was secured pathologically. After the surgery, 6-cycle adjuvant chemotherapy was performed using epirubicin, ifosfamide and dacarbazine.
Eighteen months later, multiple recurrences were found in the patient's right lung, kidney, and retroperitoneum. After two cycles of chemotherapy with cisplatin and ifosmide, and 6-cycle chemotherapy with the regimen of a combination of dacarbazine, doxorubicin, cyclophosphamide, and vincristine sulfate, a surgery to remove the recurrent tumor in the retroperitoneum was performed. For 30 days after the second surgery, radiotherapy was carried out at a total 5,400 cGY; however, she died of multi-organ metastasis in the 36th month after the first surgery.
Case 3
This patient is a female at her age 63. She came in presenting with chronic pain in her right abdomen. In a CT scan in our hospital, a 8 cm tumor was found. This tumor was located at the junction between the right renal vein and the IVC. After an excision of the IVC and right renal vein, an IVC replacement was carried out using a PTFE graft, and an interposition with PTFE graft was performed to reconstruct the right renal vein. During the surgery, there was invasion into the liver's caudate lobe, so accompanying resection was carried out.
After the surgery, radiotherapy with a dose of 5,580 cGY was operated during 31 days while adjuvant chemotherapy was not carried out.
Forty-seven months after the surgery, wedge resection was performed for the right lung metastasis and three months later, the left lung metastasis was found again, so lobectomy of the left lower lobe was carried out. Then follow-up failed, but 97 months after the surgery, it was confirmed finally that she died of multiple metastasis in another hospital.
Case 4
This patient is a female at her age 57. She came to the hospital with her epigastric pain starting several months ago. A CT scan was shot and a mass which is considered starting from the IVC was found so a surgery was performed. At the time, the mass was 5 cm, located in the middle segment of the IVC, and the left renal vein was involved; however, there was no infiltration into another organ. After the resection of the IVC and the left renal vein, IVC replacement and interposition of the left renal vein were operated. However, a pathologic negative margin was not secured in a permanent report while the IVC's naked-eye resection margin was secured. Adjuvant radiotherapy was performed for 29 days with a total dose of 5,300 cGY while chemotherapy was not carried out.
Ninety-one months after the surgery, wide excision was carried out for the recurrence in the left thigh muscle, radiotherapy was operated again, and since then, she has survived stably without any evidence of another relapse.
Case 5
This patient is a male at his age 36. He came to another hospital presenting with the back and abdominal pain, and low leg edema having started 5 months ago, and was transferred to our hospital with leiomyosarcoma in the IVC presented on a CT scan. In the operative opinion, the mass was located in the middle segment completely blocking the lumen. Because of the leiomyosarcoma showing an extra-luminal growing in the IVC origin, there was involvement of both renal veins, without any infiltration to another organ. Since the IVC was at the status of complete obstruction, no replacement was made, and as the renal veins on both sides were also at the status of complete obstruction, the surgery was completed without any special reconstruction. Immediately after the surgery, there was neither complication except a temporary leg edema nor abnormality in the renal function. However, securing a pathological tumor free margin at the upper and lower margins failed.
After the surgery, adjuvant radiotherapy was operated with a dose of 5,640 cGY during 31 days while no chemotherapy was performed. Five months after the surgery, an intra-abdominal peritoneal single mass was found and excised. With a definite diagnosis as recurring mass, radiotherapy was carried out again at the resection site. Ten months after the first surgery a small nodular metastasis was found in the right lower lung, and needle biopsy was performed and it got a definite diagnosis as metastatic nodule. However, the patient refused an operation, so 6-cycle of chemotherapy with a combination of cisplatin, ifosfamide and etoposide were performed and it got a complete remission. However, in the 59th months after the first surgery, a left buttock mass was detected so radiotherapy was carried out again. Five months later, on the CT scan and magnetic resonance imaging scan in a follow-up observation, a nodule was found. It was thought to be a metastasis in the lung and lumbar spine. However, his reaction to radiotherapy was poor and it was considered a multiple small metastasis, so no additional treatment was performed and currently a follow-up observation is in progress. For about 2 years, he has survived at a stationary status without any significant aggravation.
Case 6
The patient is a female at her age 30. She had had upper abdominal pain since 5 months before she came to our hospital and had come to another hospital as she felt leg edema and abdominal mass since 1 month ago. After having been diagnosed of the IVC tumor on a CT scan in the hospital, she was transferred to ours. During the surgery, there was involvement from the iliac bifurcation to the supra-hepatic IVC, and both renal veins also were invaded. Since there was direct invasion into the left hepatic vein, ex situ resection was carried out in the IVC along with the whole liver. After that, hepatic vein venoplasty was carried out through a bench procedure, and then the IVC was replaced with a PTFE graft and auto-transplantation was carried out in the liver. Both renal veins were not reconstructed and were left the status of ligation. Immediately after the surgery, there was no complication related to the surgery, and the renal function and the liver function were maintained without any problem. Adjuvant therapy was not carried out.
Three months after the surgery, a multiple liver metastases were found, and later 7-cycle chemotherapy was carried out with doxorubicin and ifosfamide, and since then as chemotherapy was carried out with several clinical trial medications, she has survived at a stationary status.
RESULTS
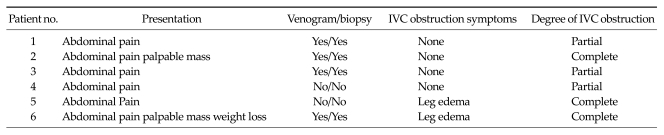
The six cases comprised five females and one male. The median patient age was 44 years (range, 25 to 64 years). The initial presenting symptoms included abdominal pain (n = 6, 100%), weight loss (n = 2, 33%), lower extremity edema (n = 2, 33%) and palpable mass (n = 1, 16%). All tumors were located above the renal vein, with five (83%) being in the middle segment, and one (17%) in the upper segment. That latter case involved the suprahepatic IVC and extended to the bilateral common iliac vein (Tables 1, 2). Complete gross resection of the tumor was undertaken in all six cases. For the upper segment tumor, the whole liver was removed and the tumor then excised ex situ. The resected liver was then auto-transplanted using Bench venoplasty with an autologous vein graft, and the IVC was replaced with a PTFE prosthetic graft (Fig. 2). For middle segment tumors, leiomyosarcomas were resected in situ and PTFE grafts were used for prosthetic IVC replacement. We didn't use anti-coagulative agent or anti-platelet agent routinely. All PTFE graft has been keep patency during follow-up period.
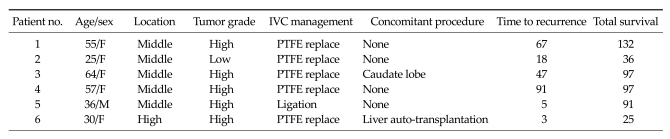
Table 1.
Patient characteristics
PTFE, polytetrafluoroethylene.
Table 2.
Clinical findings at presentation
Fig. 2.
A large leiomyosarcoma in the upper segment with middle hepatic vein involvement. The patient underwent ex situ excision with the whole liver and auto-transplantation after venoplasty.
One case showed that IVC was complete obstruction at the suprarenal level. That patient showed hemodynamic stability and maintenance of urine output during IVC clamping, had IVC total occlusion in association with extensive long-segment disease, and well-developed venous collaterals. That patient had normal renal function both pre- and postoperatively.
At least one renal vein was ligated in three patients, both renal veins were ligated in two patients and one renal vein was ligated in one patient. None of those patients showed postoperative renal impairment.
Organ en bloc removal with the primary tumor was performed in 2 (33%) patients, comprising a partial hepatectomy in one patient and a whole liver ex situ excision followed by auto-transplantation in one patient.
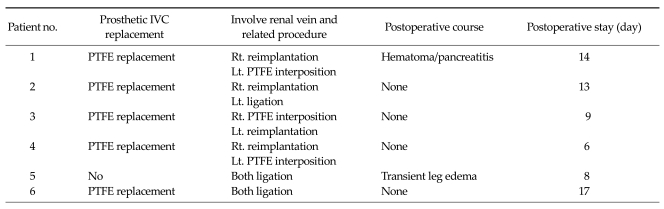
The mean length of hospital stay was 11 days. There were no intraoperative or postoperative deaths. Postoperative morbidity comprised transitional leg edema in a patient who did not undergo IVC replacement, and hematoma and mild pancreatitis in another patient (Table 3).
Table 3.
Surgical procedures and outcomes
IVC, inferior vena cava; PTFE, polytetrafluoroethylene; Rt, right; Lt, left.
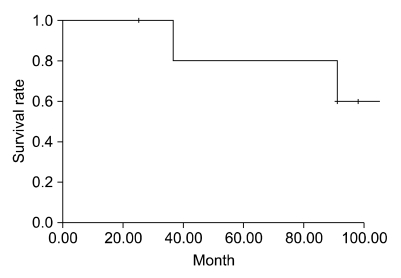
The mean tumor size was 9.3 cm (range, 5 to 20 cm). Three tumors (50%) grew endoluminally, and the other three grew exoluminally. Histological examination showed that there were five high-grade tumors and one low-grade tumor. Four (66%) patients had negative microscopic margins at initial resection. Two cases showed evidence of the tumor invading adjacent structures extraluminally. Tumor necrosis was present in 5 (84%) tumors. Measurement of mitotic rates showed that one tumor was at or below 5/10 HPF, four tumors were above 5/10 HPF and at or below 20/10 HPF, and one tumor was above 20/10 HPF. The tumor of the longest-surviving patient (144 months) had a unique combination of characteristics showing no necrosis and a low mitotic rate (3/10 HPF) (Table 4). The mean follow-up period was 80 months (range, 6 to 118 months). After resection, all patients developed recurrence, and the mean recurrence time was 38 months. And the median survival period was 94 months (range, 25 to 144 months). All patients received adjuvant therapy, comprising chemotherapy for one patient, radiotherapy for two patients, and chemoradiotherapy for three patients. The 3- and 5-year survival rates were 80% and 60%, respectively (Fig. 3).
Table 4.
Pathology findings
Fig. 3.
Overall survival rate. The 3- and 5-year survival rates were 80% and 60%, respectively.
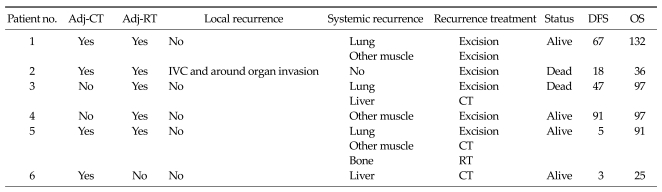
There were a total of 15 recurrences in the six patients. Local recurrence occurred in one patient (16%) at 18 months. Distant recurrence occurred in six patients (100%) at a median of 40 months. The lung was the most common site of distant recurrence (five recurrences in three patients), followed by the thigh muscle (four recurrences in two patients). Surgery was performed for eight recurrences in five patients. One lung recurrence was controlled using chemotherapy, and one buttock muscle recurrence was resolved using radiotherapy. Two patients died at 36 and 97 months after the first operation, respectively, due to multiorgan metastasis (Table 5).
Table 5.
Summary of adjuvant therapies and recurrences
Adj, adjuvant; CT, chemotherapy; RT, radiotherapy; IVC, inferior vena cava; DFS, disease free survival; OS, overall survival.
DISCUSSION
Two thirds of patients with leiomyosarcoma of the IVC present with localized disease amenable to curative resection [2]. In the present study, five of the six patients were female, and all patients had abdominal pain as a presenting symptom. These findings are consistent with those described in the Mingoli register which include female predilection, mean age in the sixth decade, abdominal pain being a frequent presenting symptom, inconsistent association with edema of the lower extremities, and potential for development of Budd-Chiari syndrome and intracardiac extension [1]. A diagnosis of IVC leiomyosarcoma can be delayed since the tumors are slow-growing and remain confined to the vessel wall in the early stages and hence can stay asymptomatic for a long time. Discovery is made incidentally in 10.5% of patients and at autopsy in 33% [3].
The most important prognostic indicator for IVC leiomyosarcoma patients is surgical resection with negative margins, which confers a 33 to 68% 5-year survival rate [4-7]. The present study found that patients with negative margins had a median survival of 86 months. These findings support the view that aggressive resection with negative margins should be the goal of therapy for those without widespread metastases and who are acceptable surgical candidates.
There is little information regarding the efficacy of neoadjuvant and adjuvant therapy for IVC leiomyosarcoma, and there is no consensus regarding the optimal treatment strategy [6]. However, we believe that in the absence of a negative margin after resection, survival can be improved with the use of appropriate chemotherapy or radiotherapy. The 1999 report from University of California quoted a 5-year survival of 53 percent. Those patients received adjuvant radiation therapy, which may have improved outcomes [4]. In the present study, negative margins were not obtained in two patients. However, those patients remain alive at 97 and 91 months postoperatively. Our findings demonstrate that despite high rates of disease recurrence, long-term survival can be achieved in IVC leiomyosarcoma patients.
Surgical procedures for IVC leiomyosarcoma extirpation are frequently complex due to the retro hepatic location and close proximity to major branches of the IVC. Involvement of the renal vein confluence by the tumor may necessitate nephrectomy, kidney auto-transplantation or re-attachment of the tumor-free renal vein stump to the IVC [8]. In the current study, we performed renal vein reimplantation on one side and renal vein PTFE graft interposition on the opposite side in three patients, ligation of both renal veins in two patients, and vein reimplantation on one side and ligation of the other renal vein in one patient. No patient experienced renal impairment.
IVC reconstruction options include placement of a synthetic interposition graft, primary repair, or patch repair of the IVC. The proponents of the ligation technique suggest that extensive development of the collateral vessels obviates the need for IVC reconstruction, and that patients with stable renal function in the presence of complete IVC thrombosis tolerate ligation well [9]. Because leiomyosarcoma usually causes gradual obstruction of the IVC lumen and formation of collateral veins, IVC resection can usually be performed under stable hemodynamic conditions [10]. In our series, IVC reconstruction with PTFE was performed in five of the six patients. The remaining patient had complete IVC obstruction, dual renal vein involvement and good preoperative renal function. Postoperatively, that patient had transient leg edema but no other complications.
One present patient was a 30-year-old female with a tumor located suprahepatic to both iliac veins and involving the middle hepatic vein. For this case, we performed ex situ en bloc resection IVC with the whole liver, and then hepatic vein angioplasty in a bench procedure with the great saphenous vein to make a common channel, and reimplantation to the PTFE graft. This patient showed good postoperative recovery, and no hepatic dysfunction. However, tumor recurrence as multiple hepatic metastases was observed at postoperative three months. To date, she continues to be treated using chemotherapy, and is currently in a stable state.
Debulking may be the only means of tumor control for locally advanced primary caval malignancy [3]. This approach may not only prevent death from liver failure by hepatic vein obstruction, but also achieve long-term survival without venous sequelae. Recent studies indicate aggressive surgical management and adjuvant chemoradiotherapy is the best treatment for IVC leiomyosarcoma [4].
Few publications discuss the management of recurrent IVC leiomyosarcoma. As a result, a standardized approach has not been established. Currently, surgery is the only option offered for recurrent disease if associated with minimal morbidity, even for isolated metastatic disease. The most commonly performed procedure is local excision for retroperitoneal recurrence and metastasectomy for lung recurrence [6,11-16]. Adjuvant chemotherapy based on doxorubicin or a combination of doxorubicin and ifosfamide may extend the time to recurrence and increase overall survival in sarcoma patients [17,18]. In the current study, there were five incidents of lung metastasis in three patients, and three incidences of thigh muscle metastasis in two patients. One lung metastasis was controlled by doxorubicin plus ifosfamide chemotherapy, and another was treated using lung resection. All thigh muscular metastases involved single sites and were treated using simple resection. One buttock muscular metastasis was controlled using radiotherapy. Although all six patients experienced recurrence, four patients remain alive for an average of 80 months. We believe appropriate adjuvant chemotherapy or radiotherapy can be effective in disease control.
Although tumor grade, size, and location are well-established prognostic factors for sarcomas in general, their predictive value for IVC leiomyosarcoma remains to be established. Positive surgical margins were predictive of worse survival in the series reported by Hines et al. [4]. Pathology findings relating to tumor grade, mitotic rate, and tumor size have been suggested as possible prognostic factors [6,19]. In the present study, five of the six tumors were high-grade, yet long-term survival was achieved in most of those patients. However, the small number of cases in our study prevented meaningful statistical analysis regarding prognostic factors.
In the longest-surviving patient in the current study (144 months), the tumor had the unique pathology combination of no necrosis and a very low mitotic rate (3/10 HPF). Almost all other tumors had a mitotic rate higher than 10/10 HPF and necrosis. Another patient in the present study had a tumor that showed very poor pathology features: a positive resection margin, high grade mitotic rate, >70% necrosis, extraluminal growth pattern, and anaplastic change associated with recurrent disease. However, to our surprise, that patient remains alive at postoperative 91 months. These findings indicate that clinicians should be cautious about using pathology factors as predictors of survival in IVC leiomyosarcoma patients.
In conclusion, the present study reported on the use of aggressive surgical resection and adjuvant chemoradiotherapy for IVC leiomyosarcoma. Although recurrence occurred in every case, long-term survival was achieved, even when tumors showed poor pathology features.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Mingoli A, Cavallaro A, Sapienza P, Di Marzo L, Feldhaus RJ, Cavallari N. International registry of inferior vena cava leiomyosarcoma: analysis of a world series on 218 patients. Anticancer Res. 1996;16(5B):3201–3205. [PubMed] [Google Scholar]
- 2.Cho SW, Marsh JW, Geller DA, Holtzman M, Zeh H, 3rd, Bartlett DL, et al. Surgical management of leiomyosarcoma of the inferior vena cava. J Gastrointest Surg. 2008;12:2141–2148. doi: 10.1007/s11605-008-0700-y. [DOI] [PubMed] [Google Scholar]
- 3.Kulaylat MN, Karakousis CP, Doerr RJ, Karamanoukian HL, O'Brien J, Peer R. Leiomyosarcoma of the inferior vena cava: a clinicopathologic review and report of three cases. J Surg Oncol. 1997;65:205–217. doi: 10.1002/(sici)1096-9098(199707)65:3<205::aid-jso11>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 4.Hines OJ, Nelson S, Quinones-Baldrich WJ, Eilber FR. Leiomyosarcoma of the inferior vena cava: prognosis and comparison with leiomyosarcoma of other anatomic sites. Cancer. 1999;85:1077–1083. [PubMed] [Google Scholar]
- 5.Dew J, Hansen K, Hammon J, McCoy T, Levine EA, Shen P. Leiomyosarcoma of the inferior vena cava: surgical management and clinical results. Am Surg. 2005;71:497–501. doi: 10.1177/000313480507100609. [DOI] [PubMed] [Google Scholar]
- 6.Ito H, Hornick JL, Bertagnolli MM, George S, Morgan JA, Baldini EH, et al. Leiomyosarcoma of the inferior vena cava: survival after aggressive management. Ann Surg Oncol. 2007;14:3534–3541. doi: 10.1245/s10434-007-9552-z. [DOI] [PubMed] [Google Scholar]
- 7.Kieffer E, Alaoui M, Piette JC, Cacoub P, Chiche L. Leiomyosarcoma of the inferior vena cava: experience in 22 cases. Ann Surg. 2006;244:289–295. doi: 10.1097/01.sla.0000229964.71743.db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraybill WG, Callery MP, Heiken JP, Flye MW. Radical resection of tumors of the inferior vena cava with vascular reconstruction and kidney autotransplantation. Surgery. 1997;121:31–36. doi: 10.1016/s0039-6060(97)90179-3. [DOI] [PubMed] [Google Scholar]
- 9.Hollenbeck ST, Grobmyer SR, Kent KC, Brennan MF. Surgical treatment and outcomes of patients with primary inferior vena cava leiomyosarcoma. J Am Coll Surg. 2003;197:575–579. doi: 10.1016/S1072-7515(03)00433-2. [DOI] [PubMed] [Google Scholar]
- 10.Hardwigsen J, Balandraud P, Ananian P, Saïsse J, Le Treut YP. Leiomyosarcoma of the retrohepatic portion of the inferior vena cava: clinical presentation and surgical management in five patients. J Am Coll Surg. 2005;200:57–63. doi: 10.1016/j.jamcollsurg.2004.09.035. [DOI] [PubMed] [Google Scholar]
- 11.Varela-Duran J, Oliva H, Rosai J. Vascular leiomyosarcoma: the malignant counterpart of vascular leiomyoma. Cancer. 1979;44:1684–1691. doi: 10.1002/1097-0142(197911)44:5<1684::aid-cncr2820440523>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 12.Dzsinich C, Gloviczki P, van Heerden JA, Nagorney DM, Pairolero PC, Johnson CM, et al. Primary venous leiomyosarcoma: a rare but lethal disease. J Vasc Surg. 1992;15:595–603. [PubMed] [Google Scholar]
- 13.Beiles CB, Jones RM, Fell G. Recurrent leiomyosarcoma of the inferior vena cava. Aust N Z J Surg. 1997;67:67–68. doi: 10.1111/j.1445-2197.1997.tb01903.x. [DOI] [PubMed] [Google Scholar]
- 14.Demers ML, Curley SA, Romsdahl MM. Inferior vena cava leiomyosarcoma. J Surg Oncol. 1992;51:89–92. doi: 10.1002/jso.2930510205. [DOI] [PubMed] [Google Scholar]
- 15.Kasano Y, Tanimura H, Kumada K, Taniguchi K, Takifuji K, Ohnishi H, et al. Resectable leiomyosarcoma of inferior vena cava extended into the right atrium with the use of cardiopulmonary bypass and graft replacement. Surgery. 1995;117:473–475. doi: 10.1016/s0039-6060(05)80070-4. [DOI] [PubMed] [Google Scholar]
- 16.Yuzer Y, Zeytunlu M, Makay O, Sozbilen M, Yuce G. Leiomyosarcoma of the inferior vena cava: report of a case. Surg Today. 2004;34:370–373. doi: 10.1007/s00595-003-2706-0. [DOI] [PubMed] [Google Scholar]
- 17.Pervaiz N, Colterjohn N, Farrokhyar F, Tozer R, Figueredo A, Ghert M. A systematic meta-analysis of randomized controlled trials of adjuvant chemotherapy for localized resectable soft-tissue sarcoma. Cancer. 2008;113:573–581. doi: 10.1002/cncr.23592. [DOI] [PubMed] [Google Scholar]
- 18.Adjuvant chemotherapy for localised resectable soft-tissue sarcoma of adults: meta-analysis of individual data. Sarcoma Meta-analysis Collaboration. Lancet. 1997;350:1647–1654. [PubMed] [Google Scholar]
- 19.Kwon TW, Sung KB, Cho YP, Kim DK, Yang SM, Ro JY, et al. Pararenal leiomyosarcoma of the inferior vena cava. J Korean Med Sci. 2003;18:355–359. doi: 10.3346/jkms.2003.18.3.355. [DOI] [PMC free article] [PubMed] [Google Scholar]