Abstract
Background
We studied the characteristics and resource utilization of patients with syncope in a German emergency department (ED).
Methods
We carried out a single-center retrospective analysis of patients with syncope who presented to the ED of the Klinikum Nürnberg (a municipal hospital in Nuremberg, Germany).
Results
Among the 28 477 patients who presented to the ED from 15 May 2009 to 30 September 2009, 440 (1.5%) presented with syncope. Their mean age was 62 years (standard deviation, 20 years); 50.4% were women, 43.4% were over age 70, 11.8% had cardiogenic and 4.8% neurological syncope, and 18.2% had more than two comorbid conditions. 20.7% were discharged after evaluation in the ED, 14.1% were brielfly hospitalized in the ED’s clinical observation unit, and 56.6% were admitted to one of the hospital’s specialty wards. 8.6% left the ED against medical advice. All of the syncope patients were evaluated by history-taking, physical examination, and 12-lead electrocardiogragraphy (ECG); ECG revealed abnormal findings in 36.4% of patients. Nearly all patients also underwent laboratory testing, which revealed hyponatremia (a serum sodium concentration under 130 mmol/L) in 5.9% and a serum creatinine level above 2 mg/dL in 5.3%. Many underwent technology-intensive tests such as cranial computed tomography (129 patients), but these tests only rarely yielded abnormal findings (3.1%). 27% of the syncope patients underwent Doppler ultrasonography of the vessels supplying the brain, with abnormal findings in 6.7% of cases. (Orthostatic testing was performed in 14.5% of the patients and was positive in 26.6%.)
Conclusion
Many patients presenting with syncope to a German ED are elderly, and multiple comorbidities are common. Technology-intensive testing in patients with syncope has a low diagnostic yield and consumes resources. The introduction of standards for the evaluation of syncope in the ED would be helpful.
Syncope is a temporary loss of consciousness with a global cerebral hypoperfusion that is often associated with a loss of muscle tone (1, 2). Syncope usually occurs rapidly and is characterized by short duration and a complete and spontaneous recovery (2). As patients with syncope or near-syncope experiences have similar pathophysiology and prognosis (3), we therefore refer in the following to both types of occurrences as „syncope.“
Patients with cardiac or cerebrovascular syncope represent a high risk population and have a limited prognosis, while the outcome for vasovagal syncope is favorable (4). These observations, which arise from epidemiological perspective based on population studies, have been emphasized in guidelines (2). However, they cannot be directly transferred to the emergency department (ED), where the attending physician must clarify not only the cause of syncope but also whether the affected patient should be hospitalized based on comorbidity, a decision which is taken independently of the event and the type of syncope (5, 6). The decision about which examinations are necessary requires risk stratification evaluation and is complex, yet it has been insufficiently examined in Germany until now.
Approximately 1% to 3% of patients entering ED present with syncope as the main symptom (2). Whether patients presenting with syncope are admitted to ED depends on:
the subjective feeling of the patient,
the patient’s relatives,
the primary treating physician.
Due to the complexity of the disorder and the associated diagnostic difficulties, numerous diagnostic procedures are undertaken that are neither clinically effective nor economically justifiable (7).
Differences in the structures of national health care only allows a limited transfer of international study results to practice with syncope in German EDs. After a systematic literature review, we found no current data pertaining to the diagnosis and treatment of ED patients presenting with syncope in Germany. The aim of this survey was to describe the syncope patients who were treated in the ED of a large urban hospital in Germany, and to analyze and evaluate the diagnostic procedures that are initiated in ED.
Methods
Patients and study design
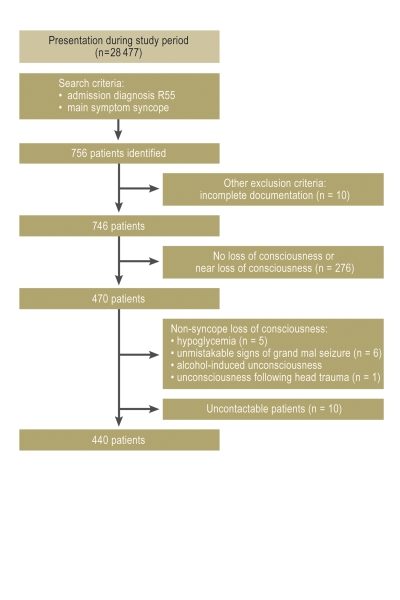
This study was performed in the ED of an urban hospital with maximum care (with about 75 000 emergency patients/year). All patients who were admitted with syncope between 15 May and 30 September 2009 were identified through the hospital records. The search consisted of querying the database for the admission and/or discharge diagnosis of „syncope and collapse“ (R55, ICD-10-GM version 2009), as well as manually researching the presentation reasons for the emergency admission, for the study period. Only patients presenting with syncope or near-syncope were considered (2). Incompletely documented cases were also excluded (eFigure). Study variables were selected according to established recommendations (2, 7, 8). Concomitant conditions were characterized by the Charlson Comorbidity Index (5, 9).
eFIGURE.
Analysis of patients who presented to the Klinikum Nürnberg with syncope or near syncope as their main symptom during the study period. Medical records for 10 patients were incomplete or were not taken; these cases were excluded from the analysis
Endpoint, diagnostic resources
Clinical endpoint
In addition to characterizing the ED patient collective, clinical endpoints—based on the index—that appeared within 30 days were quantified (e.g., any required invasive interventions or serious adverse events [8, 10, 11]).
Invasive interventions were considered to be pacemaker or defibrillator implantation, percutaneous coronary intervention, operations, blood transfusion, cardiopulmonary resuscitation, modification in antiarrhythmic therapy, endoscopic intervention, or correction of carotid stenosis. Serious adverse events were sudden cardiac death, pulmonary embolism, stroke, severe infection or sepsis, severe electrolyte disturbances, renal dysfunction, ventricular or atrial arrhythmias, intracranial bleeding, anemia, myocardial infarction, life-threatening conditions as a consequence of syncope (such as skull or long bone fractures), or re-admission within 30 days for syncope.
Diagnostic tests
The following diagnostic tests were analyzed:
Blood chemistry analysis upon admission
12-lead electrocardiogram (ECG)
ECG monitoring or long-term ECG
Echocardiography
Electroencephalography (EEG)
Conventional chest X-ray
Cranial computed tomography (CCT)
Other CT scans
Magnetic resonance imaging (MRI)
Carotid artery ultrasonography.
Laboratory test results were considered to be pathological when they showed clinically relevant differences (7). In order for pathological results to justify further instrumental examinations, both the pathological test results and the clinical relevance of the treatment for syncope were taken into consideration (eTable).
eTable. Definition of test results considered as pathological for the decision to hospitalize patients with syncope.
| Test | |
| Long-term ECG |
|
| Echocardiography |
|
| Coronary angiography |
|
| Carotid artery ultrasonography |
|
| Orthostatin test |
|
| Chest X-ray |
|
| Cranial computed tomography (CCT) |
|
Stasticial analysis
All collected data are presented with the frequency, means, and standard deviations, given with 95% confidence intervals or as median and interquartile ranges. Normal distribution was tested for with the Shapiro-Wilk test; normally distributed data were compared with Student’s t-test for unpaired samples, while non-normally distributed data were compared with non-parametric tests (e.g., the Kruskal-Wallis analysis and the U test).
Categorical data were analyzed with the chi-square test. P values are given to highlight the differences between the post hoc defined groups but were not Bonferroni-corrected and should not be considered to be statistically significant.
Statistical tests were carried out with R software (R Foundation for Statistical Computing, Version 2.11.0) or with the SPSS software (version 16; IBM, Munich).
Results
Over the study period, 28 477 syncope patients presented to the ED, whereby 297 of these had suffered an epileptic attack. Syncope was documented for 440 patients (1.5%; eFigure). Overall, 49.5% of the syncope patients were men, 43.4% were over age 70, and 19.8% were over age 80 (Table 1). Comorbidities and pathological test results are listed in Tables 1 and 2. Patients were admitted to the hospital following referral by an emergency physician (201; 45.7%) or a general or specialist physician in private practice (70; 15.9%), or on their own accord (169; 38.4%). The syncope types are shown in Table 3.
Table 1. Characteristics of patients with syncope who visited the emergency department of the Klinikum Nürnberg*1.
| Variable/parameter | Total patients | With endpoint | Without endpoint | p = |
| Male sex, n (%) | 218 (49.6) | 49 (55.1) | 169 (48.2) | 0.25 |
| Age, in years*2 | 62 ± 20 | 71 ± 17 | 60 ± 20 | 0.001 |
| – over 70 years old, n (%)*2 | 191 (43.4) | 53 (59.6) | 138 (39.3) | 0.01 |
| – over 80 years old, n (%)*2 | 87 (19.8) | 28 (31.5) | 59 (16.8) | 0.01 |
| Medical history | ||||
| Coronary heart disease or myocardial infarction, n (%)*2 | 80 (18.2) | 23 (25.8) | 57 (16.2) | 0.03 |
| Arrhythmia, n (%)*2 | 51 (11.6) | 20 (22.5) | 31 (8.8) | 0.001 |
| Heart failure, n (%)*2 | 37 (8.4) | 20 (22.5) | 17 (4.8) | 0.001 |
| Peripheral arterial occlusive disease, n (%)*2 | 22 (5) | 9 (10.1) | 13 (3.7) | 0.01 |
| Diabetes Mellitus, n (%)*2 | 80 (18.2) | 24 (27.0) | 56 (16.0) | 0.01 |
| High blood pressure, n (%)*2 | 186 (42.3) | 47 (52.8) | 139 (39.6) | 0.02 |
| Dementia, n (%) | 26 (5.9) | 6 (6.7) | 20 (5.7) | 0.79 |
| Lung disease, n (%) | 29 (6.6) | 10 (11.2) | 19 (5.4) | 0.06 |
| Tumor, n (%)*2 | 24 (5.5) | 11 (12.4) | 13 (3.7) | 0.01 |
| Renal dysfunction, n (%)*2 | 72 (16.4) | 22 (24.7) | 50 (14.3) | 0.03 |
| Liver dysfunction, n (%)*2 | 13 (3.0) | 6 (6.7) | 7 (2.0) | 0.03 |
| Vital parameters | ||||
| Respiratory rate, 1/min*2 | 17 ± 4 (16.6 – 17.4) | 18 ± 5 (17 – 19) | 16 ± 4 (15.6 – 16.4) | 0.02 |
| Heart rate, 1/min*2 | 78 ± 17 (76.4 – 79.6) | 83 ± 23 (78.2 – 87.8) | 75 ± 15 (73.4 – 76.6) | 0.001 |
| Systolic blood pressure, mmHg*2 | 134 ± 23 (131.9 – 136.1) | 129 ± 26 (123.6 – 134.4) | 136 ± 23 (133.6 – 138.4) | 0.01 |
| Oxygen saturation, %*2 | 97 ± 4 (96.6 – 97.4) | 96 ± 8 (94.3 – 97.7) | 98 ± 2 (97.8 – 98.2) | 0.001 |
| Temperature, °C*2 | 36.7 ± 0.7 (36.6 – 36.8) | 37.0 ± 1.1 (36.8 – 37.2) | 36.7 ± 0.5 (36.6 – 36.8) | 0.001 |
| Laboratory parameters | ||||
| Leukocytes, 103/µL*2 | 9.2 ± 5.4 (8.7 – 9.7) | 9.9 ± 4.4 (9 – 10.8) | 8.9 ± 5.6 (8.3 – 9.5) | 0.01 |
| Hemoglobin, g/dL*2 | 13.3 ± 2.0(13.1 – 13.5) | 12.5 ± 2.5 (12 – 13) | 13.5 ± 1.8 (13.3 – 13.7) | 0.001 |
| Sodium, mmol/L*2 | 137 ± 4(136.6 – 137.4) | 135 ± 5 (134 – 136) | 137 ± 4 (136.6 – 137.4) | 0.001 |
| Potassium, mmol/L*2 | 3.9 ± 0.5 (3.9 – 3.9) | 4.1 ± 0.7 (4 – 4.2) | 3.9 ± 0.5 (3.8 – 4) | 0.04 |
| Creatinine, mg/dL*2 | 1.1 ± 0.7 (1 – 1.2) | 1.3 ± 0.8 (1.1 – 1.5) | 1.0 ± 0.6 (0.9 – 1.1) | 0.001 |
| Glucose, mg/dL*2 | 131 ± 46 (126.7 – 135.3) | 157 ± 72 (142 – 172) | 125 ± 36 (121.2 – 128.8) | 0.001 |
*1In addition to frequency, means, and standard deviations, vital and laboratory parameters are given with a 95% confidence interval.
*2These show p value of <0.05, indicating possible statistic significance between groups
Table 2. Proportion of pathological results with respect to the overall study group*1.
| Parameter | Performed | Pathological with respect to the reference values |
| Vital parameters | ||
| Respiratory rate, n (%) | 388 (88.2) | 75 (19.3) |
| Oxygen saturation, n (%) | 425 (96.6) | 32 (7.5) |
| Heart rate, n (%) | 438 (99.5) | 37 (8.4) |
| Systolic blood pressure, n (%) | 439 (99.8) | 19 (4.3) |
| Laboratory tests | ||
| Hemoglobin, n (%) | 438 (99.5) | 6 (1.4) |
| Glucose, n (%) | 432 (98.2) | 31 (7.2) |
| Sodium, n (%) | 438 (99.5) | |
| – Sodium <130 mmol/l, n (%) | 26 (5.9) | |
| – Sodium <120 mmol/l, n (%) | 3 (0.7) | |
| Potassium, n (%) | 436 (99.1) | 87 (20.0) |
| Creatinine, n (%) | 437 (99.3) | |
| – Creatinine >2.0 mg/dL, n (%) | 23 (5.3) | |
| – Creatinine >3.0 mg/dL, n (%) | 7 (1.6) | |
| Troponin T, n (%) | 332 (75.5) | 24 (7.2) |
| Instrumental tests (not large instruments) | Pathological results (%) | |
| 12-lead ECG, n (%) | 440 (100) | 160 (36.4) |
| – new finding, n (%) | 34 (21.3) | |
| – known finding, n (%) | 48 (30.0) | |
| – not documented, n (%) | 78 (48.8) | |
| Orthostatic test, n (%) | 64 (14.5) | 17 (26.6) |
| Chest X-ray, n (%) | 159 (36.1) | 21 (13.2) |
| Echocardiography, n (%) | 175 (39.8) | 22 (12.6) |
| Carotid artery ultrasonography, n (%) | 119 (27.0) | 8 (6.7) |
| ECG monitoring >8 h, n (%) | 228 (51,8) | 25 (11,0) |
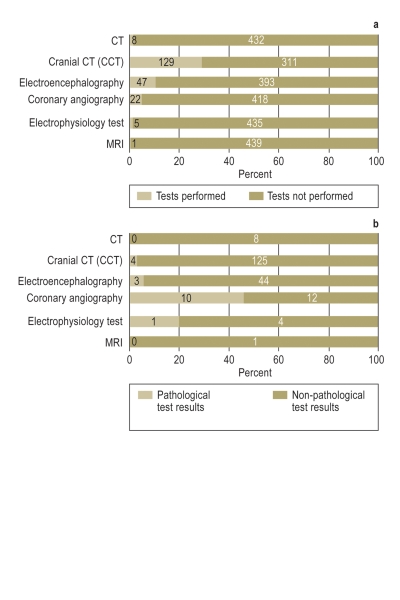
*1test results from large instruments (e.g., CT, MRI) are shown in Figure 2
Table 3. Classification of syncope causes, based on the guidelines of the European Society of Cardiology, with respect to the age distribution in our study and related comorbidities*1.
| Type of synkope | No of patients (%) | Age(mean) | Distribution acc. to CCI | ||
| 0 | 1–2 | >2 | |||
| Unexplained syncope | 200 (45.4) | 67 | 80 | 77 | 43 |
| Neurological syncope | 21 (4.8) | 66 | 13 | 4 | 4 |
| Cardiac syncope | 52 (11.8) | 68 | 24 | 18 | 10 |
| Orthostatic syncope | 117 (26.6) | 59 | 59 | 39 | 19 |
| Vasovagal syncope | 46 (10.4) | 46 | 35 | 7 | 4 |
| Psychogenic syncope | 4 (0.9) | 44 | 4 | 0 | 0 |
*1Syncope events that could not be clearly classified based on the medical records available to the authors were classified as "unexplained syncope." acc = according; CCI = Charlson Comorbidity Index
Clinical Endpoints
Of the 440 patients, 89 (20.2%) suffered an adverse event within 30 days after syncope (Table 4). Of these, 12 (13.5%) experienced bradycardic rhythm disturbance, an indication for pacemaker implantation, 5 (5.6%) had an acute myocardial infarction, and 35 (39.3%) suffered another type of cardiac event. Non-cardiac endpoints are shown in Table 4. Five patients experienced another syncope; of these, three had acute renal failure, and two had a tumor in an advanced stage. Of the 89 patients with clinical endpoints, 29 had unexplained syncope (32.6%), while only 61 of the 351 patients without an endpoint had unexplained syncope (17.4%; p<0.001).
Table 4. Distrubution of the endpoints for 89 out of 440 patients that occurred within 30 days after hospitalization*1.
| Endpoint | n (%) |
| Cardiac endpoint | 35 (39.3) |
| Myocardial infarction | 5 (5.6) |
| Cardioversion for atrial fibrillation | 2 (2.2) |
| Pacemaker/ICD implantation | 12 (13.5) |
| Resuscitation | 2 (2.2) |
| Valve defects/stenosis (requires OP) | 3 (3.4) |
| Ventricular tachycardia | 4 (4.5) |
| Percutaneous coronary intervention or requirement for coronary artery bypass intervention | 4 (4.5) |
| Absolute tachyarrhythmia without cardioversion (only with tachycardia-induced heart failure) | 2 (2.2) |
| Supraventricular tachycardia | 1 (1.1) |
| Non-cardiac endpoint | 41 (46.1) |
| Endoscopy with intervention | 7 (7.9) |
| Blood transfusion | 8 (9) |
| Carotid operation | 0 (0) |
| Pulmonary embolism | 0 (0) |
| Stroke (recent ischemic or hemorrhagic insult) | 5 (5.6) |
| Traumatic brain injury | 4 (4.5) |
| Severe infection | 17 (19.1) |
| Other endpoints | 13 (14.6) |
| Re-admittance within 30 days | 2 (2.2) |
| Other life-threatening conditions | 11 (12.4) |
| Sudden death | 0 (0) |
*1Endpoints are divided into the groups "cardiac endpoints," "non-cardiac endpoints," and "other endpoints"
Length of stay and patient disposition
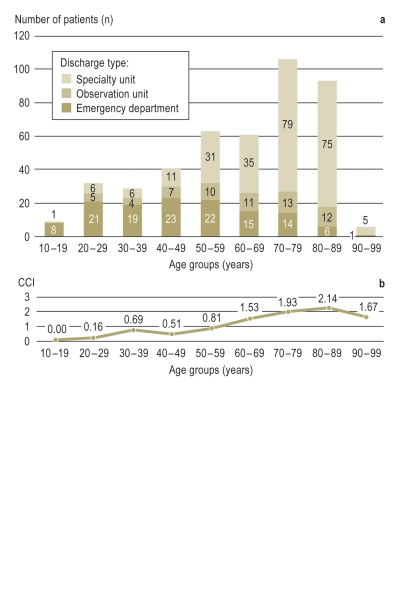
Of the 440 patients, 91 (20.7%) were directly discharged after treatment in the ED. Of the 349 (79.3%) patients admitted for inpatient care, 62 (17.8%) were observed in an ED clinical observation unit, and 249 patients (71.3%) were assigned to other specialty wards. Thirty-eight (10.9%) of the patients were released from the hospital against medical advice. Of the 34 (7.7%) patients who presented mainly due to injury caused by syncope, 17.7% were treated on an outpatient basis, 8.8% were treated in the ED observation unit, and 73.5% were hospitalized. Figure 1 shows—grouped by age—the type of discharge for the study population (Figure 1a) and comorbidities of affected patients (Figure 1b). The median Charlson comorbidity score for patients in the observation unit was significantly lower than for those in the other departments (0 compared to 1; p<0.001), as was the median effective relative weight of the billed diagnosis related groups (DRGs) (0.21 [IQR 0.37] compared to 0.58 [IQR 0.27]; p<0.001).
Figure 1.
Age-dependent distribution of patients with syncope
Patients with syncope according to age group and indicating the type of care (inpatient care in a speciality unit, inpatient care in the ED observation unit, or discharge from the emergency department (ED) for outpatient follow-up care).
Patients discharged against medical advice (n = 38) are represented here according to discharge from the ED. Comorbidities (according to the Charlson Comorbidity Index, CCI) are shown according to the different age groups.
Diagnostic process
The vital parameters for nearly all patients with syncope were measured in the ED (blood pressure, for 99.8% of patients; heart rate, for 99.5%; respiration rate, for 88.2%; and oxygen saturation, for 96.6%). For the majority of patients (99.3%), a laboratory blood analysis was performed, and all were evaluated with a physical examination and medical history. Further, 75.5% of patients were tested for troponin T, whereby the levels in 7.2% of the cases deviated from the reference range (Table 2). All patients were examined by 12-lead ECG, 14.5% with an orthostatic test, and 36.1% by conventional chest X-ray; of these, pathological outcomes were observed for 36.4%, 26.6%, and 13.2% of the patients, respectively. An echocardiogram was performed for 175 patients (39.8% of the total), which resulted in pathological findings in 12.6% of the cases. Further results are listed in Table 2.
Additional, more technology-intense diagnostic procedures, coded in the German Procedure Classification (Operationen- und Prozedurenschlüssel, OPS), are depicted in Figure 2. CCT was carried out for 129 of the 440 patients (29.3%) but only revealed abnormal findings for 4 patients (3.1%). EEG was performed on 10.7% of patients, coronary angiography, on 5%, and an electrophysiology test, on 1.1% (Figure 2a). The proportion of abnormal findings is shown in Figure 2b.
Figure 2.
Instrumental examinations patient groups
a) Frequency of instrumental examinations performed
b) Percentage of pathological findings that were related to syncope by the performed tests
Discussion
Patients with syncope or near-syncope present a challenge for the initial medical evaluation due to the complexity of the disorder (2, 12).
The main results of this retrospective analysis on patients with syncope are:
Syncope is a common reason for ED visits. Of the patients presenting with syncope, 20.7% were released with out-patient care and 79.3% were admitted to the hospital.
Elderly persons represent a large portion of the patients with syncope who are admitted for inpatient care; they also have a higher rate of comorbidity than non-elderly patients.
Approximately 20% of patients experienced a syncope-related endpoint within 30 days following index presentation. In addition to cardiac syncope, independent comorbidities (such as medication side effects), serious infections, hypovolemia, and hemorrhage, play a relevant role.
The recommended basic diagnostic criteria for the ED were carried out for nearly all patients. However, simple tests with high diagnostic yield, such as the orthostatic test, are rarely used, while more technically-intensive tests with low diagnostic yield for explaining syncope, such as carotid artery ultrasonography, long-term ECG, or a CCT, are frequently performed. This worsens the cost-benefit ratio of syncope investigation.
Frequency of hospital admission, comorbidity
Various studies have shown that about 25% to 63% of patients presenting with syncope at an ED are admitted for inpatient care (13, 14). The high admission rate observed in this study could be due to diagnostic uncertainties or to inadequate adherence to guidelines (13). Here, we show that the cohort was composed mainly of elderly patients, and that primarily elderly patients with syncope were admitted for inpatient care. Similar conclusions were reached by a study from the USA (15). The high rate of inpatient care of elderly patients that we observed in our hospital can be explained by the presence of comorbid conditions that required treatment, such as the high percentage of patients with relevant hyponatremia or renal impairment. The lack of information about occurring comorbidities makes it difficult to interpret other studies (11, 16– 18). It is possible that more patients are admitted to German EDs with relevant comorbidities, which would reflect a well-functioning, dual health care structure in Germany.
The high risk of adverse events occurring in multi-morbid patients with syncope supports this hypothesis (5). It could also be that the symptom of „syncope“ in elderly persons is an indicator of serious underlying health problems and should be interpreted as a red flag that should prompt hospital admission. Thus, hospitalization would not be necessary due to syncope per se but rather due to the underlying comorbidity (19).
Diagnostic tests for syncope
The basic diagnostics recommended by guidelines (medical history taking, physical examination, and performing 12-lead ECGs and laboratory analyses) were carried out for almost all patients with syncope (2). Additionally, technically-intensive tests with low diagnostic efficiency are performed. Current publications confirm that the decisions to perform many of the diagnostic tests on patients to explain syncope appear to be unreflected, as these test results are often irrelevant to syncope (7). Mendu et al. have proposed that the cost of diagnostic tests should be weighed against their effectiveness, and that this should be considered when selecting tests and planning further patient management (7). The resulting medical economic parameter would be defined as „medical cost“ or as „cost per conspicuous finding“. Tests that are not recommended in the guidelines and that had a low diagnostic yield in our study would therefore be characterized with a very high cost per conspicuous finding (such as CCT, EEG, and carotid artery ultrasonography). In addition, the lack of systematic evaluation of patients with syncope adds a burden to the relevant hospital departments.
A targeted diagnostic evaluation—based primarily on medical history and physical examination—is desirable (20). When the ED examinations are based on relevant findings (such as the presence of focal neurological deficits and headaches), CCT examinations are reduced by over half (21). Similarly, carotid artery ultrasonography is reduced when the decisions for treating patients with syncope are based on relevant (symptomatic) findings (22). The surprising fact that the orthostatic test was not often used at our facility may be attributable to a lack of awareness of its effectiveness. It is possible that reducing the current problem of over-diagnosis on the one hand and under usage of the orthostatic test on the other can only occur if stricter indications are set and used within a special „syncope unit,“ which could be located for example in the ED’s observation unit (23). A study from the USA revealed that introducing internal hospital guidelines and instructions had little effect on emergency physicians’ diagnostic decisions in the ED; this is likely due to the complexity of syncope (24). Introducing evidence-based decision aids when investigating relevant intracranial hemorrhage can also lead to a more frequent use of native CCT scans when presented with a minor head injury (25).
Current guidelines for evaluating syncope recommend monitoring hemoglobin and blood glucose levels (2). In fact, additional laboratory tests (such as troponin T, D-dimer, and the coagulation tests) were performed in our cohort, although they have a low diagnostic yield. Further, we were able to show that a large percentage of our patients had renal insufficiency or clinically relevant hyponatremia. However, this may be due to a selection for seriously ill patients in German EDs, which suggests that international guidelines can only be partially implemented in German patient care.
Limitation of the study
This study represents the first presentation of a large, unselected data set for patients with syncope in a German emergency department. Since data presentation varies between published studies, and since no other German data set has been published to date, our ability to compare studies and interpret the available data is restricted.
The high rate of syncope with unknown etiology could be due to the difficulty of adequately evaluating medical histories in a retrospective analysis. A prospective study of acquisition would have likely made more precise differentiations possible. High rates of unexplained syncope is common in clinical practice and is well-described in publications, and represents a severe limitation of interpreting the available data.
Summary and conclusions
In the ED of the large German urban hospital studied, approximately 80% of patients with syncope were admitted to the hospital, of which about 20% were evaluated during a brief stay in the ED’s clinical observation unit. Approximately 20% of patients were directly discharged into outpatient care. The high hospitalization rate observed here as compared to other (international) study groups is likely due to a higher rate of multiple comorbidity and/or elderly patients in our study. In almost all cases, patients presenting with syncope at our ED underwent a basic diagnostic procedure that complied with guidelines. However, the additional use of untargeted diagnostic tests with low accuracy resulted in high resource utilization and unnecessary costs. Introducing operating procedures or checklists that are based on a focused and complete medical history could promote using apparatus-based diagnostics according to guidelines and could improve the care process for patients with syncope. Providing a collection of relevant prognostic indicators could make individual diagnostic decisions more transparent and could thus promote sustainable change in the operating procedures.
Key Messages.
Patients with syncope or near-syncope frequently visit German emergency departments, but their medical evaluation is challenging due to the heterogeneous and complex nature of the disorder.
A majority of patients with syncope are elderly persons who, in contrast to the non-elderly, have higher rates of comorbidity and longer hospital stays.
Almost all patients in our study were evaluated by basic diagnostics according to recommended guidelines.
Simple tests with high diagnostic yield, such as the orthostatic test, were seldomly performed, while technically-intensive procedures with low diagnostic yield, such as carotid artery ultrasonography, long-term ECG, and CCT, were performed disproportionately frequently, which strongly burdens clinical diagnostic capacities.
Introducing standard operating procedures based on recommendations from relevant guidelines could improve care of patients with syncope.
Acknowledgments
Translated from the original German by Veronica A. Raker, PhD.
The authors thank Dr. A. Estelmann, Director of the Klinikum Nürnberg, for critically reading the manuscript, and M. Langada for professional database management.
Footnotes
Conflict of interest statement
Prof. Dr. M. Christ received consulting fees from Philips and Roche AG, congress fees from MSD and Pfizer, and fees for the preparation of advanced education seminars from Roche AG, Abbott GmbH, Brahms, Alere AG, and Radiometer.
Prof. Dr. H. Mang received fees for the preparation of advanced education seminars from Paul Hartmann AG.
Dr. H.J. Heppner, V. Langada, and S. Güldner declare that no conflict of interest exists.
References
- 1.Kapoor WN. Syncope. N Engl J Med. 2000;343:1856–1862. doi: 10.1056/NEJM200012213432507. [DOI] [PubMed] [Google Scholar]
- 2.Moya A. Guidelines for the diagnosis and management of syncope (version 2009): The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC): Developed in collaboration with, European Heart Rhythm Association (EHRA)1. European Heart Journal. 2009;30:2631–2671. doi: 10.1093/eurheartj/ehp298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grossman SA, Babineau M, Burke L, et al. Do outcomes of near syncope parallel syncope? Am J Emerg Med. 2010 doi: 10.1016/j.ajem.2010.11.001. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N Engl J Med. 2002;347:878–885. doi: 10.1056/NEJMoa012407. [DOI] [PubMed] [Google Scholar]
- 5.Getchell WS, Larsen GC, Morris CD, Mcanulty JH. Epidemiology of Syncope in hospitalized patients. J Gen Intern Med. 1999;14:677–687. doi: 10.1046/j.1525-1497.1999.03199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vetta F, Ronzoni S, Costarella M, et al. Recurrent syncope in elderly patients and tilt test table outcome: the role of comorbidities. Arch Gerontol Geriatr. 2009;49(1):231–236. doi: 10.1016/j.archger.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 7.Mendu Ml, Mcavay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Archives of Internal Medicine. 2009;169:1299–1305. doi: 10.1001/archinternmed.2009.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quinn JV, Stiell IG, Mcdermott DA, Sellers Kl, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Annals of Emergency Medicine. 2004;43:224–232. doi: 10.1016/s0196-0644(03)00823-0. [DOI] [PubMed] [Google Scholar]
- 9.Charlson ME, Pompei P, Ales Kl, Mackenzie C. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 10.Colivicchi F, Ammirati F, Melina D, Guido V, Imperoli G, Santini M. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. European Heart Jjournal. 2003;24:811–819. doi: 10.1016/s0195-668x(02)00827-8. [DOI] [PubMed] [Google Scholar]
- 11.Reed MJ, Newby DE, Coull AJ, Prescott RJ, Jacques KG, Gray AJ. The ROSE (risk stratification of syncope in the emergency department) study. Journal of the American College of Cardiology. 2010;55:713–721. doi: 10.1016/j.jacc.2009.09.049. [DOI] [PubMed] [Google Scholar]
- 12.Huff JS, Decker WW, Quinn JV, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with syncope. Annals of Emergency Medicine. 2007;49:431–444. doi: 10.1016/j.annemergmed.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 13.Baron-Esquivias G, Martínez-Alday J, Martín A, et al. Epidemiological characteristics and diagnostic approach in patients admitted to the emergency room for transient loss of consciousness: Group for Syncope Study in the Emergency Room (GESINUR) study. Europace. 2010;12:869–876. doi: 10.1093/europace/euq018. [DOI] [PubMed] [Google Scholar]
- 14.McCarthy F, McMahon CG, Geary U, Plunkett PK, Kenny RA, Cunningham CJ. Management of syncope in the Emergency Department: a single hospital observational case series based on the application of European Society of Cardiology Guidelines. Europace. 2009;112:16–24. doi: 10.1093/europace/eun323. [DOI] [PubMed] [Google Scholar]
- 15.Grossman SA, Fischer C, Lipsitz LA, et al. Predicting adverse outcomes in syncope. The Journal of Emergency Medicine. 2007;33:233–239. doi: 10.1016/j.jemermed.2007.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Costantino G, Perego F, Dipaola F, et al. Short- and long-term prognosis of syncope, risk factors, and role of hospital admission: results from the STePS (Short-Term Prognosis of Syncope) study. J Am Coll Cardiol. 2008;51:276–283. doi: 10.1016/j.jacc.2007.08.059. [DOI] [PubMed] [Google Scholar]
- 17.Dipaola F, Costantino G, Perego F, et al. San Francisco Syncope Rule, Osservatorio Epidemiologico sulla Sincope nel Lazio risk score, and clinical judgment in the assessment of short-term out-come of syncope. The American Journal of Emergency Medicine. 2010;28:432–439. doi: 10.1016/j.ajem.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 18.Quinn J, McDermott D, Stiell I, Kohn M, Wells G. Prospective validation of the San Francisco Syncope Rule to predict patients with serious outcomes. Annals of Emergency Medicine. 2006;47:448–454. doi: 10.1016/j.annemergmed.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 19.Kapoor WN, Hanusa BH. Is syncope a risk factor for poor outcomes? Comparison of patients with and without syncope. The American Journal of Medicine. 1996;100:646–655. doi: 10.1016/s0002-9343(95)00052-6. [DOI] [PubMed] [Google Scholar]
- 20.Kapoor WN, Karpf M, Maher Y, Miller RA, Levey GS. Syncope of unknown origin. The need for a more cost-effective approach to its diagnosis evaluation. JAMA. 1982;247:2687–2691. doi: 10.1001/jama.247.19.2687. [DOI] [PubMed] [Google Scholar]
- 21.Grossman SA, Fischer C, Bar Jl, et al. The yield of head CT in syncope: a pilot study. Internal and Emergency Medicine. 2007;2:46–49. doi: 10.1007/s11739-007-0010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schnipper Jl, Ackerman RH, Krier JB, Honour M. Diagnostic yield and utility of neurovascular ultrasonography in the evaluation of patients with syncope. Mayo Clinic proceedings. Mayo Clinic. 2005;80:480–488. doi: 10.4065/80.4.480. [DOI] [PubMed] [Google Scholar]
- 23.Brignole M, Ungar A, Bartoletti A, et al. Standardized-care pathway vs. usual management of syncope patients presenting as emergencies at general hospitals. Europace. 2006;8:644–650. doi: 10.1093/europace/eul071. [DOI] [PubMed] [Google Scholar]
- 24.Melnick ER, Genes NG, Chawla NK, Akerman M, Baumlin KM, Jagoda A. Knowledge translation of the American College of Emergency Physicians’ clinical policy on syncope using computerized clinical decision support. Int J Emerg Med. 2010;3:97–104. doi: 10.1007/s12245-010-0168-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goodacre S. Hospital admissions with head injury following publication of NICE guidance. Emerg Med J. 2008;25:556–557. doi: 10.1136/emj.2007.055723. [DOI] [PubMed] [Google Scholar]