Abstract
Introduction:
Childhood obesity is a major public health crisis nationally and internationally. The prevalence of childhood obesity has increased over few years. It is caused by imbalance between calorie intake and calories utilized. One or more factors (genetic, behavioral, and environmental) cause obesity in children. Physical, psychological, and social health problems are caused due to childhood obesity. Hence, effective intervention strategies are being used to prevent and control obesity in children. The purpose of this manuscript is to address various factors influencing childhood obesity, a variety of interventions and governmental actions addressing obesity and the challenges ahead for managing this epidemic.
Methods:
In order to collect materials for this review a detailed search of CINAHL, MEDLINE, ERIC, Academic Search Premier databases was carried out for the time period 1999-2011.
Results:
Some of the interventions used were family based, school based, community based, play based, and hospital based. The effective school-based interventions were seen targeting physical activity along with healthy diet education. The major challenges faced by these intervention programs are financial, along with stigmatization of obese children. Governments along with other health care organizations are taking effective actions like policy changing and environmentally safe interventions for children to improve physical activity.
Conclusions:
In conclusion, childhood obesity can be tackled at the population level by education, prevention and sustainable interventions related to healthy nutrition practices and physical activity promotion.
Keywords: Calorie imbalance, childhood obesity, interventions, physical activity, policy changing
INTRODUCTION
Obesity is a major public health crisis among children and adults.[1,2] The range of weights for individuals if greater than the ideal weight, which is considered healthy for the particular height, is termed as either overweight or obese. Childhood-related obesity is an increasing concern with respect to the health and well-being of the child. Body mass index (BMI), a measure of weight with relation to height, is not only used as an outcome measure to determine obesity but also as a useful anthropometric index for cardiovascular risk.[3] For children between 2 and 19 years, BMI is plotted on the CDC growth chart to check for the corresponding age and sex related percentile. Childhood obesity is defined as a BMI at or above 95th percentile for children of same age and sex.[4] Classifications of obesity in children depend upon the body composition of the child, as it varies with respect to age and sex of the child.[4]
MAGNITUDE OF THE PROBLEM
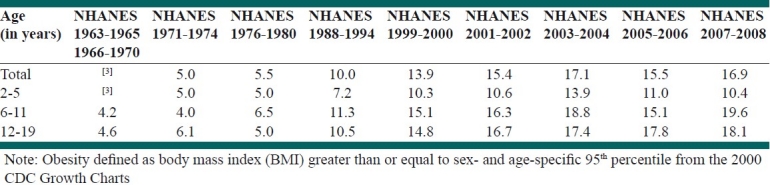
The prevalence of childhood obesity is increasing in developed and underdeveloped countries.[5] The development in reducing the problem of obesity and overweight is monitored nationally by using data from National Health and Nutrition Examination Survey. The report presented by NHANES for the year 2007-2008 estimated that 16.9% of children and adolescent in the age group of 2-19 years were obese.[6] Childhood obesity prevalence among preschool children between age group of 2-5-year-old girls and boys has increased from 5.0 to 10% between 1976-1980 and 2007-2008 and it has increased from 6.5 to 19.6% among age group of 6-11 year olds.[6] The data collected for the same period shows that the adolescent (age group 12-19 years) obesity has increased from 5.0 to 18.1% [Figure 1, Table 1].[6]
Figure 1.
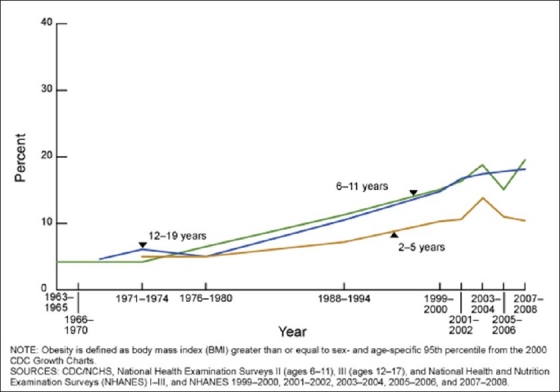
Graphically shows the increasing trend of obesity among children and adolescent population from 1963 to 2008. Source: CDC/NCHS, National Health Examination Surveys 11 (ages 6-11), 111 (ages 12-17), and National Health and Nutrition Examination Surveys (NHANES) 1-111 and NHANES 1999-2000, 2001-2002, 2003-2004, 2005-2006, and 2007-2008[6]
Table 1.
Prevalence of obesity among US children and adolescents aged 2-19, for selected years 1963-1965 through 2007-2008[6]
Healthy people 2010 have ranked obesity as number one health problem showing that prevalence of childhood obesity has increased over the years.[7] Increased prevalence of childhood obesity may have adverse morbidity and mortality implications in the adult life of the child.[8] Childhood obesity concern has increased worldwide. There has been increased prevalence of childhood obesity in England, especially among school children over last few decades.[9] Childhood obesity is common in United Kingdom and according to the health survey conducted in 2004, obesity among 2-10-year olds was 14% and among 11-15-year olds was 15%.[5]
METHODS
In order to collect materials for this review a detailed search of CINAHL, MEDLINE, ERIC, Academic Search Premier databases was carried out for the time period 1999-2011.
A Boolean search strategy where the key words entered for search were “factors” and “childhood obesity” “interventions” and “governmental actions” and “economic problems” in differing orders were used to extract studies for this narrative review.
FACTORS INFLUENCING CHILDHOOD OBESITY
Childhood obesity is due to the imbalance between caloric intake of the child and the calories utilized (for growth, development, metabolism, and physical activities). Normally the amount of calories a child consumes through food or beverages, if not used for energy activities, leads to obesity.[10] Factors causing childhood obesity are genetic, behavioral, and environmental. Obesity can be multifactorial in children.
GENETIC FACTORS
There are certain genetic factors which may lead to obesity in children. These genetic factors increase the child's susceptibility for obesity.[10] Genetic factors may influence the metabolism, by changing the body fat content and energy intake and energy expenditure. Heritability of obesity from parents also influences obesity in children.[11]
BEHAVIORAL FACTORS
There are some behavioral factors which can cause obesity. Sometimes children eat more or consume more energy via food and beverages which are not utilized appropriately.[10] Children may eat large portions of food, foods high in sugar, and energy-rich foods. Hence, energy intake is higher than energy expenditure. So this may lead to weight gain in children.[10]
Lack of physical activity also plays an important role in obesity. Energy gained should be properly balanced by energy expenditure. It is seen that children and teens nowadays lack the required amount of physical activity; hence the calories are not used properly and can lead to obesity.[10] In a recently conducted mixed-methods study conducted in Iran, lack of safe and easy – access place for physical activity and unsupportive family were the main barriers to physical activity among adolescents.[12]
It is seen that sedentary lifestyle is an important factor for obesity, as many children spend most of their time in front of television sets, play video games, and watch computers. Children snack more in front of television and spent most of their time sitting without any physical activity.[10] All these behavioral factors are in a vicious circle with one leading to another. Children are prone to sedentary lifestyle such as watching television, consuming more energy-dense foods or snacks with large portion sizes, and having reduced physical activity, giving rise to obesity. The television advertisements of energy-rich and sugar-rich foods influence children to make unhealthy choices. These unhealthy food choices may lead to weight gain and obesity.[10]
ENVIRONMENTAL FACTORS
Environmental factors are those that surround the children and influence their food intake and physical activity.[10] These factors are seen in various settings such as at home, in school, and in the community. At home, the parent-child interaction is very crucial as parents can influence children food choices and motivate them to have a healthy lifestyle. Children spend most of their time at school, so school can promote healthy food choices and physical activity among them.[10] Community's lack of accessibility and affordability of healthy food can affect the nutrition of these children. Their lack of physical activity may be because of lack of facilities like safe side walks, bike paths, and safe parks.[10]
CONSEQUENCES OF CHILDHOOD OBESITY
Much health-related problems are associated with obesity in children. Childhood obesity also leads to health risks in adulthood. Health problems related to obesity are not only physical but psychological and social as well.[13]
PSYCHOLOGICAL AND SOCIAL HEALTH ISSUES
Children who are obese have a negative body-image, which leads to lower self-esteem. Children feel depressed and are nervous about their obesity issue and this has a negative effect on their behavior. This may also reflect negatively on their academic and social progress. They feel socially discriminated and stigmatized by their peers and adults.[13,14]
OTHER HEALTH RISKS
Obese children have high risk of cardiovascular diseases, high blood pressure, and increased cholesterol levels.[13] Childhood obesity increases the risk of having insulin resistant type 2 diabetes.[14] Children may have high risk of having respiratory problems like asthma as well. Obesity causes shortness of breath and sleep apnea. The physical effects may also reflect on musculoskeletal system causing discomfort due to increased weight on joint, causing muscle and bone disorder.[14] Obesity may affect liver causing fatty degeneration of liver.[13]
BEHAVIORAL INTERVENTIONS
Childhood obesity is a major public health issue. The complications caused due to childhood obesity are severe and could continue to affect the health of a child even in adulthood.[13] Hence, there is need to address this problem at every possible step through effective interventions and motivation strategies.
FAMILY-BASED LIFESTYLE INTERVENTIONS
Family bonding is a strong structure in the behavioral molding of the child. Parents and siblings are the people around the child who can influence child behavior and lifestyle.[15] Hence, effective interventions in a family setting can be beneficial to change child's behavior of overeating and unhealthy choice of food. Physical activity can be improved by small strategies like parking cars away from stores so that kids can walk and to take stairs instead of elevators or escalators. It is essential that parents are aware of the potential risk the child is facing due to obesity and take actions to control the problem. Effective measures to prevent obesity in future can be promoted by these interventions.[14] These weight-control interventions can be achieved and sustained by providing good support and a variety of strategies to parents.[16]
SCHOOL-BASED INTERVENTIONS
Children spend most of their time in schools. Hence, school plays an important role in the life of the child. There are many school-based intervention strategies. Some interventions focus on nutrition-based or physical-based aspect of weight-control independently, while others jointly focus on both aspects of nutrition and physical activity to achieve the aim of weight control in children.[17] Children take at least one meal at school. Hence, schools can encourage kids to make a healthy food choice like reducing the intake of carbonated drinks or sugary foods, encourage kids to drink healthy fruit juices, water, vegetables, and fruits. Schools which provide meals can have healthy nutritious food items with emphasis on a balanced diet.[18] Schools can involve kids in physical activity by strategies like lengthening the time of physical activity; involving them in moderate to vigorous physical activity for short durations, encouraging them to walk or active commuting, and taking stairs instead of elevators. Kids should be encouraged to participate in various physical activities like games and dance groups with more emphasis on non-competitiveness. Some school-based programs along with the help of community members can help to promote physical education skills and healthy nutrition among children, with focus on implementing this education for maintaining long-term healthy behavior. Classroom-based health education can make older children and teens aware of eating nutritious diet and engaging in regular physical activity.[17]
COMMUNITY-BASED INTERVENTIONS
Community plays a crucial role in healthy lifestyle of children. The term ‘community’ includes the environment around children along with other factors like geographic location, race, ethnicity, and socioeconomic status.[19] This resource can be effectively used to promote healthy nutrition and healthy behavior. Community support is invaluable in implementing interventions and organizing social events like healthy food festivals, harvest festivals, imparting healthy messages, and educating and encouraging people to adopt healthy lifestyle. Thus, community can help children to get affordable and accessible healthy food options and encourage healthy nutrition.[19] Community organizations along with parents can promote nutrition and physical activity-based programs for children, eg., walk to school. Community can make the neighborhood safe and accessible to children and motivate them to increase physical activity.[20] Other programs like providing play groups with safe play grounds and bike paths for kids to play outside will reduce their time spent in front of television sets. Community can provide children with easy accessible facilities like gymnasiums and supervised physical education with strategies such as music for physical activities. Community can influence media or local entertainment to promote healthy educational programs for parents and children. Hence, making them aware of healthy intervention programs via the community is important to reduce childhood obesity.[20]
PLAY-BASED INTERVENTIONS
Instead of just advising children what to eat they can appreciate nutrition-related education in a better way when it comes to them via fun activities like playing games. Some countries are using board games for children to make them understand about balanced diet and thus leading to knowledge gain.[17] Interactive multimedia can be used for interventions. Interactive multimedia like CD ROM can promote healthy nutrition in children with the help of virtual educational games. When these games are used in real-life situations children can make healthy food choices. They can promote decision making and self-esteem for healthy eating behavior. Thus, these programs can help and motivate children to make healthy food choices and also understand the benefits of making such choices.[17] These innovative interventions can encourage children to lead a healthy life.
CHILDHOOD-OBESITY PREVENTION INTERVENTIONS
Preventive programs are conducted to control obesity in children and to modify the social and behavioral aspect of developing obesity. Some of the preventive programs revolve around educating the general population about healthy nutrition and providing information about health problems caused due to childhood obesity.[15] Health care professionals can advise their patients, especially parents, about healthy child nutrition, tackling health problems due to childhood obesity, and benefits of breast feeding among newborn children to prevent weight gain.[21] Federal or state actions to deal with childhood obesity are directing all the food vendors to provide exact calorie readable labels on their products, mentioning calories upfront on menus, restricting advertisements of unhealthy foods, and promoting healthy food making among parents. Some of the other actions are to improve transportation facility for people and children, like providing bike paths, making sidewalks, and providing safe and clean surrounding for children to walk and play eg. no-car roads.[15]
HOSPITAL-BASED INTERVENTIONS
Laboratory investigations of children who are obese and at risk of complications are important. Children aged 7 years and younger with no secondary complications of obesity are advised weight management.[8] Weight-loss programs like dietary management (eating more of fiber-rich foods) and increasing physical activity are recommended for children above 7 years of age with risk of secondary complications. Pharmacological therapy for children with obesity above the age of 12 years can include drugs like orlistat (which blocks fat from the intestine thus giving negative energy balance).[8] Medical professionals are considering the benefits of bariatric surgery in extremely obese children to avoid complications of obesity in adulthood.[22]
POTENTIAL CHANGES
There may be some potential barriers to these interventions, which may make the task of promoting healthy behavior and improving physical activity in children challenging. Some of these challenges are:
FINANCIAL CHALLENGES
Financial investment in these interventions is very crucial. All the intervention-based programs need monitoring of progress and sustainability over many years, which may be costly. In today's world of economic problems funding for such programs is limited.[17] School-based intervention programs require much effort on budgeting and planning, as the cost of educating the teachers about the program, and providing facilities and infrastructure to conduct physical activities is enormous and prohibitive.[17] Communities also find it challenging to make the neighborhood safe for children to play, to organize events, and to provide adequate facilities.
STIGMATIZATION OF OBESE CHILDREN
Obese children are mostly discriminated due to their body image. This may lead to a potential challenge for these children to come forward and opt for healthy programs. Stigmatization of these children by their peers and by others acts as a mental barrier leading to negative body image and fear of food.[17]
LOGISTICAL ISSUES
Literature reviews of school-based interventions conducted in the past have shown mixed outcomes. According to a recent review about school-based interventions for obesity prevention, 17 out of 25 intervention studies were effective in reducing the body mass index.[23] Some interventions targeting physical activity through physical education along with nutritional education worked in reducing obesity. Interventions targeting physical activity education and television viewing were seen to be successful in this review study.[23] While another review addressed school-based interventions by conducting a meta-analysis, concluding that body mass index may not be a good outcome measure among school kids.[24]
US GOVERNMENTAL STRATEGIES TO REDUCE CHILDHOOD OBESITY
According to the Centers for Disease Control and Prevention, identifying effective intervention strategies that can target both improvements in physical activity and providing nutritious diet to reduce childhood obesity are important. These evidence-based programs can be effective in managing obesity in children.[21] Interventions encouraging mothers to breastfeed their babies can be effective in reducing the risk of obesity in children.[21] The United States government is changing the health policies involving transportation, land use, education, agriculture, and economics so that it can have an important impact on healthy environment and health of people in turn reducing obesity.[21] The United States government, along with other health organizations, is developing healthy environments like improving population access to healthy and fresh foods, building walk paths, bike paths, and playgrounds in underserved communities. State governments with the assistance of different health organizations are also getting involved in promoting healthy lifestyles for people. The First Lady has also initiated an obesity prevention and control program titled ‘Let's move’.[21]
FUTURE IMPLICATIONS
Childhood obesity is a major public health problem. Hence, implementation of the available effective intervention programs is essential. Important data regarding evaluation of childhood obesity prevention schemes can be collected and can be used to make stronger and more effective strategies including policy building to reduce future childhood obesity rates.[25]
CONCLUSIONS
Childhood obesity has become a public health crisis, not just in the United States but all over the world. Childhood obesity problem can be reduced by educating children and parents about healthy nutrition and encouraging them to be physically active. There are effective interventions and government policies for prevention and control of childhood obesity. Sustainability of these interventions is a key factor, so that children can adopt these healthy behaviors as a lifelong practice and have a healthy life. This will lead to a nationwide healthy future for the kids.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Centers for Disease Control and Prevention, Overweight and obesity; Defining overweight and obesity. [Last accessed on 2010]. Available from: http://www.cdc.gov/obesity/defining.html .
- 2.Theodore LA, Bray MA, Kehle TJ. Introduction to the special issue: Childhood obesity. Psychol Sch. 2009;46:693–4. [Google Scholar]
- 3.Ribiero RC, Coutinho M, Bramorski MA, Giuliano IC, Pavan J. Association of the waist-to-height ratio with cardiovascular risk factors in children and adolescents: The three cities heart study. Int J Prev Mednone. 2010;1:39–49. [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention, Overweight and obesity; Childhood overweight and obesity. [Last accessed on 2009]. Available from: http://www.cdc.gov/obesity/childhood/defining.html .
- 5.Reilly JJ. Childhood obesity: An overview. Child Soc. 2007;21:390–6. [Google Scholar]
- 6.Ogden C, Carroll M. Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2007–2008. Retrieved from National center for health statistics, Center for Disease Control and Prevention. [Last accessed on 2010]. Available from: http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.pdf .
- 7.Tulchinsky TH, Varavikova EA. The new public health. 2nd ed. Burlington, MA: Elsevier academic press; 2009. [Google Scholar]
- 8.Singhal V, Schwenk WF, Kumar S. Evaluation and management of childhood and adolescent obesity. Mayo Clin Proc. 2007;82:1258–64. doi: 10.4065/82.10.1258. [DOI] [PubMed] [Google Scholar]
- 9.Stamatakis E, Wardle J, Cole TJ. Childhood obesity and overweight prevalence trends in England: Evidence for growing socioeconomic disparities. Int J Obes (Lond) 2010;34:41–7. doi: 10.1038/ijo.2009.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention, Overweight and obesity; childhood overweight and obesity, contributing factors. [Last accessed on 2009]. Available from: http://www.cdc.gov/obesity/childhood/causes.html .
- 11.Perusse L, Bouchard C. Role of genetic factors in childhood obesity and in susceptibility to dietary variations. [Last accessed on 2011 Sept 03];Ann Med. 1999 31:19–25. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10342496 . [PubMed] [Google Scholar]
- 12.Kelishadi R, Ghatrehsamani S, Hosseini M, Mirmoghtadaee P, Mansouri S, Poursafa P. Barriers to physical activity in a population-based sample of children and adolescent in Isfahn, Iran. Int J Prev Med. 2009;1:131–7. [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Overweight and obesity; childhood overweight and obesity, consequences. [Last accessed on 2009]. Available from: http://www.cdc.gov/obesity/childhood/consequences.html .
- 14.Ben-Sefer E, Ben-Natan M, Ehrenfeld M. Childhood obesity: Current literature, policy and implications for practice. Int Nurs Rev. 2009;56:166–73. doi: 10.1111/j.1466-7657.2008.00708.x. [DOI] [PubMed] [Google Scholar]
- 15.Carraro R, García Cebrián M. Role of prevention in the contention of the obesity epidemic. Eur J Clin Nutr. 2003;57(Suppl 1):S94–6. doi: 10.1038/sj.ejcn.1601808. [DOI] [PubMed] [Google Scholar]
- 16.Pott W, Albayrak O, Hebebrand J, Pauli-Pott U. Treating childhood obesity: Family background variables and the child's success in a weight-control intervention. Int J Eat Disord. 2009;42:284–9. doi: 10.1002/eat.20655. [DOI] [PubMed] [Google Scholar]
- 17.Hutchinson G. Tackling obesity through school-based interventions. Br J Sch Nurs. 2010;5:335–7. [Google Scholar]
- 18.Rahman T, Cushing RA, Jackson RJ. Contributions of built environment to childhood obesity. Mt Sinai J Med. 2011;78:49–57. doi: 10.1002/msj.20235. [DOI] [PubMed] [Google Scholar]
- 19.Economos CD, Irish-Hauser S. Community interventions: A brief overview and their application to the obesity epidemic. J Law Med Ethics. 2007;35:131–7. doi: 10.1111/j.1748-720X.2007.00117.x. [DOI] [PubMed] [Google Scholar]
- 20.Tucker P, Irwin JD, Bouck LM, He M, Pollett G. Preventing paediatric obesity; recommendations from a community-based qualitative investigation. Obes Rev. 2006;7:251–60. doi: 10.1111/j.1467-789X.2004.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention (2011) [Last retrieved on 2011 Feb 03];CDC grand rounds: Childhood obesity in the United States. Morbidity and Mortality Weekly Report. 60(02):42–46. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6002a2.htm?s_cid=mm6002a2_w . [PubMed] [Google Scholar]
- 22.Inge TH, Xanthakos SA, Zeller MH. Bariatric surgery for pediatric extreme obesity: Now or later? Int J Obes (Lond) 2007;31:1–14. doi: 10.1038/sj.ijo.0803525. [DOI] [PubMed] [Google Scholar]
- 23.Doak CM, Visscher TLS, Renders CM, Seidell JC. The prevention of overweight and obesity in children and adolescents: A review of interventions and programmes. Obes Rev. 2006;7:111–36. doi: 10.1111/j.1467-789X.2006.00234.x. [DOI] [PubMed] [Google Scholar]
- 24.Kanekar A, Sharma M. Meta-analysis of school-based childhood obesity interventions in the U.K. and U.S. Int Q Community Health Educ. 2009;29:241–56. doi: 10.2190/IQ.29.3.d. [DOI] [PubMed] [Google Scholar]
- 25.Fussenegger D, Pietrobelli A, Widhalm K. Childhood obesity: Political developments in Europe and related perspectives for future action on prevention. Obes Rev. 2008;9:76–82. doi: 10.1111/j.1467-789X.2007.00405.x. [DOI] [PubMed] [Google Scholar]


