Abstract
Background:
In Iran, diarrheal disease is the fourth cause of under five-year mortality. Proper care-seeking behavior and system-based disease management in the national field will have a great effect in reducing morbidity and mortality.
Methods:
This nationwide study was performed on a target population of rural and urban communities; in all 31 provinces of the Islamic Republic of Iran. One lakh three thousand three hundred and thirty one (103331) families were sampled by multi-stage stratified random sampling and were interviewed with a standard data collection form. The collected data was entered into the Stata 8.0 software and analyzed by the survey analysis method.
Results:
Of the 14625 (10.1%) children who were reported to have diarrheal diseases two weeks prior to the interview, 8.8% were cured and 1.5% were not. About 70% of them had at least one visit for health seeking the most of patients were seen by a rural health worker (Behvarz) in the rural and by a general pediatrician in the urban areas. About 62% of the patients in urban and 57% in the rural areas had been treated with antibiotics and these rates for ORS were 51% and 65%, respectively. The factors most related to a care-seeking pattern were the level of routine preventive well-child care, number of siblings, child age, and living area.
Conclusion:
According to this national survey, our health system needs to integrate all the levels of prevention, especially the Integrated Management of Child Illnesses (IMCI) programs with a family physician project. Futher more, there is a great need for empowering the referral system and gate keeping in all referral levels, to make efficient national integrated programs.
Keywords: Diarrhea, antibiotic, health service, national survey, preventive child care, referral system, Iran
INTRODUCTION
Diarrheal diseases are the fourth cause of under-five-year mortality and kills children almost three times more than injuries in I. R. Iran.[1] Proper care-seeking behavior and system-based disease management in national fields have a great effect on reducing the morbidity and mortality.[2]
Childhood diarrheal diseases and acute lower respiratory infections are two of the leading causes of the world's burden of disease.[3] Monitoring the distribution of these diseases in developing countries may be useful in providing information for health policy. Demographic and Health Surveys (DHSs) are possibly the leading sources of maternal and child health data in the developing world, with over 200 DHSs having been conducted in more than 75 developing countries over the last 20 years, often with financial support from the United States Agency for International Development (USAID).[4,5]
The health system in I.R. Iran includes three main levels, which all together form the health system network. There is at least one Medical Science University in each province, which is the official representative of the Ministry of Health and Medical Education (MOHME) in that province. The District Health Network is the official administrator of health and medical care in the districts. The first level of medical service presentations are the Health Houses in rural areas and the Health Posts in urban areas. These Health Houses are situated in most rural areas (86%), but the growing population of the cities prevents the same degree of cover in the urban areas. The health staff who works at the Rural Health Houses is called Behvarz and the staff who work in health posts are health experts, but not medical doctors or general physicians (GP).[6] The GPs, as a family physician team or not, work in the health centers (rural or urban) and officially have to accept the patients who visit the health houses or health posts, who are called Referral patients; and if the patients need more special care the GPs refer them to the third level, for assessing by a medical specialist — in our study a pediatrician.
In I.R. Iran, an integrated program, for evaluation and care giving to children's illnesses, was introduced in January 2000, and expansion to the whole country began in January 2002, and covered 100 percent of the first level of care in health houses and health posts by 2006, but it could not cover the whole country population, especially in the urban area, because of the lack of complete family physician coverage, and only 66 percent of the children had access to this care till 2006. The integrated program has not enough penetration in the country, so the care content is different from patient to patient and from care center to care center, according to the caregiver's knowledge and previous practice.[7] I. R. Iran has established an expanded healthcare system, with non-specialist family physicians on the top of a health team, in the rural regions of the country, since 2005.[8] Recently, the MOHME, coverage of this system to the urban area in the country and our research results could clarify the potential of effectiveness of such an intervention in children's health. Therefore, we assessed the care-seeking pattern for child diarrheal diseases and its related factors during the year 2006, to find the main pattern of rural and urban areas and to find the differences between these, and therefore, to discover the relationship between the care-seeking pattern and the access to the health system and community factors.
METHODS
The data related to the present study has been extracted from the National Integrated Monitoring and Evaluation Survey (IMES on 2006) data bank. This was established in all the cities of I.R.Iran through household survey and a client exit interview. This project comprised of all the families in the urban and rural regions and the participants were sampled by multi-stage stratified and Quota random sampling, with an unequal cluster, considering appropriate sharing of the urban and rural regions for each city within the entire population of the provinces (about 12,000,000 families) with a standardized data collection form. Regarding population differences in the various regions of the country and to estimate an acceptable sampling weight, a selected sample size from each city had been chosen based on the proportion of [Table 1] and the number of individuals, considered as ten families within each cluster. The survey was carried out by groups, including two surveyors who were technicians or experts on Family health and Midwifery. The surveying tool of the standardized questionnaire was based on the DHS questionnaire, but researchers had changed it to adapt it with the content of (Integrated Management of Childhood Illness) IMCI[9] and preventive programs like Well Child Care(WCC).[10]
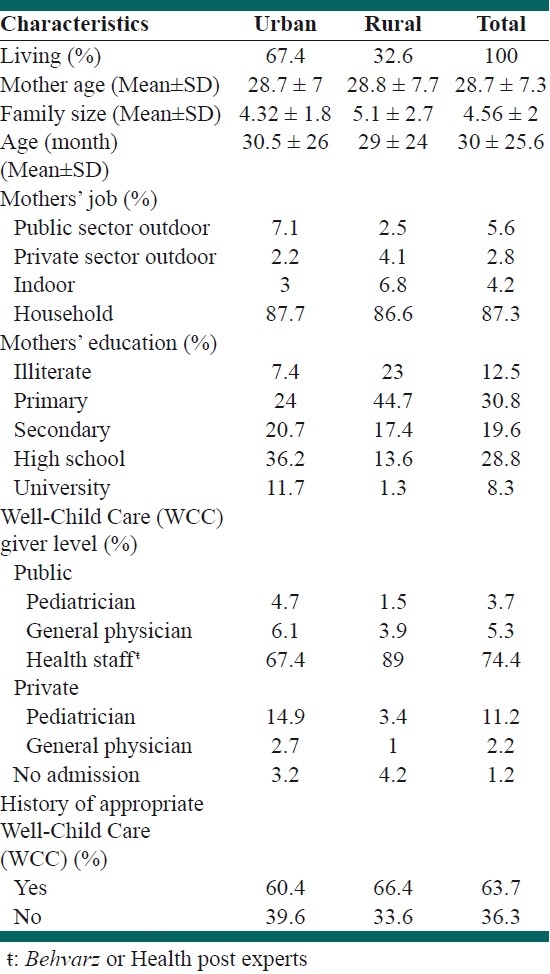
Table 1.
Demographic characteristics of children and their mothers
The items chosen from the questionnaire and their responses employed in the present study have been related to the demographic characteristics of clients (including: living site, maternal job, child age, number of siblings, number of family members, maternal education level, history of routine well-child care visits, and date of interviewing (for adjusting the seasonal pattern), status of utilizing child care during diseases, place and person that presents this care, and also suggestions and treatment plans.
Statistical analysis
The data extracted from the database was coded in this manner: each cluster or service point was coded as a primary sampling unit (PSU) and a proportion of the sampled child number to the urban or rural children population of the under-studied regions as returned to sampling weight, and each university was selected as a specific strata, and then the coded data was entered to STATA 8.0 software[11] and analyzed using the survey analysis statistics methods. All relationship analyses were done using the multinomial regression method. The proportional estimates were employed to perform estimation and a significant level of 0.05 was considered for statistical tests.
RESULTS
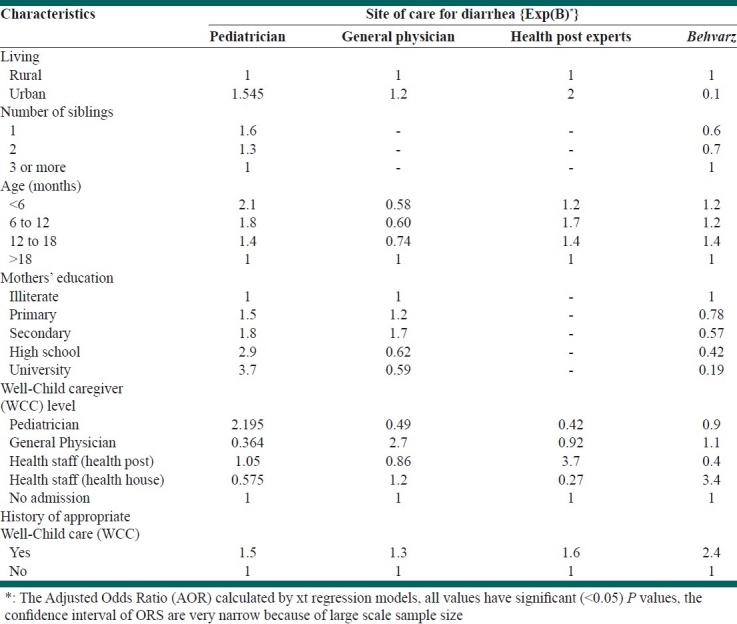
Interviewers visited a total of 103,331 households, where 145,107 children younger than eight years lived. Almost 55 percent of them lived in urban sites and 17.8 percent of the sampled children lived in a city that had a medical university (we called it the big city or academic city). Table 1 shows the demographic features of sampled children and their mothers. Of the 14,625 (10.1%) children who were reported to have diarrheal diseases two weeks prior to the interview, 8.8% were cured and 1.5% continued until interview time, and nearly one-third of them had had at least one co-morbid disease [Figure 1]. About 70% of them had at least one visit for health seeking (69.1% rural versus 70.4% urban residents). Most of them in the rural area were visited by the rural health staff (Behvarz) and in the urban areas by a pediatrician [Table 2]. Only a small group of general physician visits had been done after referring from the lower level (15.2% in urban and 27.9% in rural areas). About 62% of the patients in urban and 57% of them in rural areas had been treated with antibiotics (P<0.05) and the rates for ORS therapy were 51 and 65% (P<0.05), respectively, for urban and rural areas [Tables 3 and 4]. The factors most related to a care-seeking pattern were a history of appropriate preventive well-child care (according to the national guideline), level of the well-child caregiver, child age, maternal education level, number of siblings, and living site. (Logistic regression, P<0.05) [Table 5].
Figure 1.
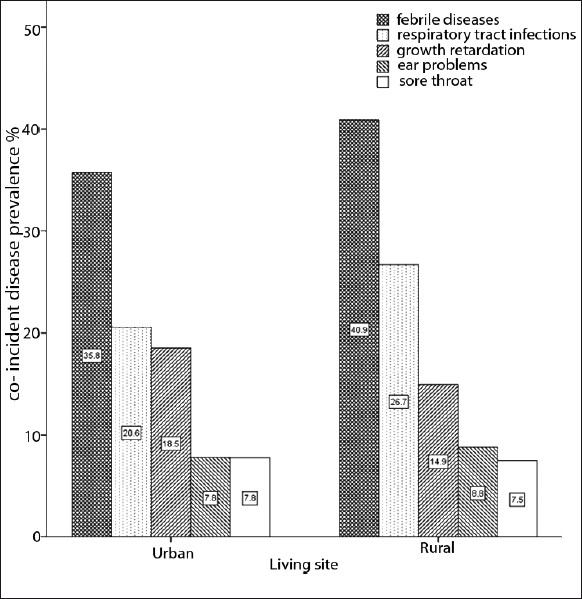
Prevalence of coincident diseases with diarrhea during the last two weeks of interview in children under eight years
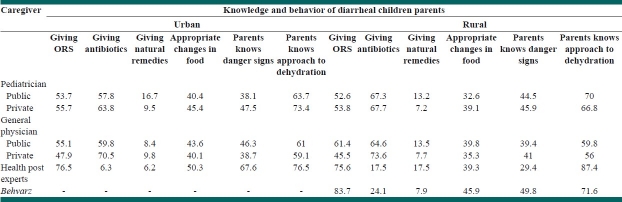
Table 2.
General care pattern for children with diarrheal diseases
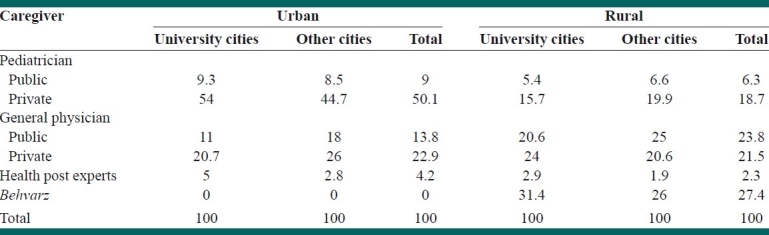
Table 3.
Content of care and prescriptions of variable caregivers for children with diarrheal disease
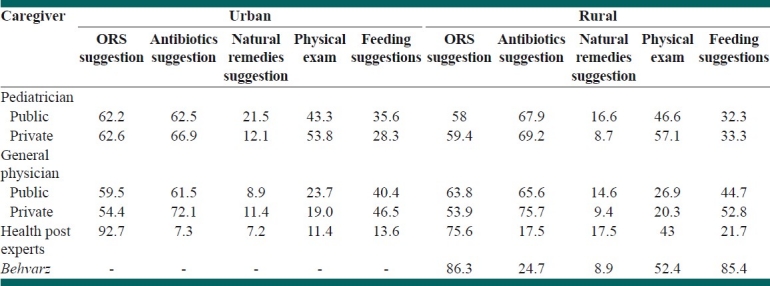
Table 4.
Outcome of care of variable caregivers for children with diarrheal disease
Table 5.
Related factors of care-seeking pattern for children with diarrheal diseases
DISCUSSION
This study did not confirm the past findings of differences in access to health care services among rural children, compared to their urban counterparts (if we accept the ability of rural health house staff (Behvarz) for care giving according to primary health care (PHC) and health service protocols).[12] It also found that there is better access for rural residents to the PHC and preventive wcc than urban citizens. Nevertheless, there is still a great difference between the patterns of care seeking in rural and urban parents, which shows non-adherence to the referral system by urban parents. In the second level of our health service, more than 40 percent of the patients had not received the appropriate and complete content of care [Table 4] and also there was a similar condition in the third level, probably because of the lack of continuity of care and poor system-based practice in our general practitioners and specialists, in both the private and public sectors.[13]
Although IMCI is a naturally effective program,[14,15] to get the best effect from this program we must integrate it with all the levels of health systems in our country and implement this program as a family physician project,[16] because of the very poor implementation of the referral system (less than 15% of the patients had a history of referring from the lower level to the upper level of health care). There is a great need to empower the referral system, at all levels, with a new vision to manage care and insurance mechanisms.[17]
Despite recent changes in the family physician project and its coverage in rural sites, rural children are still at some disadvantage, because of the non-implementation of the referral system and irrational drug usage because of non-health professional orders and traditional drug usage. This study suggests that a higher percentage of appropriate knowledge and behavior among some populations of urban parents may explain, in part, similar reports of a higher socioeconomic level among urban residents.[18] It is well established that introduction of a new policy requires some preliminaries, such as, gathering the opinions of those who will deal with it. Furthermore, it is crucially important to consider the limitations and lack of knowledge at the bottom level to carry out the policy, as sometimes, an organization might function contrary to its own rules and aims.[19] Therefore, it is not unpredictable that our GPs and pediatricians did not have excellent adherence to the health service protocols, because of lack of mutual communications with the health service protocols and fair knowledge about those protocols and programs.[20]
In our study, about 62% of the diarrheal patients in the urban and 57% in the rural areas have been treated with antibiotics. The broad principles of management of acute gastroenteritis in children include oral rehydration therapy, enteral feeding, and diet selection, zinc supplementation and additional therapies such as probiotics. Timely antibiotic therapy in selected cases of diarrhea may reduce the duration and severity of diarrhea and prevent complications. Even as these agents are important to use in specific cases, their widespread and indiscriminate use leads to the development of antimicrobial resistance.[21] Moreover, antibiotics may cause Clostridium difficile-associated diarrhea, also known as antibiotic-associated diarrhea or pseudomembranous colitis, which is a major cause of health care-associated diarrhea. Content of care and prescriptions of variable caregivers for children with diarrheal disease is shown in Table 4. As it is seen, rates of antibiotic suggestion are so high, not only between GPs, but also pediatricians. On the contrary, the rates of ORS suggestion in these two groups of caregivers are less than others. There is an urgent need to scale up the educational and promotional activities with regard to the management of diarrheal disease.[22] For the present, proper, continuous, medical education programs are needed for proper use of antibiotics by physicians, for the management of childhood diarrhea. Obviously, public education is also important and we need a new paradigm toward training family physicians for a better system-based practice.[23]
As our study population was from different socioeconomic levels and we used regression models for the control of rural–urban differences, the most likely explanation for the different care-seeking patterns relates to factors influencing the availability of services. The higher rural rates of visiting by GPs may have been due to higher accessibility of this level of caregivers to rural communities (physical and economical). Specialty care services are often broader in urban areas. It is definitely unclear whether the prevalence of special health care by pediatricians in big cities, which have medical university and tertiary clinics, is much more than in other cities, but it may be due to better accessibility to pediatricians in big cities and lack of the gate keeping system in these areas. This pattern is clearly the opposite for rural residents in big city areas, which shows that the referral system of rural areas works efficiently in big and academic cities, rather than in other cities. Although it is not possible to offer a wide array of specialized services in isolated areas, workforce shortages may still contribute to the unmet tertiary health care in some rural areas, but it is a very small problem.
CONCLUSION
We confront the lack of evidence that helps us to compare our integrated programs in the PHC and our health networks with the different parts of the world, but evidences in the family physician–based care system around the world and this national survey show that we strongly need to integrate all levels of prevention in the child health area, especially in the urban sites, together, to have a cost-effective and complete accessible care for diarrheal diseases in children.
ACKNOWLEDGMENTS
The authors would like to thank the health professionals and health service staff and managers all over the country for their invaluable work and lifelong sacrifice.
Footnotes
Source of Support: This research was funded by the Deputy of Health, Ministry of Health, and Medical Education of I.R.Iran and United Nations Population Fund (UNFPA).
Conflict of Interest: None to declare.
REFERENCES
- 1.World health organization [Internet].Iran (Islamic republic of) health profile. Distribution of causes of death in children under 5 – 2008. [Last accessed on 2011 Sep 02]. Available from: http://www.who.int/gho/countries/irn.pdf .
- 2.Pérez-Cuevas R, Guiscafré H, Romero G, Rodríguez L, Gutiérrez G. Mothers’ health-seeking behavior in acute diarrhea in Tlaxcala, Mexico. J Diarrheal Dis Res. 1996;14:260–8. [PubMed] [Google Scholar]
- 3.Mathers C, Boerma T, MaFat D. Geneva: World Health Organization; 2008. [Last accessed on 2011 Sep 02]. The global burden of disease: 2004 update. Available from: http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.html . [Google Scholar]
- 4.Vaessen M A, Thiam M, Le T. Household Sample Surveys in Developing and Transition Countries. ESA/STAT/AC.85/23. New York: United Nations: Departmentof Economic and Social Affairs, Statistics Division; 2005. The Demographic and Health Surveys; pp. 495–518. [Google Scholar]
- 5.Macro International. Demographic and Health Surveys, Overview. [Last Accessed on 2006 Jan 1]. Available from: http://www measuredhs com/aboutsurveys/dhs/start cfm .
- 6.World Health Organization. Health Systems Profile-Islamic Republic of Iran Regional Health Systems Observatory- EMRO: Executive Summary. World Health Organization. 2000 [Last cited on 2008 Apr 22] [Google Scholar]
- 7.World Health Organization. Regional office of the eastern Mediterranean(EMRO) Child and Adolescent Health and Development, Implementation of IMCI in Iran, Islamic Republic of. [Last cited on 2011 Sep 02]. Available from: http://www.emro.who.int/cah/imci-implementation-ira.htm .
- 8.Khayyati F, Motlagh ME, Kabir MJ, Kazemeini H, Gharibi F, Jafari N. The Role of Family Physician in Case Finding, Referral, and Insurance Coverage in the Rural Areas. Iranian J Publ Health. 2011;40:136–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Technical updates of the guidelines on the IMCI Evidence and recommendations for further adaptations. Geneva: WHO Document Production Services; [Last cited on 2011 Sep 02]. World Health Organization. Available from: http://www.who.int/child_adolescent_health/documents/9241593482/en/index.html . [Google Scholar]
- 10.American Academy of pediatrics [Internet] Recommendations for Preventive Pediatric Health Care. 2008. [Last cited on 2011 Sep 02]. Available from: http://practice.aap.org/content.aspx?aid=1599 .
- 11.Stata Corp. Stata Statistical Software: Release 8. College Station, TX: StataCorp LP; 2003. [Google Scholar]
- 12.Mehryar A. Primary Health Care and the Rural Poor in the Islamic Republic of Iran. Scaling Up Poverty Reduction: A Global Learning Process and Conference Shanghai. 2004. May 25ñ27, [Last cited on 2011 Sep 02]. Available from: http://info.worldbank.org/etools/docs/reducingpoverty/case/22/fullcase/iran%20rural%20healthcare%20full%20case.pdf .
- 13.Sohrabi MR, Mohammad AR. Clients’ Satisfaction with primary health care in Tehran: A cross-sectional study on Iranian Health Centers. J Res Med Sci. 2011;16:756–62. [PMC free article] [PubMed] [Google Scholar]
- 14.Arifeen SE, Hoque DM, Akter T, Rahman M, Hoque ME, Begum K, et al. Effect of the Integrated Management of Childhood Illness strategy on childhood mortality and nutrition in a rural area in Bangladesh: A cluster randomised trial. Lancet. 2009;374:393–403. doi: 10.1016/S0140-6736(09)60828-X. [DOI] [PubMed] [Google Scholar]
- 15.Moti M, Vince JD. Does integrated management of childhood illness (IMCI) make a difference to the assessment of sick children in Papua New Guinea? P N G Med J. 2008;51:138–48. [PubMed] [Google Scholar]
- 16.Paranhos VD, Pina JC, Mello DF. Integrated management of childhood illness with the focus on caregivers: an integrative literature review. Rev Lat Am Enfermagem. 2011;19:203–11. doi: 10.1590/s0104-11692011000100027. [DOI] [PubMed] [Google Scholar]
- 17.Franco LM, Diop FP, Burgert CR, Kelley AG, Makinen M, Simpara CH. Effects of mutual health organizations on use of priority health-care services in urban and rural Mali: A case-control study. Bull World Health Organ. 2008;86:830–8. doi: 10.2471/BLT.08.051045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sreeramareddy CT, Shankar RP, Sreekumaranl BV, Subba1 SH, Joshi1 HS, Ramachandran U. Care seeking behavior for childhood illness- a questionnaire survey in western Nepal. BMC Int Health Hum Rights. 2006;6:7. doi: 10.1186/1472-698X-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zolala1 F, Haghdoost AA. A gap between policy and practice: A case study on maternal mortality reports, Kerman, Iran. Int J Prev Med. 2011;2:88–93. [PMC free article] [PubMed] [Google Scholar]
- 20.Amini-Ranjbar S, Bavafa B. Physicians’ Knowledge Regarding Nutritional Management in Children with Diarrhea: A study in Kerman, Iran (I.R.) Pak J Nutr. 2007;6:638–40. [Google Scholar]
- 21.Bhutta ZA. Acute gastroenteritis in children. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson Textbook of Pediatrics. 18th ed. Philadelphia: Elsevier Saunders; 2007. pp. 1605–17. [Google Scholar]
- 22.Ogunrinde OG, Raji T, Owolabi OA, Anigo KM. Knowledge, attitude and practice of home management of childhood diarrhea among Caregivers of Under-5 Children with Diarrheal Disease in Northwestern Nigeria. J Trop Pediatr. 2011 doi: 10.1093/tropej/fmr048. [In Press] [DOI] [PubMed] [Google Scholar]
- 23.Lebaron SW, Schultz SH. Family medicine in Iran: The birth of a new specialty. Fam Med. 2005;37:502–5. [PubMed] [Google Scholar]