Abstract
The current report examines the rates of psychiatric comorbidity in a sample of 539 primary care patients diagnosed with anxiety disorders using the Structured Clinical Interview for DSM-IV (SCID-IV). Though not a typical psychiatric sample, rates of comorbidity were found to be as high or higher than those reported in studies conducted in traditional mental health settings. Multiple anxiety disorders were diagnosed in over 60% of participants and over 70% of participants had more than one current axis I diagnosis. Rates of current and lifetime comorbid major depression were also very high. Patterns of diagnostic comorbidity were also examined, with significantly elevated risks for the co-occurrence of several specific pairings of disorders being found. The study results are discussed in context of a recently published, large-scale study of anxiety disorder comorbidity in psychiatric patients (Brown et al., 2001). Implications of these results for both the mental health and primary care fields are also discussed.
Epidemiological and clinical studies consistently document high rates of comorbidity in patients diagnosed with anxiety and mood disorders.1–5 In studies of clinical samples, 50% or more of patients with a primary anxiety disorder have at least one additional anxiety or mood disorder.6–8 Rates of comorbidity for certain individual disorders can be even higher.9,10 Such significant rates of comorbidity have prompted numerous critiques of the current DSM-based diagnostic nosology,11,12 and several intriguing theoretical models to explain the common diagnostic overlap.13
The consistent results from comorbidity studies point to an important and pragmatic clinical reality: A patient presenting for treatment with a single anxiety or mood disorder without an additional current or historical axis I condition would be a rare exception rather than the rule. As such, these comorbidity findings may be of heuristic value to clinicians involved in patient diagnostic conceptualization and treatment planning, given the poor clinical outcomes associated with comorbid conditions.14 The robustness of the comorbidity data begs additional questions about the aggregation of anxiety and mood disorders and if specific patterns of comorbidity exist.
In a recent study of anxiety disorder comorbidity, Brown et al.15 reported high comorbidity rates in a large sample (N = 1,127) of anxiety and mood disorder patients seeking treatment at a university-based clinic specializing in the treatment of anxiety disorders. Overall, they found 57% of patients with a principal anxiety or mood disorder had an additional current axis I disorder and 81% had a lifetime history of one. Reported rates of comorbidity for specific anxiety and mood disorders were even higher. Notable among these were generalized anxiety disorder (GAD) patients, of whom 65% had a current and 88% had a lifetime comorbid anxiety or mood disorder, and post-traumatic stress disorder (PTSD) patients with 92% current and 100% lifetime comorbidity rates.
While illustrating the high rates of co-occurrence of DSM-IV16 anxiety and mood disorders, results from the Brown et al.15 study need to be considered within the context of the study sample. All study participants were seeking treatment at a clinic specializing in the treatment of anxiety and mood disorders. Since seeking treatment is associated with both illness severity and diagnostic comorbidity (i.e., “Berkson’s bias”17), the generalizability of these comorbidity rates to non–treatment-seeking samples may be inappropriate. Furthermore, the applicability of the comorbidity rates to patients seeking treatment in other settings is questionable.
To date, psychological and psychiatric research has only begun to examine the problem of anxiety disorders in the primary care setting, focusing mostly on issues of prevalence, poor diagnostic recognition, significant costs, or disability of these patients.18–27 No studies have attempted to comprehensively examine the rates and patterns of diagnostic comorbidity in a primary care population, which is a notable departure from the traditional psychiatric treatment–seeking samples of prior comorbidity studies.7,8,15 In the present study, we hope to bridge this gap in the comorbidity literature by examining rates and patterns of anxiety disorder comorbidity in a large sample of primary care patients enrolled in the Primary Care Anxiety Project (PCAP), a longitudinal study of the course of anxiety disorders in primary care. PCAP is not a treatment study, nor is it a study of the treatment of anxiety within the primary care and general medical setting. Rather, PCAP is a naturalistic examination of the long-term course of anxiety disorders among primary care patients, with the main study inclusion criteria being that the patient had a medical appointment scheduled on the day of initial screening.
METHOD
Participants
Participants were 539 primary care patients recruited from physician offices and medical clinics throughout New England. The majority (76%) of the sample were female with an average participant age of 39.1 years (SD 11.6). PCAP participants were fairly well educated, with 90% of the sample reporting at least a high school degree or GED, and 24% having an associates degree or better. With regard to marital status at intake, 27% of participants were single, 50% married, and 19% divorced. The racial/ethnic breakdown of the sample was as follows: 83% Caucasian, 8% African-American, 9% other.
Participant Recruitment and Assessment
Participants were recruited from 15 internal medicine and family medicine practices in New Hampshire, Massachusetts, Rhode Island, and Vermont. Five sites were located in rural areas and 10 sites were in urban or suburban areas. Four of the sites were small, private practices, four were free-standing clinics with a university affiliation, and seven were large university teaching hospital–based clinics.
Recruitment for PCAP began in July 1997. For inclusion in the study, participants needed to be a minimum of 18 years of age, English speaking, and scheduled for a general medical appointment on the day of recruitment. Participants were excluded from the study if they were suffering from active psychosis, had no current address and phone number, or were pregnant.
Participants were recruited on the day of a visit to the medical practice. A research assistant approached eligible patients of the clinic in the practice waiting room, asking them if they were interested in participating in a study to gather information on different types of stress or nervousness that some people experience. Interested participants signed a statement indicating their voluntary informed consent to participate in the study prior to completion of any study measures. They then completed a screening form that assessed for the presence of key features of DSM-IV anxiety disorders. Patients screening positive were invited for a full diagnostic interview.
Measures
Anxiety screener
A 32-item self-report anxiety screener was developed for PCAP to assess the presence of essential features of DSM-IV anxiety disorders. The questions on the instrument were derived directly from DSM-IV diagnostic criteria. Sample items include “Have you ever had a sudden attack when you felt afraid or anxious and did not know why?” and “In the past month have you been anxious or worried more days than not, even when you tried not to worry?”
The anxiety screening form was designed to be highly sensitive to the presence of any anxiety disorder symptoms, so as to intentionally over sample potential participants and reduce the chances of false negatives. In a separate validation study of this measure, 64 primary care patients completed both the screening form and the Structured Clinical Interview for DSM-IV (SCID-IV).28 The interviewers administering the SCID-IV were blind to the results of the screening measure. Of 38 individuals who screened negative, none were positive for an anxiety disorder according to the SCID-IV; there were no false negatives. Twenty-six participants screened positive. Eight of these (31%) were true positives (SCID-IV positive for an anxiety disorder). Eighteen (69%) were false positives (screen-positive—SCID-negative). One participant who screened negative was excluded at the SCID for psychotic symptoms.
Clinical interview
All clinical diagnoses were established by means of in-person diagnostic interviews that employed the SCID-IV,28 a frequently used and well-validated assessment instrument. In PCAP, the psychotic screen, mood, anxiety, substance use, and eating disorders modules of the SCID-IV were administered. Since the primary interest of PCAP was to recruit patients with anxiety disorders, the SCID-IV was reordered so that the anxiety disorders module was administered first, with participants completing a full battery only if they were diagnosed positive for an anxiety disorder.
All clinical interviewers had at least a bachelors degree in psychology and underwent a rigorous, multi-stage training program employed with excellent results in other large-scale research studies conducted through the Brown Psychiatry Department. Interviewers received an initial introduction to the SCID-IV by reading the instrument’s user’s manual29 and watching the New York State Psychiatric Institute videotape series on SCID administration.30 Next, interviewers participated in several role-played interviews with trained research staff functioning as patients to practice SCID-IV administration. All interviewers were next required to observe a minimum of three SCID-IV batteries conducted by trained interviewers, followed by performing a minimum of three SCID-IV interviews themselves under the supervision of SCID-trained clinical staff. Finally, all interviewers were required to conduct a SCID interview under observation by a doctoral level psychologist trained in administering the SCID-IV, before being certified to conduct SCID-IV interviews independently.
To ensure accuracy of diagnosis, SCID-IV interviews were routinely reviewed at PCAP staff meetings where issues regarding diagnosis were resolved through consultation with other interviewers, senior research assistants, and doctoral-level clinicians. In addition, a narrative report for each SCID-IV interview was composed. This report was reviewed and edited by senior research staff that included doctoral-level clinicians to resolve any remaining clinical questions. DSM-IV diagnostic rules were strictly adhered to throughout the assessment process, including hierarchical and exclusionary criteria regarding conditions or symptoms due to general medical conditions or psychoactive substances.
Statistical Analyses
Replicating the methodology employed by Brown et al.,15 rates and patterns of diagnostic comorbidity were examined by calculating the percentage of PCAP participants having different pairings of co-occurring disorders. The relative risk of the disorders co-occurring was then calculated and the statistical significance of this risk was determined using a 95% confidence interval criterion derived from a chi-square analysis. All risks of specific disorder pairings were calculated using participants in the sample without the particular index anxiety disorder of interest as the comparison group. These analyses were conducted both for current and lifetime diagnoses. Analyses were conducting using SAS version 8.2 using PROC FREQ, and PROC MEANS (SAS Institute, Cary, NC).
RESULTS
Initial Screening and Sample Disgnostic Composition
A total of 14,320 eligible patients were approached; 4,383 potential participants (31% of approached patients) completed the questionnaire screening for symptoms of anxiety and 9,937 refused to complete the screening form. Of those participants completing the screener, 2,755 participants (63%) screened positive for anxiety symptoms. The SCID-IV was administered to 1,634 potential participants who screened positive (456 patients who screened positive refused to participate in the SCID, 665 patients who screened positive repeatedly cancelled or failed to show up for their SCID appointments).
There were no significant differences in age, gender, marital status, or education between the participants who screened positive and completed the SCID-IV and those who screened positive and did not complete the interview. The only demographic factor that differed between the groups was race, with those individuals completing the SCID-IV being more likely to be white [χ2 (1) = 18.54, P < .001]. Although this difference was statistically significant, in part due to the large number in each group, the actual percentage did not differ greatly between the two groups; 81% of those interviewed were white, as compared to 74% of those who screened positive but refused the interview. The difference was not significantly attributable to a particular ethnic minority.
Of the 1,634 participants who completed the SCID-IV, 539 met criteria for one or more of the following index anxiety disorders and were enrolled in the study: panic disorder (PD; n = 86) panic disorder with agoraphobia (PDA; n = 149), agoraphobia without history of panic disorder (AWOPD; n = 23), generalized anxiety disorder (GAD; n = 135), social phobia (SOC; n = 182), post-traumatic stress disorder (PTSD; n = 199), mixed anxiety-depressive disorder (MAD; n = 10), or generalized anxiety disorder features occurring exclusively within the course of a mood disorder (GAD/major depressive disorder [MDD]; n = 28). This last category was created for exploratory purposes to capture individuals who met full DSM-IV criteria for GAD, with the exception that their symptoms occurred exclusively during the course of a mood disorder. However, this diagnosis was not counted as an anxiety disorder for any of the analyses in this report. Diagnoses of MAD were made based on the provisional diagnostic criteria set published in the DSM-IV appendix, with the exclusionary rule of no past history of major depression, GAD, or PD waived in order to include more potential MAD cases to study. Additionally, diagnoses of obsessive compulsive disorder (OCD; n = 39) and specific phobia (n = 92) were made at intake, but only as comorbid conditions as they were not among the identified index anxiety disorders required for inclusion in the study.
Comorbidity of Axis I Disorders
Current comorbidity
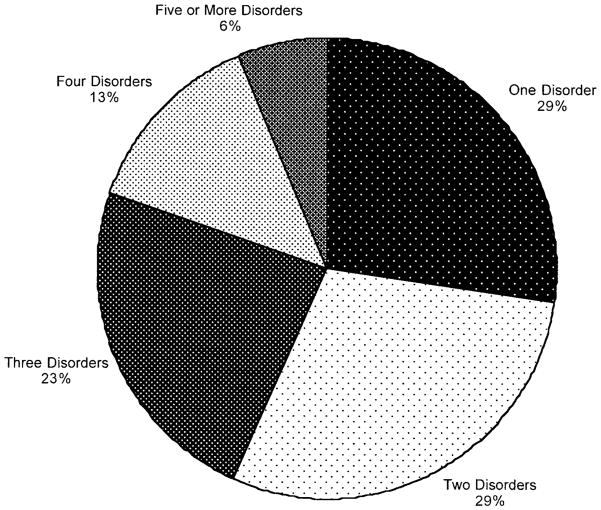
Figure 1 depicts the rates of comorbidity in the overall PCAP sample (N = 539). As can be seen in the chart, more than 70% of the PCAP sample could be diagnosed with multiple current axis I disorders at the time of study intake, with 19% having four or more current axis I conditions.
Fig 1.
Percentages of PCAP participants with multiple current comorbid diagnoses.
Table 1 presents the rates and patterns of current comorbid diagnoses for patients with current DSM-IV diagnoses (N = 516)* of PD, PDA, AWOPD, SOC, PTSD, and GAD. Comorbid diagnoses were very common in this sample. Looking at each disorder individually, over 79% of participants with a given anxiety diagnosis had more than one current axis I disorder, over 60% of participants had more than one anxiety disorder, and over 40% had comorbid MDD.
Table 1.
Overall Percentage Rates (relative risks) of Current Comorbid Diagnoses With DSM-IV Anxiety Disorders
| Co-occurring Diagnosis | Anxiety Diagnosis
|
||||||
|---|---|---|---|---|---|---|---|
| PD (n = 86) | PDA (n = 149) | PD/A (n = 235) | AWOPD (n = 23) | SOC (n = 182) | PTSD (n = 199) | GAD (n = 135) | |
| Any axis Ia | 68 | 126 | 194 | 19 | 156 | 160 | 107 |
| 79% (1.10) | 85% (1.23*) | 83% (1.26*) | 83% (1.13) | 86% (1.29*) | 80% (1.17*) | 79% (1.11*) | |
| Any anxiety/moodb | 63 | 123 | 186 | 19 | 154 | 159 | 103 |
| 73% (1.05) | 83% (1.26*) | 79% (1.26*) | 83% (1.18) | 85% (1.35*) | 80% (1.24*) | 76% (1.12*) | |
| Any anxietyc | 53 | 103 | 156 | 17 | 129 | 134 | 82 |
| 62% (1.29*) | 69% (1.64*) | 66% (1.83*) | 74% (1.51*) | 71% (1.84*) | 67% (1.72*) | 61% (1.31*) | |
| Any moodd | 39 | 76 | 115 | 11 | 96 | 97 | 64 |
| 45% (.97) | 51% (1.13) | 49% (1.09) | 48% (1.02) | 53% (1.22*) | 49% (1.07) | 47% (1.02) | |
| MDD | 36 | 68 | 104 | 10 | 81 | 84 | 57 |
| 42% (1.05) | 46% (1.20) | 44% (1.20) | 43% (1.08) | 45% (1.17) | 42% (1.08) | 42% (1.07) | |
| Anxiety disorders | |||||||
| PD | 17 | 27 | 15 | ||||
| – | – | – | – | 9% (.45*) | 14% (.73) | 11% (.60) | |
| PDA | 48 | 49 | 32 | ||||
| – | – | – | – | 26% (.87) | 25% (.78) | 24% (.77) | |
| PD/A | 65 | 76 | 49 | ||||
| – | – | – | – | 36% (.70*) | 38% (.76*) | 35% (.61*) | |
| AWOPD | 7 | 8 | 4 | ||||
| – | – | – | – | 4% (.80) | 4% (.85) | 3% (.59) | |
| SOC | 17 | 48 | 65 | 7 | 68 | 29 | |
| 20% (.52*) | 32% (.88) | 28% (.66) | 30% (.86) | – | 34% (.95) | 21% (.54*) | |
| PTSD | 27 | 49 | 76 | 8 | 68 | 19 | |
| 31% (.78) | 33% (.80) | 32% (.74*) | 35% (.90) | 37% (.95) | – | 14% (.30*) | |
| GAD | 15 | 32 | 47 | 4 | 39 | 19 | |
| 17% (.63) | 22% (.77) | 20% (.64*) | 17% (.65) | 16% (.50*) | 10% (.26*) | – | |
| Other anxiety disorders | |||||||
| OCD | 6 | 14 | 20 | 2 | 14 | 16 | 11 |
| 7% (.91) | 9% (1.38) | 9% (1.26) | 9% (1.16) | 8% (1.03) | 8% (1.11) | 8% (1.11) | |
| SPEC | 16 | 37 | 53 | 3 | 38 | 42 | 24 |
| 19% (1.07) | 25% (1.69*) | 23% (1.67*) | 13% (.73) | 21% (1.32) | 21% (1.37) | 18% (1.01) | |
| Other diagnosis | |||||||
| SUD | 8 | 20 | 28 | 4 | 17 | 17 | 21 |
| 9% (.91) | 13% (1.54) | 15% (1.40) | 17% (1.79) | 9% (.89) | 13% (.77) | 16% (1.91*) | |
| Eating disorder | 13 | 18 | 29 | 3 | 20 | 33 | 9 |
| 13% (1.31) | 12% (1.27) | 12% (1.44) | 13% (1.29) | 11% (1.11) | 17% (2.63*) | 7% (.58) | |
NOTE. When the category listed in the column is present, the number and percentage of participants diagnosed with condition listed in the rows is indicated. The relative risk of having the diagnosis is printed in parenthesis and was calculated using participants without the index disorder denoted in the column as the comparison group. Dashes indicate the percentage or relative risk is inapplicable.
Denotes significantly increased or decreased risk of co-occurring condition (95% confidence interval).
Any additional anxiety, mood, substance use, or other psychiatric diagnosis.
Any additional anxiety disorder (including OCD and SPEC) or mood (including MDD, dysthymia, bipolar I and II, depression NOS).
Any additional anxiety disorder (including OCD and SPEC).
Any additional mood disorder (including MDD, dysthymia, bipolar I and II, depression NOS).
Abbreviations: PD, panic disorder; PDA, panic disorder with agoraphobia; PD/A, PD or PDA; AWOPD, agoraphobia without a history of panic disorder; SOC, social phobia; PTSD, post-traumatic stress disorder; GAD, generalized anxiety disorder; MDD, major depressive disorder; OCD, obsessive compulsive disorder; SPEC, specific phobia; SUD, alcohol or drug use disorder.
The relative risk (RR) of the co-occurrence of specific anxiety disorders and diagnostic conditions were also examined. Except for PD and AWOPD, all intake anxiety disorders carried significant risks of having an additional comorbid axis I diagnosis and all had a risk of an additional anxiety disorder diagnosis. Even though there was a high prevalence of MDD in the PCAP sample, only SOC demonstrated a statistically significant risk of having an additional current mood disorder diagnosis. No disorder showed a significant association with having current MDD. Also, none of the index anxiety disorders showed an increased risk of co-occurrence with another index anxiety disorder. Rather, most index anxiety disorders showed either no association or a significantly decreased risk of comorbidity with another specific anxiety disorder.
Examining the risk of co-occurrence between an index anxiety disorder and a non-index axis I diagnosis, patients with PDA showed an increased risk of a comorbid specific phobia. Patients with PTSD also demonstrated an increased risk of having an additional current comorbid eating disorder. Surprisingly, GAD showed an increased risk of a current comorbid alcohol or substance use diagnosis (SUD).
Lifetime comorbidity
Rates of lifetime comorbidity were also extremely high (Table 2). With the exception of participants with the AWOPD diagnosis, more than 90% of participants were diagnosed as having a history of at least two axis I conditions. More than 70% of PCAP participants with PDA, AWOPD, SOC, and PTSD had a lifetime history of more than one anxiety disorder. Over 70% of PCAP patients had a lifetime history of an additional mood diagnosis, with between 64% and 78% having a lifetime history of MDD. The highest percentages of lifetime MDD was found for participants diagnosed with SOC and PTSD. With the exception of GAD, more than 50% of participants in each anxiety disorder category met lifetime diagnostic criteria for a SUD.
Table 2.
Overall Percentage Rates (relative risks) of Lifetime Comorbid Diagnoses With DSM-IV Anxiety Disorders
| Co-occurring Diagnosis | Anxiety Diagnosis
|
||||||
|---|---|---|---|---|---|---|---|
| PD (n = 104) | PDA (n = 159) | PD/A (n = 263) | AWOPD (n = 25) | SOC (n = 190) | PTSD (n = 208) | GAD (n = 135) | |
| Any axis Ia | 97 | 154 | 251 | 22 | 186 | 203 | 124 |
| 93% (1.00) | 97% (1.06*) | 95% (1.05*) | 88% (.94) | 98% (1.08*) | 98% (1.08*) | 92% (.98) | |
| Any anxiety/moodb | 89 | 147 | 236 | 22 | 181 | 199 | 118 |
| 86% (.97) | 92% (1.09*) | 90% (1.06) | 88% (1.01) | 95% (1.15*) | 96% (1.17*) | 87% (1.00) | |
| Any anxietyc | 71 | 119 | 190 | 19 | 143 | 152 | 91 |
| 68% (1.30*) | 75% (1.58*) | 72% (1.87*) | 76% (1.39*) | 75% (1.69*) | 73% (1.66*) | 67% (1.30*) | |
| Any moodd | 79 | 125 | 204 | 18 | 167 | 183 | 96 |
| 76% (.96) | 79% (1.01) | 78% (.98) | 72% (.92) | 88% (1.21*) | 88% (1.23*) | 71% (.88*) | |
| MDD | 73 | 118 | 191 | 17 | 149 | 167 | 86 |
| 70% (.98) | 74% (1.06) | 73% (1.03) | 68% (.95) | 78% (1.16*) | 80% (1.22*) | 64% (.86*) | |
| Anxiety disorders | |||||||
| PD | 26 | 38 | 21 | ||||
| – | – | – | – | 14% (.57*) | 18% (.85) | 16% (.71) | |
| PDA | 58 | 58 | 37 | ||||
| – | – | – | – | 31% (.99) | 28% (.85) | 27% (.86) | |
| PD/A | 84 | 96 | 58 | ||||
| – | – | – | – | 44% (.81*) | 46% (.85) | 43% (.80*) | |
| AWOPD | 8 | 9 | 4 | ||||
| – | – | – | – | 4% (.81) | 4% (.83) | 3% (.54) | |
| SOC | 26 | 58 | 84 | 8 | 76 | 32 | |
| 25% (.63*) | 37% (.99) | 32% (.76*) | 32% (.86) | – | 37% (.99) | 24% (.57*) | |
| PTSD | 38 | 58 | 96 | 9 | 76 | 21 | |
| 37% (.89) | 36% (.87) | 37% (.82) | 36% (.89) | 40% (.99) | – | 16% (.32*) | |
| GAD | 21 | 37 | 58 | 4 | 32 | 21 | |
| 20% (.73) | 23% (.85) | 22% (.72*) | 16% (.60) | 17% (.53) | 10% (.27*) | – | |
| Other anxiety disorders | |||||||
| OCD | 8 | 17 | 25 | 3 | 19 | 22 | 12 |
| 8% (.83) | 11% (1.31) | 10% (1.15) | 12% (1.37) | 10% (1.21) | 11% (1.36) | 9% (1.00) | |
| SPEC | 17 | 41 | 58 | 4 | 43 | 45 | 27 |
| 16% (.85) | 26% (1.67*) | 22% (1.47*) | 16% (.85) | 23% (1.39) | 22% (1.31) | 20% (1.10) | |
| Other diagnosis | |||||||
| SUD | 52 | 90 | 142 | 13 | 110 | 127 | 64 |
| 50% (.92) | 57% (1.09) | 54% (1.02) | 52% (.97) | 58% (1.14) | 61% (1.26*) | 47% (.85) | |
| Eating disorder | 16 | 25 | 41 | 5 | 32 | 46 | 14 |
| 15% (1.06) | 16% (1.10) | 16% (1.13) | 20% (1.38) | 17% (1.25) | 22% (2.27*) | 10% (.64) | |
NOTE. When the category listed in the column is present, the number and percentage of participants diagnosed with condition listed in the rows is indicated. The relative risk of having the diagnosis is printed in parenthesis and was calculated using participants without the index disorder denoted in the column as the comparison group. Dashes indicate the percentage or relative risk is inapplicable.
Denotes significantly increased or decreased risk of co-occurring condition (95% confidence interval).
Any additional anxiety, mood, substance use, or other psychiatric diagnosis.
Any additional anxiety disorder (including OCD and SPEC) or mood (including MDD, dysthymia, bipolar I and II, depression NOS).
Any additional anxiety disorder (including OCD and SPEC).
Any additional mood disorder (including MDD, dysthymia, bipolar I and II, depression NOS).
Abbreviations: PD, panic disorder; PDA, panic disorder with agoraphobia; PD/A, PD or PDA; AWOPD, agoraphobia without a history of panic disorder; SOC, social phobia; PTSD, post-traumatic stress disorder; GAD, generalized anxiety disorder; MDD, major depressive disorder; OCD, obsessive compulsive disorder; SPEC, specific phobia; SUD, alcohol or drug use disorder.
The RRs of the lifetime co-occurrence of specific anxiety disorders and diagnostic conditions were also examined. Slightly, but significantly elevated risks of additional lifetime axis I disorders were found for PDA, PD, SOC, and PTSD. As was the case with current comorbidity, all anxiety disorder categories had significantly elevated risks of an additional lifetime anxiety diagnosis. Unlike the case for current comorbidity, both SOC and PTSD had significantly elevated risks of both a lifetime mood disorder and lifetime MDD.
No anxiety disorder showed a significantly increased risk of lifetime co-occurrence with another specific anxiety disorder. Rather, most anxiety disorders showed either no association, or significantly decreased risks of lifetime comorbidity with another specific anxiety disorder. The notably reduced lifetime risks of comorbid GAD given PTSD and comorbid PTSD given GAD were likely the result of the DSM-IV hierarchy rule excluding the diagnosis of GAD if it occurs solely during the course of PTSD.
Among the non-index disorders, lifetime rates of specific phobia were significantly elevated for participants with PDA and PD. Lifetime risk of SUD was significantly elevated for participants with PTSD. Patients with lifetime PTSD also showed a signifcantly increased risk of lifetime eating disorders. Unlike the case with current comorbidity, patients with lifetime GAD showed no risk of lifetime SUD.
DISCUSSION
As was the case in other studies employing both DSM-III-R7,8 and DSM-IV diagnostic criteria,15 analysis of the PCAP sample revealed significant rates of comorbidity for current and lifetime anxiety and mood disorders. The typical PCAP patient had multiple comorbid Axis I conditions. More than 40% of the sample was currently in episode of MDD at intake and 70% had a lifetime history of the disorder. Alcohol abuse or SUD was diagnosed currently in 14% of participants, but half met lifetime criteria for either disorder. More than 80% of the PCAP sample reported a lifetime history of at least one additional axis I condition. Our results provide further evidence that mental illnesses in general, and anxiety and mood disorders in particular, rarely exist in isolation from one another.
The high rates of comorbidity found in PCAP are all the more striking since the sample is composed of primary care patients and not treatment-seeking psychiatric patients. Seeking treatment for psychiatric problems has often been considered to be an indication that patients are “sicker” and more impaired than individuals with psychiatric problems who do not seek treatment.17 That rates of comorbidity in PCAP were similar to, if not higher than those reported in traditional psychiatric treatment-seeking clinical samples suggests that this may not necessarily be the case. The main requirement for inclusion in PCAP was that the participant had a medical appointment scheduled the day of screening. While some appointments may have been related to emotional problems, and some participants were receiving mental health treatment from outside sources, additional studies by our research group indicate a substantial proportion of PCAP patients were not receiving treatment for their mental illnesses.31,32 The comorbidity rates found in PCAP further argue against the notion that patients who seek and receive treatment at a specialized mental health clinic are more severely ill or impaired than those who seek and receive treatment in primary care settings. These data add to arguments that anxiety disorders in primary care represent a significant problem requiring additional research and resources.18,33–35
There are some limitations to the present study. A large proportion of potential subjects refused initial screening and a significant number screening positive failed to complete the SCID-IV. It is unknown what biases may have been introduced into the sample as a result of these refusals. It is possible that the individuals comprising PCAP were in some way self-selected by a greater awareness and/or concern about their mental health, which may have affected the observed comorbidity rates. Thus, the generalizability of the current findings to a truly random sample of primary care patients with anxiety disorders is not appropriate. Similarly, because the actual level of psychopathology that existed in study refusers is unknown, our results cannot be considered in an epidemiological fashion to reflect the prevalence of anxiety disorder comorbidity in the general primary care population. Also, because nearly half of our participants were receiving some form of mental health treatment from either a mental health professional or their primary care physician, the generalizability of our comorbidity rates to a completely untreated or a mental health treatment-naive population is limited. With these sample characteristics in mind, however, our results do still provide some insight into the rates of axis I comorbidity among primary care patients with anxiety disorders.
The present study attempted to replicate some of the analyses performed by Brown et al.15 for purposes of direct comparison between a sample seeking mental health treatment in a specialty anxiety disorders clinic and a primary care sample. In general, the percentages of the PCAP sample with specific DSM-IV anxiety disorder comorbidities were comparable, if not slightly higher than those reported by Brown et al. Additionally, the relative risks of diagnostic co-occurrence found among PCAP participants were not discrepant from those reported in Brown et al.15 in most circumstances. There were, however, two instances where our relative risk findings do not agree with those found by Brown et al. Specifically, Brown et al. reported a significantly elevated risk of the current and lifetime co-occurrence of PD and PTSD and for the lifetime co-occurrence of SOC and GAD. In the PCAP sample, we found no association for panic and PTSD and significantly reduced risks for SOC and GAD.
Besides being a sample of primary care patients rather than a self-identified, psychiatric treatment–seeking sample, the PCAP sample differs from the Brown et al.15 sample in several important ways. PCAP included a higher proportion of participants with PD without agoraphobia and PTSD, as well as a sample of participants diagnosed with AWOPD. Also, PCAP only included patients meeting criteria for one of nine index anxiety disorders, whereas Brown and colleagues included patients with complaints of both anxiety and mood disorders. Further, the PCAP sample had a slightly higher rate of current and lifetime comorbid MDD than that found in Brown et al. (40% and 71% PCAP, v 28% and 54% Brown et al., respectively). These differences in basic sample composition may explain some of the differences in relative risk of comorbidity noted between the two samples. On the other hand, in the majority of cases the percentages of PCAP participants with specific comorbidities were not meaningfully different from those reported by Brown et al. This would suggest that both studies may have with some degree of accuracy detected the rates, proportions, and patterns of diagnostic comorbidity in DSM-IV mood and anxiety disorders.
Interestingly, all index anxiety disorders showed an elevated risk of current and lifetime anxiety disorder comorbidity. However, risks of specific anxiety disorder pairings tended to show either no association or a significantly decreased risk of comorbidity. Thus, it appears that the increased risk of current and lifetime anxiety disorder comorbidity may be a nonspecific one. That is, having one anxiety disorder may increase one’s risk of having one or more additional disorders of anxiety in general, but not any one anxiety disorder in particular. Others have suggested the manifestation of any anxiety phenomenon in an individual is dependent on that person’s dispositional and temperamental traits.36–38 Future studies of patterns of comorbidity in anxiety and mood disorders should examine these diagnostic entities within the context of participant personality and temperament.
In summary, the present study documents the high rates of comorbidity found in a large sample of primary care patients diagnosed with DSM-IV anxiety disorders. Our comorbidity results replicate the results of a recent similar study that examined comorbidity in a sample of psychiatric outpatients and suggest previous assumptions about treatment-seeking in mental health settings as an indication of illness severity may not have been accurate. That the primary care patients enrolled in PCAP showed as much Axis I comorbidity as psychiatric treatment–seeking populations is an important finding for both the mental health and primary care fields, indicating an area in need of attention for both disciplines.
Acknowledgments
The Primary Care Anxiety Project (PCAP) is supported by an unrestricted grant from Pfizer Pharmaceuticals, Inc.
APPENDIX
PCAP is conducted with the participation of the following investigators: Martin B. Keller, M.D. (Chairperson), Risa Weisberg, Ph.D., Regina Dolan, Ph.D., Steven Bruce, Ph.D., Meredith Warshaw, M.S.S., M.A. (Brown University Medical School); Robert Birnbaum, M.D., Randall Paulsen, M.D. (Beth Israel Deaconess Medical Center); Larry Culpepper, M.D., Thomas Gilbert, M.D. (Boston University Medical Center, Codman Square Community Health Center); Mark Fagan, M.D. (Rhode Island Hospital); David Fried, M.D. (Coastal Medical Center, Renaissance Group), Gertrude Manchester, M.D., Ann Massion, M.D. (UMASS Medical Center); Donya Powers, M.D. (partners in Family Health, Inc.); Bruce Ditzion, M.D. (Mount Auburn Hospital); Richard Lain, M.D. (Memorial Hospital of Rhode Island); John Wasson, M.D. (Dartmouth Medical School COOP); Ernst Berndt, Ph.D., Stan Finkelstein, M.D. (Massachusetts Institute of Technology).
Footnotes
Portions of this paper were presented at the 21st Annual Conference of the Anxiety Disorders Association of America, March 21–24, 2002, Austin, TX and at the 30th Annual Meeting of the North American Primary Care Research Group, November 17–20, 2002, New Orleans, LA.
Ten participants with a diagnosis of mixed anxiety-depressive disorder were excluded from these and subsequent analyses since by definition, they could not meet diagnostic criteria for an additional comorbid anxiety or mood disorder. Additionally, 13 participants were not included in these and subsequent analyses because their only current diagnosis was GAD that occurred solely during the course of a mood disorder. This last group was excluded since they would not meet study criteria for having an anxiety disorder if DSM-IV exclusionary rules were strictly followed.
References
- 1.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Psychol Med. 1994;29:555–567. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Nelson CB, McGonagle KA, Lui J, Swartz M, Blazer DG. Comorbidity of DSM-III-R major depressive disorder in the general population: results from the National Comorbidity Survey. Br J Psychiatry. 1996;168:17–30. [PubMed] [Google Scholar]
- 3.Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Stang PE, Wittchen HU, Ustan TB, Roy-Byrne PP, Walters EE. Lifetime panic-depression comorbidity in the National Comorbidity Survey. Arch Gen Psychiatry. 1998;55:801–808. doi: 10.1001/archpsyc.55.9.801. [DOI] [PubMed] [Google Scholar]
- 5.Regier DA, Rae DS, Narrow WE, Kaelber CT, Schatzberg AF. Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. Br J Psychiatry. 1998;173(34 Suppl):24–28. [PubMed] [Google Scholar]
- 6.Brown TA, Barlow DH. Comorbidity among anxiety disorders: implications for treatment and DSM-IV. J Consult Clin Psychol. 1992;6:835–844. doi: 10.1037//0022-006x.60.6.835. [DOI] [PubMed] [Google Scholar]
- 7.Goisman RM, Goldenberg I, Vasile RG, Keller MB. Comorbidity of anxiety disorders in a multicenter anxiety study. Compr Psychiatry. 1995;36:303–311. doi: 10.1016/s0010-440x(95)90076-4. [DOI] [PubMed] [Google Scholar]
- 8.Sanderson WC, DiNardo PA, Rapee RM, Barlow DH. Syndrome comorbidity in patients diagnosed with a DSM-III-R anxiety disorder. J Abnorm Psychol. 1990;99:308–312. doi: 10.1037//0021-843x.99.3.308. [DOI] [PubMed] [Google Scholar]
- 9.Brawman-Mintzer O, Lydiard RB, Emmanuel N, Payeur R, Johnson M, Roberts, et al. Psychiatric comorbidity in patients with generalized anxiety disorder. Am J Psychiatry. 1993;150:1216–1218. doi: 10.1176/ajp.150.8.1216. [DOI] [PubMed] [Google Scholar]
- 10.Massion AO, Warshaw MG, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. Am J Psychiatry. 1993;150:600–607. doi: 10.1176/ajp.150.4.600. [DOI] [PubMed] [Google Scholar]
- 11.Andrews G. Comorbidity in neurotic disorders: The similarities are more important than the differences. In: Rapee RM, editor. Current Controversies in the Anxiety Disorders. New York, NY: Guilford Press; 1993. pp. 3–20. [Google Scholar]
- 12.Clark LA, Watson D, Reynolds S. Diagnosis and classification of psychopathology: challenges to the current system and future directions. Annu Rev Psychol. 1995;46:121–153. doi: 10.1146/annurev.ps.46.020195.001005. [DOI] [PubMed] [Google Scholar]
- 13.Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 14.Emmanuel J, Simmonds S, Tyrer P. Systematic review of the outcome of anxiety and depressive disorders. Br J Psychiatry. 1998;173(34 Suppl):35–41. [PubMed] [Google Scholar]
- 15.Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancil RB. Current and lifetime comorbidity of DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: APA; 1994. [Google Scholar]
- 17.Berkson J. Limitations of the application of fourfold table analysis to hospital data. Biometrics. 1946;2:47–53. [PubMed] [Google Scholar]
- 18.Weillier E, Brisserbe JC, Maier W, Lecrubier Y. Prevalence and recognition of anxiety syndromes in five European primary care settings: a report from the WHO study on Pathological Problems in General Health Care. Br J Psychiatry. 1998;173(34 Suppl):18–23. [PubMed] [Google Scholar]
- 19.Fifer SK, Mathias SD, Patrick DL, Mazonson PD, Lubeck DP, Buesching DP. Untreated anxiety among adult primary care patients in a health maintenance organization. Arch Gen Psychiatry. 1994;51:740–750. doi: 10.1001/archpsyc.1994.03950090072010. [DOI] [PubMed] [Google Scholar]
- 20.Leon AC, Olfson M, Portera L. Service utilization and expenditures for the treatment of panic disorder. Gen Hosp Psychiatry. 1997;19:82–88. doi: 10.1016/s0163-8343(96)00154-5. [DOI] [PubMed] [Google Scholar]
- 21.Rice DP, Miller LS. Health economics and cost implications of anxiety and other mental disorders in the United States. Br J Psychiatry. 1998;173(34 Suppl):4–9. [PubMed] [Google Scholar]
- 22.Simon G, Ormel J, VonKorff M, Barlow W. Healthcare costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995;152:352–356. doi: 10.1176/ajp.152.3.352. [DOI] [PubMed] [Google Scholar]
- 23.Nisenson LG, Pepper CM, Schwenk TL, Coyne JC. The nature and prevalence of anxiety disorders in primary care. Gen Hosp Psychiatry. 1998;20:21–28. doi: 10.1016/s0163-8343(97)00096-0. [DOI] [PubMed] [Google Scholar]
- 24.Spitzer RL, Williams JBW, Kroenke K, Linzer M, de-Gruy FV, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 25.Zajecka J. Importance of establishing the diagnosis of persistent anxiety. J Clin Psychiatry. 1997;58(3 Suppl):9–13. [PubMed] [Google Scholar]
- 26.Zimmerman M, Mattia JI. Psychiatric diagnosis in clinical practice: is comorbidity being missed? Compr Psychiatry. 1999;40:182–191. doi: 10.1016/s0010-440x(99)90001-9. [DOI] [PubMed] [Google Scholar]
- 27.Zimmerman M, Mattia JI. Principal and additional DSM-IV disorders for which outpatients seek treatment. Psychiatr Serv. 2000;51:1299–1304. doi: 10.1176/appi.ps.51.10.1299. [DOI] [PubMed] [Google Scholar]
- 28.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for the DSM-IV Axis I Disorders. New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 29.First MB, Gibbon M, Williams JBW, Spitzer RL. User’s Guide for the Structured Clinical Interview for the DSM-IV Axis I Disorders–Research Version. New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 30.First MB, Gibbon M, Williams JBW, Spitzer RL. SCID-101: Instructional Videotapes for SCID for DSM-IV. New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 31.Maki KM, Weisberg RB, Machan JT, Keller MB. Treatments received for social anxiety disorder in a primary care setting. Poster presented at the annual meeting of the Anxiety Disorders Association of America; Austin, TX. March 2002. [Google Scholar]
- 32.Weisberg RB, Culpepper L, Keller MB. The underutilization of cognitive-behavioral therapy techniques in a sample of primary care patients with anxiety disorders. Presented at the Association for Advancement of Behavior Therapy Annual Conference; Philadelphia, PA. November 2001. [Google Scholar]
- 33.Kennedy BL, Schwab JJ. Utilization of medical specialists by anxiety disorder patients. Psychosomatics. 1997;38:109–112. doi: 10.1016/S0033-3182(97)71478-6. [DOI] [PubMed] [Google Scholar]
- 34.Price D, Beck A, Nimmer C, Bensen S. The treatment of anxiety disorders in a primary care HMO setting. Psychiatr Q. 2000;71:31–45. doi: 10.1023/a:1004662600803. [DOI] [PubMed] [Google Scholar]
- 35.Roy-Byrne PP, Stein MB, Russo J, Mercier E, Thomas R, McQuaid J, et al. Panic disorder in the primary care setting: Comorbidity, disability, service utilization, and treatment. J Clin Psychiatry. 1999;60:492–499. doi: 10.4088/jcp.v60n0713. [DOI] [PubMed] [Google Scholar]
- 36.Lilienfeld SO, Turner SM, Jacob RG. Anxiety sensitivity: an examination of theoretical and methodological issues. Adv Behav Res Ther. 1993;15:147–183. [Google Scholar]
- 37.Reiss S. Expectancy model of fear, anxiety, and panic. Clin Psychol Rev. 1991;11:141–153. [Google Scholar]
- 38.Reiss S, Havercamp SH. The sensitivity theory of motivation: implications for psychopathology. Behav Res Ther. 1996;34:621–632. doi: 10.1016/0005-7967(96)00041-1. [DOI] [PubMed] [Google Scholar]