Abstract
Introduction
To assess the effect of a comprehensive community-based programme for increasing physical activity (PA) after 2 years of interventions.
Material and methods
A 6-year, action-oriented, comprehensive, and integrated community-based study, entitled the Isfahan Healthy Heart Programme, was conducted in Iran from the year 2000. The interventions targeted the whole population of nearly 2,180,000 living in two cities, and were compared with another city considered as a reference. Educational, environmental and legislative interventions were conducted at the community level. Annual evaluations were performed among 6,000 representative individuals. This paper presents the changes in PA habits after 2 years of interventions for increasing PA. The PA habits were assessed by using the Baecke questionnaire, and an energy expenditure of 150 kcal for daily leisure time physical activity was adopted as a cut-off for defining active and inactive lifestyle.
Results
In the intervention and reference areas, respectively 85 and 83% of the population were physically inactive. From 2000 to 2002, the daily PA among both genders decreased in both intervention and reference communities. Meanwhile, the leisure-time PA increased significantly in the intervention area, but decreased in the reference area. The transportation PA did not significantly change in the intervention area, but showed a remarkable decline in the reference area.
Conclusions
We suggest that the synergism resulting from community collaborations has been effective in improving some aspects of PA in our community. The ongoing changes in environmental factors and policies can help in increasing the worksite and transportation PA in later stages of this community-based programme.
Keywords: lifestyle, physical activity, community-based intervention, prevention, non-communicable diseases
Introduction
It is well documented that regular physical activity (PA) is related to a decreased mortality rate [1, 2], and a lower risk of the development of most non-communicable diseases (NCDs) [4–6]. Studies on PA and its impact on health began in the second half of the twentieth century [7]. Increasing PA is now recognized as an effective health promoting strategy [8, 9].
Physical activity is a complex behaviour consisting of various aspects related to occupation, leisure time, transportation, and housekeeping [14]. There is a large body of evidence demonstrating a decreasing trend of PAsince the Second World War [15]. Currently, few professions require intense PA and high energy consumption [16]. Thus, despite recent increases in leisure-time activity in many parts of the world [17], the overall energy consumption of the populations has declined because of the decrease in the worksite PA [18]. Therefore, strategies for increasing PA put forth by various scientific authorities are aimed at increasing all types of PA [19, 20]. The large number of strategies proposed by different countries for increasing various types of physical activities is based on increasing the population's knowledge through educational strategies, especially in primary health care settings [21], as well as environmental changes [8], and legislative measures [20].
The epidemiological transition and the ageing trend of populations in developing countries will exacerbate the burden of NCDs in low and middle income countries. It is estimated that, by 2020, NCDs will account for about 70 percent of the global burden of disease in such countries [22]. Meanwhile, it is documented that dietary and PA changes in low- and middle-income countries are occurring at great speed and at earlier stages of countries’ economic and social development [23]. However, experience in community-based interventions for increasing PA is limited in the developing world.
Our previous studies showed that cardiovascular diseases are one of the major causes of mortality in Iran [24], and their risk factors are highly prevalent in our population [25]. As a public health response to this situation, the Isfahan Healthy Heart Programme (IHHP), a 6-year, action-oriented, comprehensive, and integrated community-based demonstration study for prevention and control of non-communicable diseases (NCDs) was launched in 1999 in Iran. Isfahan Healthy Heart Programme's goals were to improve population behaviour, prevent and control risk factors and diseases, delay the onset of diseases, postpone death, reduce disabilities and disparities in treatment, and change the disease care system approach to a health care system one. The main strategy of this programme was promoting healthy lifestyle through increasing PA, healthy nutrition, tobacco control, and stress management [26]. Isfahan Healthy Heart Programme also aimed to assess the feasibility and impact of a comprehensive, community-based approach in a developing country setting.
This paper presents some short-term results of IHHP for increasing PA after two years from interventional strategies of the programme, especially the Isfahan Exercise and Air Pollution Control Project (IEAPCP), for increasing PA in the general adult population.
Material and methods
Study population
Isfahan Healthy Heart Programme is a community-based programme, conducted on the whole community of two cities in central Iran in comparison to a reference area. The interventions were implemented on the whole population of the urban and rural areas of Isfahan and Najafabad, with a population of 1,895,856 and 275,984 respectively. In order to facilitate the interventions, the intervention community was divided into 8 target groups: women, workers, children, young people, cardiovascular patients and their family members, high risk population, health professionals and NGO members.
The reference community was the urban and rural population of Arak, with a population of 668,531, where only governmental health programmes applied at a national level were considered.
Baseline data collection
Isfahan Healthy Heart Programme is a quasi-experimental demonstration programme with simultaneous evaluation and research studies. The baseline survey was conducted on 20,000 participants, selected by random cluster sampling from the population living in the aforementioned three cities with similar socio-demographic situations. The whole baseline survey will be repeated on an independent sample in both intervention and reference communities at the end of the study [25].
Information on PA was collected using the Baecke questionnaire, and the types of PA (worksite, housekeeping, leisure time and transportation) were documented. Using the responses in the practice part of the questionnaire, the PA levels of participants were measured in four fields of leisure time, worksite, household and transportation PA. In all fields, the duration and frequency of doing each specific activity were asked. The amount of PA was calculated (in the unit of MET-minutes per day) by using extent coefficients of each particular activity, multiplying by the duration of performing it in a day. One MET is reflective of energy expenditure during rest [26]. The sum of calculated PA amount for various questionnaire items in every field was used as the total PA in each field, and in turn, the sum of total PA in all four fields was considered as the total PA of participants. The non-dynamic or sedentary activity of each field was not included in the calculation of the total PA level. The amount of energy corresponding to each type of PA and the total energy expenditure were calculated by using information from the questionnaire. Validity and reliability of this questionnaire were verified by the Education Development Centre of Isfahan University of Medical Sciences [27].
Interventional strategies
As explained before, IHHP is an interventional programme to modify lifestyle at the community level. In order to apply these interventions the programme was divided into 10 executive projects: Heart Health Promotion from Childhood (HHPC), Youth Intervention Project (YIP), Women Healthy Heart Project (WHHP), Worksite Intervention Project (WIP), Health Professionals Education Project (HPEP), Non-Governmental Organizations and Volunteers (NGOV), Healthy Lifestyle for High-Risk groups (HLHR), Healthy Lifestyle for Cardiovascular Patients (HLCP), Healthy Food for Healthy Community (HFHC), and Isfahan Exercise and Air Pollution Control Project (IEAPCP).
The last two projects (Healthy Food for Healthy Community [HFHC] and Isfahan Exercise and Air Pollution Control Project [IEAPCP]) were in charge of legislative level, urban structure modification or comprehensive education interventions regardless of the target communities.
All interventions in each project, according to their nature, were categorized in three groups, including educational, environmental and legislative strategies. The interventions in each project were designed based on the information obtained from a primary survey showing the community lifestyle problems.
The purpose of the PA-related interventions in IEAPCP was to reach an activity level of at least 30 min on at least five days a week. We also aimed to integrate an aerobic activity of medium intensity, e.g. walking, jogging or bicycling, in the population daily life. The interventions of this project were as follows:
1) Educational interventions
Educational interventions related to PA increment included educating all people through campaigns and public media, as well as education of specific target groups, e.g. women attending health care clinics, workers and employees in factories and offices, etc.
Face to face education, class education, using educational materials, educational campaigns and educating via media, especially television and radio, were used as other educational methods.
Educational interventions were designed based on promoting different PA increment methods in an integrated way. These interventions included encouragement not to use personal motor vehicles and using cycling and walking for in-city trips, educating on using stairs instead of elevators, performing aerobic exercise with medium intensity for at least 30 min a day during leisure time, educating on exercise in worksites according to the type of people's jobs and educating housewives on simple exercises.
2) Environmental interventions
These included modification and improvement of urban environments, as well as development of the infrastructures required for reducing the use of personal motor vehicles and encouraging cycling, walking, or the use of public transportation. These interventions were performed in cooperation with Isfahan Municipality, Isfahan Physical Education Department, and the Environment Protection Organization. Interventions included organizing rallies and healthy heart exercise fairs on designated “No-automobile” days – part of a series of environmental and educational interventions carried out monthly in one of Isfahan's busiest streets (historical Chaharbagh Street) – aimed at sensitizing the public. Environmental interventions intended to provide education for the community and to develop the necessary infrastructure for encouraging the public to avoid the use of personal motor vehicles for in-city trips.
Another environmental intervention of IEAPCP was to demand the development of public exercise areas and green spaces in residential complexes, and construction and increase in the number of sport centres in cooperation with other authorities, including Isfahan Provincial Government.
3) Legislative interventions
Since some rules – including daily exercise in the morning shift of schools and the official permission to exercise up to 3 h at worksite for workers – already existed, IEAPCP and other IHHP projects followed their execution. In addition, directives on adding exercise time in the afternoon shift of schools were issued to schools by the Provincial Education Administration.
We considered an energy expenditure of 150 kcal for daily leisure time PA as the cut-off for defining active and inactive lifestyle. To investigate the impact of interventions on knowledge, attitude and practice (KAP), and lifestyle (including PA) of the adult population (19+) studied, we used the data obtained in the baseline survey, and the two annual surveys conducted for assessment of short-term results of the interventions.
Evaluation
The intervention activities and evaluation were integrated components in IHHP, i.e. the functions of monitoring and evaluation were to assess the extent to which the programme has attained its objectives and to assess the process of programme development and performance. Monitoring was regularly implemented on small samples in order to assess the effect of different interventional strategies. The process evaluation was undertaken in the intervention area only, while the impact and outcome evaluations were undertaken in both intervention and reference areas. The short-term impacts of the interventions on behavioural changes were evaluated in four repeated independent sample surveys from 2002 to 2005, in order to compare modifiable behavioural risk factors in intervention and reference areas. Because the interventions target the whole community, in the baseline and annual surveys, data were collected from samples that represented the whole population. Multistage random sampling and age-based CINDI protocol sampling methods were used for the baseline and subsequent annual impact evaluations. According to the CINDI protocol and by the 1.5 design effect, the sample size for community-based approach sampling was about 250 individuals in each sex and age group. We defined six age groups in this study (20–29, 30–39, 40–49, 50-59, 60–69 and≥70); hence in the annual evaluations, 6000 individuals (3000 males, 3000 females) were studied in the intervention and reference areas.
Statistical analysis
Data were stored in a computer database, and were analyzed using the SPSS statistical package version 12.0 for Windows (SPSS Inc., Chicago, USA). The mean intensity and duration of each type of PA in leisure time and daily transportation, as well as total daily PA, were calculated. Mean amounts of PA in the intervention and reference cities were calculated and compared using the analysis of variance (ANOVA). Annual changes in quantitative data in each city were also compared using t-test. Qualitative data, including the frequency of cycling and walking, were analyzed by using the χ2 test.
Results
The results obtained from the evaluation of PA levels in three successive years in intervention and reference areas, conducted as a cross-sectional survey with independent samples, are as follows. The general characteristics of communities studied in 3 different years are shown in Table I.
Table I.
General characteristics of the study population: 2000-2002 – IHHP
| 2000 | 2001 | 2002 | |
|---|---|---|---|
| N | 6175 (6339) | 2994 (2897) | 2400 (2393) |
| Age [years] | |||
| Intervention area | 38.6±14.7 | 40.4±15.4 | 40.7±15.6 |
| Reference area | 39.1±15.1 | 40.5±15.3 | 40.5±15.9 |
| Females (%) | |||
| Intervention area | 51.3 | 50 | 50.3 |
| Reference area | 50.8 | 51 | 50.5 |
| Place of residence (% of rural) | |||
| Intervention area | 21.0 | 18.5 | 18.7 |
| Reference area | 33.4 | 33.3 | 35 |
Based on the energy expenditure for leisure time PA, in the intervention and reference areas 85 and 83% of the population were respectively considered to be physically inactive.
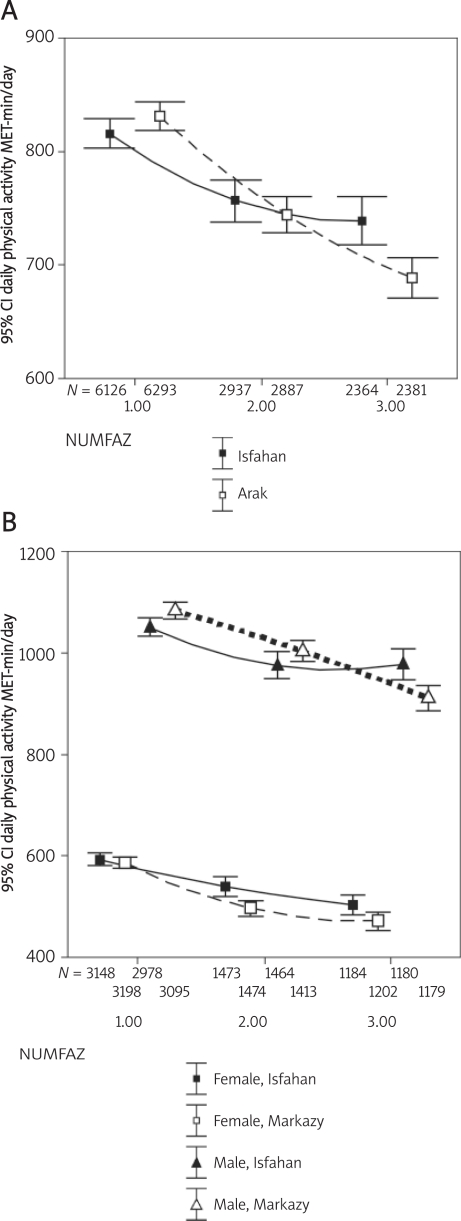
As presented in Figure 1, from 2000 to 2002, among both genders, the daily PA decreased in both intervention and reference communities.
Figure 1.
Changes in daily physical activity in the total population (A), and by gender (B): 2000-2002: IHHP
Meanwhile, the leisure-time PA increased significantly in the intervention area, whereas it decreased in the reference area. Among men, leisure-time PA showed no significant change in the intervention area, but showed a sharp decline in the reference area. This type of activity increased in women of both communities, but the slope of this change was greater in the intervention area (Table II).
Table II.
Changes in the leisure time and transportation physical activity by gender in the intervention vs. the reference community: 2000-2002 – IHHP
| Year of study | Mean (SD) | p | ∆2001 vs. 2000 | ∆2002 vs. 2001 | |
|---|---|---|---|---|---|
| Leisure time physical activity (MET-min/day) | |||||
| Females | |||||
| Intervention community | 2000 | 3169.00 (64.43) | <0.0001 | 13.38* | 4.26 |
| 2001 | 1496.00 (68.70) | ||||
| 2002 | 1206.00 (73.46) | ||||
| Reference community | 2000 | 3222.00 (64.18) | <0.0001 | 6.46* | 1.92 |
| 2001 | 1477.00 (57.50) | ||||
| 2002 | 1209.00 (60.96) | ||||
| Males | |||||
| Intervention community | 2000 | 3006.00 (94.25) | 0.05 | 7.28** | −5.24 |
| 2001 | 1498.00 (98.86) | ||||
| 2002 | 1193.00 (98.35) | ||||
| Reference community | 2000 | 3117.00 (93.88) | <0.0001 | −10.87 | −4.46 |
| 2001 | 1419.00 (78.55) | ||||
| 2002 | 1189.00 (76.94) | ||||
| Transportation physical activity (MET-min/day) | |||||
| Females | |||||
| Intervention community | 2000 | 3167.00 (132.32) | 0.60 | −3.30 | 4.10 |
| 2001 | 1495.00 (142.45) | ||||
| 2002 | 1202.00 (135.29) | ||||
| Reference community | 2000 | 3211.00 (141.71) | <0.0001 | −30.93* | −21.01¶ |
| 2001 | 1476.00 (114.34) | ||||
| 2002 | 1209.00 (100.32) | ||||
| Males | |||||
| Intervention community | 2000 | 2954.00 (201.42) | 0.06 | −12.40 | −1.28 |
| 2001 | 1467.00 (214.80) | ||||
| 2002 | 1176.00 (204.73) | ||||
| Reference community | 2000 | 3079.00 (192.41) | <0.0001 | −46.72* | −28.79 ¶ |
| 2001 | 1409.00 (144.93) | ||||
| 2002 | 1186.00 (140.84) | ||||
* p < 0.0001 2001 vs. 2000
** p < 0.05 2001 vs. 2000
¶ p < 0.0001 2002 vs. 2001
The transportation PA did not significantly change in the intervention area, but showed a sharp decrease in the reference area. These changes were similar in both genders (Table II). The worksite PA showed no significant change.
Discussion
Our findings showed a high prevalence of sedentary lifestyle in the study population, notably among women. We found that in both intervention and reference areas, more than 80% of participants were physically inactive. This rate is different from many other parts of the world; for example, in European countries, less than 30% of the population are physically inactive, although the Eastern European countries were less active [28].
Various studies have underscored the possibility of an increase in PA in different communities through culturally appropriate interventions, which would vary between studies. In general, different studies categorize PA-related interventions into three groups based on the interventional settings: community-based interventions (such as PA increment through cycling and walking for in-city trips), worksite (including offices, factories and schools) interventions, and interventions through the health system by health professionals. The effects of each group have been investigated in various studies [29–32].
In a study conducted by Lawlor et al. in 1999, 135 general physicians were educated for PA increment strategies in the community. In turn, the PA of those people who were educated by these physicians was assessed. The findings indicated that physicians have acceptable knowledge about the health effects of regular PA and the amount of necessary PA, but they do not fully use their knowledge in communicating information on PA to the people. Based on this study, physicians only try to improve the PA of the high-risk patients who regularly visit them and who have risk factors or a special disease, while the whole community do not benefit from their knowledge [33]. Furthermore, in the review of Lawlor et al. in 2001, a series of 8 studies showing an increase in PA due to education through the health system was investigated. They concluded that counselling and education provided by general physicians would only result in short-term changes in PA, and are not sustainable [34]. It might be suggested that interventions based on the health system and general physicians are not considered as practical approaches to increase PA at the community level.
A number of studies have conducted interventions through increasing transportation PA [8, 35–37]. Among these studies, the one performed by Lawlor et al. in 2003 concluded that interventions which encourage environmental changes through regular cycling or walking have a pivotal role in increasing PA at the community level. In their study, the British National Cycling Organization has played a valuable role in increasing PA [8].
In 2004, Hilsdon et al. demonstrated that community-based interventions have several short-term effects and many such interventions may also lead to long-term impacts [38]. Studies have also shown that interventions encouraging moderate-intensity PA and those requiring no special facilities have had longer-term effects [39].
In 2007 Ogilvie and his colleagues assessed different PA increment methods and concluded that different types of people may respond to various approaches, tailored to their psychological characteristics or life circumstances. In other words, one size may not fit all and various approaches should be offered: some people may respond best to personal advice from their physician, others may prefer private feedback from a device such as a pedometer, others (perhaps those in a more advantaged socioeconomic position) may benefit from interventions delivered through the internet, others may benefit from the social support of a walking group, and others may increase their PA in response to prompts about reducing their car use on environmental grounds [40].
The comparison of changes in PA habits in the intervention and reference areas of the current study suggest that the community-based interventions of IHHP were successful in increasing the leisure time PA. We suggest that the synergism resulting from community collaborations has been effective in improving some aspects of PA in our community.
However, since these interventions were conducted in all areas – including the community, worksites, schools and also the health system – and included different environmental, educational and legislative strategies, it is not possible to determine the exact intervention which has caused the increase in leisure time PA. We can generally conclude that using different ways for community-based interventions may be beneficial. It is worth mentioning that the amount of total PA decreased in both intervention and reference areas, which is likely related to decreased transportation and worksite activities. It seems that the changes in working methods and lifestyle toward using more technological equipment are the main reason for the decrease in worksite and transportation PA and therefore total PA.
Since environmental or legislative changes were implemented at the societal level to reduce exposure to health risk factors as well as to increase healthy behaviours, and did not require personal action, they are more likely to be successful than efforts of individual change to promote and maintain behavioural changes of individuals. The ongoing activities of IHHP in providing facilities for using public transportation instead of personal motor vehicles and, in addition, improving worksite PA might result in more successful results in the next annual evaluations of the programme.
In addition to environmental and legislative initiatives, IHHP interventions were based on educating both health professionals and the public; thus they can be successful in increasing PA at the community level. We found that the leisure-time and transportation activities had a better trend in cities of intervention as compared to the reference community. By considering the increased number of manufactured and sold automobiles in Iran and the growing perception of the use of personal vehicles as a measure of higher socioeconomic status, Iranian society is seemingly on a trend towards a more sedentary lifestyle. Therefore, we propose interventions like those conducted in Isfahan for educating the public on not using personal vehicles.
It is well documented that small behavioural changes observed among the whole population were likely to have considerable beneficial effects at the population level [32]. The magnitude of the results of community-based interventional trials must be judged according to their potential impacts on public health or population level during the later stages of the IHHP.
In conclusion, the low level of PA in countries such as Iran highlights the necessity of implementing community-based interventions for promoting an active lifestyle. Effective interventions should be identified and extended at the national level. An improvement in PA levels or a decline in sedentary activities can be expected through designing community-based interventions.
We suggest that the community-based interventional programmes in developing countries with limited facilities should emphasize comprehensive approaches, integrated risk management, policy and environmental changes, community organization, individual empowerment and participation, as well as collaboration with various sectors in order to benefit from the synergism of activities, and in turn to increase the intensity of interventions.
References
- 1.Hayes L, White M, Unwin N, et al. Patterns of physical activity and relationship with risk markers for cardiovascular disease and diabetes in Indian, Pakistani, Bangladeshiand European adults in a UK population. J Publ Health Med. 2002;24:170–8. doi: 10.1093/pubmed/24.3.170. [DOI] [PubMed] [Google Scholar]
- 2.Nazroo J. London: PSI; 1997. The health of Britain's ethnic minorities. [Google Scholar]
- 3.Andersen LB, Schnohr P, Schroll M, Hein HO. All-cause mortality associated with physical activity during leisure time, work, sports, and cycling to work. Arch Intern Med. 2000;160:1621–8. doi: 10.1001/archinte.160.11.1621. [DOI] [PubMed] [Google Scholar]
- 4.Sesso HD, Paffenbarger RSJ, Lee IM. Physical activity and coronary heart disease in men. The Harvard Alumni Health Study. Circulation. 2000;102:975–80. doi: 10.1161/01.cir.102.9.975. [DOI] [PubMed] [Google Scholar]
- 5.Berlin JA, Colditz GA. A meta-analysis of physical activity in the prevention of coronary heart disease. Am J Epidemiol. 1990;132:612–28. doi: 10.1093/oxfordjournals.aje.a115704. [DOI] [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services. 1996. Physical activity and health: a report of the surgeon general Atlanta GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. [Google Scholar]
- 7.Morris JN, Heady JA, Raffle PAB, Parks JW. Coronary heart disease and physical activity of work. Lancet. 1953;ii:1111–20. doi: 10.1016/s0140-6736(53)91495-0. [DOI] [PubMed] [Google Scholar]
- 8.Lawlor DA, Ness AR, Cope AM, Davis A, Insall P, Riddoch C. The challenges of evaluating environmental interventions to increase population levels of physical activity: the case of the UK, National Cycle Network. J Epidemiol Community Health. 2003;57:96–101. doi: 10.1136/jech.57.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morris JN. Exercise in the prevention of coronary heart disease: today, s best buy in public health. Med Sci Sports Exerc. 1994;26:807–14. [PubMed] [Google Scholar]
- 10.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–7. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization/International Federation of Sports Medicine. Committee on physical activity for health. Exercise for health. Bull World Health Organ. 1995;73:135–6. [PMC free article] [PubMed] [Google Scholar]
- 12.Do H. London: DoH; 1996. Strategy statement on physical activity. [Google Scholar]
- 13.Physical activity and health, a report of the surgeon general. U.S. Department of health and human services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, The President's Council on Physical Fitness and Sports; [Google Scholar]
- 14.Paffenbarger RS, Jr, Blair SN, Lee IM. A history of physical activity, cardiovascular health and longevity: the scientific contributions of Jeremy N Morris, DSc, DPH, FRCP. Int J Epidemiol. 2001;30:1184–92. doi: 10.1093/ije/30.5.1184. [DOI] [PubMed] [Google Scholar]
- 15.Takao S, Kawakami N, Ohtsu T. Japan Work Stress and Health Cohort Study Group.Occupational class and physical activity among Japanese employees. Soc Sci Med. 2003;57:2281–9. doi: 10.1016/s0277-9536(03)00134-5. [DOI] [PubMed] [Google Scholar]
- 16.Salonen JT, Slater JS, Tuomilehto J, Rauramaa R. Leisure time and occupational physical activity: risk of death from ischemic heart disease. Am J Epidemiol. 1988;127:87–94. doi: 10.1093/oxfordjournals.aje.a114794. [DOI] [PubMed] [Google Scholar]
- 17.McGraw SA, Sellers D, Stone E, et al. Measuring Implementation of school programs and policies to promote healthy eating and physical activity among youth. Prev Med. 2000;31:S86–97. [Google Scholar]
- 18.Sallis JF, Bauman A, Pratt M. Environmental and policy interventions to promote physical activity. Am J Prev Med. 1998;15:379–97. doi: 10.1016/s0749-3797(98)00076-2. [DOI] [PubMed] [Google Scholar]
- 19.Task Force on Community Preventive Services. Recommendations to increase physical activity in communities. Am J Prev Med. 2002;22:67–72. [Google Scholar]
- 20.Harland J, White M, Drinkwater C, et al. The Newcastle exercise project: a randomised controlled trial of methods to promote physical activity in primary care. BMJ. 1999;319:828–32. doi: 10.1136/bmj.319.7213.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U.S. Preventive Services Task Force. Behavioral counseling in primary care to promote physical activity: recommendation and rationale. Ann Intern Med. 2002;137:205–7. doi: 10.7326/0003-4819-137-3-200208060-00014. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organisation. Diet, Nutrition and the prevention of Chronic Diseases. In Technical report Series 916 Geneva; World Health Organization; 2003. [PubMed] [Google Scholar]
- 23.Popkin BM. Nutrition transition in the developing world. Develop Policy Rev. 2003;21:581–97. [Google Scholar]
- 24.Sarraf-Zadegan N, Boshtam M, Malekafzali H, Bashardoost N, Tabatabaei FA, Rafiei M. Secular trends in cardiovascular mortality in Iran, with special reference to Isfahan. Acta Cardiol. 1999;54:327–33. [PubMed] [Google Scholar]
- 25.Sarraf-Zadegan N, Boshtam M, Rafiei M. Risk factors for coronary artery disease in Isfahan, Iran. Eur J Publ Health. 1999;9:20–6. [Google Scholar]
- 26.Sternfeld B, Ainsworth BE, Quesenberry CP. Physical activity patterns in a diverse population of women. Prev Med. 1999;28:313–23. doi: 10.1006/pmed.1998.0470. [DOI] [PubMed] [Google Scholar]
- 27.Sarraf-Zadegan N, Sadri G, Malek-Afzali H, et al. Isfahan Healthy Heart program: a comprehensive integrated community-based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiol. 2003;58:309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 28.Myint PK, Surtees PG, Wainwright NW, et al. Modifiable lifestyle behaviors and functional health in the European Prospective Investigation into Cancer (EPIC)-Norfolk population study. Prev Med. 2007;44:109–16. doi: 10.1016/j.ypmed.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 29.Schafer A, Victor D. The future mobility of the world's population. Transportation Research. Part A: policy and practice. 2000;34:171–205. [Google Scholar]
- 30.Frank L. Land use and transportation interaction: implications on public health and quality of life. J Plan Edu Res. 2007;20:6–2. [Google Scholar]
- 31.Lawlor DA, Ness AR, Cope AM, et al. The challenges of evaluating environmental interventions to increase population levels of physical activity: the case of the UK National Cycle Network. J Epidemiol Community Health. 2003;57:96–101. doi: 10.1136/jech.57.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dunn AL, Marcus BH, Kampert JB, et al. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999;281:327–34. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 33.Lawlor DA, Keen S, Neal RD. Increasing population levels of physical activity through primary care: GPs’ knowledge, attitudes and self-reported practice. Fam Pract. 1999;16:250–4. doi: 10.1093/fampra/16.3.250. [DOI] [PubMed] [Google Scholar]
- 34.Lawlor DA, Hanratty B. The effect of physical activity advice given in routine primary care consultations: a systematic review. J Public Health Med. 2001;23:219–26. doi: 10.1093/pubmed/23.3.219. [DOI] [PubMed] [Google Scholar]
- 35.Dunn AL, Garcia ME, Marcus BH, et al. Six-month physical activity and fitness changes in Project Active, a randomized trial. Med Sci Sports Exerc. 1998;30:1076–83. doi: 10.1097/00005768-199807000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Pazoki R, Nabipour I, Seyednezami N, Imami SR. Effects of a community-based healthy heart program on increasing healthy women's physical activity: a randomized controlled trial guided by community-based Participatory Research (CBPR) BMC Public Health. 2007;7:216–11. doi: 10.1186/1471-2458-7-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Andersen RE, Wadden TA, Bartlett SJ, et al. Effects of lifestyle activity vs structured aerobic exercise in obese women: a randomized trial. JAMA. 1999;281:335–40. doi: 10.1001/jama.281.4.335. [DOI] [PubMed] [Google Scholar]
- 38.Hillsdon M, Foster C, Naidoo B, Crombie H. The effectiveness of public health interventions for increasing physical activity among adults: a review of reviews. London: Health Development Agency; 2005. pp. 1–3. [Google Scholar]
- 39.Dunn AL, Andersen RE, Jakicic JM. Lifestyle physical activity interventions. History, short- and long-term effects, and recommendations. Am J Prev Med. 1998;15:398–412. doi: 10.1016/s0749-3797(98)00084-1. [DOI] [PubMed] [Google Scholar]
- 40.Rose G. Oxford: Oxford University Press; 1992. The Strategy of Preventive Medicine. [Google Scholar]