Abstract
Background
A two-year quality improvement campaign at a single teaching hospital was launched to improve the identification, documentation, and treatment of pressure ulcers (PUs) after Centers for Medicare & Medicaid Services (CMS) declared severe hospital-acquired PUs are “never-events.”
Method
The campaign included (1) reference materials, (2) new documentation templates, (3) staff education, and (4) hospital-wide mattress replacement. An ongoing retrospective chart review of frail older patients determined the presence of PU documentation, which provider (nurse or physician) documented the PU, and which descriptors (stage, size, or location) were used.
Results
The campaign significantly increased the proportion of PUs completely documented by nurses from 27% to 55% following mattress replacement and resident education (OR 3.68, p = 0.001, 95% CI: 1.68–8.08). A similar improvement was observed for physician documentation increasing from 12% to 36% following the same interventions however this change was not statistically significant (OR 2.11, p = 0.12, 95% CI: 0.82–5.39).
These improvements were short-lived due to the implementation of electronic medical records (EMR) for nursing notes. Although the percentage of PUs completely documented by nurses decreased following EMR implementation, it increased in the following months, above the pre-campaign baseline as nurses adapted to the new documentation system. However, after EMR implementation, complete PU documentation by physicians fell to a nadir of 0% and did not recover.
Discussion
A multi-component campaign to improve the quality of PU documentation by both physicians and nurses can yield positive gains. However, these improvements were short-lived due to EMR implementation, which acutely worsened documentation of PUs. This emphasizes the importance of frequent and repeated interventions to sustain quality improvement successes.
Introduction
Background Knowledge
An estimated 15% to 24% of hospitalized patients have a diagnosed pressure ulcer (PU).1 A PU is an area of skin that breaks down when a vulnerable patient remains in the same position for as short as 2 to 6 hours.2 Frail elder patients are at a higher risk of developing a PU due to multiple aging-related chronic health conditions, which slow wound recovery and extend hospitalizations. 3 Furthermore, PUs are considered preventable by improving quality of care, documentation practices, and medical staff awareness. 4,5,6
As such, the Institute for Healthcare Improvement (IHI) has included PU prevention as one of the twelve interventions included in the “5 Million Lives Campaign.” 7 Going one step further, the Centers for Medicare & Medicaid Services (CMS) has deemed the most severe hospital-acquired PUs (Stage III and Stage IV) “never events” indicating that they should not occur if a hospital follows adequate performance standards and thus should not be reimbursed.8 Current estimates suggest that the annual cost of hospital-acquired PUs is between $2.2 to $3.6 billion.9 The change in reimbursement can be especially costly to hospitals that do not have effective PU prevention and treatment initiatives in place. Interestingly, this policy change stresses the importance of complete PU documentation since PUs that are “present on admission” or stage I or II hospital-acquired PUs are not considered “never events.” In addition, current guidelines recommend that all patients are screened for PUs10 and that if a PU is found, the location, stage, and size should be evaluated.11 Thus, an important first step to improve PU care is to improve PU documentation.
Local Problem
In preparation of the CMS reimbursement change, a pilot study was conducted to assess the accuracy of PU documentation in our institution. In accordance with NDNQI and established practice guideline recommendations,12 teams of nurse champions conducted quarterly skin exams on all hospitalized patients and monitored PU prevalence. A retrospective chart review on patients who received these skin exams revealed that only 50% of PUs found on physical exam were documented in the chart.11 Additionally, documented PUs were frequently missing key descriptors, such as the stage, location, and size, and thus were not meeting quality guidelines. The documentation of PU characteristics is important not only for reimbursement, but also for treatment and communication within the health care team.
Intended Improvement
These findings led to the development of a multi-component campaign designed to improve PU documentation and wound care. In response to the pilot study’s results and the CMS reimbursement change, in June 2007, our institution launched a multi-component campaign to encourage full documentation of PUs as a first step towards reducing hospital-acquired PU prevalence.
A clinical nursing specialist (CNS) was hired to focus on improving nursing staff knowledge of wound management and increasing documentation completeness. This wound care CNS worked directly with a group of nurse champions, the “Skin Care Team,” already formed to attempt to improve wound management. Additionally, a “PU Quality Improvement Team” was formed to quantify PU prevalence and measure quality of care at UCMC. This team was composed of the wound care CNS (CB), a hospitalist physician (VA), a resident physician (DD), and three employees from the UCMC Center for Quality (TB).
Study Question
The aim of this study was to evaluate the impact of a multi-component campaign on the quality of PU documentation as a method of quantifying the improvement in PU prevention and care.
Methods
Ethical Issues
As a part of an ongoing research study for vulnerable elder patients, consent had already been obtained for a retrospective chart review on the quality of PU care. The remainder of the study was deemed exempt from the University of Chicago Internal Review Board. The authors report no conflicts of interest.
Setting
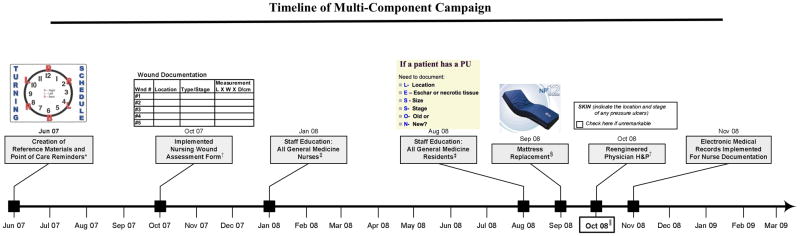
The University of Chicago Medical Center (UCMC) is a 596-bed tertiary-care facility and the largest academic medical center on the South Side of Chicago. In fiscal year 2006, UCMC had 26,933 admissions and 79,534 emergency department visits. In an effort to both encourage full documentation of PUs and decrease hospital-acquired PU prevalence at UCMC, a multi-component campaign was instituted consisting of (1) creation of reference materials and point of care reminders, (2) reengineered documentation templates, (3) staff education, and (4) hospital mattress replacement. (Figure 1)
Figure 1.
Timeline of the interventions included in the multi-component campaign designed to increase pressure ulcer documentation and quality of care
* Point of care reminders included multiple posters and visual cues posted in general medicine patient rooms and doors. For example, the turning schedule clocks were posted above each general medicine bed to remind the health care team to turn the patient every two hours.
† Documentation templates were reengineered to remind the provider to completely document each pressure ulcer’s location, stage, and size.
‡ Nurse and resident education included information on staging, proper documentation, and wound management techniques.
§ All general medicine inpatient beds were replaced with non-powered pressure redistribution mattresses, which are equipped with a built-in alternating pressure pump for pressure management.
|| In October 2008, the Centers for Medicare & Medicaid Services (CMS) ended reimbursement for hospital-acquired pressure ulcers.
Planning the Intervention
Creation of Reference Materials and Point of Care Reminders
In June 2007, the CNS for wound care (CB) created a product formulary reference tool, which listed all available wound-care products and a description of when they should be used. A reference website was also created on the hospital intranet, which contained the information in the product formulary as well as a detailed description of specific wound management procedures and standard of care. Wound care related posters and mnemonics were displayed in the general medicine floors and at the patient bedside in June 2007. An example of these “point of care” interventions included a picture of a clock posted above patients’ beds reminding the health care team to turn the patient every two hours (Figure 1). Additionally, pocket cards were developed for both nurses and physicians, which described PU staging and instructions for documentation.
Reengineered Documentation Templates
The second component of the intervention involved a modification to the nursing admission wound assessment form in October 2007. The new template included specific boxes to describe the location, stage, and size for each documented PU. Additionally, in October 2008, the physician H&P form was modified to include a reminder to document the size and location of each PU. In November 2008, UCMC underwent an institution-wide change to an electronic medical record (EMR) system (Epic Systems Corporation, Verona, WI) for nursing documentation. In anticipation of this switch, with input from the PU Quality Improvement Team, a similar PU specific template was incorporated into the new electronic wound documentation form.
Staff Education
In January 2008, all general medicine nurses attended wound care lectures delivered by the CNS for wound care (CB). This education focused on the importance of wound identification, assessment, prevention, and accurate documentation. Similarly, in August 2008, all general internal medicine residents attended a PU prevention presentation delivered by the physician members of the “PU Quality Improvement Team” (VA, DD). This lecture focused on staging, documentation, and wound management techniques previously shown to improve PU care in an academic setting.13 Specifically, residents were instructed to look through the nursing notes for each patient to recognize the patient’s PU risk as well as any documented PUs.14 The importance of these actions was stressed due to the pending “never event” declaration for severe hospital-acquired PUs. Additionally, the skin care reference website was displayed, PU pocket cards were distributed, and residents were informed about the upcoming mattress replacement. This initiative was supported by the departmental quality committee and promoted at grand rounds and other educational lectures.
Mattress Replacement
Prior to the campaign, vulnerable patients who needed extra pressure support were required to have a physician order for a mattress overlay. Prior data showed mattress overlays were underutilized in high-risk patients despite their indication from nursing risk assessments. In an attempt to streamline these support surface orders, in September 2008, all inpatient beds were replaced with non-powered pressure redistribution, SW NP12 and SW NP24, mattresses (SIZEWise Rentals, LLC, Kansas City, MO). These mattresses are adequate for preventing less severe (Stage I and Stage II) PUs and are equipped with a built-in alternating pressure pump, which can be used to treat severe (Stage III and Stage IV) PUs.
As a part of this campaign, the CNS for wound care presented the benefits of replacing the general medicine mattresses to the UCMC senior leadership. The argument was twofold: (1) all patients would immediately have pressure reduction support thus reducing hospital-acquired PUs and (2) because mattress overlays would no longer need to be rented, a return on investment was estimated to occur 11 months after replacement.
Planning the Study of Intervention
To evaluate this QI initiative, data were obtained from a large ongoing project that examined the quality of care in frail general medicine patients. The University of Chicago Internal Review Board independently approved this study and the validity of the analysis.11 One of the measured components was the quality of PU documentation and prevention. Poor adherence to PU guidelines was found before the initiation of the campaign. This finding was used as the baseline for this improvement study.15 These data were accumulated and analyzed by trained research assistants, with verified concordance, over the course of the campaign to determine the impact of the interventions on adherence to PU guidelines.
Methods of evaluation
Between October 2006 and June 2009, trained research assistants identified patients aged 65 and older, received the patient’s consent to participate, and then administered the Vulnerable Elders Survey (VES-13). 16,17,18 This survey uses simple indicators such as age, functional limitation, and self-reported health to quickly identify patients who are at an increased risk for functional decline and increased morbidity and mortality. A score of 3 or higher indicates that the patient is “vulnerable.” If the patient was determined to be “vulnerable,” trained research assistants conducted a retrospective “vulnerable elder” chart abstraction.
This abstraction evaluated the presence of a PU risk assessment and documentation by either a nurse or physician using ACOVE quality indicators. 11 Additionally, each documented PU was further assessed to determine which specific descriptors were used (location, stage, or size). Stage I PUs were excluded from this study due to the variability of identification especially in African-American patients as demonstrated in other studies. 19,20
Analysis
Descriptive statistics were used to quantify PU documentation accuracy before, during, and after the multi-component campaign. The proportions of PUs documented by nurses and physicians were compared using control charts and a two-sample test of proportions (p values < 0.05 were considered to be statistically significant). Additionally, the proportion of documented PUs, which were documented completely by physicians and nurses were compared using a two-sample test of proportions and over the course of the campaign by quarter with a pairwise correlation coefficient. Finally, significant changes in the quality of documentation by quarter over the course of the campaign were determined using multivariate logistic regression adjusting for age, gender, and ICU transfer status. Statistical analysis was completed using Stata 10.0 (Stata Corporation, College Station, TX).
Results
Outcomes
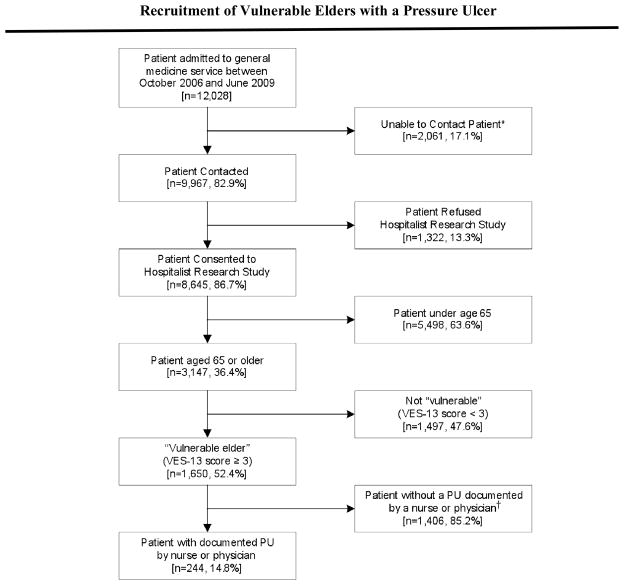
The campaign was successfully implemented on schedule between the second quarter (Q2) 2007 and Q2 2009 (Figure 1). 244 (14.8%) vulnerable elder general medicine patients had a stage II through stage IV PU documented by either a nurse or a physician throughout the campaign (Figure 2). The majority of the 244 patients in this study were African-American females, with a mean age of 79.0 (Table 1). Our initial goal was to decrease the prevalence of PUs but once we started our campaign we witnessed an increase in case finding and thus chose to focus on quality of documentation as a proxy for PU guideline adherence rather than actual prevalence.
Figure 2.
Flow of patients through the study.
*2,046 patients were discharged from the hospital before contact could be made and 15 patients died before they were approached
†PU = Pressure Ulcer.
Table 1.
Characteristics of the study population (n=244)
| n (%)1 | |
|---|---|
| Age in years, mean +/− SD | 79.0 ± 8.99 |
| Female | 163 (66.8) |
| African-American | 195 (79.9) |
| Hispanic | 5 (2.05) |
| Mini Mental Status Exam score, mean +/− SD2 | 20.9 ± 1.92 |
| Length of hospital stay in days, mean +/− SD | 9.51 ± 9.44 |
| VES-13 score3, mean +/− SD | 6.69 ± 2.16 |
| Patients with any ICU Stay | 41 (16.8) |
Except where noted
For Mini Mental Status Exam, n=172
VES-13, 13-item Vulnerable Elders Survey, scored 0–13
From Q2 2007 to Q2 2009, nurses documented PUs significantly more frequently than physicians (96.7% vs 70.6%; p < 0.001). Additionally, PU documentation was complete (specifically noting the stage, size, and location) significantly more often when documented by a nurse than by a physician (46.2% vs 15.2%; p < 0.001). Although physicians documented PUs at a much lower rate than nurses, the documentation rates of physicians and nurses were strongly correlated between Q2 2007 and Q4 2008 with a pairwise correlation coefficient of 0.66.
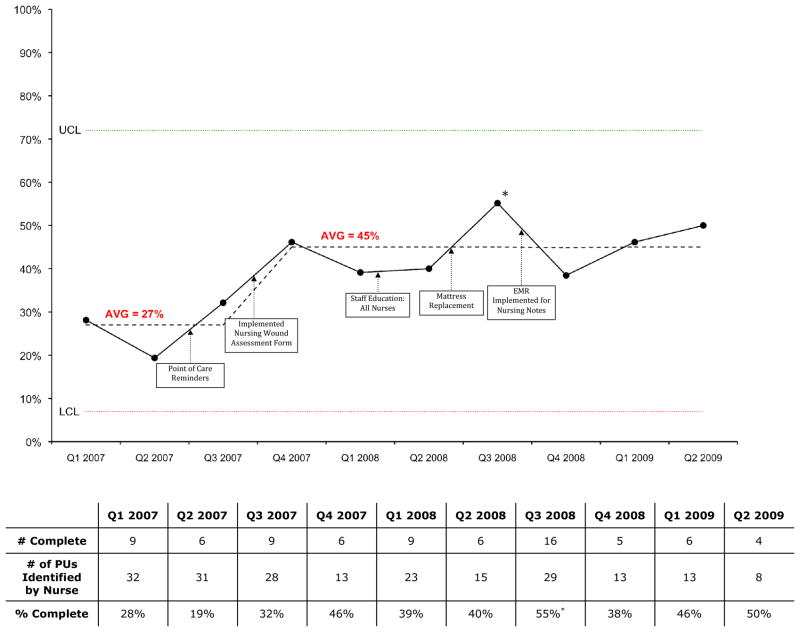
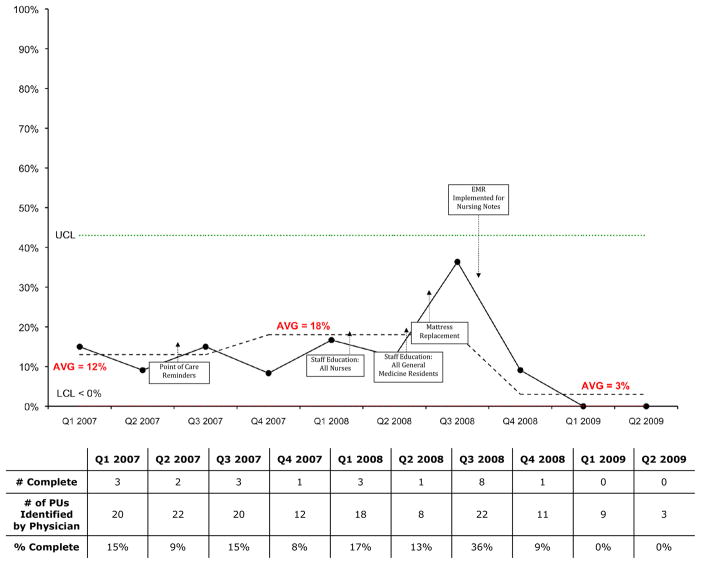
A time course analysis by quarter demonstrates the impact of the multi-component campaign on both physician and nurse documentation practices. Between Q4 2006 and Q2 2007, prior to the implementation of the multi-component campaign, 29% of PUs were completely documented by nurses (Figure 3). After nursing-specific interventions (implementation of the wound assessment form and point of care reminders) in Q2 and Q3 2007, complete documentation by nurses increased to 46% in Q4 2007. These nursing-specific assessments resulted in no discernible deviation in complete documentation by physicians, which remained relatively constant at the baseline of 12% (Figure 4).
Figure 3.
Complete Documentation of Pressure Ulcers in Frail Elders by Nurses (%)
* The improvement in Q3 2008 was statistically significant (p = 0.001)
Figure 4.
Complete Documentation of Pressure Ulcers in Frail Elders by Physicians (%)
The house-wide mattress replacement and general internal medicine resident education, in Q3 2008, resulted in a dramatic increase in documentation quality by both nurses and physicians. Nurses surpassed the goal by completely documenting 55% of PUs (Figure 3) and physicians surpassed the goal and tripled the baseline percentage by completely documenting 36% of PUs (Figure 4). Multivariate logistic regression, adjusting for age, gender, floor, and ICU transfer status, confirms that the increase in Q3 2008 resulted in a significant improvement over the baseline period for nurses. After the resident education and mattress replacement, the odds of a nurse completely documenting a PU were 3.68 (95% CI: 1.68–8.08) greater than baseline (p = 0.001). Although the odds of complete documentation of a PU by a physician also increased, this change was not statistically significant (OR 2.11, p = 0.12, 95% CI: 0.82–5.39).
Unfortunately, the gains were short-lived due to the implementation of EMR for nursing notes in Q4 2008. This change was associated with a large decline in quality of documentation for both physicians and nurses. The decline took place in spite of standard nursing assessments developed by the PU Quality Improvement Team that were embedded in the EMR. The quality of nurse documentation increased once again in Q1 and Q2 2009 with continued instruction. In contrast, during this increase by nurses, complete documentation by physicians fell to a nadir in which no PUs were completely documented. After EMR implementation in Q4 2008, complete documentation rates between physicians and nurses were negatively correlated with a correlation coefficient of −0.95.
Discussion
Summary
The multi-component campaign significantly increased the proportion of completely documented PUs for both physicians and nurses. Specifically, we found that the quality of documentation was significantly increased in the quarter following the general medicine resident education and mattress replacement. However, implementing EMR for nursing notes subsequently decreased the quality of PU documentation.
The time course analysis demonstrated that a majority of the components in the campaign were correlated with improvements in the quality of documentation. However, these improvements were temporary, which emphasizes the need for frequent and repeated educational interventions. The time course analysis, rather than a pre-post analysis, enabled us to assess the positive impact of each component as well as the negative effect EMR implementation had on documentation practices.
When thinking about these results, it is important to consider the documentation practices of physicians and nurses together. First, the multi-component campaign improved physician and nurse documentation of PUs in unison. Second, after EMR implementation decreased the quality of documentation, nurses quickly adapted to the new documentation procedure and their documentation increased in quality once again. However, the quality of physician documentation remained lower than baseline even though the method of physician PU documentation was unchanged. This finding suggests that physicians were documenting PUs using nursing notes rather than physical exam. When EMR was implemented, physicians anecdotally reported that viewing wound documentation in the nursing notes became too cumbersome resulting in fewer PUs documented by physicians.
Relation to other evidence
This campaign attempted to bring the PU improvement model used in long-term care facilities to an academic medical center.21 The significant improvements in PU quality of care we observed closely mirrored those previously seen in long-term care facilities. In both settings, the improvements were short-lived and thus require the interventions to be repeated as well as adapted to changing environments. Additionally, our finding that incorporating EMR actually worsened documentation practices is similar to other studies.22 This further emphasizes the importance of a careful transition to EMR while attempting to reduce potential unintended consequences. This is especially important given the current national interest in transitioning all health care settings to EMR.
Limitations
Because this QI intervention occurred at a single academic institution, generalizability of the results are somewhat limited. Also, CMS’s declaration that Stage III and Stage IV hospital-acquired PUs are “never events” may have encouraged documentation by nurses and physicians. Additionally, the implementation of EMR during the campaign altered the method in which we measured the quality of nurse documentation. This abstraction adjustment required research assistants to be retrained. Finally, the analysis was restricted to those measures on the existing chart abstraction tool. Thus, we are unable to report the changes in other markers of PU care (turning frequency) or documentation in patients who were not deemed to be “frail elders.” Even with these limitations, the chart abstraction proved to be a reliable method to determine documentation practices and the accuracy was assessed throughout the campaign by reviewing a random sample of audited charts. This data collection is ongoing and thus will be used to monitor changes in future documentation practices.
Interpretation
These results indicate that PU specific campaigns, which have traditionally only occurred in long-term care settings can be adapted successfully in an academic medical center. The unexpected decrease in adherence to PU guidelines after EMR was implemented clearly demonstrates the importance of regularly adapting quality improvement campaigns. Additionally, this study shows that PU documentation is remarkably unreliable and thus it should not be used as a trigger for delivering necessary PU support surfaces or care for vulnerable patients. This finding reemphasizes the value of replacing all of the general medicine hospital mattresses with PU specific mattresses. The mattress replacement bypassed the unreliable documentation requirement for delivering PU support, benefited all hospitalized patients, and was found to be cost saving after 11 months.
Conclusions
This study clearly demonstrates that a multi-component campaign can improve PU guideline adherence for both nurses and physicians. However, maintaining this improvement was not possible after nurse documentation was changed to EMR. This emphasizes the need for educational interventions and campaigns to be repeated and adapted to the changing documentation environment to maintain high-quality care. With the national focus on switching to EMR, there is clearly a need for more information on how to successfully transition, while limiting unintended and oftentimes overlooked consequences.
Acknowledgments
This study was funded through the National Institute on Aging Short-Term Aging-Related Research Program (T35AG029795), the Hartford Foundation Health Outcomes Research Scholars Award, Agency for Healthcare Research and Quality Centers for Education and Research on Therapeutics (1U18HS016967-01), and the Pritzker Summer Research Program. Prior presentations on this data include Institute of Healthcare Improvement 2009 Annual Conference in Orlando, FL.
References
- 1.Dharmarajan TS, Ahmed S. The growing problem of pressure ulcers. Evaluation and management for an aging population. Postgrad Med. 2003 May;113(5):77–8. 81–4, 88–90. doi: 10.3810/pgm.2003.05.1409. [DOI] [PubMed] [Google Scholar]
- 2.Bates-Jensen BM, et al. Quality indicators for the care of pressure ulcers in vulnerable elders. J AmGeriatr Soc. 2007 Oct;55(Suppl 2):S409–16. doi: 10.1111/j.1532-5415.2007.01349.x. [DOI] [PubMed] [Google Scholar]
- 3.Allman RM, et al. Pressure ulcers, hospital complications, and disease severity: impact on hospital costs and length of stay. AdvWound Care. 1999 Jan–Feb;12:22–30. [PubMed] [Google Scholar]
- 4.Courtney BA, et al. Save our skin: initiative cuts pressure ulcer incidence in half. Nurs Manage. 2006 Apr;37:36, 38. doi: 10.1097/00006247-200604000-00010. 40 passim. [DOI] [PubMed] [Google Scholar]
- 5.Fried LP. Establishing benchmarks for quality care for an aging population: caring for vulnerable older adults. Ann Intern Med. 2003 Nov 4;139:784–786. doi: 10.7326/0003-4819-139-9-200311040-00014. [DOI] [PubMed] [Google Scholar]
- 6.Lyder CH, et al. A comprehensive program to prevent pressure ulcers in long-term care: exploring costs and coutcomes. Ostomy Wound Manage. 2002 Apr;48:52–62. [PubMed] [Google Scholar]
- 7.McCannon CJ, et al. Miles to go: An introduction to the 5 Million Lives Campaign. Jt Comm J Qual Patient Saf. 2007 Aug;33:477–484. doi: 10.1016/s1553-7250(07)33051-1. [DOI] [PubMed] [Google Scholar]
- 8. [last accessed July 8, 2009];Eliminating Serious, Preventable, and Costly Medical Errors – Never Events. http://www.cms.hhs.gov/apps/media/press/release.asp?Counter=1863.
- 9.Whittington KT, et al. National Prevalence and Incidence Study: 6-year sequential acute care data. Adv Skin Wound Care. 2004 Nov.–Dec;17:490–494. doi: 10.1097/00129334-200411000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Duncan KD. Preventing Pressure Ulcers: The Goal Is Zero. Jt Comm J Qual Patient Saf. 2007 Oct;33:605–610. doi: 10.1016/s1553-7250(07)33069-9. [DOI] [PubMed] [Google Scholar]
- 11.Arora VM, et al. Using assessing care of vulnerable elders quality indicators to measure quality of hospital care for vulnerable elders. J Am Geriatr Soc. 2007 Nov;55:1705–1711. doi: 10.1111/j.1532-5415.2007.01444.x. [DOI] [PubMed] [Google Scholar]
- 12.Harrison MB, Mackey M, Friedberg E, editors. Jt Comm J Qual Patient Saf. 6. Vol. 34. 2008. Jun, Pressure ulcer monitoring: a process of evidence-based practice, quality, and research; pp. 355–9. [DOI] [PubMed] [Google Scholar]
- 13.LeMaster KM, editor. Jt Comm J Qual Patient Saf. 10. Vol. 33. 2007. Oct, Reducing incidence and prevalence of hospital-acquired pressure ulcers at Genesis Medical Center; pp. 611–6.pp. 585 [DOI] [PubMed] [Google Scholar]
- 14.Gibbons W, Shanks HT, Kleinhelter P, Jones P, editors. Jt Comm J Qual Patient Saf. 9. Vol. 32. 2006. Sep, Eliminating facility-acquired pressure ulcers at Ascension Health; pp. 488–96. [DOI] [PubMed] [Google Scholar]
- 15.Arora VM, et al. Relationship Between Quality of Care and Functional Decline in Hospitalized Vulnerable Elders. Med Care. 2009 Aug;47:900–906. doi: 10.1097/MLR.0b013e3181a7e3ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meltzer DM, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002 Dec 3;137:866–874. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 17.Min LC, et al. Higher vulnerable elders survey scores predict death and functional decline in vulnerable older people. J Am Geriatr Soc. 2006 Mar;54:507–511. doi: 10.1111/j.1532-5415.2005.00615.x. [DOI] [PubMed] [Google Scholar]
- 18.Wenger NS, et al. Introduction to the assessing care of vulnerable elders-3 quality indicator measurement set. J Am Geriatr Soc. 2007 Oct;55(Suppl 2):S247–52. doi: 10.1111/j.1532-5415.2007.01328.x. [DOI] [PubMed] [Google Scholar]
- 19.Kottner J, et al. Diagnosis and classification of pressure ulcers and other skin lesions: interrater reliability and agreement. Pflege Z. 2009 Apr;62:225–30. [PubMed] [Google Scholar]
- 20.Baumgarten M, et al. Pressure ulcers among elderly patients early in the hospital stay. J Gerontol A Biol Sci Med Sci. 2006 Jul;61:749–54. doi: 10.1093/gerona/61.7.749. [DOI] [PubMed] [Google Scholar]
- 21.Lyder CH, Shannon R, Empleo-Frazier O, et al. A Comprehensive Program to Prevent Pressure Ulcers in Long-Term Care: Exploring Costs and Outcomes. Ostomy/Wound Management. 2002 Apr;48(4):52–62. [PubMed] [Google Scholar]
- 22.O’Malley A, et al. Are Electronic Medical Records Helpful for Care Coordination? Experiences of Physician Practices. J Gen Intern Med. doi: 10.1007/s11606-009-1195-2. Epub, Dec. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]