Abstract
Using simulation to teach pharmacy practice skills may result in knowledge that is transferable to patient care. Key areas in which simulation is being used in pharmacy education include therapeutics, communication, physical assessment, patient safety, and populations to which students may have infrequent exposure. Enhancing interprofessional healthcare team dynamics and the skills of practicing healthcare professionals are other practical applications for simulation education. Educators should continue to be creative in the incorporation of simulation into pharmacy education and conduct more studies on the impact of simulation education on patient care to demonstrate the efficacy of this teaching modality.
Keywords: assessment, interprofessional education, simulation
INTRODUCTION
The use of simulation for training in areas such as space travel, aviation, and warfare has been widely accepted.1-5 In the healthcare setting, however, the acceptance and adoption of simulation has been embraced only recently.6,7 Increased emphasis on quality of care and patient safety has encouraged the use of simulated medical education experiences in health professions training.8 The use of simulation-based learning has expanded beyond physician education and training to other healthcare disciplines including nursing, physical therapy, and pharmacy.9-12
The Accreditation Council for Pharmacy Education (ACPE) defines simulation as an activity or event that replicates pharmacy practice.13 Simulation-based learning provides students an opportunity to apply previously acquired knowledge and skills in a realistic clinical setting that is a safe and controlled educational environment.14 Simulation-based learning uses a range of mediums from standardized patients to high-fidelity human patient simulation.12,13,15,16
In their 2006 standards and guidelines for pharmacy education programs leading to the doctorate of pharmacy (PharmD) degree, ACPE recommends that faculty members use educational technologies and techniques that encompass a variety of methods of educational delivery and assessment. These standards support the use of simulation to aid in the development of students’ critical-thinking and problem-solving skills.17,18 The use of simulation-based learning in pharmacy education provides students with clinical experiences that they otherwise would not likely acquire in training, such as caring for patients in high-risk and less frequently encountered medical scenarios.13,19-22
In June 2010, ACPE acknowledged simulation-based education as a valuable resource and approved its use in introductory pharmacy practice experiences (IPPEs) to fulfill a portion of a college or school's IPPE program goals and objectives. ACPE recognizes numerous types of simulation as acceptable for use in IPPEs as long as they meet specific criteria that ensure the provision of a learning experience that is comparable to a real patient encounter.13 ACPE deemed the use of simulation to be appropriate for scenarios that are difficult for students to experience in an actual patient care setting, and that are structured around specific learning objectives, include assessment activities, and are supervised by pharmacy educators, practitioners, or appropriately trained facilitators. Contact hours obtained through simulated experiences are perceived as providing similar knowledge as that gained from interacting with live patients in a “real world” setting. However, actual patient contact hours is still to remain a large portion of IPPEs, with simulation allowed to count for up to 20% of required contact hours.13 Although the use of simulation in the pharmacy curriculum has increased, the best applications of this learning method are still being investigated. The purpose of this paper is to describe the benefits of using simulation to teach pharmacy practice skills that are likely to translate into patient care.
SIMULATION IMPROVES STUDENT KNOWLEDGE
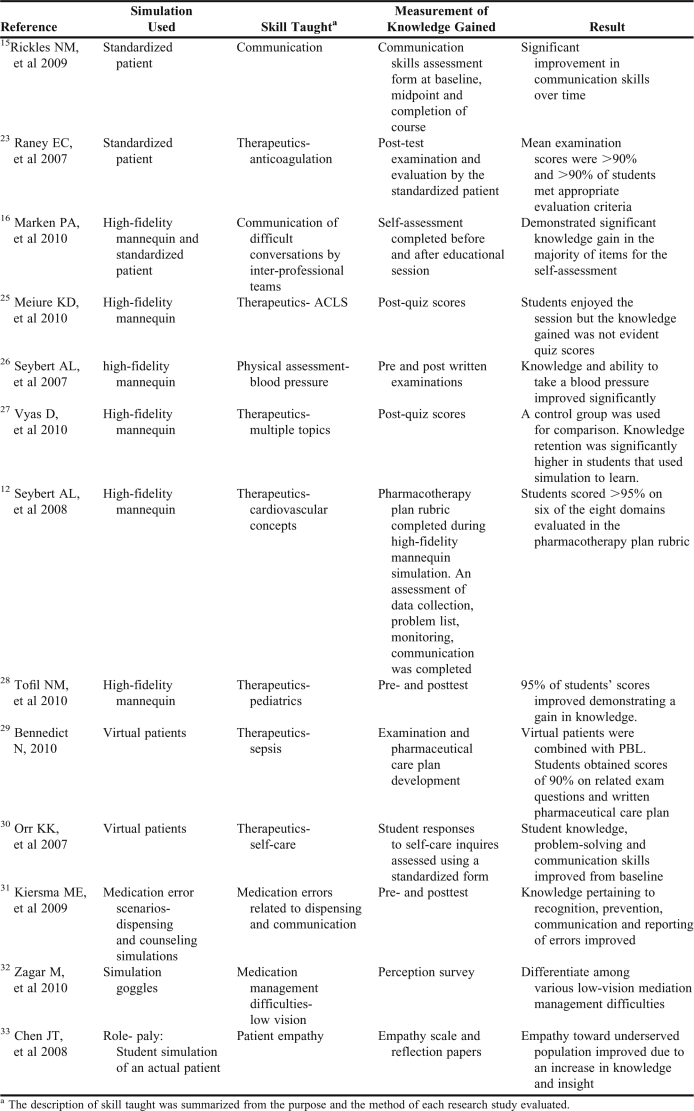
A possible rationale contributing to the ACPE's decision to approve simulation for IPPE contact hours is that improvement in knowledge through active learning can translate into clinical practice. Simulation education is provided in various manners through standardized patients, virtual patients, computer-based simulations, objective structured clinical examinations, and human patient simulation. An extensive review of the literature from 1948 to March 2011 in MEDLINE using the search terms “patient simulation,” “computer simulation” and/or “knowledge or clinical competence” and “pharmacy” or “pharmacist” identified only 69 research articles, the majority of which were not applicable, a second search of only pharmacy education journals available in MEDLINE and the terms “patient simulation” and “computer simulation” was conducted. Twenty articles, all published in the Journal, were identified, and the 13 that involved studies designed to provide simulation learning and assessment of knowledge were included in this review (Table 1).12, 15, 16, 23-33
Table 1.
Use of Simulation to Teach Knowledge to Pharmacy Students
Based on the articles found in the literature review, the areas in which simulation is most often used to teach pharmacy students are: therapeutics, communication, physical assessment, patient safety, and care for patient populations to which students may have infrequent exposure (eg, patients with low vision, underserved patients). Pharmacy educators should continue to be creative in their teaching methods and use of simulation in hopes of enhancing students’ retention of knowledge and their ability to translate the knowledge to clinical practice.
INTERPROFESSIONAL USE OF SIMULATION
Collaborative interdisciplinary learning and training is a central component in the provision of safe, quality patient care.8 The education of healthcare professionals focuses on the development of technical and clinical skills required in their specific discipline and commonly takes place within the profession, with limited exposure and contact with healthcare professionals from other disciplines. There is a lack of training and opportunities to enhance interdisciplinary and team performance in healthcare, even though health care professionals working in teams make less mistakes than health professionals acting independently.34-37
The ACPE has recognized the importance of team-based learning and communication in the education of future pharmacists and stresses the importance of interprofessional team work within the PharmD curriculum.17 Simulation can be used to create scenarios that engage health professions students from multiple disciplines in a stressful environment that presents them with clinical challenges and necessitates communication and teamwork to successfully care for a patient. Simulated scenarios can be used to present health professions students with language barriers, patient-family social issues, lack of readily available clinical information, and other communication conflicts that may arise when working as part of a healthcare team.38 A simulated environment provides a “safe harbor” where the timing in which a scenario normally occurs can be slowed down so that participants can focus on a specific educational aspect, such as the development and acquisition of communication skills.39 During a simulated scenario, healthcare team members are able to identify issues that arise in their daily practice with their daily processes and discuss their professional role and how they can contribute to patient care with other members of the interdisciplinary team.39,40 Common interprofessional simulation scenarios include trauma training, cardiac arrest training, operating room situations, and intensive care unit (ICU) care.19-22
Published studies of the effects of team-based training using simulation support its continued use in pharmacy education. In the setting of trauma training, both subjective and objective improvement in team performance was reported. The trauma teams performed with increased communication and efficiency after sequential simulation experience, and it is believed that simulation not only improved team performance, but was also useful to identify potential safety issues.19 The incorporation of simulation into the training of interprofessional teams for emergency situations produced similar results. Participants reported increased knowledge and insight into the importance of communication in a crisis scenario involving an obstetric emergency.20 A simulation training exercise exposed participants to the health care team's responsibilities in the operating room, promoted effective interaction among team members, and maximized the strengths of each member.21 When simulation was applied to the operating room, significant improvements in role clarity (p = 0.02), cross monitoring (p < 0 .01), anticipatory response (p = 0 .01), and team cohesion and interaction (p < 0.01) took place.30 Using simulation to teach interdisciplinary skills in a high-risk environment provides a safe situation for errors to occur and an effective means of teaching skills that can be transferred and applied in clinical practice.
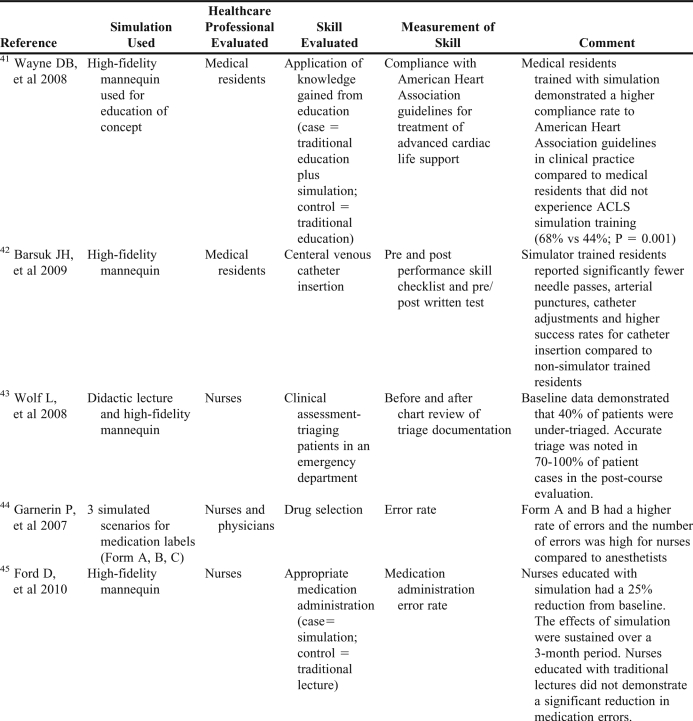
TEACHING KNOWLEDGE AND SKILLS THAT TRANSLATE INTO PRACTICE
Skills taught using simulation scenarios translate into clinical practice improvements (Table 2).41-45 Wayne and colleagues evaluated simulation education provided to second-year medical residents and the translation of this knowledge to clinical practice. 41 Second- and third-year medical residents were included in this analysis with third-year residents being the controls that did not receive simulation education and the second-year residents were the simulation trained group. An evaluation of cardiac arrest team responses for actual in-hospital patients was completed retrospectively. The treatment logs for these patients were evaluated for adherence to the American Heart Association ACLS guidelines and compared for second- and third-year resident led code teams. Simulation education improved the quality of ACLS care since the second-year residents had significantly higher adherence to the guidelines (68% vs. 44%; p = 0.001).
Table 2.
Studies Using Simulation for Education that Demonstrated Improvement in Clinical Practice
No studies evaluating the use of simulation education to train pharmacists in pharmacotherapy skills and the impact of such training on actual clinical practice were found in the literature. Increasing the use of simulation training in pharmacy education may first require the identification of areas that can be enhanced by simulation based education, such as treatment plan development.46,47
Simulation Training to Improve Clinical Skills
The improvement in clinical skills in actual practice as a result of simulation training has also been demonstrated. For example, the use of simulation-based education was effective at increasing the number of successful insertions of central venous catheters in actual patients by medical residents compared to the number successfully inserted by non-simulator trained residents (95% vs. 81%; p = 0.005).42 Similarly, simulation-based training also could be used to hone the compounding and drug preparation skills of practicing pharmacists. Although simulation has been adopted by colleges and schools for use in many pharmacy practice experiences, simulation experiences could also be used to further refine the skills of practicing pharmacists during competency assessments and continuing education sessions. Simulation education also could be used to teach drug preparation and calculations to nurses and pharmacy technicians. Incorporating this active-learning strategy may help health professionals to create a system of zero tolerance for these types of errors.44
Standardized patients disguised as random shoppers/patients to evaluate clinical and communication skills of pharmacists in practice have also been used.47-51 This is an interesting application of simulation as a tool for assessment; however, the primary goal of these studies was not simulation-based learning. Instead, the use of standardized patients could be used as a teaching tool for the enhancement of communication skills for practicing pharmacists as is being done in pharmacy student education. Again, while educators are using simulation to teach skills such as drug preparation and communication to pharmacy students, the value of this teaching modality has not been transmitted to hands-on continuing education of practicing pharmacists nor evaluated for clinical impact in actual patients.
Simulation has been used to improve emergency department nurses’ triaging skills. After completing an educational program that included lectures and scenarios with high-fidelity human patient simulation, the nurses’ triage skills improved 30% to 60%.43 Likewise, pharmacists’clinical skills in detection and reporting of adverse drug reactions may benefit from simulation training such as was used in a computer-based simulation program to improve pharmacists’ ability to identify heparin-induced thrombocytopenia.30,52
An important component of pharmacists’ daily function is to educate other healthcare professionals on the safe use of medications.53 Pharmacists’ use of human patient simulation to educate nurses resulted in a 25% reduction in medication administration errors.45
Because technology changes so rapidly, research studies on the impact of a pharmacy implementing new technology, such as an active medication monitoring system, may not be available.54 Using simulation to test the new technology may prevent errors, or in the case of medication alert systems, prevent alert burden.
Simulation has been used by patient safety organizations such as The Leapfrog Group (Washington, DC) to test the efficacy of active medication monitoring systems at detecting adverse drug events.55-57 In one simulation, a set of physician orders that would result in an adverse drug event was entered in a fictitious electronic patient health record at 62 institutions to determine how well their clinical decision support systems could detect the adverse events.56 The clinical decision support systems at the 62 hospitals detected 53% of medication orders that could have resulted in death and 10% to 82% that could have caused an adverse drug event. As this study illustrates, simulation can be used to test and improve clinical decision support systems.
SUMMARY
A variety of simulation modalities have been used in health care education and practice to teach knowledge and skills, encourage effective team communication, and improve patient care. There are opportunities to increase the use of simulation to train pharmacists’ that could translate into improved pharmacy practice. Pharmacy educators should continue to be creative in the incorporation of simulation into the pharmacy curriculum. Additionally, the use of simulation in educational scenarios should be evaluated for the impact on actual patient care to demonstrate the efficacy of this teaching modality.
REFERENCES
- 1.De Witt JK, Perusek GP, Lewandowski BE, et al. Locomotion in simulated and real microgratvity: horizontal suspension vs. parabolic flight. Aviat Space Environ Med. 2010;81(12):1092–1099. doi: 10.3357/asem.2413.2010. [DOI] [PubMed] [Google Scholar]
- 2.Anderson SB, Morrison RH. Lessons learned from a historical review of piloted aircraft simulations. August 1993; AIAA. Paper 93–3547. http://www.aviationsystemsdivision.arc.nasa.gov/publications/hitl/technical/93-3547.pdf. Accessed October 12, 2011.
- 3.Sullivan BT, Soukup PA. The NASA 747–400 flight simulator: a national resource for aviation safety research. July 1996; AIAA. Paper 96-3517. http://www.aviationsystemsdivision.arc.nasa.gov/publications/hitl/technical/1996_3517.pdf. Accessed October 12, 2011.
- 4.Chung WWY. A review of approaches to determine the effectiveness of ground-based flight simulations. August 2000; AIAA. Paper 2000-4298. http://www.aviationsystemsdivision.arc.nasa.gov/publications/hitl/technical/2000_4298.pdf. Accessed October 12, 2011.
- 5.Kizakevich PN, Lux L, Duncan S, et al. Virtual simulated patients for bioterrorism preparedness training. Studies Health Technol Inf. 2003;94:165–167. [PubMed] [Google Scholar]
- 6.Ostergaard D. National medical simulation training program in Denmark. Crit Care Med. 2004;32(2 Suppl):S58–S60. doi: 10.1097/01.ccm.0000110743.55038.94. [DOI] [PubMed] [Google Scholar]
- 7.Lippert A, Lippert FK, Nielson J, et al. Full-scale simulations in Copenhagen. Am J Anesthesiol. 2000;27:221–225. [Google Scholar]
- 8.Long KA. Institute of Medicine report: health professions education: a bridge to quality report. Policy Polit Nurs Pract. 2003;4(4):259–262. [Google Scholar]
- 9.Gaba DM. Improving anesthesiologists’ performance by simulating reality. Anesthesiology. 1992;76(4):491–494. [PubMed] [Google Scholar]
- 10.Nehring WM, Lashley FR. Current use and opinions regarding human patient simulation in nursing education: an international survey. Nurs Educ Perspect. 2004;25(5):244–248. [PubMed] [Google Scholar]
- 11.Havrilla KJ. Abstract presented at the Association of Schools of Allied Health Professions, Annual Conference; Charlotte, NC: October 21, 2010. High-Fidelity Human simulation – an opportunity for the identification of student preparation for the assessment and treatment of patients in the ICU. [Google Scholar]
- 12.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2):Article 37. doi: 10.5688/aj720237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ACPE. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. S2007, Guidelines 2.0, Preamble Addendum, Appendix D. Chicago, ILL: 2011. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed on October 12, 2011.
- 14.Steadman RH, Coates WC, Huang YM, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34(1):151–157. doi: 10.1097/01.ccm.0000190619.42013.94. [DOI] [PubMed] [Google Scholar]
- 15.Rickles NM, Tieu P, Myers L, Galal S, Chung V. The impact of a standardized patient program on student learning of communication skills. Am J Pharm Educ. 2009;73(1):Article 4. doi: 10.5688/aj730104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marken PA, Zimmerman C, Kennedy, Schremmer R, Smith KV. Human simulators and standardized patients to teach difficult conversations to interprofessional healthcare teams. Am J Pharm Educ. 2010;74(7):Article 120. doi: 10.5688/aj7407120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.ACPE. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree, Standard 25.7. Chicago, ILL: 2011. http://www.acpe-accredit.org/pdf/S2007Guidelines2.0_ChangesIdentifiedInRed.pdf. Accessed on October 12, 2011.
- 18.ACPE. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree, Standard 11.2. Chicago, ILL: 2011. http://www.acpe-accredit.org/pdf/S2007Guidelines2.0_ChangesIdentifiedInRed.pdf. Accessed on October 12, 2011.
- 19.Falcone RA, Daugherty M, Schweer, Patterson M, Browm RL, Garcia VF. Multidisciplinary pediatric trauma team training using high fidelity trauma simulation. J Pediatr Surgery. 2008;43(6):1065–1071. doi: 10.1016/j.jpedsurg.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 20.Freeth D, Ayida G, Berridge EJ, et al. Multidisciplinary obstetric simulated emergency scenarios (MOSES) promoting patient safety in obstetrics with teamwork-focused interprofessional simulations. J Contin Educ Health Prof. 2009;29(2):98–104. doi: 10.1002/chp.20018. [DOI] [PubMed] [Google Scholar]
- 21.Paige JT, Kozmenko V, Yang T, et al. High-fidelity, simulation-based, interdisciplinary operating room team training at the point of care. Surgery. 2009;145(2):138–146. doi: 10.1016/j.surg.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Smith JR, Cole FS. Patient safety, effective interdisciplinary teamwork through simulation and debriefing in the neonatal ICU. Crit Care Nurs Clin North Am. 2009;21(2):163–179. doi: 10.1016/j.ccell.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Raney EC. Assessment of anticoagulation management in a simulated ambulatory care clinic. Am J Pharm Educ. 2007;71(5):Article 97. doi: 10.5688/aj710597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meiure KD, Vincent WE, Cox ME, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiac life support. Am J Pharm Educ. 2010;74(2):Article 22. doi: 10.5688/aj740222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3):Article 48. doi: 10.5688/aj710348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vyas D, Wombwell E, Russell E, Caliguirui F. High-fidelity patient simulation series to supplement introductory pharmacy practice experience. Am J Pharm Educ. 2010;74(9):Article 169. doi: 10.5688/aj7409169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tofil NM, Benner KW, Worthington MA, Zinkan L, White ML. Use of simulation to enhance learning in a pediatric elective. Am J Pharm Educ. 2010;74(2):Article 21. doi: 10.5688/aj740221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bennedict N. Virtual patients and problem=based learning in advance therapeutics. Am J Pharm Educ. 2010;74(8):Atricle 143. doi: 10.5688/aj7408143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Orr KK. Integrating virtual patients into a self-care course. Am J Pharm Educ. 2007;71(2):Article 30. doi: 10.5688/aj710230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kiersma ME, Darbishire PL, Plake K, Oswald C, Walthers BM. Laboratory session to improve first-year pharmacy students’ knowledge and confidence concerning the prevention of medication errors. Am J Pharm Educ. 2009;73(6):Article 99. doi: 10.5688/aj730699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zagar M, Baggarly S. Simulation-based learning about medication management difficulties of low-vision patients. Am J Pharm Educ. 2010;74(8):Article 146. doi: 10.5688/aj7408146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen JT, LaLopa J, Dang DK. Impact of patient empathy modeling on pharmacy students caring for the underserved. Am J Pharm Educ. 2008;72(2):Article 40. doi: 10.5688/aj720240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mesquita AR, Lyra DP, Brito GC, Balisa-Rocha BJ, Aquiar PM, de Almeida Neto AC. Developing communication skills in pharmacy: a systematic review of the use of simulated patient methods. Pat Educ Couns. 2010;78(2):143–148. doi: 10.1016/j.pec.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 34.Salas E, Cannon-Bowers JA, Johnston JH. Naturalistic Decision Making. Mahwah, NJ: Lawrence Erlbaum Assoc; 1997. How can you turn a team of experts into an expert team? emerging training strategies; pp. 359–370. [Google Scholar]
- 35.Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Serv Res. 2006;41(4 Pt 2):1576–1598. doi: 10.1111/j.1475-6773.2006.00566.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith-Jentsch KA, Salas E, Baker DP. Training team performance-related assertiveness. Pers Psychol. 1996;49(4):909–936. [Google Scholar]
- 37.Salas E, Cannon-Bowlers JA. Training and Retraining: A Handbook for Business, Industry, Government, and the Military. New York, NY: Macmillan Reference; 2000. The anatomy of team training; pp. 312–335. [Google Scholar]
- 38.Miller KK, Riley W, Davis S, Hansen H. In situ simulation: a method of experiential learning to promote safety and team behavior. J Perinat Neonatal Nurs. 2008;22(2):105–113. doi: 10.1097/01.JPN.0000319096.97790.f7. [DOI] [PubMed] [Google Scholar]
- 39.Forsythe L. Action research, simulation, team communication, and bringing the tacit into voice society for simulation in healthcare. Simul Healthcare. 2009;4(3):143–148. doi: 10.1097/SIH.0b013e3181986814. [DOI] [PubMed] [Google Scholar]
- 40.Helmreich RL, Merritt AC, Wilhelm JA. The evolution of crew resource management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19–32. doi: 10.1207/s15327108ijap0901_2. [DOI] [PubMed] [Google Scholar]
- 41.Wayne DB, Didwania A, Feinglass J, Fudala MJ. Barsuk, McGaghie. Simulation based education improves quality of care during cardiac arrest them responses at an academic teaching hospital: a case-control study. Chest. 2008;133:56–61. doi: 10.1378/chest.07-0131. [DOI] [PubMed] [Google Scholar]
- 42.Barsuk JH, McGaghie WC, Cohen ER, O'Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive car unit. Crit Care Med. 2009;37:2697–2701. [PubMed] [Google Scholar]
- 43.Wolf L, Mass A. The use of human patient simulation in ED triage training can improve nursing confidence and patient outcomes. J Emerg Nurs. 2008;34:169–171. doi: 10.1016/j.jen.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 44.Garnerin P, Pellet-Meier B, Chopard P, Perneger T, Bonnabry P. Measuring human-error probabilities in drug preparation: a pilot simulation study. Eur J Clin Pharmacol. 2007;63(8):769–776. doi: 10.1007/s00228-007-0319-z. [DOI] [PubMed] [Google Scholar]
- 45.Ford DG, Seybert AL, Smithburger PL, Kobulinsky L, Samosky J, Kane-Gill SL. Impact of simulation-based learning on medication error rates in critically ill patients. Intens Care Med. 2010;36(9):1526–1531. doi: 10.1007/s00134-010-1860-2. [DOI] [PubMed] [Google Scholar]
- 46.Dolovich L, Sabharwal M, Aro K, et al. The effect of pharmacist education on asthma treatment plans for simulated patients. Pharm Word Sci. 2007;29(3):228–229. doi: 10.1007/s11096-006-9080-0. [DOI] [PubMed] [Google Scholar]
- 47.Weiss MC, Booth A, Jones B, Ramjeet S, Wong E. Use of simulated patient to assess the clinical and communication skills of community pharmacist. Pharm World Sci. 2010;32(3):353–361. doi: 10.1007/s11096-010-9375-z. [DOI] [PubMed] [Google Scholar]
- 48.Dyck A, Deschamps M, Taylor J. Pharmacists’ discussions of medication side effects: a descriptive study. Patient Educ Couns. 2005;56(1):21–27. doi: 10.1016/j.pec.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 49.Werner JB, Benrimog SI. Audio taping simulated patient encounters in community pharmacy to enhance the reliability of assessments. Am J Pharm Educ. 2008;72(6):Article 136. doi: 10.5688/aj7206136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schneider CR, Everett AW, Geelhoed E, Kendall PA, Clifford RM. Measuring the assessment and counseling provided with the supply of nonprescription asthma reliever medication: a simulated patient study. Ann Pharmacother. 2009;43(9):1512–1518. doi: 10.1345/aph.1M086. [DOI] [PubMed] [Google Scholar]
- 51.Contopoulos-Ioannidis DG, Koliofoti ID, Koutroumpa IC, Giannakakis IA, Ioannidis PA. Pathways for inappropriate dispensing of antibiotics for rhinosinusitis: a randomized trial. Clin Infect Dis. 2001;33(1):76–82. doi: 10.1086/320888. [DOI] [PubMed] [Google Scholar]
- 52.Rickles NM, Noland CM, Tramontozzi A, et al. Pharmacy student knowledge and communication of mediation errors. Am J Pharm Educ. 2010;74(4):Article 60. doi: 10.5688/aj740460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rudis MI, Brandl KM. Position paper on critical care pharmacy services. Crit Care Med. 2000;28(11):3746–3750. doi: 10.1097/00003246-200011000-00037. [DOI] [PubMed] [Google Scholar]
- 54.Kane-Gill SL, Bellamy CJ, Verrico MM, Saul MI, Handler SM, Weber RJ. Evaluating the positive predictive values of antidote signals to detect potential adverse drug reactions (ADRs) in the medical intensive care unit (ICU) Pharmacoepidemiol Drug Saf. 2009;18(12):1185–1191. doi: 10.1002/pds.1837. [DOI] [PubMed] [Google Scholar]
- 55.Metzger J, Welebob E, Bates DW, Lipsitz S, Classen DC. Mixed results in the safety performance of computerized physician order entry. Health Aff. 2010;29(4):1417. doi: 10.1377/hlthaff.2010.0160. [DOI] [PubMed] [Google Scholar]
- 56.Van der Sijs H, van Gelder T, Vulto A, Berg M, Aarts J. Understanding handling of drug safety alerts: a simulation study. Intern J Med Inform. 2010;79(5):361–369. doi: 10.1016/j.ijmedinf.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 57.Facchinetti NJ, Campbell GM, Jones DP. Evaluating dispensing error detection rates in a hospital pharmacy. Med Care. 1999;37(1):39–43. doi: 10.1097/00005650-199901000-00007. [DOI] [PubMed] [Google Scholar]