Summary
Celiac disease (CD), a malabsorption syndrome with a genetic base, is a consequence of hypersensitivity to GLUTEN-containing foods. CD can manifest with classic symptoms; however, some unusual features like osteomalacia that has become more and more rare, may be the presenting symptom. We describe here a case of osteomalacia secondary to delayed diagnosis of celiac disease. This patient complained about progressive limping, weakness, short stature, and skeletal deformities. Radiological and laboratory findings were all in favor of osteomalacia. Celiac disease was mentioned according to the history of subtle intermittent diarrhea, abdominal discomfort and confirmed with intestinal biopsy and detection of specific autoantibodies. Improvement of patient’s weakness and laboratory abnormalities was obvious after treatment with gluten free diet, vitamin D, calcium and other trace elements. In conclusion, this case affirms that chronic celiac disease especially untreated one, can lead to irreversible complications like skeletal deformities and short stature.
Keywords: osteomalacia, celiac disease, short stature
Introduction
Case Report
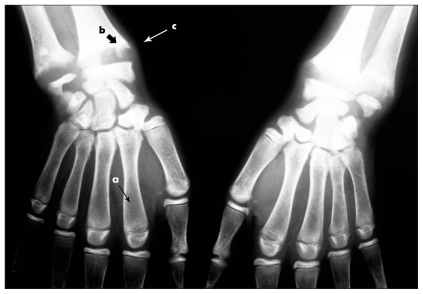
The patient was a 15- year-old girl with growth retardation. She complained about limping and weakness progressed during last previous 6 months. Physical examinations showed proximal myopathy, leg length discrepancy, knee valgus, and wrist widening (Figure 1a,b). Direct enquiry declared that she had no problem until the age of six. After that, she had some weakness, bloating, loss of appetite and a history of intermittent subtle diarrhea, which was not considered important for her parents. She was noted to be 134.5 cm tall and weighed 34 kg with a BMI of 18.79 kg/m2. She experienced her first menstrual cycle when she was fourteen and after that, she had delayed irregular menstrual cycles.
Figure 1.
a) The tissues at the wrists are prominent, a condition reflecting latitudinal widening of the bulky growth plate due to osteomalacia (arrows); b) Genovalgus secondary to growth abnormality in the epiphyseal plate, due to osteomalacia.
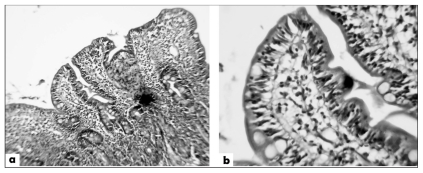
Table 1 shows important laboratory findings in this patient. Low 25OHD, low phosphate, increased alkaline phosphatase and low-normal calcium serum values on top of the skeletal changes (Figure 2) all are in favor of osteomalacia. Muscle enzymes and electromyography study were normal. To explore the etiology of osteomalacia, wide investigations were conducted. Celiac disease (CD) was mentioned according to the history of intermittent slight diarrhea and abdominal discomfort. Elevated serum values of anti tissue trance glutaminase and anti gliadin antibodies, biopsy of intestine (Figure 3), recovery of diarrhea and abdominal discomfort after a gluten free diet, demonstrated the diagnosis of celiac disease. Considering of normal hormonal evaluations, short stature in this patient was attributed to CD. Low serum value of magnesium secondary to chronic diarrhea could explain the normal PTH level, despite of severe osteomalacia in this patient. After treatment with gluten free diet, vitamin D3 (50,000 U weekly for 8 weeks, then 2000U daily for 3 months, and 800 U daily for next 6 months), calcium (1200 mg daily) and other trace elements, patient’s weakness and laboratory abnormalities improved. After 6-months follow up frequency of the diarrhea decreased significantly, she had no bloating, muscle weakness was improved, and she gained weight about 5 kg. Serum values of vitamin D3 (41 ng/dl) and alkaline phosphates (1000 U/l) returned to near normal values. However, it was impossible for her to adhere the gluten free diet completely, therefore calcium (1000 mg/d) and vitamin D(800 U/d) therapy considered for her for a long time with cyclic measurement of serum Ca, and VitD3 concentrations.
Table 1.
Important laboratory parameters in this patient.
| Laboratory test | Result | Normal range |
|---|---|---|
| Calcium (mg/dl) | 8.2 | 8.5–10.5 |
| Phosphorus (mg/dl) | 2.3 | 2.9–5.1 |
| Alkaline phosphates U/l | 1960 | 180–1200 |
| Vitamin 25OHD (ng/dl) | 7 | 20–60 |
| Magnesium (mg/dl) | 1 | 1.9–2.5 |
| 24/h urine calcium (mmol/24h) | 3.9 | 0–7.5 |
| Parotid hormone (PTH) (pg/ml) | 60 | 10–65 |
| Thyroid stimulating hormone (TSH) (U/L) | 9 | 1.33–8.65 |
| Insulin Growth factor 1 (IGF1) (ng/ml) | 252 | 131–540 |
| 24/h urine Cortisol (mcg/24h) | 17 | 10–100 |
| Luteinizing hormone (LH) (IU/l) | 4.9 | <10 |
| Follicle stimulating hormone (FSH) (IU/l) | 2 | <11.5 |
| Estradiol (pg/ml) | 50 | 15–71 |
| Hemoglobin (mg/dl) | 8.1 | 12–15.2 |
| Creatinine (mg/dl) | 0.5 | 0.6–1.3 |
| Anti tissue transglutaminase antibody (U/ml) | >200 | Up to 20 |
| Anti gliadin antibody IgG (U/ml) | 50 | UP to 5 |
Figure 2.
Generalized demineralization (a) is present, with disorganization (b) and widening of the areas (c) subjacent to the growth plates in the wrists, secondary to severe osteomalacia.
Figure 3.
a) Intestinal biopsy in celiac disease: blunting of the villi, decrease in villi crypt ratio, villi abnormality, infiltration of lymphocyte cells in lamina properia and epithelial cells; b) Infiltration of lymphocyte cells in epithelial cells.
Discussion
Celiac disease is a malabsorption syndrome that is precipitated by the ingestion of gluten-containing foods, characterized by inflammation of the small intestine leading to malnutrition (1). Genetical susceptibility and autoimmunity are the most important predisposing factors for CD. It can be manifested with classic symptoms such as diarrhea, weight loss, and anemia; but, sometimes with unusual symptoms like osteoporosis and osteomalacia (2). Intestinal malabsorption, a result of celiac disease can present with different clinical manifestations, including growth retardation; osteoporosis and occasionally osteomalacia. Osteomalacia in CD is a result of decreased absorption of vitamin D secondary to the involvement of small intestine. Malekzadeh et al. proposed similar or even higher prevalence of CD in developing countries like Iran, compared with western countries (3). Celiac disease induced osteomalacia, was first reported in 1953 (4). In an old child, valgus deformities of the legs may be apparent as we saw in this case. Although clinical and radiological evidence of osteomalacia, a late feature of vitamin D deficiency, has become rare in CD (5), this patient showed typical manifestations. Mazure et al. (6) and Valdimarsson et al. (7) proposed that despite the decreasing of bone mineral density secondary to malabsorption in CD, osteomalacia is a rare finding. Few case-reports demonstrated the correlation between osteomalacia and CD, most of them were clinically asymptomatic form of CD (1). However, these severe manifestations of osteomalacia and growth retardation in our patient, seems to be presented due to delayed diagnosis of CD. In conclusion, this case affirms that chronic celiac disease especially untreated one, can lead to irreversible complications like skeletal deformities and short stature.
Acknowledgments
We appreciate this patient and her family for giving permission to submit her information in this report. We also express appreciation to Dr Nema Mohammadian Roshan, Assistant Professor of Pathology.
References
- 1.Harzy T, Benbouazza K, Amine B, Rahmouni R, Hajjaj-Hassouni N. An unusual case of osteomalacia as the presenting feature of coeliac disease. Rheumatol Int. 2005;26:90–1. doi: 10.1007/s00296-005-0601-2. [DOI] [PubMed] [Google Scholar]
- 2.Albany C, Servetnyk Z. Disabling osteomalacia and myopathy as the only presenting features of celiac disease: a case report. Cases J. 2009;2:20. doi: 10.1186/1757-1626-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malekzadeh R, Shakeri R. Celiac disease in Iran. TUMJ. 2007;65:1–11. [Google Scholar]
- 4.Basu RA, Elmer K, Babu A, Kelly CA. Coeliac disease can still present with osteomalacia! Rheumatology (Oxford) 2000;39:335–6. doi: 10.1093/rheumatology/39.3.335. [DOI] [PubMed] [Google Scholar]
- 5.Landolsi H, Bouajina E, Mankai A, Zeglaoui H, Skandrani K, Ghedira I. Severe osteomalacia due to undiagnosed coeliac disease: three case reports of Tunisian women. Rheumatol Int. 2006;26:261–3. doi: 10.1007/s00296-005-0618-6. [DOI] [PubMed] [Google Scholar]
- 6.Mazure R, Vazquez H, Gonzalez D, et al. Bone mineral affection in asymptomatic adult patients with celiac disease. Am J Gastroenterol. 1994;89:2130–4. [PubMed] [Google Scholar]
- 7.Valdimarsson T, Toss G, Ross I, Lofman O, Strom M. Bone mineral density in coeliac disease. Scand J Gastroenterol. 1994;29:457–61. doi: 10.3109/00365529409096838. [DOI] [PubMed] [Google Scholar]