Summary
There are many conditions that may be responsible of a painful knee prosthesis. The possible causes are not always easily diagnosed. Common causes of prosthetic failure, such as aseptic loosening, infection, instability, progressive patellar arthropathy and recurrent synovitis are associated with clearly defined radiographic and/or clinical evidence. Prosthetic infection should always be considered first until any other cause has been demonstrated. In the presence of an infected prosthesis we carry out a two-step revision. Aseptic loosening needs implant revision more often with increasing prosthesis stability. Varus-valgus, anteroposterior, global and patello-femoral instability are failures often due to technical errors; superstabilized or constrained implants are needed depending on the instability entity.
In presence of patello-femoral pain it is necessary to evaluate the stability of the patellar component and any alterations in its motion. Patellar progressive arthropathy can often cause late-onset knee pain; in this case patella resurfacing is needed. Altered patellar tracking, may need a lateral release but in some cases is related to misalignment of the components and the revision procedure is mandatory. Nevertheless, the diagnosis and treatment of a painful knee prosthesis can be extremely difficult if there is no clear evidence of any of the most common causes of failure. Referred pain, ligament and tendon dysfunction, cutaneous neuromas, synovitis, a patellar clunk have to be diagnosed and treated.
A possible aetiological understimated factor is painful knee prosthesis due to metals sensibilization, in particular to nickel. In this event the quantity of nickel in the revision prosthesis must be minimal.
Keywords: painful total knee arthroplasty, prosthesis failure, knee revision, hypersensitivity to metals
Introduction
The number of revision of total knee arthroplasties is rising exponentially with a projected increase of 601% from 2005 to 2030 (1). For this reason it is very important to have a systematic approach dealing with a patient presenting with a painful TKA. A painful knee prosthesis is, unfortunately, a condition whose possible causes are not always easily diagnosed. As a consequence, it can be difficult to resolve.
Common causes of prosthetic failure, such as infection, aseptic loosening, instability, progressive patellar arthropathy and recurrent synovitis, are associated with clearly defined radiographic and/or clinical evidence.
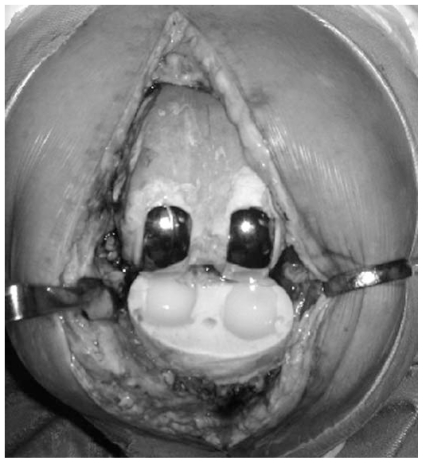
Prosthetic infection should always be considered first, and remain a possibility of failure until any other cause has been demonstrated. Commonly used laboratory tests, including a complete blood count with differential (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and knee aspiration for cell count and culture are always to be considered of primary importance in the diagnostic work up of a painful prosthesis. In the presence of an infected prosthesis we carry out a two-step revision, first using an articulating antibiotic-impregnated cement spacer with two mono-compartment components to preserve the range of movement (Figure 1). After the infection has been resolved, we carry out new prosthetic surgery, generally using prostheses of increasing stability and bone grafts depending on the residual bone stock.
Figure 1.
Articulating antibiotic-impregnated cement spacer is assembled with two unicompartmental knee components.
Aseptic loosening of a knee prosthesis is a complication that is easily identified radiographically due to the presence of lines of radiolucency at the bone/prosthesis interface, associated with migration or angulation of the components. In these cases, it is necessary to revise the prosthesis, increasing its stability with diaphyseal stems. With regard to this problem, we have, recently, also been evaluating the opportunity and efficacy of pre and post-operative treatment with bone-forming agents in patients with poor bone quality, in order to reduce the risk of loosening and extend the life of the prosthesis.
Varus-valgus, anteroposterior, global and patello-femoral instability are failures, often due to technical errors, that can be diagnosed through clinical examination. In the presence of a painful prosthesis associated with frank instability, we perform revision using superstabilised or constrained implants, depending on the particular case.
If pain is of patello-femoral origin it is necessary, in the case of a prosthetic patella, to evaluate the stability of the component and any alterations in its motion. As far as the surgical technique is concerned, in cases in which patellar lateralisation is performed, medialising the button so as to obtain improved tracking, we recommend not using a too small patellar component and performing an oblique osteotomy laterally to the button in order to reduce the risk of pain due to non-lined patella/femoral component interference.
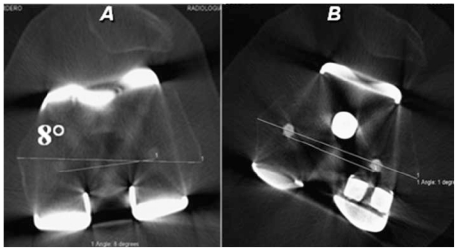
In the presence of a natural patella progressive arthropathy can often cause late-onset knee pain at anterior patellar level; in this case, prosthetic patella insertion is needed with, in the event of altered tracking, lateral release. In some cases patello-femoral pain is related to malalignment of the components, which can be evaluated precisely through the superimposition of references in CT images (2). Briard and Hungerford (3) described this relationship that explains the failed knee arthroplasty.
In this situation it is essential to perform a revision of the prosthesis, seeking to obtain the correct rotations and correct mechanical axis alignment. In our experience we prefer an implant with asymmetrical condyles in order to avoid medial femoral condyle sacrifice to reach the correct component rotation (Figure 2). Diaphiseal extended shaft with off-set can lateralize the implant to improve patellar tracking if necessary.
Figure 2.
Superimposition of references in CT images shows 8° internal rotation of the femoral component (A). Correct alignment after revision (B).
Nevertheless, the diagnosis and treatment of a painful knee prosthesis can be extremely difficult if there is no clear evidence of any of the most common causes of failure.
Referred pain related to an upper lumbar radiculopathy, an ipsilateral hip arthritis or a vascular disease, may be not a rare condition and must be distinguished from knee pain.
In the presence of prosthetic components having large diaphyseal shafts, a sharp pain can be detected; in these situations, it is sometimes possible to observe, on radiographic examinations, effects of periprosthetic stress shielding. To solve the problem, the component has to be replaced with one having a stem with a smaller diameter.
A painful prosthesis accompanied by a patellar clunk can be attributed to the formation of a subquadricipital fibrous nodule proximal to the patella which can be responsible of impingement with the anterior margin of the posterior-stabilising femoral component box (4). The nodule may be caused by chronic quadriceps tendon irritation correlated to a thin patellar component, a flexed femoral component, or for a too high patellar botton. The nodule becomes entrapped within the intercondylar notch of the femoral component and then “clunks” as the knee extends. Arthroscopic removal of the fibrous nodule can solve the pain.
Painful, recurrent hemarthroses have been reported by several authors (5,6) and usually are the result of synovial entrapment or the presence of pigmented villonodular synovitis. Intra-articular soft-tissue irritation can occur from a number of sources, including retained distal femoral osteophytes (7), extruded bone cement, or intra-articular fibrous bands (8). These conditions can be effectively treated arthroscopically.
Popliteus tendon dysfunction with lateral pain and snapping may occur in case of tendon subluxation over a retained lateral femoral osteophyte or an overhanging lateral edge of the femoral component. Arthroscopic release of the tendon has shown good results (9).
Irritation of the collateral ligaments can result from an overhang of the tibial component beyond the osseus periphery. This is observed most commonly at the medial aspect of the tibia because of the close proximity of the medial collateral ligament.
Pes anserinum bursitis and ileotibial band irritation are particular conditions that can produce knee pain.
Cutaneous neuromas are not frequent cause of pain following TKA. Dellon reported results 70 patients with painful cutaneous neuromas following TKA (10). Infrapatellar branch of the saphenous or the medial retinacular nerves are most commonly interested. Pain resolution was obtained in 86% of patients with denervation procedures.
A stiff knee is a not rare condition of TKA pain. Different and unbalanced flexion/extension gaps, malalignment of components, oversized femoral component, posterior ostephytes at the femoral condyles and heterotopic ossification can be responsible of stiffness and must be treated.
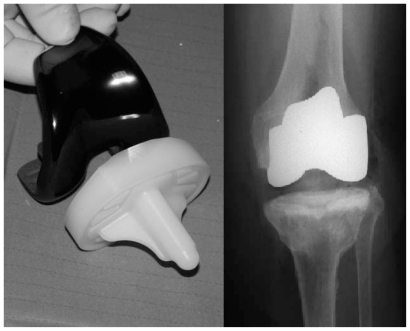
Another possible aetiological factor in painful knee prosthesis is allergy to metals, in particular to nickel. Diagnosis of metal allergy, but above all its role in the pain, is currently much debated. Therefore, before carrying out the revision procedure, it is worth excluding all other possible causes and ascertaining, beyond doubt, the degree of the allergy itself. Diagnosis by means of a skin patch test does not currently seem to be of undisputed diagnostic value (11); in our practice, we effect diagnoses on the basis of blood tests, looking carefully for specific cytokines, activated cell lines with thymidine labelling and confocal microscopy. Laboratory diagnostic work up of patients identified on the basis of history makes it possible to avoid failures due to sensitivity to metals. We use to implant femoral component in oxidized zirconium, lacking in nickel, and all-poly tibial component to prevent metal sensibilization problem in allergic patients (Figure 3). In the event of allergy-related failure, the quantity of nickel in the revision prosthesis must be minimal as possible.
Figure 3.
Oxidized zirconium femoral component and all-poly tibial tray implanted in an allergic patient.
In summary, there are multiple causes of pain following total knee arthroplasty. A systematic approach with physical examination, laboratory testing and radiographic evaluation is necessary to determine the etiology of pain. Proceeding with revision is unwise if the etiology of pain cannot be determined. If revision surgery is performed without a defined diagnosis is frequently associated with poor results (12).
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Berger RA, Crossett LS, Jacobs JJ, et al. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop. 1998;356:144. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Briard JH, Hungerford DS. Patellofemoral instability in total knee arthroplasty. J Arthroplasty. 1989;4(Suppl):S87. doi: 10.1016/s0883-5403(89)80013-0. [DOI] [PubMed] [Google Scholar]
- 4.Hozack WJ, Rothman RH, Booth RE, et al. The patellar clunk syndrome. A complication of posterior stabilized total knee arthroplasty. Clin Orthop. 1989;241:203. [PubMed] [Google Scholar]
- 5.Worland RL, Jessup DE. Recurrent hemarthrosis after total knee arthroplasty. J Arthroplasty. 1996;11:977. doi: 10.1016/s0883-5403(96)80144-6. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham RB, Mariani EM. Spontaneous hemarthrosis 6 years after total knee arthroplasty. J Arthroplasty. 2001;16:133. doi: 10.1054/arth.2001.9050. [DOI] [PubMed] [Google Scholar]
- 7.Dennis DA, Channer M. Retained distal femoral osteophyte: an infrequent cause of postoperative pain following total knee arthroplasty. J Arthroplasty. 1992;7:193. doi: 10.1016/0883-5403(92)90016-j. [DOI] [PubMed] [Google Scholar]
- 8.Lintner DM, Bocell JR, Tullos HS. Arthroscopic treatment of intraarticular fibrous bands after total knee arthroplasty. A follow-up note. Clin Orthop. 1994;309:230. [PubMed] [Google Scholar]
- 9.Barnes CL, Scott RD. Popliteus tendon dysfunction following total knee arthroplasty. J Arthroplasty. 1995;10:543. doi: 10.1016/s0883-5403(05)80159-7. [DOI] [PubMed] [Google Scholar]
- 10.Dellon AL, Mont MA, Mullick T, et al. Partial denervation for persistent neuroma pain around the knee. Clin Orthop. 1996;329:216. doi: 10.1097/00003086-199608000-00027. [DOI] [PubMed] [Google Scholar]
- 11.Brown GC, Lockshin MD, Salvati EA, et al. Sensitivity to metal as a possible cause of sterile loosening after cobalt-chromium total hip-replacement arthroplasty. J Bone Joint Surg Am. 1977 Mar;59(2):164–8. [PubMed] [Google Scholar]
- 12.Mont MA, Serna FK, Krackow KA, et al. Exploration of radiographically normal total knee replacement for unexplained pain. Clin Orthop. 1996;331:216. doi: 10.1097/00003086-199610000-00030. [DOI] [PubMed] [Google Scholar]