Summary
Total Knee Arthroplasty (TKA) is one of the most successful procedures in Orthopaedic Surgery, with good clinical results and high survival rate in more than 90% of the cases at long-term follow-up. Since the increase of population’s mean age, worsening of articular degenerative alterations, and articular sequelae related to previous fractures, there is a persistent growing of the number of knee arthroplasties in every country each year, with expected increase of complications rates. Painful TKA is considered an unusual complication, but several reports focus on this challenging clinical issue.
Common causes of painful TKA may be divided as early or late, and in referred, periarticular or intra-articular. Among the early, we recall implant instability (related to surgical and technical mistakes) and problems of extensor mechanism (patella not resurfaced, malalignment of femoral, tibial, or patellar component, tendons failure or degeneration). Late causes of painful TKA are almost related to aseptic loosening and infection, but also, even if unusual, reflex sympathetic dystrophy, synovitis, and hypersensitivity to metal implants are represented.
Hypersensitivity to metal is a clinical issue with significative increase, but to date without a specific characterization. The Authors report about incidence, clinical features, and diagnostic pathways of hypersensitivity to metal implants, focusing on the prevention of this challenging problem.
Keywords: painful total knee arthroplasty, hypersensitivity to metal
Introduction
Total knee arthroplasty (TKA) is one of the most successful procedures of orthopaedic surgery, according good clinical results in more than 90% of cases at long-term follow-up (1–3).
Increase in population’s mean age and related worstening of articular diseases during last decades induced a worldwide arise of the number of knee arthroplasties each year: as result, complications and failures rates also show an expected growing (1,2). Even its proven efficacy in large series, a little percentage of implants may not induce a relief from symptoms, determining patients’ complaints and surgeons’ frustration: thus, it becomes fundamental to understand the cause of the unsuccessful situation in a way to find an efficient resolution.
Causes of painful total knee arthroplasty
Historically, common causes of failure of TKAs needing revision include aseptic loosening, infection, and instability (2). Majority of surgeons is familiar with classical findings associated with these conditions, and diagnosis is generally easy.
Commonly, loosening represents a late mechanism of failure, leading to progressive arising of pain, functional limitation, difficult weight-bearing, gait alterations. Clinical history and periodic evaluation with x-rays are sufficient to assess this condition and usually success is reached when revision is performed.
Instability after TKA is an early cause of revision. Usually, patients complaint symptoms since the outset of a TKA, and diagnosis is made with clinical examination, x-rays evaluation (also by means of stress devices or fluoroscopy), and CT scan with study of rotational positioning of the components. Revision is mandatory, possibly substituting the only components involved in malpositioning.
Occurrence of a septic involvement is quite unpredictable, and has to be always considered in differential diagnosis in painful implants: as general rule, a painful TKA has to be presumed as infected until otherwise proven. Clinical history, imaging, bone scan with marked leukocytes, repeated laboratory tests focused on erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), complete blood cell count, and in some cases knee aspiration are usually enough to prove infection. Two-stage revision with implant of an antibiotics-charged spacer is commonly considered the gold standard in these cases.
However, painful TKA may not correspond to any of the previous mechanisms of failure: thus, a symptomatic knee arthroplasty without any altered clinical, radiological, and laboratory findings represents a challenge in modern Orthopaedics.
It is useful to divide the causes of painful TKA in referred, periarticular, and articular (4). Majority of this conditions may be treated by medical and physical therapy, while others need a surgical approach, usually challenging and not free from further complications. Referred causes of painful TKA may be commonly related to spinal pathologies, as lumbar stenosis, discopathy, discal hernia with crural irradiation of pain. Moreover, an ipsilateral hip situation may presents with knee pain (arthritis, avascular necrosis of proximal femur, femoro-acetabular impingement).
Periarticular causes of pain may be principally related to iliotibial band irritation or inflammation, and pes anserinus bursitis: the latter, often present in knee arthritis before TKA, may be persistent for months after surgery.
Fibromyalgia is a rare dysfunctional disease that may overlapping or sprouting after TKA, even it is generally associated with other regional complaints by patients usually affected by behaviour disorders.
Among intra-articular causes of painful TKA, abnormal patellar tracking may represents one of the most frequent mechanisms. Malposition of femoral and/or tibial component, in particular concerning their rotational alignment or medial/lateral position, may alter the interaction between patella (resurfaced or native) and femoral throclea, leading to anterior knee pain and even instability (lateral subluxation or dislocation).
A tibial component positioned too medially or larger than necessary (in lateral size) may explain an anteromedially pain over the tibial plateau, with poor response to medical or physical therapy. Even not frequent, cementless stemmed TKA may cause persistent symptoms over the middle and distal femur or proximal and middle tibia. A not resurfaced patella with progression of degenerative changes after TKA may also produce anterior knee pain during flexion activities.
Patellar clunk is the result of a fibrous nodular structure forming between the bone and the quadriceps tendon, catching over the box generally of a posterior stabilized femoral component, and causing painful and palpable crepitus while sitting on or rising from a chair. Chronic inflammation or degenerative changes of patellar tendon can produce symptoms and lead to functional impairment after a knee replacement. Sympathetic reflex dystrophy is an uncommon disease involving joints generally after a minor trauma or immobilization: persistent pain at rest and during movement, limp, and skin alterations (dyschromic changes, excessive sweating, hyperalgesia).
Synovitis is a not frequent cause of pain in a TKA, due generally to joint effusion or haemarthrosis and typical of patients with haematological disease, as Haemophilia or other coagulopathy. Nonetheless, it may represent the result of an abnormal response of immunologic status for hypersensitivity to metals: this represent an arising problem, still to be well understood, and leading often to a symptomatic synovitis.
Particularly, this is one of the most challenging situation recently presenting to Orthopaedic Surgeons.
Hypersensitivity to metals
Hypersensitivity to metals is thought to affect almost 10% of general population, principally determined by professional exposure or daily contact with jewerly, beauty and cleaning products. Result is a pending risk of abnormal response of joints and whole body after contact with such substances (5–10).
On a side, some patients know theirselves to be allergic, tipically to Nickel, having experienced before some dermal irritation to such material.
The actual challenge is to identify a sensitive patient candidate to joint replacement never suspected to be. Patch tests for metal hypersensitivity is a common tool to verify altered immunological status on these substances (Nickel, Chromium, Cobalt) (5,6); however, it is a high-sensibility but low-specificity test, and it is clear that dermal response may not equally correspond to articular space, since synovial tissue, well represented in the knee, is particularly reactive to immunogenic stimuli (7). In vitro assessments as Limphocyte Transformation Test (LTT), Migration Inhibition Factor (MIF), and evaluation of cytokines concentration with ELISA method are investigations recently introduced, but still now there is debate on how quantify and qualify the response in terms of reproducibility (8).
On the other side, suspect sensitive patients present after replacement with well-functioning and integrated TKAs, but with large symptomatic effusion of the knee, itching on different part of their body, and important functional impairment. Treatment with anti-inflammatory drugs, steroids, physical therapy do not minimize symptoms: usually, revision with a non-allergic implant is the solution to this unpleasant issue.
Implant of a non-allergic TKA is obviously the unique way to prevent clinical issues in well-known metal-allergic patient: nowadays, it is possible to dispose of various primary knee systems with alternative bearings or coatings (Oxidized Zirconium, Zirconium Ni-trure, Ceramic).
Personal diagnostic protocol
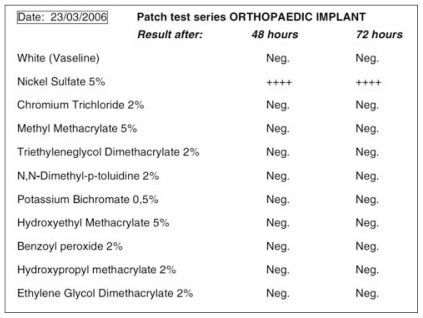
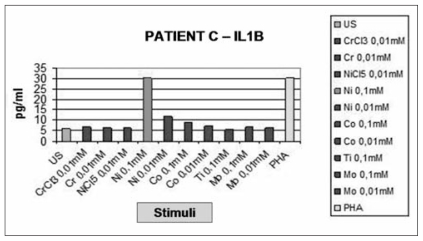
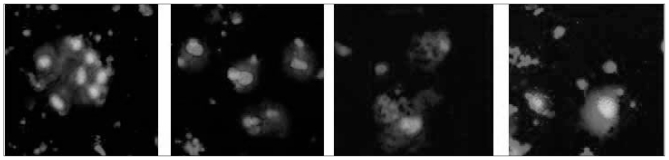
In our Department, since 2007, each patient candidate to joint arthroplasty is deeply questioned on his previous occupation, eventual exposition to specific substances and about familiar allergies: in case of suspect, we perform a patch testing (Nickel, Chromium, Cobalt), blood examination to assess the concentration of specific cytokines, macrophages colture and reaction and radioimmunotesting for thymidine activated cell lines evaluated by LASER confocal microscopy. If any of these results is supposed to be positive, we proceed on knee replacement with a primary anallergic implant, in a way to prevent any future hypersensitivity (Figures 1a-d).
Figure 1a.
Patch test in suspected metal hypersensitive patient.
Figure 1b.
Cytokines assay on the same patient’s blood sample.
Figure 1c.
Confocal microscopic analysis by LASER and “Z-stack” method.
Figure 1d.
Microscopy evaluation of monocytes before (1 and 2 frames) and after (3 and 4 frames) nickel stimulation.
Preliminary results show patient-dependent patterns of excessive immune response with altered production of specific cytokines, as Interleukin 8 (IL-8) and Macrophage Inflammatory Protein-1 (MIP1 alpha and beta), even if IL-1 and IL-2 are still well represented, demonstrating a T-cell and macrophages hyperstimulation. Future challenge will be to assess a reproducible qualitative and quantitative standard of evaluation (11–14).
On the other side, we treat also many cases of painful TKA, coming from several regions of the country, and our management is firstly concentrated on the study of the actual cause of failure.
It is in fact of paramount importance before proceeding with a revision to be sure of the real factors leading to symptoms, in order to plan as better possible any single procedure.
Classical approach to the assessment of a painful TKA starts with clinical history, data concerning previous surgery and implanted components, accurate physical examination: these are basically essential to approach a painful joint after a replacement, particularly, focus on extra-articular causes and assessment of correct implant positioning, mandatory to make a differential diagnosis. Full radiographic study of the entire limb, CT scan to verify correct alignment and rotational positioning of the components, and MRI scan to rule out soft tissue pathologies are also necessary. Moreover, if these studies are not useful to define a specific clue, it is necessary to re-assess the entire examinations after a certain period, or to switch to uncommon causes, as fibromyalgia, synovitis, hypersensitivity to metals. In the latter, we use to proceed as previously mentioned, and in case of heavy suspect, we perform revision arthroplasty. It is clear that the better strategy is to prevent any form of intra- or post-operative problem, even if common causes of TKA failure (aseptic loosening, infection) are not predictable and not always under Surgeon’s control.
Further studies will be necessary to be sure that this diagnostic pathway is correct and to reach a reproducibility in the assessment of a metal hypersensitivity, that would have an important relevance on clinical settings, and impact on population and society.
Acknowledgements
Each Author certifies the originality of this paper and its content. All Authors certify that no commercial associations or consultancies have posed any conflict of interest in connection with the submitted article.
No fundings from companies or industry were considered and have not biased the result on the paper.
The Authors wish to thank Prof. M.L. Brandi and Dr. A.M. Carossino for their precious contribution.
References
- 1.Knutson K, Lewold S, Robertsson O, Lidgren L. The Swedish knee arthroplasty register: A nation-wide study of 30,003 knees 1976–1992. Acta Orthop Scand. 1994;65:375–386. doi: 10.3109/17453679408995475. [DOI] [PubMed] [Google Scholar]
- 2.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Ritter MA. The Anatomical Graduated Component total knee replacement. A long-term evaluation with 20-years survival analysis. J Bone Joint Surg Br. 2009;91:45–49. doi: 10.1302/0301-620X.91B6.21854. [DOI] [PubMed] [Google Scholar]
- 4.Fhering TK, Christie MJ, Lavernia C, Bohannon Mason J, McAuley JP, MacDonald SJ, Springer BD. Revision total knee arthroplasty: planning, management and controversies. AAOS Instr Course Lect. 2008;57:341–362. [PubMed] [Google Scholar]
- 5.Basketter DA, Briatico-Vangosa G, Kaestner W, Lally C, Bontick WJ. Nickel, Cobalt and Chromium in consumer products: a role in allergic contact dermatitis? Contact Dermatitis. 1993;28:15–25. doi: 10.1111/j.1600-0536.1993.tb03318.x. [DOI] [PubMed] [Google Scholar]
- 6.Swiontkowsky MF, Agel J, Schwappach J, McNair P, Welch M. Cutaneous metal sensitivity in patients with orthopaedic injuries. J Orthop Trauma. 2001;2:86–89. doi: 10.1097/00005131-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Granchi D, Cenni E, Tignai D, Trisolino G, Baldini N, Giunti A. Sensitivity to implant materials in patients with total knee arthroplasty. Bio-materials. 2008;29:1494–1500. doi: 10.1016/j.biomaterials.2007.11.038. [DOI] [PubMed] [Google Scholar]
- 8.Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surgery. 2001;83-A:428–436. doi: 10.2106/00004623-200103000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Merritt K, Rodrigo JJ. Immune response to synthetic materials. Sensitization of patients receiving orthopaedic implants. Clin Orthop Relat Res. 1996;326:71–9. [PubMed] [Google Scholar]
- 10.McKenzie AW, Aitken CV, Ridsdill-Smith R. Urticaria after insertion of Smith-Petersen Vitallium nail. Br Med J. 1967;5570:36. doi: 10.1136/bmj.4.5570.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hallab NJ, Caicedo M, Epstein R, McAllister K, Jacobs JJ. In vitro reactivity to implant metals demonstrates a person-dependent association with both T-cell and B-cell activation. J Biomed Mater Res. 2010;92:667–82. doi: 10.1002/jbm.a.32368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hallab NJ, Caicedo M, Finnegan A, Jacobs JJ. Th1 type lymphocyte reactivity to metals in patients with total hip arthroplasty. J Orthop Surg Res. 2008;13:3–6. doi: 10.1186/1749-799X-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacobs JJ, Hallab NJ. Loosening and osteolysis associated with metal-on-metal bearings: A local effect of metal hypersensitivity? J Bone Joint Surg. 2006;88-Am:1171–2. doi: 10.2106/JBJS.F.00453. [DOI] [PubMed] [Google Scholar]
- 14.Hallab NJ, Jacobs JJ. Biologic effects of implant debris. Bull NYU Hosp Jt Dis. 2009;67:182–8. [PubMed] [Google Scholar]