Abstract
Objective: To investigate the diagnostic value of MCA/UA pulsatility index ratio for the prediction of adverse perinatal outcome in the fetuses with preeclampsia and gestational hypertension.
Materials and methods: We included in the study 738 patients recovered in our Hospital with the diagnosis of preeclampsia and gestational hypertension, from January 2006 to December 2009. All the patients underwent accurate color Doppler velocimetry examination. The study population was divided into two groups depending on the normal or abnormal values of MCA/UA pulsatility index ratio.
Outcome variables were intrauterine and early neo natal death, admission to the neonatal intensive care unit and the duration of treatment, Apgar score below 7 at 5 minutes,cesarean delivery for fetal distress, gestational age at delivery, neonatal birth weight, IUGR.
Results: We divided the study population into two groups depending on normal or abnormal value of MCA/UA pulsatility index ratio. In 314 patients we found abnormal values of MCA/UA pulsatility index ratio. Neonates of mothers with abnormal values of MCA/UA pulsatility index ratio had significantly lower gestational age at delivery (34.8 versus 38.4, P<0.0001), lower birth weight (2174.6 g versus 3215.0g, P<0.001), significantly greater risk for perinatal death (30.8% versus 0.23%, P<0.0001) significantly greater risk of admission to intensive care unit (77.8% versus 47.4%, P<0.0001), longer duration of treatment in NICU (10.6 days versus 6.5 days, P<0.0001), greater rate of cesarean delivery for fetal distress (76.7% versus 62.5%,P<0.0001), a great number of neonates with low Apgar score at 5 minute (61.9% versus 22.4%, P<0.0001) greater rate of cesarean delivery for fetal distress (71.9% versus 62.5%,P<0.0001), a great number of fetuses IUGR (7.18% versus 1.76%,P<0.0001).
Conclusion: ACM/UA pulsatility index ratio is a very good predictor of adverse outcome in the fetuses of women with preeclampsia and gestational hypertension.
Key Words: Doppler, preeclampsia, gestational hypertension
Introduction
Preeclampsia affects 5-10% of pregnancies and is a major cause of maternal and fetal morbidity and mortality (1,2).
Although there is no proven effective method for the prevention of the preeclampsia, routine antenatal care has the aim to identify women who are at risk for more intensive antenatal care.
Abnormal placentacion is a main preeclampsia characteristic. Its cause is a maternal spiral veins trophoblastic invasion failure, which conditions vascular resistances raise and uterus-placental perfusion decrease.
For the first time Satomura demonstrated that the Doppler technique could evaluate blood flow (3). Nowadays, Doppler ultrasound velocimetry of uteroplacental umbilical and fetal vessels has become established method of antenatal monitoring, allowing the noninvasive assessment of fetal circulation (4). Its indices provide important information on the hemodynamics of the vascular area under study (5). Circulatory changes, reflected in certain fetal Doppler waveforms, predict adverse perinatal outcome (6).
Umbilical arteries are the common vessels assessed by Doppler ultrasound, but recent studies confirm the efficacy of middle cerebral artery (MCA) Doppler assessment and advocate it (7,8). MCA Doppler measurement is a well-known modality for detecting fetal compromise (9). Some studies has showed that MCA blood flow abnormalities were associated with hypoxia (1,8,10) and adverse perinatal outcome (11). Relationship between fetal Doppler findings and perinatal risks have been defined in numerous cross-sectional studies (12).
Several studies have reported higher sensitivities and spe cificities for middle cerebral artery/umbilical artery (MCA/UA) Doppler ratio compared with umbilical artery velocimetry alone for the prediction of the fetal prognosis (13-16).
MCA/UA ratio reflects not only the circulatory insufficiency of the umbilical velocimetry of the placenta manifested by alterations in the umbilical S/D ratio but also the adaptive changes resulting in modifications of the middle cerebral S/D ratio (13). In this study we evaluated the predicting value of the MCA/UA ratio, for fetal prognosis in women with gestational hypertension and preeclampsia.
Materials and methods
The study group consisted of 738 singleton pregnancies of women with preeclampsia and gestational hypertension who were recovered at the University Hospital of Obstetric and Gynecology of Tirana and delivered between January 2008-January 2009. The pregnancy outcome and clinical data of all women were collected from Hospital records following delivery.
The gestational age of all women was confirmed, either by menstrual dates or by first trimester ultrasonography.
Preeclampsia was diagnosed in those women who were normotensive during early pregnancy, but later demonstrated elevated blood pressure. All of them had a mild (systolic blood pressure > 140 mmHg, diastolic >90 mmHg and proteinuria 300 mg/24 h or = + 1 dipstick) or severe preeclampsia (systolic blood pressure > 160 mmHg, diastolic > 100 mmHg and severe proteinuria 2 g/24 h or +2 dipstick). The diagnosis of gestational hypertension was made in women whose blood pressure reached 140/ 90 mmHg or greater for the first time during pregnancy but in whom proteinuria was not developed (17.) Women with twin pregnancies, chromosomal abnormalities, gestational diabetes, were excluded from the study. Those included were followed by periodical Doppler flow measurements at least one time per week measurements until delivery.
The UA color Doppler waveforms were obtained from a free floating portion of the umbilical cord during minimal fetal activity and the absence of fetal breathing. All measurements were performed in the semi recumbent positions with the head and chest slightly elevated. For measurement of the MCA, an axial view of the fetal head was obtained at the level of cerebral peduncles, then the color Doppler was used to visualize the circle of Willis, and Doppler sample volume was placed within 1 cm of the origin of the MCA that was easily identified as a major branch running anterolateral from the circle of Willis toward to the lateral edge of the orbit.
The angle between the ultrasonographic beam and direction of blood flow was always <30 degrees. The Doppler signals were recorded with a 3.5 mHz curved array duplex transducer.
The UA pulsatility index were considered abnormal when the values were >2SD,the MCA pulsatility index was considered abnormal when the values were <5th percentile. MCA/UA PI<1 was considered abnormal (18). The reference values are according to Gramellini et al. (19).
Major adverse perinatal outcome were stillbirth and neonatal death. Minor adverse perinatal outcome were cesarean delivery for fetal distress, admission to the neonatal intensive care unit, Apgar score below 7 at 5 minutes, IUGR fetuses.
Statistical analysis included the χ2 test to compare proportions and the non paired Student t test to compare continuous variables. Also we used the test of sensitivity specificity, positive and negative predictive values and likelihood ratios. P values less than 0.05 were considered statistically significant.
Results
The 738 women underwent Doppler sonography until delivery. The results of the last Doppler sonography examination before delivery were collected for the statistical analyzes. The study population was divided into 2 groups based on the MCA/UA ratio. Group A, MCA/UA ratio>1 (n=424); group B MCA/UA ratio <=1 (n=314).
There were no significant differences in maternal age and gravidity. There is a statistical significant difference in gestational age at delivery between two groups, route of delivery and proteinuria between two groups (P<0.0001) (Table 1).
Table 1.
Maternal characteristics in correlation with normal or abnormal MCA/UA ratio.
| MCA/UA>1 (n=424) | MCA/UA<1 (n=314) | Statistical Tests values | P value | |
| Maternal age | 27.3+/-5.0 | 31.1+/-7.2 | ||
| Gestational age at delivery (week) | 38.4 | 34.8 | t-13.86 | <0.0001 |
| Gravidity | 2.5+/-3.2 | 3.6+/-2.1 | ||
| Proteinuria | 323 (76.1%) | 281 (89.4%) | +0.17 (χ2 ) | <0.0001 |
| Cesarean delivery | 265 (62.5%) | 241 (76.7%) | +0.15 (χ2) | <0.0001 |
| Vaginal delivery | 159 (37.5%) | 73 (23.2%) | -0.15(χ2) | <0.0001 |
The characteristics of the neonates are summarized in table 2 from the total of 738 delivery there were 481 (65.18 %) term babies. There were 54 (7.3%) stillbirths and 684 livebirths 44 (5.96%) neonates died within neonatal period. Of the 684 livebirths, 457 (66.81%) were admitted to the neonatal intensive care unit, 310 (45.32%) neonates have Apgar score less than 7 at 5 minute. There were 506 (73.97%) cesarean delivery for fetal distress. IUGR was diagnosed in 8.94% of cases.
Table 2.
Neonatal characteristics of the study population.
| Neonatal characteristics | No | % |
| Term babies | 481 | 65.18 |
| Stillbirth | 54 | 7.31 |
| Neonatal deaths | 44 | 5.96 |
| Perinatal deaths | 98 | 13.27 |
| Admission to NICU | 403 | 58.91 |
| Apgar at 5 min <7 | 256 | 37.42 |
| Cesarean delivery for fetal distress | 506 | 73.97 |
| IUGR | 66 | 8.94 |
As showed in table 3, a statistically significant difference in neonatal weight and gestational age at delivery was found between the two groups (P<0.0001). There was a significant increase in perinatal deaths in cases with abnormal MCA/UA PI ratio, 97 cases (30.8%) versus 1 case (0.23%) (P <0.0001). All the stillbirths were in the group of abnormal MCA/UA PI ratio. There is a statistically significant difference in neonatal deaths between two groups, 43 (13.6%) versus 1 (0.23%) (P<0.0001).
Table 3.
Minor and major adverse perinatal outcome in correlation with two groups of MCA/UA pulsatility index ratio.
| Normal MCA/UA (n=424) | Abnormal MCA/UA (n=314) | Statistical tests value | P - value | |
| Average birth weight (grams) | 3215.0 | 2174.6 | -18.8 (t) | <.0001 |
| Gestational age(weeks) | 38.4 | 34.8 | -13.86 (t) | <.0001 |
| Perinatal deaths | 1 (0.23%) | 97 (30.8%) | +0.45 (χ2) | <.0001 |
| Stillbirths | 0 (0%) | 54 (17.1%) | +0.33 (χ2) | <.0001 |
| Neonatal deaths | 1 (0.23%) | 43 (13.6%) | +0.32 (χ2) | <.0001 |
| Need for NICU | 201 (47.4%) | 202 (77.6%) | +0.3 (χ2) | <.0001 |
| Duration of treatment to NICU | 6.5 (days) | 10.6 (days) | -10.49 (t) | <.0001 |
| Apgar < 7 at 5 minute | 95 (22.4%) | 161 (61.9%) | +0.4 (χ2) | <.0001 |
| Cesarean delivery for fetal distress | 265 (62.5%) | 187 (71.9%) | +0.1 (χ2) | 0.01 |
| IUGR | 13 (1.76%) | 53 (7.18%) | +0.24 (χ2) | <.0001 |
Perinatal morbidity is increased significantly in the group with abnormal MCA/UA pulsatility index comparing to the group with normal MCA/UA pulsatility index ratio; 202 neonates (77.6%) versus 201 neonates (47.4%) were admitted to neonatal intensive care unit (NICU) (P<0,0001). There is a significant difference between the duration (in days) of treatment at neonatal intensive care unit (10.6 days versus 6.5 days) (P<0.0001).
It was found to be more neonates with Apgar scores less than 7 at 5 minute in the group with abnormal MCA/UA PI ratio than in group with normal MCA/ UA PI ratio 161 (61.9%) versus 95 (22.4%) (P<0.0001).
It was found a statistically difference between two groups for the elective cesarean delivery for fetal distress (P=0.01).
There are more IUGR cases in the group with MCA/UA <1 (7.18% versus 1.76%), there is a significant difference between two groups (P<0.0001).
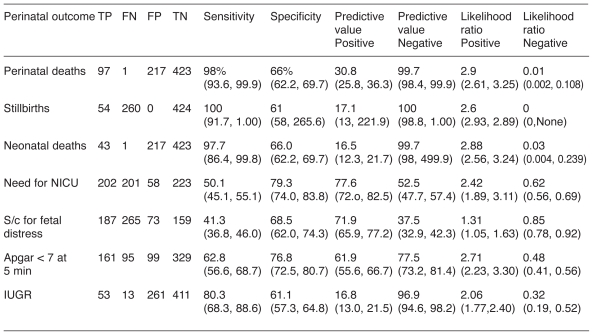
Table 4 show the sensitivity, specificity, positive predictive value, negative predictive value, and likelihood ratios positive and negative of MCA/UA PI ratio for major and minor adverse outcome. MCA/UA PI ratio <1 has the higher sensitivity (100%) for stillbirth, higher specificity and positive predicted value for admission to neonatal care unit (79.3% and 77.6%). The likelihood positive ratio for th MCA/UA PI ratio<1 was higher in perinatal deaths (2.9). Table 5 show a comparation of densitivity, specificity, positive predictive value negative predictive value of MCA/UA in our study and in those of Gramellini et al. (19).
Table 4.
Diagnostic performance of MCA/UA pulsatility index ratio for major and minor adverse outcome.
Table 5.
Comparation of our results of the sensitivity, specificity, positive predictive value, negative predictive value of MCA/UA ratio with those of the study of Gramellini et al.
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | |
| Gramellini D | 68.0% | 98.4% | 94.4% | 88.0% |
| Our study | 98% | 66% | 30.8% | 99.7% |
Discussion
Advances in Doppler ultrasonography have improved access to the fetal circulation. There has been a great deal of interest in the fetal intracranial vessels (20).
Knowledge of Doppler flow velocimetry of the fetal MCA may assist in perinatal diagnosis and management of complicated pregnancies. A low index of pulsatility in the middle cerebral artery associated with fetal compromise has been described (21-24). Because the MCA/UA ratio incorporates data not only on placental status but also on fetal response, it is potentially more advantageous in predicting perinatal outcome. Doppler data combining both umbilical and cerebral velocimetry provide additional information on fetal consequences of the placental abnormality (25).
Abnormal MCA/UA PI Doppler ratio is strongly correlated with worse fetal prognosis. In normal pregnancies the diastolic component in the cerebral arteries is lower than in the umbilical arteries at any gestational age. Therefore, the cerebro-vascular resistance remains higher than the placental resistance and the MCA/UA ratio is greater than 1. The index becomes less than 1 if the flow distribution is in favor of the brain in pathological pregnancies.
We observed reduction in placental perfusion and an increase in flow towards the brain. This phenomenon, called the brain sparing effect, is supposed to compensate for fetal hypoxia and is associated most of the time with fetal growth retardation with low umbilical artery pH. The cerebrovascular index decreases progressively, as in the normal fetuses so the hypoxia to be compensated by the brain hyperperfusion (26).
Fetuses with abnormal Doppler MCA/UA PI ratio in our study had a significantly lower birth weight, lower gestational age at delivery, l significantly higher incidence of perinatal deaths, higher incidence of admission to NICU and longer duration of treatment there, lower Apgar score at 5 minute (22).
Brar et al. (23) recognized that Doppler studies of the internal carotid artery or a ratio of cerebral to umbilical resistance could be used to identify pregnancies with a compromised post date fetus. The fetuses in our study with adverse outcome had a lower middle cerebral artery PI index, supporting the finding of Brar et al. (27).
According to Gramellini et al. and Arduini et al, assessment of MCA/UA PI index provide better information in predicting perinatal outcome when compared with umbilical or middle cerebral artery Doppler indices alone (19,28). In our study we found high sensitivity of the MCA/UA PI ratio in predicting stillbirth (100%). Also we found a high specificity and positive predicting value in need for treatment in neonatal intensive care unit.
Arduini and Rizzo (14) studied the test characteristics of the pulsatility index from UA, MCA and RA to predict adverse perinatal outcome in 120 SGA fetuses. In 46.7% (56 of 120) of fetuses there was at least one of the following adverse outcomes: perinatal deaths, caesarean delivery for fetal distress, asphyxia that necessitate admission to the neonatal intensive care unit for more than 48 hours. The author found that UA/MCA PI index ratio was the best test when compared with MCA, UA, and RA PI indices (sensitivity 89%, specificity 94%). Doppler velocimetry studies of placental and fetal circulation can provide important information regarding fetal well-being, yielding an opportunity to improve fetal outcome. Our results suggested that the MCA/UA PI Doppler ratio of less than 1 was a good predictive tool for neonatal outcome in preeclamptic and hypertensive pregnant women and could be used to identify fetuses at risk of morbidity and mortality.
The use of Doppler ultrasound in high risk pregnancies appears to improve a number of obstetric care outcomes and promising in reducing perinatal deaths (20).
References
- 1.Sibai B, Dekker G, Kupfermine M. Pre-eclampsia. Lancet. 2005;365:785–99. doi: 10.1016/S0140-6736(05)17987-2. [DOI] [PubMed] [Google Scholar]
- 2.Khan KS, Wojdyla D, Say L, et al. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–74. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 3.Satomura S. Ultrasonic Doppler method for the inspection of cardiac function. J Acoust Soc Am. 1957;29:1181–1185. [Google Scholar]
- 4.Dubiel M, Breborowicz GH, Marsal K, Gudmundsson S. Fetal adrenal and middle cerebral artery in high risk pregnancy. Ultrasound Obstet Gynecol. 2000;16:414–418. doi: 10.1046/j.1469-0705.2000.00278.x. [DOI] [PubMed] [Google Scholar]
- 5.Kurjak A, Kupesic S, Zudenigo D. Doppler ultrasound in all three trimesters of pregnancy. Curr Opin Obstet Gynecol. 1994;6:472–8. [PubMed] [Google Scholar]
- 6.Arduini D, Rizzo G. Doppler studies of deteriorating growth retarded fetuses. Curr Opin Obstet Gynecol. 1993;5:195–223. [PubMed] [Google Scholar]
- 7.Hernandez-Andrade E, S cheier M, Dzerega V, Carmo A, Nicolaides KH. Fetal middle cerebral artery peak systolic velocity in the investigation of non-imune hydrops. Ultrasound Obstet Gynecol. 2004;23:442–445. doi: 10.1002/uog.1009. [DOI] [PubMed] [Google Scholar]
- 8.Kassanos D, Siristatidis C, Vitoratos N, Salamalekis E, Creatsas G. The clinical significance of Doppler findings in fetal middle cerebral artery during labor. J Obstet Gynecol Reprod Biol. 2004;23:442–445. doi: 10.1016/s0301-2115(02)00512-2. [DOI] [PubMed] [Google Scholar]
- 9.Hershkovitz R, Kingdom JCP, Geary M, Rodeck CH. Fetal cerebral blood flow redistribution in late gestation: identification of compromise in small fetuses with normal umbilical artery Doppler. Ultrasound Obstet Gynecol. 2000;15:209–212. doi: 10.1046/j.1469-0705.2000.00079.x. [DOI] [PubMed] [Google Scholar]
- 10.Vyas S, Nicolaides KH, Bower S, Campbell S. Middle cerebral artery flow velocity waveforms in fetal hypoxaemia. Br J Obstet Gynaecol. 1990;97:797–803. doi: 10.1111/j.1471-0528.1990.tb02573.x. [DOI] [PubMed] [Google Scholar]
- 11.Strigini FA, De Luca G, Lencioni G, Scida P, Giusti G, Genazzani AR. Middle cerebral artery velocimetry: different clinical relevance depending on umbilical velocimetry. Obstet Gynecol. 1997;90:953–957. doi: 10.1016/s0029-7844(97)00482-1. [DOI] [PubMed] [Google Scholar]
- 12.Baschat AA. Doppler application in the delivery timing of the preterm growth-restricted fetus: another step in the right direction. Ultrasound Obstet Gynecol. 2004;23:111–118. doi: 10.1002/uog.989. [DOI] [PubMed] [Google Scholar]
- 13.Sterne G, Shields LE, Dubinsky TJ. Abnormal fetal cerebral and umbilical Doppler measurements in fetuses with intrauterine growth restriction predicts the severity of perinatal morbidity. J Clin Ultrasound. 2001;29:146–51. doi: 10.1002/1097-0096(200103/04)29:3<146::aid-jcu1014>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 14.Arduini D, Rizzo G, Romanini C. Changes of pulsatility index from fetal vessels preceding the onset of late decelerations in growth retarded fetuses. Obstet Gynecol. 1992;79:605–10. [PubMed] [Google Scholar]
- 15.Arias F. Accuracy of the middle-cerebral-to-umbilical- artery resistance index ratio in the prediction of neonatal outcome in patients at high risk for fetal and neonatal complications. Am J Obstet Gynecol. 1994;171:1541–5. doi: 10.1016/0002-9378(94)90398-0. [DOI] [PubMed] [Google Scholar]
- 16.Makhseed M, Jirous J, Ahmed MA, Viswanathan DL. Middle cerebral artery to umbilical artery resistance index ratio in the prediction of neonatal outcome. Int J Gynaecol Obstet. 2000;71:119–25. doi: 10.1016/s0020-7292(00)00262-9. [DOI] [PubMed] [Google Scholar]
- 17.Cunnigham FG, Gant NF, Leveno KJ, Gilstrap LC, Hauth JC, Wenstrom FD. Cunnigham FG, Gant NF, Leveno KJ, Gilstrap LC, Hauth JC, Wenstrom FD. Hypertensive disorders in pregnancy. In: Seils A, Noujaim SR, Devis K, editors. Williams obstetrics, 21st ed. USA: The Mc-Graw-Hill. 2001. pp. 568–9.
- 18.Williams KP, Wilson S. Maternal cerebral blood flow changes associated with eclampsia. Am J Perinatol. 1995;12:189–91. doi: 10.1055/s-2007-994449. [DOI] [PubMed] [Google Scholar]
- 19.Gramellini D, Folli MC, Raboni S, Vadora E, Merialdi A. Gramellini D, Folli MC, Raboni S, Vadora E, Merialdi A.. Cerebral umbilical Doppler ratio as a predictor of adverse perinatal outcome. Obstet Gynecol. 1992;79:416–420. doi: 10.1097/00006250-199203000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Neilson JP, Alfirevic Z. Doppler ultrasound for fetal assessment in high risk pregnancies. Cochrane Database Syst Rev. 2000 doi: 10.1002/14651858.CD000073. [DOI] [PubMed] [Google Scholar]
- 21.Madazli R, Uludag S, Ocak V. Doppler assessment of umbilical artery, thoracic aorta and middle cerebral artery in the management of pregnancies with growth restriction. Acta Obstet Gynecol Scand. 2001;80:702–7. doi: 10.1034/j.1600-0412.2001.080008702.x. [DOI] [PubMed] [Google Scholar]
- 22.Severi FM, Bocchi C, Visentin A, Falco P, Cobellis L, Florio P, et al. Uterine and fetal cerebral Doppler predict the outcome of third trimester small-for-gestational age fetuses with normal umbilical artery Doppler. Ultrasound Obstet Gynecol. 2002;19:225–8. doi: 10.1046/j.1469-0705.2002.00652.x. [DOI] [PubMed] [Google Scholar]
- 23.Dubiel M, Gudmundsson S, Gunnarsson G, Marsal K. Middle cerebral artery velocimetry as a predictor of hypoxemia in fetuses with increased resistance to blood flow in the umbilical artery. Early Hum Dev. 1997;47:177–84. doi: 10.1016/s0378-3782(96)01777-x. [DOI] [PubMed] [Google Scholar]
- 24.Seyam YS, Al-Mahmeid MS, Al-Tamimi HK. Umbilical artery Doppler flow velocimetry in intrauterine growth restriction and its relation to perinatal outcome. Int J Gynaecol Obstet. 2002;77:131–7. doi: 10.1016/s0020-7292(02)00027-9. [DOI] [PubMed] [Google Scholar]
- 25.Bahado-Singh RO, Kovanci E, Jeffres A, Oz U, Deren O, Copel J, et al. The Doppler cerebroplacental ratio and perinatal outcome in intrauterine growth restriction. Am J Obstet Gynecol. 1999;180:750–6. doi: 10.1016/s0002-9378(99)70283-8. [DOI] [PubMed] [Google Scholar]
- 26.Rizzo G, Arduini D, Luciano R, Rizzo C, Tortorolo G, Romanini C, et al. Prenatal cerebral Doppler ultrasonography and neonatal neurologic outcome. J Ultrasound Med. 1989;8:237–40. doi: 10.7863/jum.1989.8.5.237. [DOI] [PubMed] [Google Scholar]
- 27.Brar HS, Horenstein J, Medearis AL, Platt LD, Phelan JP, Paul RH. Cerebral, umbilical and uterine resistance using Doppler velocimetry in postterm pregnancy. J Ultrasound Med. 1989;8:187–91. doi: 10.7863/jum.1989.8.4.187. [DOI] [PubMed] [Google Scholar]
- 28.Arduini D, Rizzo G. Prediction of fetal outcome in small for gestational age fetuses:comparison of Doppler measurements obtained from different fetal vessels. J Perinat Med. 1992;20:29–38. doi: 10.1515/jpme.1992.20.1.29. [DOI] [PubMed] [Google Scholar]