Abstract
The impact of increased serum concentrations of plant sterols on cardiovascular risk is unclear. We conducted a systematic review and meta-analysis aimed to investigate whether there is an association between serum concentrations of two common plant sterols (sitosterol, campesterol) and cardiovascular disease (CVD). We systematically searched the databases MEDLINE, EMBASE, and COCHRANE for studies published between January 1950 and April 2010 that reported either risk ratios (RR) of CVD in relation to serum sterol concentrations (either absolute or expressed as ratios relative to total cholesterol) or serum sterol concentrations in CVD cases and controls separately. We conducted two meta-analyses, one based on RR of CVD contrasting the upper vs. the lower third of the sterol distribution, and another based on standardized mean differences between CVD cases and controls. Summary estimates were derived by fixed and random effects meta-analysis techniques. We identified 17 studies using different designs (four case–control, five nested case–control, three cohort, five cross-sectional) involving 11 182 participants. Eight studies reported RR of CVD and 15 studies reported serum concentrations in CVD cases and controls. Funnel plots showed evidence for publication bias indicating small unpublished studies with non-significant findings. Neither of our meta-analyses suggested any relationship between serum concentrations of sitosterol and campesterol (both absolute concentrations and ratios to cholesterol) and risk of CVD. Our systematic review and meta-analysis did not reveal any evidence of an association between serum concentrations of plant sterols and risk of CVD.
Keywords: Plant sterols, Phytosterols, LDL-C, Cardiovascular disease, Coronary heart disease
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide.1 Elevated LDL-cholesterol (LDL-C) concentrations constitute a major cardiovascular risk factor.2 There is substantial evidence that the incidence of CVD can be reduced by lowering LDL-C, either through diet or through the use of lipid-lowering agents, primarily statins.3–6 In this regard, it is relevant that ingestion of supplements of plant sterols (also called phytosterols) has been known to effectively lower serum concentrations of cholesterol and LDL-C since the early 1950's.7–9 Phytosterols are cholesterol homologues principally found in nuts, fruits, and seeds, and are present in the diet in quantities similar to cholesterol (200–400 mg per day).10,11 In contrast to cholesterol, phytosterols are poorly absorbed, resulting in circulating concentrations of <1 mg/dL.12 Their lipid-lowering effect is mediated by competitive inhibition of cholesterol absorption and by transcriptional induction of genes implicated in cholesterol metabolism in both enterocytes and hepatocytes.13
The cholesterol-lowering properties of phytosterols have therefore also been exploited in the preparation of functional foods.14 However, despite the potential positive impact on cardiovascular risk due to cholesterol lowering, concerns have been raised that plant sterols may also exert adverse cardiovascular effects, for two major reasons15,16 First, individuals with sitosterolaemia, a rare autosomal recessive inherited disorder, in which serum phytosterol concentrations are elevated 50–100-fold, may display premature and severe CVD.17,18 This disease was first described by Bhattacharyya and Connor19 and is caused by mutations in the intestinal and hepatic ATP-binding cassette transporters G5 and G8 (ABCG5/ABCG8).20,21 In subjects with sitosterolaemia, cholesterol and LDL-C concentrations may be normal, but also moderately increased.17,18 Secondly, some but not all population-based studies have reported associations between elevated serum concentrations of plant sterols and CVD.22–24
We conducted a systematic review and meta-analysis of epidemiological studies to investigate whether there is an association between serum concentrations of plant sterols and CVD. We focused on two common plant sterols, sitosterol and campesterol, which together constitute >90% of the sterols occurring in diet and circulating blood.11
Methods
Data sources, search strategy, and selection criteria
We conducted a systematic review of the published literature according to the PRISMA statement for the conduct of meta-analyses of epidemiological studies.25 Relevant studies were identified by searching in the following data sources: MEDLINE via PUBMED (from 1950 to April 2010), EMBASE (from 1996 to April 2010), and the COCHRANE library (from 1988 to April 2010). Search terms including key words and headings were related to plant sterol exposure (‘phytosterol’, ‘plant sterol’, ‘sitosterol’, or ‘campesterol’) and to CVD (‘atherosclerosis’, ‘coronary heart disease’, ‘coronary artery disease’, ‘angiography’, ‘cardiovascular disease’, ‘cardiovascular mortality’, ‘cardiovascular risk’, ‘cardiovascular event’, ‘stenosis’, ‘atherosclerotic plaque’, ‘coronary calcium’, ‘vascular’, ‘stroke’, ‘myocardial infarction’, ‘peripheral arterial disease’, or ‘cerebrovascular disease’). Two authors (B.G. and K.C.D.) conducted independently the literature search, data extraction, and quality assessment by using a standardized approach. We included studies with different research designs that reported data on the association between serum concentrations of campesterol/ sitosterol and CVD. Details of eligibility criteria are shown in Table 1. As few studies were eligible and as authors employed heterogeneous endpoints related to CVD, we defined a composite of major clinical cardiovascular events as the primary endpoint for our meta-analysis. The endpoint includes different definitions of CVD (shown in Table 1).
Table 1.
Eligibility criteria
| Inclusion criteria |
| Study design: cohort study, parallel- or cross-over trial, cross-sectional study, case–control study, nested case–control study |
| Provided data on one of the following definitions of CVD: |
| Non-fatal coronary heart disease: non-fatal myocardial infarction, coronary artery calcium determined by electron beam computer tomography, and carotid stenosis ≥50% verified by Doppler ultrasound |
| Non-fatal cerebrovascular events: non-fatal stroke, transient ischaemic attack, prolonged reversible ischaemic neurological deficit |
| Death due to CVD: death due to coronary heart disease, cerebrovascular disease, or peripheral vascular disease |
| Reported on exposure: serum concentrations of sitosterol/campesterol (absolute values or ratios to total cholesterol) |
| Reported association measures (hazard ratio, odds ratios, or incidence rate ratios) between exposure and CVD or descriptive statistics of exposure serum concentrations in CVD cases and controls separately |
| Publication in English, French, German, Spanish, Portuguese |
| Exclusion criteria |
| No original paper published in any periodical indexed in one of our search databases |
| Used a history based definition of CVD such as personal and/or family history of CVD |
| Used endpoints which were not unequivocally related to CVD such as aortic valve stenosis, composition of the atheromatous plaque, or carotid artery compliance |
Data extraction
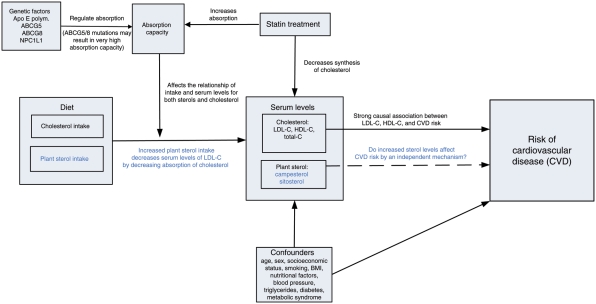
For each study identified, we obtained the original publications and extracted the following data into a spreadsheet: author, year of publication, country of origin, research design, major characteristics of the study population, descriptive statistics of the sterol serum concentrations (if provided for CVD cases and controls separately), or risk ratios (RR) with respect to CVD according to serum plant sterol concentrations (i.e. odds ratios, incidence rate ratios, or hazard ratios), the statistical method used for analysis, and the covariates adjusted in multivariate modelling. We applied standardization procedures to synthesize data from studies that used different units of measurements for sterol concentrations or used different cut-off concentrations for the calculation of RR (including comparisons of thirds, quarters, fifths, etc., or continuous increases in risk for a given absolute increase in exposure level). We transformed absolute sterol concentrations into mg/dl and ratios to total cholesterol into µg/mg. For studies that reported RR, we transformed the RR to compare individuals in the top third vs. those in the bottom third of the sterol distribution. Statistical details of the standardization approach for RR have been published elsewhere.26 If authors reported several estimates of RR derived from multiple models using different sets of adjusting variables, we considered the estimate adjusted for all potential confounding variables (that have been collected in the particular study) as the gold standard estimate. We assessed the set of potential confounding variables by a pre-defined conceptual model (Figure 1). The model presumes that phytosterol serum concentrations act at the same causal level as cholesterol concentrations, both being strongly affected by individual intake and absorption capacity. Thus, consistent risk estimates for sterols should be adjusted for cholesterol concentrations (especially LDL-C) to avoid any bias due to a common mechanism that might affect intestinal absorption of both cholesterol and non-cholesterol sterols, such as genetic factors.27
Figure 1.
Conceptual model: plant sterols and cardiovascular disease.
For studies that reported phytosterols in CVD cases and controls separately, we calculated standardized mean differences (SMD) and standard errors. Equally, we conducted separate analyses to explore the relationships of absolute phytosterol concentrations and their ratios to cholesterol with the incidence of CVD.
Statistical analysis
We examined potential publication bias using Begg's Funnel plots and Egger's test. We conducted two different meta-analyses, one based on the RR (MA 1) and another based on the SMD between CVD cases and controls (MA 2). For both analyses, we calculated pooled summary estimates by using fixed effects (the Mantel–Haenszel method)28 and random effects (the DerSimonian and Laird model)29 meta-analysis techniques. As we assumed unexplained heterogeneity among studies due to heterogeneous study designs and to different strategies for adjustment of confounding variables, we considered the random effects estimate as the preferable approach. To further explore heterogeneity among studies, we calculated I² statistics and used Forest plots visualizing study-specific estimates and the pooled fixed and random effects estimators. In addition to the core analysis using the ‘best adjusted estimate’ (i.e. the estimate adjusted for all available potential confounding variables), we conducted sensitivity analyses by including and excluding studies and/or estimates with non-appropriate adjustment. Further, if sufficient studies were available, as it was the case for MA 2, we additionally conducted subgroup analyses by study design (results are shown in the Forest plots). Statistical hypothesis testing was conducted two sided with a P-value of 0.05 to be considered significant. All statistical analyses were conducted using the statistical software package STATA (STATA Corporation, College Station, TX, USA).
Role of the funding source
The funding source had no role in data analysis, data interpretation, or in the writing of the manuscript. The first author (B.G.) had full access to all data used in the study. All authors had responsibility for the decision to submit the article for publication.
Results
Literature search and selected studies
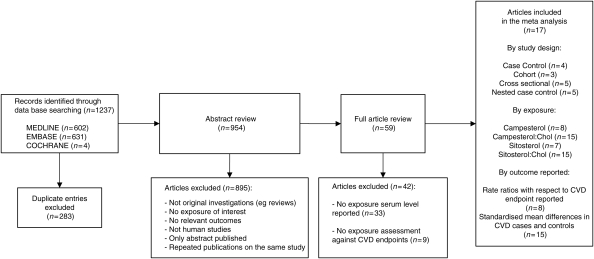
The literature search yielded 954 abstracts from three different databases, of which 59 publications were selected to be reviewed in full text (Figure 2). Of these, we excluded 33 studies as phytosterol concentrations were not explicitly reported; a further nine studies were equally excluded as study endpoints or definitions of CVD did not meet our inclusion criteria. We excluded studies that used ‘family history of CVD (or CHD)’ as the study endpoint,30–32 together with studies that employed endpoints which were not unequivocally related to CVD such as aortic valve stenosis,33 composition of the atheromatous plaque,34,35 and carotid artery compliance.36 Furthermore, we excluded a study that did not report any association measures that we could extract for the proposed data synthesis (i.e. RR or SMD), such as correlation coefficients between PS concentrations with a severity score of coronary artery disease,37 and a study that was published in abstract form only.38
Figure 2.
Identification process for eligible studies.
Finally, we selected 17 studies (4 case–control, 3 cohort, 5 cross-sectional and 5 nested case–control studies) for the present meta-analysis, including a total of 11 182 participants22–24,39–52 (Supplementary material online, Table A1). Eight studies reported relative risks based on phytosterol exposure in relation to CVD endpoints; 15 studies reported summary statistics of phytosterol concentrations in CVD cases and controls separately. Published studies involved sample sizes that ranged from 40 to 2440 participants with the mean age ranging from 48 to 78 years. Funnel plots (data not shown) indicated the presence of publication bias with a lack of publication of small studies with non-significant findings. Moreover, we found that publication bias was higher in studies which provided mean differences in phytosterol concentrations between CVD cases and controls (MA 2), when compared with those which analysed RR for CVD outcomes (MA 1).
Meta-analysis
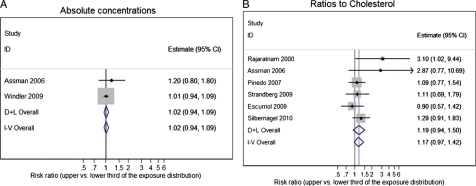
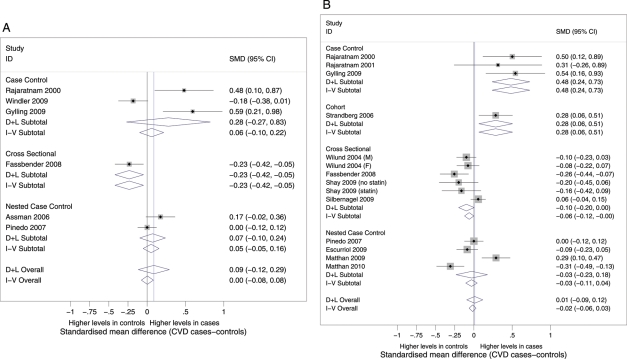
Table 2 shows a summary of the two meta-analyses (MA 1: based on RR, and MA 2: based on SMD) conducted for the two phytosterols for both absolute values and ratios to cholesterol. Figures 3–6 show Forest plots visualizing the study-specific estimates and the pooled summary estimates (both fixed and random effects).
Table 2.
Summary of the random effects meta-analysis
| Exposure | n | RRa | 95% CI | P-valueb | n | SMDc | 95% CI | P-valueb |
|---|---|---|---|---|---|---|---|---|
| Campesterol | ||||||||
| Absolute | 2 | 1.02 | 0.94–1.09 | 0.675 | 7 | 0.09 | −0.10–0.28 | 0.368 |
| Ratio to Chol | 6 | 1.19 | 0.94–1.50 | 0.150 | 15 | 0.02 | −0.10–0.14 | 0.770 |
| Sitosterol | ||||||||
| Absolute | 3 | 1.06 | 0.84–1.34 | 0.644 | 6 | 0.09 | −0.12–0.29 | 0.400 |
| Ratio to Chol | 8 | 0.94 | 0.68–1.31 | 0.730 | 14 | 0.01 | −0.09–0.12 | 0.837 |
aRandom effects estimates of the risk ratio comparing the upper vs. the lower third of the distribution with the endpoint ‘all CVD events pooled’ (MA 1).
bSignificance level of testing the hypothesis of absence of effect (i.e. RR = 1 and SMD = 0, respectively).
cStandardized mean difference between CVD cases and controls (MA 2).
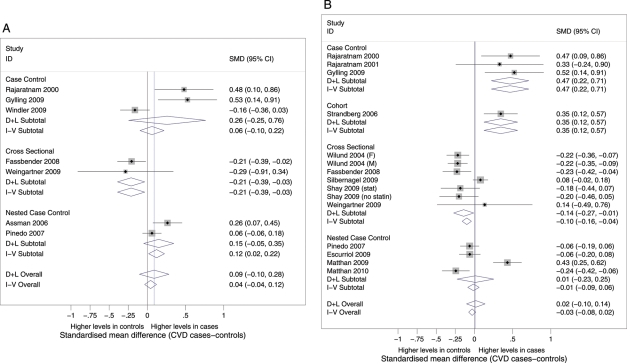
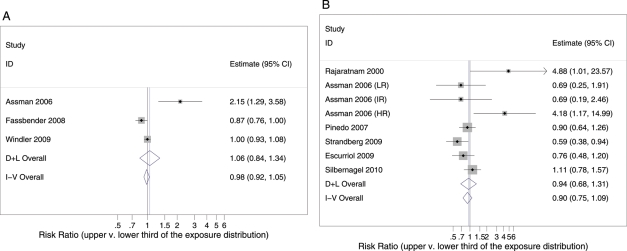
Figure 3.
Serum levels of campesterol and risk of cardiovascular disease (A: absolute concentrations, B: ratios to total cholesterol). D + L: DerSimonian & Laird random effects estimate; I-V: inverse variance fixed effects estimate; diamonds: point estimate and 95% confidence interval; boxes: size proportional to study weight for random effects approach; black line: reference line indicating the absence of effect; blue line: point estimate of random effects approach.
Figure 6.
Serum levels of sitosterol in CVD cases and controls (A: absolute concentrations, B: ratios to total cholesterol). D + L: DerSimonian & Laird random effects estimate; I-V: inverse variance fixed effects estimate; diamonds: point estimate and 95% confidence interval; boxes: size proportional to study weight for random effects approach; black line: reference line indicating absence of effect; blue line: point estimate of random effects approach.
For campesterol, the meta-analysis based on RR (Figure 3) showed homogenous estimates among studies and a non-significant pooled summary estimate for both absolute concentrations (Figure 3A: RR = 1.02, P = 0.675) and ratios to total cholesterol (Figure 3B: RR = 1.19, P = 0.150). The meta-analysis using SMDs between CVD cases and controls (Figure 4A) revealed heterogeneous estimates among studies (I² = 79%, P < 0.001), including three studies22,23,41 with positive associations. Subgroup analysis by study design partly explained these inconsistent results. Case–control studies and nested case–control studies appeared to show a tendency towards increased campesterol concentrations in CVD cases compared with controls. However, the pooled meta-analysis estimate was non-significant (SMD = 0.09, P = 0.400). The plot for campesterol to cholesterol ratios (Figure 4B) also revealed a heterogeneous pattern of estimates (I² = 83%, P < 0.001). We observed studies with either positive or negative associations that scattered around the pooled summary estimate, which itself was close to zero and non-significant (SMD = 0.02, P = 0.770). Again, subgroup analysis could only, to some extent, explain the observed heterogeneity.
Figure 4.
Serum levels of campesterol in CVD cases and controls (A: absolute concentrations, B: ratios to total cholesterol). D + L: DerSimonian & Laird random effects estimate; I-V: inverse variance fixed effects estimate; diamonds: point estimate and 95% confidence interval; boxes: size proportional to study weight for random effects approach; black line: reference line indicating absence of effect; blue line: point estimate of random effects approach.
In the case of sitosterol, only three studies reported RR (Figure 5A) with respect to CVD based on absolute serum phytosterol concentrations. The results of these studies were heterogeneous (I² = 84%, P = 0.002), including one study which reported a significant relationship.22 The summary estimate was non-significant (RR = 1.06, P = 0.644), indicating the absence of an effect. The plot for sitosterol to cholesterol ratios (Figure 5B) also demonstrated a heterogeneous pattern (I² = 55%, P = 0.030). Most studies showed non-significant results, the one by Assmann et al.22 being the only estimate which indicated a positive association. Again, the pooled estimate was not significant (RR = 0.94, P = 0.730).
Figure 5.
Serum levels of sitosterol and risk of cardiovascular disease (A: absolute concentrations, B: ratios to total cholesterol). D + L: DerSimonian & Laird random effects estimate; I-V: inverse variance fixed effects estimate; diamonds: point estimate and 95% confidence interval; boxes: size proportional to study weight for random effects approach; black line: reference line indicating absence of effect; blue line: point estimate of random effects approach.
Similarly, the meta-analysis of SMDs of sitosterol in CVD cases and controls (Figure 6A) showed substantial heterogeneity (I² = 82%, P < 0.001) and a non-significant summary estimate (SMD = 0.09, P = 0.400). We identified studies which reported either positive or negative associations of phytosterol exposure with CVD. Stratified analysis revealed that only part of this heterogeneity could be explained by study design. The plot of the SMDs for sitosterol to cholesterol ratios (Figure 6B) also showed substantial heterogeneity (I² = 78%, P < 0.001) and a non-significant pooled estimate (SMD = 0.01, P = 0.837). Again, stratified analysis by study design was able to explain some of this heterogeneity and indicated a tendency towards positive associations between phytosterol exposure and CVD in case-control studies. Of note, sensitivity analyses conducted for the meta-analysis based on the RR (MA 1) failed to reveal any major impact of excluding data from studies with non-appropriate adjustment for covariates.
Discussion
This systematic review and meta-analysis based on the findings from 17 studies involving 11 182 subjects did not yield any evidence of an association between serum concentrations of plant sterols and elevated risk of CVD. This is true for both campesterol and sitosterol, for absolute concentrations and their ratios to total cholesterol, and regardless of whether we considered RR for CVD based on tertiles of plant sterol concentrations or mean concentrations in CVD cases compared with controls.
Interestingly, the studies identified by our systematic literature review reported highly inconsistent findings. Some studies suggested that elevated circulating concentrations of plant sterol concentrations (or their ratios to cholesterol) might increase the risk of CVD, namely the PROspective CArdiovascular Münster study,22 the Framingham Offspring Study,24 the Drugs and Evidence BAsed medicine in The Elderly study,49 a cohort of subjects with aortic stenosis,50 the Pittsburgh Epidemiology of Diabetes Complications Study,45 and two Finish studies in postmenopausal women.23,41 A similar modest trend was also seen in participants of the LUdwigshafen RIsk and Cardiovascular health study in multivariate analysis adjusted for potential confounding variables.46,47 In contrast, other studies reported negative associations of plant sterols with cardiovascular risk, namely the Longitudinal Aging Study Amsterdam,39 the European Prospective Investigation of Cancer Norfolk and Spain cohorts,39,43 and the COronary Risk factors for Atherosclerosis in women study.52 Finally, three studies indicated that plant sterol concentrations are not at all related to CVD, i.e. the Dallas Heart Study,51 the PROspective Study of Pravastatin in the Elderly at Risk trial,42 and the Helsinki Businessmen Study.48
A likely explanation for the inconsistent findings is that authors used different study designs and adjustments for potential confounding variables. Bias is likely if investigators did not appropriately adjust for all potential confounding variables. Most importantly, we have to consider bias due to confounding by lipoprotein concentrations (i.e. LDL-C concentrations, an established important risk factor for CVD). According to our conceptual model, there are common factors affecting intestinal absorption of both cholesterol and plant sterols creating a correlation between sterol and lipoprotein concentrations (Figure 1).53 Indeed, cholesterol uptake in the gut resulting in increased total and LDL cholesterol serum concentrations has per se been suggested to represent an independent cardiovascular risk factor and might therefore account for a potential association of elevated plant sterol concentrations in serum with CVD.46,47,54 Furthermore, absorption in the gut is strongly influenced not only by genetic factors,27 but also by age, gender, diet, metabolic background, and medication (Figure 1).46,47,55–63 For example, the metabolic syndrome, insulin resistance, and type 2 diabetes are associated with low-circulating cholesterol absorption.55,58 In contrast, poor nutritional status, an index of frailty in elderly people, is correlated with high plant sterol concentrations. The associations of the metabolic syndrome/type 2 diabetes64,65 and frailty66 with increased cardiovascular risk may thus feign both the inverse and positive relationships of plant sterols with CVD, respectively. Further, confounding due to nutritional factors may occur. Elevated serum plant sterol concentrations reflect enrichment of plant-based food in the diet.12,39 Diets rich in fruits, seeds, vegetable protein, and polyunsaturated fatty acids, such as the Mediterranean diet, are considered healthy, may reduce cardiovascular risk, and thereby underlie the association of subnormal plant sterol concentrations with CVD.
In the meta-analysis based on the RR, we tried to minimize potential bias due to uncontrolled confounders by selecting the best-adjusted estimate according to our conceptual model. Interestingly, there was still substantial heterogeneity among studies; an explanation might be that authors used different statistical approaches and adjusted for different potential confounding variables. Of note, in our meta-analysis of mean differences of sterol concentrations between CVD cases and controls, heterogeneity among studies was even higher. This finding is not surprising since most investigators presented only crude-unadjusted statistics of the exposure distributions, so that our calculated mean differences do not provide unbiased estimates of the effect of sterols on CVD. For example, if there are any CVD risk factors with correlations to sterols (which is likely, e.g. lipoproteins) altered sterol concentrations in CVD cases might only be a proxy for other CVD risk factors.
Plant sterols have been ascribed atherogenic effects, mainly because atherosclerosis has been encountered in patients with phytosterolaemia which is accompanied by extremely high concentrations of plant sterols. Equally, however, serum phytosterol concentrations have been demonstrated to correlate with atherosclerotic plaque burden in individuals not affected by this disease.34,35 Our meta-analysis, however, argues against an association between moderately elevated concentrations of plant sterols and CVD.
In the studies recruited for this meta-analysis, plant sterol concentrations vary at least by threefold, as indicated by a comparison of the midpoints of the lower and upper tertiles of sitosterol and campesterol distributions (Table 3). This range should be wide enough to detect relevant changes of cardiovascular risk due to moderate and commonly occurring variations in phytosterol levels.
Table 3.
Average serum concentrations of plant sterols in the first and third tertiles of their distributions in the studies included in the meta-analysis
| Midpointa (first tertile) | Midpointa (third tertile) | Factorb (third /first tertile) | |
|---|---|---|---|
| Sitosterol (mg/dL) | 0.13 | 0.38 | 3.1 |
| Sitosterol:Chol | 0.44 | 1.69 | 3.6 |
| Campesterol (mg/dL) | 0.17 | 0.57 | 3.7 |
| Campesterol:Chol | 0.94 | 2.49 | 3.4 |
aAverage midpoint of tertiles across studies.
bAverage ratio (midpoint of third tertile/ midpoint of first tertile) across studies.
There is evidence that the tissue content of plant sterols relates to their concentration in the plasma.67 Tissue levels were higher in individuals consuming sterol-enriched foods than in individuals who did not. Tissue deposition of plant sterols is most likely a passive process driven by the respective plasma concentration. A similar correlation may also exist between plasma and tissue cholesterol, but this was unfortunately not examined in that study. A mere correlation between minute amounts of plant sterols in the plasma and in tissue would, in addition, not prove a specific causal role of plant sterols in atherosclerosis, at least as long as it has not been shown that plant sterols would biologically be much more active than cholesterol on a equimolar basis.
Our systematic review and meta-analysis have several limitations. First, it was based only on few observational studies and is therefore prone to bias due to uncontrolled confounding. In particular, our inability to properly adjust for all potential confounders might confound the association estimates. We have implemented an analytical strategy to minimize this potential bias due to uncontrolled confounding. First, we defined a conceptual model specifying the set of potential confounding variables. Secondly, we extracted from each study the best-adjusted estimates according to this model. Unfortunately, not all authors provided fully adjusted estimates so that we must assume some residual bias. Thus, we also considered the possibility of a sensitivity analysis, i.e. repeating the analysis by excluding all studies without appropriate adjustment for potential confounding variables. However, the number of studies was too small to effectively implement this approach. Further, the second meta-analysis based on SMD between CVD cases and controls (MA 2) is likely to be biased since most studies only provided crude-unadjusted statistics of the sterol distributions. An analysis based on multivariate predicted means of sterol concentrations adjusted for potential confounding variables, such as provided in the LUdwigshafen RIsk and Cardiovascular Health study,44 would be a preferable analytical approach to obtain further evidence for any causal relationship between sterol serum concentrations and CVD. Secondly, since only a few studies were eligible, we pooled results from studies involving different designs and dissimilar definitions of CVD.
Thus, as a direct consequence, it was necessary to define a composite cardiovascular endpoint, including not only coronary but also cerebrovascular and peripheral vascular events which might increase noise and reduce the power of our meta-analysis. Finally, we also had to consider publication bias as indicated by a lack of small studies published resulting in a slight overestimation of the true effect of plant sterols on CVD risk.
Even though our meta-analysis has several limitations, it represents the first systematic attempt to critically appraise the evidence surrounding the relationship of plant sterols and their ratios to cholesterol with CVD. We are convinced that even by pooling heterogeneous studies, one can substantially contribute to new insights if the basic assumption holds that there was no systematic methodological bias present. Study heterogeneity might increase noise and reduce power, but, if none of the investigators tried to force/mask the true effect by systematically selecting a particular research design, statistical approach, and/or strategy to adjust for potential confounding variables, then a meta-analysis should be able to obtain consistent summary estimates. However, based on the present meta-analysis of observational studies, evidence is still limited and further research will be necessary to assess whether plant sterols are causally involved in atherogenesis. The next level of evidence might be the conduct of an individual patient data meta-analysis retrieving the original data of the studies considered here. A centralized reanalysis of the data in each study in a consistent way would afford a decrease in heterogeneity and bias in summary estimates by enhancing correction for potential confounding variables.
In conclusion, our systematic review and meta-analysis do not provide any evidence that there is an association between moderate fluctuations of serum concentrations of plant sterols and CVD risk. However, our meta-analysis does not address the vascular effects or safety of long-term consumption of plant sterol-enriched foods.
Contributors
B.G., G.S., and W.M. planned the study and wrote the manuscript. B.G. and K.C.D. performed the literature search and extracted data. B.G. conducted the statistical analysis. Other authors contributed to interpretation of the data and writing of the manuscript.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
Funding to pay the Open Access publication charges for this article was provided by an Educational Grant from Danone Research, Palaiseau, France.
Conflict of interest: B.G. received an unrestricted Educational Grant from Danone Research, Palaiseau, France. Other authors declared no conflict of interest.
Supplementary Material
References
- 1.World Health Organisation. The Global Burden of Disease: 2004 Update. Geneva: World Health Organisation; 2008. [Google Scholar]
- 2.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 3.Sacks FM, Pasternak RC, Gibson CM, Rosner B, Stone PH. Effect on coronary atherosclerosis of decrease in plasma cholesterol concentrations in normocholesterolaemic patients. Harvard Atherosclerosis Reversibility Project (HARP) Group. Lancet. 1994;344:1182–1186. doi: 10.1016/s0140-6736(94)90506-1. doi:10.1016/S0140-6736(94)90506-1. [DOI] [PubMed] [Google Scholar]
- 4.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 5.Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–1307. doi: 10.1056/NEJM199511163332001. doi:10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 6.Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC, Davis BR, Braunwald E. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996;335:1001–1009. doi: 10.1056/NEJM199610033351401. doi:10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 7.Farquhar JW, Sokolow M. Response of serum lipids and lipoproteins o man to beta-sitosterol and safflower oil; a longterm study. Circulation. 1958;17:890–899. doi: 10.1161/01.cir.17.5.890. [DOI] [PubMed] [Google Scholar]
- 8.Bronte-Stewart B, Antonis A, Eales L, Brock JF. Effects of feeding different fats on serum-cholesterol level. Lancet. 1956;270:521–526. doi: 10.1016/s0140-6736(56)90592-x. doi:10.1016/S0140-6736(56)90592-X. [DOI] [PubMed] [Google Scholar]
- 9.Ahrens EH, Jr, Insull W, Jr, Blomstrand R, Hirsch J, Tsaltas TT, Peterson ML. The influence of dietary fats on serum-lipid levels in man. Lancet. 1957;272:943–953. doi: 10.1016/s0140-6736(57)91280-1. doi:10.1016/S0140-6736(57)91280-1. [DOI] [PubMed] [Google Scholar]
- 10.Ostlund RE., Jr Phytosterols in human nutrition. Annu Rev Nutr. 2002;22:533–549. doi: 10.1146/annurev.nutr.22.020702.075220. doi:10.1146/annurev.nutr.22.020702.075220. [DOI] [PubMed] [Google Scholar]
- 11.Silbernagel G, März W. Plant sterols: cardiovascular risk factors. J Lab Med. 2008;32:209–218. [Google Scholar]
- 12.Chan YM, Varady KA, Lin Y, Trautwein E, Mensink RP, Plat J, Jones PA. Plasma concentrations of plant sterols: physiology and relationship with coronary heart disease. Nutr Rev. 2006;64:385–402. doi: 10.1111/j.1753-4887.2006.tb00224.x. doi:10.1111/j.1753-4887.2006.tb00224.x. [DOI] [PubMed] [Google Scholar]
- 13.Calpe-Berdiel L, Escola-Gil JC, Blanco-Vaca F. New insights into the molecular actions of plant sterols and stanols in cholesterol metabolism. Atherosclerosis. 2009;203:18–31. doi: 10.1016/j.atherosclerosis.2008.06.026. doi:10.1016/j.atherosclerosis.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 14.Brendsel J, Green SJ. Regarding the potential perils of phytosterols. Atherosclerosis. 2007;192:227–229. doi: 10.1016/j.atherosclerosis.2006.08.019. author reply 30 doi:10.1016/j.atherosclerosis.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 15.Weingärtner O, Böhm M, Laufs U. Controversial role of plant sterol esters in the management of hypercholesterolaemia. Eur Heart J. 2009;30:404–409. doi: 10.1093/eurheartj/ehn580. doi:10.1093/eurheartj/ehn580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schonfeld G. Plant sterols in atherosclerosis prevention. Am J Clin Nutr. 2010;92:3–4. doi: 10.3945/ajcn.2010.29828. doi:10.3945/ajcn.2010.29828. [DOI] [PubMed] [Google Scholar]
- 17.Salen G, Horak I, Rothkopf M, Cohen JL, Speck J, Tint GS, Shore V, Dayal B, Chen T, Shefer S. Lethal atherosclerosis associated with abnormal plasma and tissue sterol composition in sitosterolemia with xanthomatosis. J Lipid Res. 1985;26:1126–1133. [PubMed] [Google Scholar]
- 18.Payne MY. Too young to be having a heart attack. Lancet. 2001;358(uppl)):S64. doi: 10.1016/S0140-6736(01)07076-3. doi:10.1016/S0140-6736(01)07076-3. [DOI] [PubMed] [Google Scholar]
- 19.Bhattacharyya AK, Connor WE. Beta-sitosterolemia and xanthomatosis. A newly described lipid storage disease in two sisters. J Clin Invest. 1974;53:1033–1043. doi: 10.1172/JCI107640. doi:10.1172/JCI107640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berge KE, Tian H, Graf GA, Yu L, Grishin NV, Schultz J, Kwiterovich P, Shan B, Barnes R, Hobbs HH. Accumulation of dietary cholesterol in sitosterolemia caused by mutations in adjacent ABC transporters. Science. 2000;290:1771–1775. doi: 10.1126/science.290.5497.1771. doi:10.1126/science.290.5497.1771. [DOI] [PubMed] [Google Scholar]
- 21.Lee MH, Lu K, Hazard S, Yu H, Shulenin S, Hidaka H, Kojima H, Allikmets R, Sakuma N, Pegoraro R, Srivastava AK, Salen G, Dean M, Patel SB. Identification of a gene, ABCG5, important in the regulation of dietary cholesterol absorption. Nat Genet. 2001;27:79–83. doi: 10.1038/83799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Assmann G, Cullen P, Erbey J, Ramey DR, Kannenberg F, Schulte H. Plasma sitosterol elevations are associated with an increased incidence of coronary events in men: results of a nested case-control analysis of the Prospective Cardiovascular Munster (PROCAM) study. Nutr Metab Cardiovasc Dis. 2006;16:13–21. doi: 10.1016/j.numecd.2005.04.001. doi:10.1016/j.numecd.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 23.Rajaratnam RA, Gylling H, Miettinen TA. Independent association of serum squalene and noncholesterol sterols with coronary artery disease in postmenopausal women. J Am Coll Cardiol. 2000;35:1185–1191. doi: 10.1016/s0735-1097(00)00527-1. doi:10.1016/S0735-1097(00)00527-1. [DOI] [PubMed] [Google Scholar]
- 24.Matthan NR, Pencina M, Larocque JM, Jacques PF, D'Agostino RB, Schaefer EJ, Lichtenstein AH. Alterations in cholesterol absorption and synthesis characterize Framingham offspring study participants with coronary heart disease. J Lipid Res. 2009;50:1927–1935. doi: 10.1194/jlr.P900039-JLR200. doi:10.1194/jlr.P900039-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;67:e1000097. doi: 10.1371/journal.pmed.1000097. doi:10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA. 1998;279:1477–1482. doi: 10.1001/jama.279.18.1477. doi:10.1001/jama.279.18.1477. [DOI] [PubMed] [Google Scholar]
- 27.Teupser D, Baber R, Ceglarek U, Scholz M, Illig T, Gieger C, Holdt LM, Leichtle A, Greiser KH, Huster D, Linsel-Nitschke P, Schafer A, Braund PS, Tiret L, Stark K, Raaz-Schrauder D, Fiedler GM, Wilfert W, Beutner F, Gielen S, Grosshennig A, Konig IR, Lichtner P, Heid IM, Kluttig A, El Mokhtari NE, Rubin D, Ekici AB, Reis A, Garlichs CD, Hall AS, Matthes G, Wittekind C, Hengstenberg C, Cambien F, Schreiber S, Werdan K, Meitinger T, Loeffler M, Samani NJ, Erdmann J, Wichmann HE, Schunkert H, Thiery J. Genetic regulation of serum phytosterol levels and risk of coronary artery disease. Circ Cardiovasc Genet. 2010;3:331–339. doi: 10.1161/CIRCGENETICS.109.907873. doi:10.1161/CIRCGENETICS.109.907873. [DOI] [PubMed] [Google Scholar]
- 28.Dickersin K, Berlin JA. Meta-analysis: state-of-the-science. Epidemiol Rev. 1992;14:154–176. doi: 10.1093/oxfordjournals.epirev.a036084. [DOI] [PubMed] [Google Scholar]
- 29.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. doi:10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 30.Glueck CJ, Speirs J, Tracy T, Streicher P, Illig E, Vandegrift J. Relationships of serum plant sterols (phytosterols) and cholesterol in 595 hypercholesterolemic subjects, and familial aggregation of phytosterols, cholesterol, and premature coronary heart disease in hyperphytosterolemic probands and their first-degree relatives. Metabolism. 1991;40:842–848. doi: 10.1016/0026-0495(91)90013-m. doi:10.1016/0026-0495(91)90013-M. [DOI] [PubMed] [Google Scholar]
- 31.Sudhop T, Gottwald BM, von Bergmann K. Serum plant sterols as a potential risk factor for coronary heart disease. Metabolism. 2002;51:1519–1521. doi: 10.1053/meta.2002.36298. doi:10.1053/meta.2002.36298. [DOI] [PubMed] [Google Scholar]
- 32.Weingartner O, Lutjohann D, Ji S, Weisshoff N, List F, Sudhop T, von Bergmann K, Gertz K, Koenig J, Schafers HJ, Endres M, Bohm M, Laufs U. Vascular effects of diet supplementation with plant sterols. J Am Coll Cardiol. 2008;51:1553–1561. doi: 10.1016/j.jacc.2007.09.074. doi:10.1016/j.jacc.2007.09.074. [DOI] [PubMed] [Google Scholar]
- 33.Helske S, Miettinen T, Gylling H, Mayranpaa M, Lommi J, Turto H, Werkkala K, Kupari M, Kovanen PT. Accumulation of cholesterol precursors and plant sterols in human stenotic aortic valves. J Lipid Res. 2008;49:1511–1518. doi: 10.1194/jlr.M800058-JLR200. doi:10.1194/jlr.M800058-JLR200. [DOI] [PubMed] [Google Scholar]
- 34.Miettinen TA, Nissinen M, Lepantalo M, Alback A, Railo M, Vikatmaa P, Kaste M, Mustanoja S, Gylling H. Non-cholesterol sterols in serum and endarterectomized carotid arteries after a short-term plant stanol and sterol ester challenge. Nutr Metab Cardiovasc Dis. 2010 doi: 10.1016/j.numecd.2009.09.006. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 35.Miettinen TA, Railo M, Lepantalo M, Gylling H. Plant sterols in serum and in atherosclerotic plaques of patients undergoing carotid endarterectomy. J Am Coll Cardiol. 2005;45:1794–1801. doi: 10.1016/j.jacc.2005.02.063. doi:10.1016/j.jacc.2005.02.063. [DOI] [PubMed] [Google Scholar]
- 36.Raitakari OT, Salo P, Gylling H, Miettinen TA. Plant stanol ester consumption and arterial elasticity and endothelial function. Br J Nutr. 2008;100:603–608. doi: 10.1017/S0007114508922546. [DOI] [PubMed] [Google Scholar]
- 37.Sutherland WHF, Williams MJA, Nye ER, Restiaux NJ, de Jong SA, Walker HL. Associations of plasma noncholesterol sterol levels with severity of coronary disease. Nutr Metab Cardiovasc Dis. 1998;8:386–391. [Google Scholar]
- 38.Thiery J, Ceglarek U, Fiedler GM, Leichtle A, Baumann S, Deupser D, Lang O, Baumert J, Meisinger C, Loewel H, Doering A. Elevated campesterol serum levels: a significant predictor of incident myocardial infarction: results of the Population-based MONICA/KORA Follow-up Study 1994 to 2005. Circulation. 2006;114 II_884. [Google Scholar]
- 39.Escurriol V, Cofan M, Moreno-Iribas C, Larranaga N, Martinez C, Navarro C, Rodriguez L, Gonzalez CA, Corella D, Ros E. Phytosterol plasma concentrations and coronary heart disease in the prospective Spanish EPIC cohort. J Lipid Res. 2010;51:618–624. doi: 10.1194/jlr.P000471. doi:10.1194/jlr.P000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fassbender K, Lutjohann D, Dik MG, Bremmer M, Konig J, Walter S, Liu Y, Letiembre M, von Bergmann K, Jonker C. Moderately elevated plant sterol levels are associated with reduced cardiovascular risk-the LASA study. Atherosclerosis. 2008;196:283–288. doi: 10.1016/j.atherosclerosis.2006.10.032. doi:10.1016/j.atherosclerosis.2006.10.032. [DOI] [PubMed] [Google Scholar]
- 41.Gylling H, Hallikainen M, Rajaratnam RA, Simonen P, Pihlajamaki J, Laakso M, Miettinen TA. The metabolism of plant sterols is disturbed in postmenopausal women with coronary artery disease. Metabolism. 2009;58:401–407. doi: 10.1016/j.metabol.2008.10.015. doi:10.1016/j.metabol.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 42.Matthan NR, Resteghini N, Robertson M, Ford I, Shepherd J, Packard C, Buckley BM, Jukema JW, Lichtenstein AH, Schaefer EJ. Cholesterol absorption and synthesis markers in individuals with and without a CHD event during pravastatin therapy: insights from the PROSPER trial. J Lipid Res. 2010;51:202–209. doi: 10.1194/jlr.M900032-JLR200. doi:10.1194/jlr.M900032-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pinedo S, Vissers MN, von Bergmann K, Elharchaoui K, Lutjohann D, Luben R, Wareham NJ, Kastelein JJ, Khaw KT, Boekholdt SM. Plasma levels of plant sterols and the risk of coronary artery disease: the prospective EPIC-Norfolk Population Study. J Lipid Res. 2007;48:139–144. doi: 10.1194/jlr.M600371-JLR200. doi:10.1194/jlr.M600371-JLR200. [DOI] [PubMed] [Google Scholar]
- 44.Rajaratnam RA, Gylling H, Miettinen TA. Cholesterol absorption, synthesis, and fecal output in postmenopausal women with and without coronary artery disease. Arterioscler Thromb Vasc Biol. 2001;21:1650–1655. doi: 10.1161/hq1001.097019. doi:10.1161/hq1001.097019. [DOI] [PubMed] [Google Scholar]
- 45.Shay CM, Evans RW, Orchard TJ. Do plant sterol concentrations correlate with coronary artery disease in type 1 diabetes? A report from the Pittsburgh Epidemiology of Diabetes Complications Study. J Diabetes. 2009;1:112–117. doi: 10.1111/j.1753-0407.2009.00012.x. doi:10.1111/j.1753-0407.2009.00012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Silbernagel G, Fauler G, Hoffmann MM, Lutjohann D, Winkelmann BR, Boehm BO, Maerz W. The associations of cholesterol metabolism and plasma plant sterols with all-cause- and cardiovascular mortality. J Lipid Res. 2010;51:2384–2393. doi: 10.1194/jlr.P002899. doi:10.1194/jlr.P002899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Silbernagel G, Fauler G, Renner W, Landl EM, Hoffmann MM, Winkelmann BR, Boehm BO, Maerz W. The relationships of cholesterol metabolism and plasma plant sterols with the severity of coronary artery disease. J Lipid Res. 2009;50:334–341. doi: 10.1194/jlr.P800013-JLR200. doi:10.1194/jlr.P800013-JLR200. [DOI] [PubMed] [Google Scholar]
- 48.Strandberg TE, Gylling H, Tilvis RS, Miettinen TA. Serum plant and other noncholesterol sterols, cholesterol metabolism and 22-year mortality among middle-aged men. Atherosclerosis. 2010;210:282–287. doi: 10.1016/j.atherosclerosis.2009.11.007. doi:10.1016/j.atherosclerosis.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 49.Strandberg TE, Tilvis RS, Pitkala KH, Miettinen TA. Cholesterol and glucose metabolism and recurrent cardiovascular events among the elderly: a prospective study. J Am Coll Cardiol. 2006;48:708–714. doi: 10.1016/j.jacc.2006.04.081. doi:10.1016/j.jacc.2006.04.081. [DOI] [PubMed] [Google Scholar]
- 50.Weingartner O, Weingartner N, Scheller B, Lutjohann D, Graber S, Schafers HJ, Böhm M, Laufs U. Alterations in cholesterol homeostasis are associated with coronary heart disease in patients with aortic stenosis. Coron Artery Dis. 2009;20:376–382. doi: 10.1097/MCA.0b013e32832fa947. doi:10.1097/MCA.0b013e32832fa947. [DOI] [PubMed] [Google Scholar]
- 51.Wilund KR, Yu L, Xu F, Vega GL, Grundy SM, Cohen JC, Hobbs HH. No association between plasma levels of plant sterols and atherosclerosis in mice and men. Arterioscler Thromb Vasc Biol. 2004;24:2326–2332. doi: 10.1161/01.ATV.0000149140.00499.92. doi:10.1161/01.ATV.0000149140.00499.92. [DOI] [PubMed] [Google Scholar]
- 52.Windler E, Zyriax BC, Kuipers F, Linseisen J, Boeing H. Association of plasma phytosterol concentrations with incident coronary heart disease Data from the CORA study, a case-control study of coronary artery disease in women. Atherosclerosis. 2009;203:284–290. doi: 10.1016/j.atherosclerosis.2008.06.014. doi:10.1016/j.atherosclerosis.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 53.Miettinen TA, Tilvis RS, Kesämiemi YA. Serum plant sterols and cholesterol precursors reflect cholesterol absorption and synthesis in volunteers of a randomly selected male population. Am J Epidemiol. 1990;13:20–31. doi: 10.1093/oxfordjournals.aje.a115479. [DOI] [PubMed] [Google Scholar]
- 54.Greenberg ME, Smith JD, Sehayek E. Moderately decreased cholesterol absorption rates are associated with a large atheroprotective effect. Arterioscler Thromb Vasc Biol. 2009;29:1745–1750. doi: 10.1161/ATVBAHA.109.194605. doi:10.1161/ATVBAHA.109.194605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Simonen P, Gylling H, Howard AN, Miettinen TA. Introducing a new component of the metabolic syndrome: low cholesterol absorption. Am J Clin Nutr. 2000;72:82–88. doi: 10.1093/ajcn/72.1.82. [DOI] [PubMed] [Google Scholar]
- 56.Gylling H, Hallikainen M, Kolehmainen M, Toppinen L, Pihlajamäki J, Mykkänen H, Agren JJ, Rauramaa R, Laakso M, Miettinen TA. Cholesterol synthesis prevails over absorption in metabolic syndrome. Transl Res. 2007;149:310–316. doi: 10.1016/j.trsl.2006.11.012. doi:10.1016/j.trsl.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 57.Pihlajamaki J, Gylling H, Miettinen TA, Laakso M. Insulin resistance is associated with increased cholesterol synthesis and decreased cholesterol absorption in normoglycemic men. J Lipid Res. 2004;45:507–512. doi: 10.1194/jlr.M300368-JLR200. doi:10.1194/jlr.M300368-JLR200. [DOI] [PubMed] [Google Scholar]
- 58.Simonen PP, Gylling HK, Miettinen TA. Diabetes contributes to cholesterol metabolism regardless of obesity. Diabetes Care. 2002;25:1511–1515. doi: 10.2337/diacare.25.9.1511. doi:10.2337/diacare.25.9.1511. [DOI] [PubMed] [Google Scholar]
- 59.Hallikainen M, Kolehmainen M, Schwab U, Laaksonen DE, Niskanen L, Rauramaa R, Pihlajamaki J, Uusitupa M, Miettinen TA, Gylling H. Serum adipokines are associated with cholesterol metabolism in the metabolic syndrome. Clin Chim Acta. 2007;383:126–132. doi: 10.1016/j.cca.2007.05.006. doi:10.1016/j.cca.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 60.Gylling H, Tuominen JA, Koivisto VA, Miettinen TA. Cholesterol metabolism in type 1 diabetes. Diabetes. 2004;53:2217–2222. doi: 10.2337/diabetes.53.9.2217. doi:10.2337/diabetes.53.9.2217. [DOI] [PubMed] [Google Scholar]
- 61.Kesaniemi YA, Ehnholm C, Miettinen TA. Intestinal cholesterol absorption efficiency in man is related to apoprotein E phenotype. J Clin Invest. 1987;80:578–581. doi: 10.1172/JCI113107. doi:10.1172/JCI113107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cohen JC, Pertsemlidis A, Fahmi S, Esmail S, Vega GL, Grundy SM, Hobbs HH. Multiple rare variants in NPC1L1 associated with reduced sterol absorption and plasma low-density lipoprotein levels. Proc Natl Acad Sci USA. 2006;103:1810–1815. doi: 10.1073/pnas.0508483103. doi:10.1073/pnas.0508483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gylling H, Hallikainen M, Pihlajamaki J, Agren J, Laakso M, Rajaratnam RA, Rauramaa R, Miettinen TA. Polymorphisms in the ABCG5 and ABCG8 genes associate with cholesterol absorption and insulin sensitivity. J Lipid Res. 2004;45:1660–1665. doi: 10.1194/jlr.M300522-JLR200. doi:10.1194/jlr.M300522-JLR200. [DOI] [PubMed] [Google Scholar]
- 64.Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–414. doi: 10.1016/j.jacc.2006.09.032. doi:10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 65.Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. doi:10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 66.Strandberg TE, Pitkala KH. Frailty in elderly people. Lancet. 2007;369:1328–1329. doi: 10.1016/S0140-6736(07)60613-8. doi:10.1016/S0140-6736(07)60613-8. [DOI] [PubMed] [Google Scholar]
- 67.Weingartner O, Lutjohann D, Ji S, Weisshoff N, List F, Sudhop T, von Bergmann K, Gertz K, Konig J, Schafers HJ, Endres M, Bohm M, Laufs U. Vascular effects of diet supplementation with plant sterols. J Am Coll Cardiol. 2008;51:1553–1561. doi: 10.1016/j.jacc.2007.09.074. doi:10.1016/j.jacc.2007.09.074. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.