Abstract
OBJECTIVE
Calcium dobesilate (CaD) has been used in the treatment of diabetic retinopathy in the last decades, but its mechanisms of action are not elucidated. CaD is able to correct the excessive vascular permeability in the retina of diabetic patients and in experimental diabetes. We investigated the molecular and cellular mechanisms underlying the protective effects of CaD against the increase in blood–retinal barrier (BRB) permeability induced by diabetes.
RESEARCH DESIGN AND METHODS
Wistar rats were divided into three groups: controls, streptozotocin-induced diabetic rats, and diabetic rats treated with CaD. The BRB breakdown was evaluated using Evans blue. The content or distribution of tight junction proteins (occludin, claudin-5, and zonula occluden-1 [ZO-1]), intercellular adhesion molecule-1 (ICAM-1), and p38 mitogen-activated protein kinase (p38 MAPK) was evaluated by Western blotting and immunohistochemistry. Leukocyte adhesion was evaluated in retinal vessels and in vitro. Oxidative stress was evaluated by the detection of oxidized carbonyls and tyrosine nitration. NF-κB activation was measured by enzyme-linked immunosorbent assay.
RESULTS
Diabetes increased the BRB permeability and retinal thickness. Diabetes also decreased occludin and claudin-5 levels and altered the distribution of ZO-1 and occludin in retinal vessels. These changes were inhibited by CaD treatment. CaD also inhibited the increase in leukocyte adhesion to retinal vessels or endothelial cells and in ICAM-1 levels, induced by diabetes or elevated glucose. Moreover, CaD decreased oxidative stress and p38 MAPK and NF-κB activation caused by diabetes.
CONCLUSIONS
CaD prevents the BRB breakdown induced by diabetes, by restoring tight junction protein levels and organization and decreasing leukocyte adhesion to retinal vessels. The protective effects of CaD are likely to involve the inhibition of p38 MAPK and NF-κB activation, possibly through the inhibition of oxidative/nitrosative stress.
The blood–retinal barrier (BRB) breakdown is the hallmark of diabetic retinopathy (1). Alterations in BRB occur early in the progression of diabetic retinopathy and eventually lead to macular edema, which is responsible for vision loss (2). The increase in BRB permeability is associated with changes in the expression, content, phosphorylation, and distribution of tight junction proteins in retinal vessels (3–7), as well as with increased vesicular transport mediated by endocytotic vesicles (8).
Occludin and claudins are responsible for the direct cell-to-cell attachment in the tight junction barrier (9,10) and are a crucial determinant of tight junction permeability properties in endothelial cells (11,12). Claudin-5 is necessary to preserve the vascular barrier to small (<0.8 kDa) molecules in the brain (13), and it possibly also plays a similar role in the BRB. The zonula occluden proteins (ZO-1, -2, and -3) coordinate the assembly of the junctional complex and provide the interaction with components of the cytoskeleton (14), also important for BRB function.
Diabetes causes metabolic and physiologic abnormalities in the retina, and it appears that inflammation plays a critical role in the development of diabetic retinopathy. Those changes include the upregulation of inducible nitric oxide synthase, cyclooxygenase-2, intercellular adhesion molecule-1 (ICAM-1), caspase-1, vascular endothelial growth factor (VEGF), and nuclear factor kappa B (NF-κB), as well as increased production of nitric oxide, prostaglandin E2, and cytokines (15,16). We and others also demonstrated that the adhesion of leukocytes to retinal vessels is increased in the retinas of diabetic animals, and this increase is correlated with changes in tight junction proteins and increased BRB permeability (4,6,8,17,18). The increase in leukostasis is also associated with an increase in the expression of ICAM-1 by retinal endothelial cells (18,19). NF-κB regulates the expression of adhesion molecules, such as ICAM-1, and NF-κB activation has been correlated with the increase in leukostasis and BRB breakdown in diabetic rat retinas (20). Moreover, the p38 mitogen-activated protein kinase (p38 MAPK), a stress-activated serine/threonine protein kinase, is activated in response to proinflammatory cytokines and oxidative stress. The activation of p38 MAPK has been reported in the retinas of diabetic rats and is associated with BRB breakdown (21).
Calcium dobesilate (CaD) is considered an angioprotective drug, and it has been used in the treatment of diabetic retinopathy and chronic venous insufficiency in several countries during the last few decades (22,23), but its efficacy in the treatment of diabetic retinopathy is still a matter of controversy. Several clinical studies have shown a slowdown of the progression of diabetic retinopathy after long-term oral treatment with CaD. Its clinical effectiveness occurs mainly through a correction of the excessive vascular permeability in the retina (24,25). CaD decreases albumin leakage in the retina of diabetic animals (26), supporting its beneficial effects in BRB permeability. Other studies did not find beneficial effects in patients with diabetic retinopathy (27–29), but patients were treated with lower doses of CaD and for shorter periods (6–12 months). Recently, in a follow-up study (CALDIRET) of five years involving 635 patients with mild-to-moderate nonproliferative diabetic retinopathy, treatment with CaD was not able to reduce macular edema (30).
Despite the use of CaD in the treatment of diabetic retinopathy in the last few decades, very low attention has been given to the molecular and cellular mechanisms underlying its vascular protective effects. In diabetic rats, the protective effect of CaD against BRB leakage was correlated with a decrease in the levels of advanced glycation end products and VEGF in the retina (26). It also has been suggested that the beneficial effects of CaD might be due to its antioxidant properties (31,32). The present study aimed to clarify the molecular and cellular mechanisms underlying the protective effect of CaD against BRB permeability induced by diabetes. We evaluated for the first time whether CaD efficacy, in the early stages of diabetes, is linked to its effects on tight junctions and leukostasis. Moreover, its effects on the activation of p38 MAPK and NF-κB pathways, and on oxidative and nitrosative stress, were also addressed.
RESEARCH DESIGN AND METHODS
Materials and reagents used to carry out the experiments are described in the supplementary Materials and Methods, available in an online appendix at http://diabetes.diabetesjournals.org/cgi/content/full/db09-1421/DC1.
Animal model.
All procedures involving animals were conducted in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research. Diabetes was induced in 8–9-week-old male Wistar rats with an intraperitoneal injection of streptozotocin (65 mg/kg, in 10 mmol/l citrate buffer, pH 4.5). Two days later, animals with blood glucose levels >250 mg/dl were considered diabetic. The experiments were performed 1 month after diabetes induction.
The animals were divided into three groups (7–9 animals/group): control, diabetics, and diabetics treated with CaD (100 mg/kg/day; orally given) during the last 10 days of diabetes. We also evaluated the effect of CaD on weight, blood glucose levels, retinal vascular permeability, retinal thickness, leukocyte adhesion to retinal vessels, tight junction protein content and localization, ICAM-1 content, formation of oxidized carbonyls and nitrotyrosine residues in proteins, and p38 MAPK and NF-κB activation. The results were similar to those obtained with control animals.
Measurement of BRB permeability.
BRB permeability was quantified with Evans blue, which binds to the plasma albumin, using the method described by Xu and colleagues (33), with some modifications. A more detailed description can be found in the supplementary Materials and Methods.
Retinal thickness.
Retinal thickness was determined in retinal sections stained with hematoxylin/eosin as described in the supplementary Materials and Methods.
Visualization of retinal vessel leakage.
Retinal vascular leakage was visualized using Evans blue. Under anesthesia, the rats were administered Evans blue (100 mg/kg) via tail vein and kept on a warm pad for 60 min. The eyes were enucleated and fixed with 2% paraformaldehyde in PBS for 2 h. The retina was isolated, flat-mounted, and examined under a confocal microscope (LSM 510, Carl Zeiss, Gottingen, Germany) to check for Evans blue extravasation from retinal vessels.
Western blot analysis.
Western blotting of cellular lysates was performed as detailed in the supplementary Materials and Methods.
Immunolocalization of occludin, claudin-5, and ZO-1 in retinal vessels.
The retinas were isolated (three animals) and immersed in 2% paraformaldehyde for 2 × 5 min at room temperature. After washing 2 × 5 min in PBS with 0.3% Triton X-100, the retinas were immersed in blocking solution (6% goat serum) in PBS with 0.3% Triton X-100 for 30 min, and then incubated for 3 days at 4°C with anti-occludin (1:100), anti-claudin-5 (1:100), or anti-ZO-1 (1:100) antibodies. After incubation, the retinas were washed for 24 h and incubated with an Alexa 488-conjugated secondary antibody (goat anti-rabbit IgG, 1:250) in PBS with 0.3% Triton X-100. After incubation, the retinas were washed and flat-mounted for visualization under a confocal microscope (LSM510, Carl Zeiss, Gottingen, Germany).
Leukocyte labeling.
Leukocyte suspensions were obtained from the spleen of normal Wistar rats. The cells were resuspended in 20 ml of complete medium [RPMI 1,640 supplemented with 10% heat-inactivated FCS, 1% sodium pyruvate, 4 mmol/l l-glutamine, 1× nonessential amino acids]. To label the cells, 2 × 107 cells/ml were incubated with 40 μg/ml calcein-AM for 30 min at 37°C (34). Calcein-AM is nontoxic and has no effect on cell adhesion (35). The cells were washed, and 4 × 107 leukocytes in 200 μl RPMI were adoptively transferred into each rat through the tail vein.
Leukocyte adhesion to retinal vessels in whole-mounted retinas.
Approximately 30 min after labeled leukocytes injection, Evans blue (100 mg/kg) was injected through the tail vein. Thirty min later, the animals were perfused with citrate-buffered 4% paraformaldehyde (37°C), and then the eyes were removed and immersed in 2% paraformaldehyde for 2 h at room temperature. The retinas were dissected, flat-mounted, and analyzed by confocal microscopy (LSM 510, Carl Zeiss, Gottingen, Germany) to count the leukocytes adhering to retinal vessels.
Retinal endothelial cell culture.
Rat retinal endothelial cells (TR-iBRB2 cell line) (36) were cultured in low-glucose Dulbecco's modified Eagle's medium containing 10% FBS, 17.8 mmol/l sodium bicarbonate, 0.1 mg/ml streptomycin, and 100 units/ml penicillin. Cells were maintained at 33°C in a humidified atmosphere of 5% CO2/air. Cells were incubated with 24.5 mmol/l glucose (30 mmol/l final concentration) or with mannitol (24.5 mmol/l + 5.5. mM glucose; osmotic control) for 4 days. Endothelial cells were also incubated with 12.5, 25, and 50 μg/ml of CaD for 4 days.
In vitro leukocyte adhesion.
Endothelial cells were plated in a 24-well plate for 4 days. Leukocytes were harvested and labeled with Calcein-AM. The suspension of leukocytes was added to the monolayer of endothelial cells (2 × 106 leukocytes/well) for 90 min at 37°C. After incubation, nonadherent cells were removed by gentle washing with RPMI. The emitted fluorescence (arbitrary units) of adherent leukocytes was measured in a fluorescence plate reader (excitation wavelength, 490 nm; emission wavelength, 530 nm).
Detection of oxidized carbonyls in proteins.
We used the 2,4-dinitrophenylhydrazone (DNP) to examine the direct oxidative injury to proteins. DNP specifically reacts with the oxidized carbonyl residues present in proteins. A more detailed description can be found in the supplementary Materials and Methods.
NF-κB activation.
Activation of NF-κB was determined in retinal extracts by enzyme-linked immunosorbent assay, using a NF-κB transcription factor kit (Active Motif, Rixensart, Belgium), following the manufacturer's instructions, as briefly described in the supplementary Materials and Methods.
Immunohistochemistry in retinal sections.
The formation of nitrotyrosine residues in the retina was evaluated in retinal sections by immunohistochemistry, as described in the supplementary Materials and Methods.
Data are expressed as mean ± SEM. Statistical significance was determined by ANOVA, followed by Dunnett or Bonferroni post hoc test, as indicated in figure legends.
RESULTS
CaD inhibits the increase in BRB permeability and retinal thickness induced by diabetes.
CaD was orally administered (100 mg/kg/day) during the last 10 days of diabetes (30 days duration). After 1 month of diabetes, the weight gain in diabetic animals was significantly less when compared with controls (219.5 ± 6.6 and 344.6 ± 5.8 g, respectively) and the blood glucose levels were significantly higher (496.2 ± 15.0 and 96.3 ± 2.4 mg/dl, respectively). The weight and the blood glucose levels in diabetic animals treated with CaD were found to be similar to the values obtained for diabetic animals without treatment (217.3 ± 4.5 g and 470.9 ± 20.5 mg/dl, respectively) (Table 1).
TABLE 1.
Weight and blood glucose levels of control, diabetic, and diabetic CaD-treated animals
| Weight (g) | Glycemia (mg/dl) | N | |
|---|---|---|---|
| Control | 344.6 ± 5.8 | 96.3 ± 2.7 | 29 |
| Diabetic | 219.5 ± 6.6*** | 496.2 ± 15.0*** | 24 |
| Diabetic + CaD | 217.3 ± 4.5*** | 470.9 ± 20.5*** | 26 |
Diabetic animals (1-month diabetes duration) were treated with CaD (100 mg/kg) in the last 10 days of diabetes. Weight (g) and blood glucose levels (mg/dl) were measured before animal sacrifice and represent the mean ± SEM.
***P < 0.01, significantly different from control; ANOVA (one-way) followed by Dunnett post hoc test.
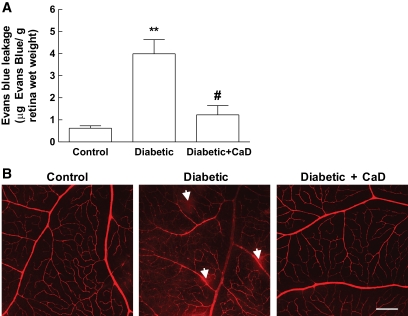
Diabetes increased the BRB permeability in diabetic rats (4.0 ± 0.6 μg Evans blue/g wet wt retina) when compared with control animals (0.6 ± 0.1 μg Evans blue/g wet wt retina). In diabetic rats treated with CaD, there was a significant decrease in BRB permeability (1.2 ± 0.4 μg Evans blue/g wet wt retina) when compared with diabetic animals (Fig. 1A). The blood vessel leakage was also visualized with Evans blue in retina flat mounts. In control retinas, Evans blue fluorescence was limited to the blood vessels. In diabetic rats, focal leakage of the dye from capillaries and larger vessels was detected, and the treatment with CaD prevented this effect (Fig. 1B), corroborating the data obtained with the quantitative Evans blue assay. Moreover, CaD inhibited the increase in retinal thickness induced by diabetes. Diabetic retinas were significantly thicker than control retinas (153.0 ± 4.0 vs. 135.7 ± 5.0 μm), and no significant difference was found in retinal thickness between diabetic animals treated with CaD and control animals (145.2 ± 5.6 vs. 135.7 ± 5.0 μm) (Table 2).
FIG. 1.
Diabetes increases BRB permeability: protective effect of CaD. A: Quantitative measure of BRB permeability by quantification of extravasated Evans blue. Data are presented as μg of Evans blue per retina wet wt (g) and represent the mean ± SEM of 7–10 animals. **P < 0.01, significantly different from control; ANOVA (one-way) followed by Dunnett post hoc test. #P < 0.05, significantly different from diabetic; ANOVA (one-way) followed by Bonferroni post hoc test. B: Representative images showing Evans blue fluorescence, allowing the detection of leaking sites (arrows) in retinal vessels. In the retina of control animals, Evans blue fluorescence is limited to the blood vessels, while in diabetic retinas, the dye leaks out of the vessels to the retinal tissue. CaD treatment prevents the leakage of Evans blue. Magnification: 100×; bar 200 μm. (A high-quality color representation of this figure is available in the online issue.)
TABLE 2.
Retinal thickness measured in hematoxylin and eosin-stained retina sections from control, diabetic, and diabetic CaD-treated animals
| Retinal thickness (μm) | N | |
|---|---|---|
| Control | 135.7 ± 5.0 | 6 |
| Diabetic | 153.0 ± 4.0* | 6 |
| Diabetic + CaD | 145.2 ± 5.6 | 6 |
Diabetic animals (1-month diabetes duration) were treated with CaD (100 mg/kg) in the last 10 days of diabetes. The eye sections, from the proximity of optical disc, were stained with hematoxylin/eosin. The retinal thickness was measured by image analysis of 5 fields per section, from six animals. The results represent the mean ± SEM.
*P < 0.05, significantly different from control; ANOVA (one-way) followed by Dunnett post hoc test.
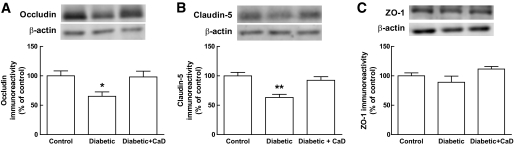
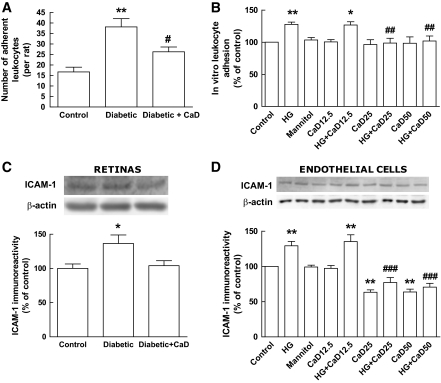
CaD prevents the changes in the content and/or distribution of tight junction proteins in retinal vessels induced by diabetes.
Diabetes induced a decrease in occludin and claudin-5 protein levels to 65.2% ± 7.5% and 63.2% ± 5.4% of the control, respectively. However, the total protein content of ZO-1 in retinal extracts of diabetic animals was not significantly different from the controls. Treatment of diabetic rats with CaD prevented the decrease in occludin and claudin-5 protein levels induced by diabetes (98.2% ± 9.7% and 92.4% ± 6.2% of the control, respectively; Fig. 2A and B). In the retinas of CaD-treated diabetic animals, the protein levels of ZO-1 were also similar to control values (Fig. 2C). Immunocytochemistry experiments confirmed these results (Fig. 3). The immunoreactivity of occludin and claudin-5 clearly decreased in the retinal vessels of diabetic animals. In addition, the localization of occludin and ZO-1, but not of claudin-5, appears to be altered when compared with the retinas of control animals. In diabetic animals, occludin and ZO-1 immunostaining in retinal vessels is not so well defined at endothelial cell borders, when compared with control animals. Also, in several regions of the vasculature, occludin and ZO-1 appear to accumulate in the cytosol of endothelial cells. The oral treatment with CaD prevented the decrease in occludin and claudin-5 immunoreactivity in retinal vessels induced by diabetes, as well as the alterations in occludin and ZO-1 localization in endothelial cells.
FIG. 2.
CaD prevents the decrease in occludin and claudin-5 protein levels in the rat retinas induced by diabetes. ZO-1 levels were not significantly changed. Tight junction protein levels were assessed by Western blotting. A representative Western blot is shown above each graph. Data are presented as percentage of control and represent the mean ± SEM of 7–9 animals. *P < 0.05, **P < 0.01, significantly different from control; ANOVA (one-way) followed by Dunnett post hoc test.
FIG. 3.
CaD prevents the decrease in occludin and claudin-5 immunoreactivity and the changes in occludin and ZO-1 distribution (arrows), in rat retinal vessels induced by diabetes. Magnifications: 200× (bar 100 μm) and 400× (bar 50 μm). (A high-quality color representation of this figure is available in the online issue.)
Caveolin-1 is an indicator of vascular permeability through a transcellular transport mechanism. Diabetes induces caveolin-1 overexpression in the rat retina (8). We found that diabetes increases caveolin-1 staining, mainly in the ganglion cell layer. However, CaD treatment did not prevent the increase in caveolin-1 immunoreactivity (data not shown).
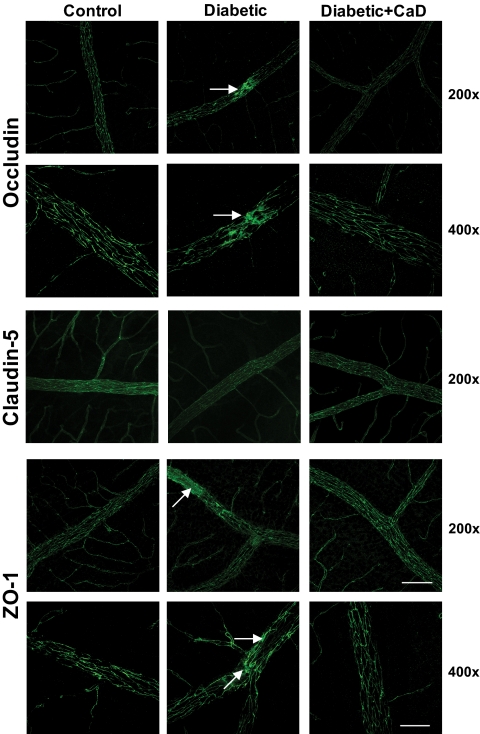
CaD inhibits leukocyte adhesion to retinal vessels induced by diabetes.
In diabetic animals, there was an increase in the number of leukocytes adhering to retinal vessels (38 ± 4 leukocytes/animal) compared with that in control animals (16 ± 2 leukocytes/animal). In diabetic rats treated with CaD, there was a significant decrease in the number of adherent leukocytes (26 ± 2 leukocytes/animal) when compared with diabetic animals (Fig. 4A).
FIG. 4.
Diabetes and elevated glucose increase the number of leukocytes adhering to retinal vessels and retinal endothelial cells and the content of ICAM-1: protective effect of CaD. A: Quantification of leukocytes adhering to retinal vessels. Data are presented as number of adherent leukocytes to retinal vessels per rat (two retinas) and represent the mean ± SEM of seven animals. B: Quantification of leukocyte adhesion to retinal endothelial cells (TR-iBRB2 cell line) using a fluorometric assay. Data are presented as percentage of control and represent the mean ± SEM of 7–10 independent experiments. C: The protein levels of ICAM-1 were evaluated in whole rat retinal extracts by Western blotting. Data are presented as percentage of control and represent the mean ± SEM of seven animals. D: The protein levels of ICAM-1 were evaluated in whole extracts of rat retinal endothelial cell cultures (TR-iBRB2 cell line) by Western blotting. Data are presented as percentage of control and represent the mean ± SEM of at least four independent experiments. *P < 0.05, **P < 0.01, significantly different from control; ANOVA (one-way) followed by Dunnett post hoc test. #P < 0.05, ##P < 0.01, ###P < 0.001, significantly different from diabetic rat or high glucose condition; ANOVA (one-way) followed by Bonferroni post hoc test. HG, high glucose (30 mmol/l, for 4 days); CaD12.5, CaD25, and CaD50, calcium dobesilate 12.5, 25, and 50 μg/ml, respectively (4 days).
CaD prevents the increase in leukocyte adhesion to retinal endothelial cells induced by high glucose.
We also evaluated the effect of CaD on the adhesion of leukocytes to retinal endothelial cells (TR-iBRB2 cell line). We reported previously that exposure of retinal endothelial cells to elevated glucose (30 mmol/l) for 4 days increases the adhesion of leukocytes to endothelial cells (18). As expected, the present data show that high glucose, but not mannitol (osmotic control), increased the adhesion of leukocytes to endothelial cells (128.7 ± 4.8% of the control). The exposure of endothelial cells to increasing concentrations of CaD (12.5, 25, and 50 μg/ml) for 4 days did not alter the adhesion of leukocytes (100.5 ± 3.5%, 96.3 ± 7.5%, and 98.4 ± 9.8% of the control, respectively). However, 25 and 50 μg/ml of CaD, but not 12.5 μg/ml, totally prevented the increase in leukocyte adhesion induced by high glucose (98.7 ± 7.5% and 101.9 ± 7.8% of the control, for 25 and 50 μg/ml, respectively; 126.8 ± 5.0% for 12.5 μg/ml) (Fig. 4B).
CaD prevents the upregulation of ICAM-1 levels in retinal endothelial cells induced by diabetes or high glucose.
The adhesion of leukocytes to retinal vessels is mediated by the interaction with ICAM-1, which is expressed in retinal endothelial cells. In the retinas of diabetic rats, the protein content of ICAM-1 increased to 136.4 ± 12.5% of the control. The upregulation of ICAM-1 induced by diabetes was prevented by CaD treatment (Fig. 4C). Similarly, in retinal endothelial cell cultures, elevated glucose (30 mmol/l), but not mannitol (osmotic control), increased the protein levels of ICAM-1 (129.2 ± 6.3% of the control). Surprisingly, 25 and 50 μg/ml of CaD, but not 12.5 μg/ml, significantly decreased the content of ICAM-1 in endothelial cells (63.3 ± 3.4% and 63.7 ± 4.0% of the control, respectively). In addition, 25 and 50 μg/ml of CaD prevented the increase in ICAM-1 levels induced by high glucose (77.2 ± 7.0% and 70.7 ± 5.2% of the control, respectively). The lower concentration of CaD used (12.5 μg/ml) did not prevent the increase in ICAM-1 content (135.2 ± 5.2% of the control) (Fig. 4D).
CaD reduces diabetes-induced oxidative and nitrosative stress.
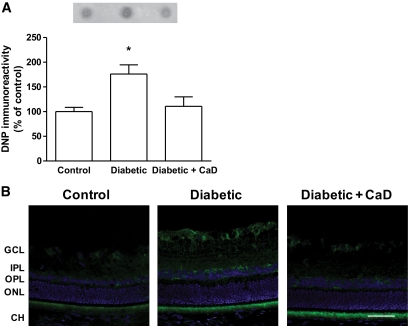
It has been claimed that CaD exerts its protective effects because of its antioxidant properties (26,32). Therefore, we evaluated the effects of CaD on the formation of oxidized carbonyl groups and on tyrosine nitration in retinal proteins. Oxidative injury to carbonyl residues significantly increased in diabetic retinas (176.2 ± 18.4% of the control) in comparison with the controls, and CaD treatment prevented that increase (110.6 ± 19.3% of the control) (Fig. 5A). Similarly, diabetes increased tyrosine nitration within retinal layers. The strongest immunoreactivity against nitrotyrosine residues was found within the ganglion cell layer (Fig. 5B). Treatment with CaD prevented the increase in tyrosine residues nitration.
FIG. 5.
CaD prevents oxidative and nitrosative stress induced by diabetes. A: The oxidized proteins were detected using an anti-DNP antibody by dot blot. A representative dot blot is shown above the graph. Data are presented as percentage of control and represent the mean ± SEM of 3–4 animals. *P < 0.05, significantly different from control; ANOVA (one-way) followed by Dunnett post hoc test. B: Representative images showing nitrotyrosine immunoreactivity (green), which allows the detection of nitrated tyrosine residues, and nuclear DAPI staining (blue). Magnification: 400×, bar 50 μm. GCL, ganglion cell layer; IPL, inner plexiform layer; OPL, outer plexiform layer; ONL, outer nuclear layer; CH, choroidal layer. (A high-quality digital representation of this figure is available in the online issue.)
CaD decreases the activation of p38 MAPK and NF-κB induced by diabetes.
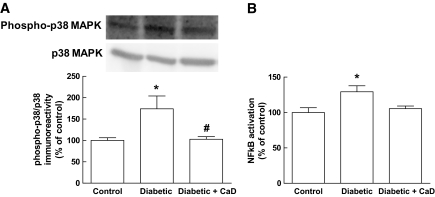
Both p38 MAPK and NF-κB were found to be activated in diabetic retinas, and their activation has been correlated with changes in BRB permeability (20,21). The activation of p38 MAPK, which was evaluated by the ratio phospho-p38/p38, significantly increased in the retinas of diabetic animals (174.1 ± 29.9% of the control) (Fig. 6A). Diabetes also increased NF-κB activity (129.3 ± 8.4% of the control) (Fig. 6B). Treatment with CaD prevented the activation of p38 MAPK and NF-κB induced by diabetes (Fig. 6A and B).
FIG. 6.
CaD inhibits the activation of p38 MAPK and NF-κB in diabetic rat retinas. A: The activation of p38 MAPK was determined by Western blotting, analyzing the phospho-p38/p38 MAPK ratio. A representative Western blot is shown above the graph. B: NF-κB activation was determined in retinal homogenates by ELISA (kit from Active Motif) using an antibody specific for the p65 subunit of NF-κB. A secondary antibody conjugated to horseradish peroxidase was used to quantify spectrophotometrically the activated form. Data are presented as percentage of control and represent the mean ± SEM of 6–7 animals. *P < 0.05, significantly different from control; ANOVA (one-way) followed by Dunnett post hoc test. #P < 0.05, significantly different from diabetic animals; ANOVA (one-way) followed by Bonferroni post hoc test.
DISCUSSION
This is the first study clearly showing that CaD inhibits changes in tight junction proteins, ICAM-1 and leukocyte adhesion to retinal vessels, which are known to underlie the increase in BRB permeability. These findings were correlated with the inhibition of oxidative/nitrosative stress, and p38 MAPK and NF-κB activity.
The potential beneficial effects of CaD on BRB are still controversial. Several studies have reported vasoprotective effects of CaD in the early stages of diabetic retinopathy (22,24,25). For example, in a double-blind, placebo-controlled study, a positive effect of CaD (2,000 mg daily for 2 years) was shown in patients with early diabetic retinopathy (25). Other studies have reported no beneficial effects of CaD in the retina of diabetic patients (27–29). In a recent study (CALDIRET) (30), where mild-to-moderate nonproliferative diabetic retinopathy patients were followed for five years, CaD failed to reduce diabetic macular edema. However, this study also shows that, within particular subgroups of patients, the treatment with CaD can be beneficial. It appears that the patients with accumulation of risk factors benefit with CaD. Altogether, these findings suggest that CaD might be effective in the early stages of the pathology, losing its efficacy in later stages (mild-to-moderate nonproliferative diabetic retinopathy), where macular edema might occur. In the later stages, CaD will possibly be effective only in some groups of patients. In animal models, where the duration of diabetes was relatively short, as is the case of this study, the beneficial effects of CaD on BRB are clear (26), supporting its use in the early stages of the disease. In humans, the genetic background, environmental conditions, and age are not as homogeneous as in animal models, and these factors certainly impact on the outcome of the study.
Diabetes decreased occludin and claudin-5 content but not the content of ZO-1. In mice, we reported that diabetes decreased retinal ZO-1 levels after two weeks of diabetes (18). A decrease in retinal ZO-1 levels was also found in diabetic rats, although with a prolonged diabetes duration (17). However, we found that diabetes disorganized ZO-1 distribution in retinal vessels, in a similar way as for occludin. Occludin interacts with ZO-1, and it must dimerize to form a four-helix bundle structure with ZO-1 (37), which may account for a similar disorganization pattern for both proteins. The distribution of claudin-5 was not affected, at least for this time point. Previous studies also showed that diabetes reduces occludin levels in retinal vessels and disorganizes occludin in retinal vessels (5,6,18). Barber and Antonetti did not find a reduction in claudin-5 levels (5), but they did not quantify claudin-5 levels in retinal extracts. Recently, two studies demonstrated that claudin-5 expression and protein content are decreased in the retinas of streptozotocin diabetic rats (8,17), but for longer periods of diabetes. Therefore, our data and these findings also point to an important role of claudin-5 in the BRB breakdown induced by diabetes.
CaD totally prevented the alterations in tight junction proteins, indicating that its protective effects against the increase in BRB permeability are due to its stabilizing effects on tight junction proteins (paracellular permeability). It has been claimed that the increase in vesicular transport (transcellular permeability) also contributes to the increase in BRB permeability (8). However, vesicular transport appears not to be affected by CaD, because it was not able to prevent the increase in caveolin-1 immunoreactivity induced by diabetes.
The increase in ICAM-1 expression and leukostasis is linked to the BRB breakdown (18,19,38,39). In retinas, CaD totally prevented the increase in ICAM-1 levels, but the increase in leukocyte adhesion was only partially inhibited. This observation suggests that other players are involved in leukocyte adhesion, which is probably not substantially affected by CaD as ICAM-1 is. For instance, in endothelial cell cultures, CaD per se decreased ICAM-1 levels. These data clearly suggest that CaD attenuates inflammatory processes occurring in diabetic retinas, which have been considered key players in BRB breakdown.
NF-κB activation is known to mediate the expression of cytokines and adhesion molecules, such as ICAM-1. In fact, it was found that NF-κB inhibition prevents the increase in ICAM-1 levels, leukocyte adhesion, and BRB leakage in diabetic retinas (20). Our results also suggest that CaD prevented the increase in ICAM-1 levels, leukocyte adhesion, and BRB leakage induced by diabetes, and this was correlated with the inhibition of NF-κB activation by CaD.
The protective effects of CaD against the BRB breakdown might also be due to its modulation of VEGF levels in the retina. VEGF is overexpressed in diabetic rat retinas and is involved in BRB leakage and leukocyte adhesion (40,41). CaD treatment decreases VEGF content in diabetic rats, and this observation was correlated with a decrease in BRB permeability (26).
Oxidative stress plays a role in leukocyte adhesion and BRB breakdown in the retinas of diabetic animals (18,42). The protective effects of CaD can be explained by its antioxidant properties. CaD is effective in scavenging hydroxyl radicals in vitro (31). Moreover, CaD stabilizes the BRB in diabetic rats, apparently because of its antioxidant action (26), and markedly reduces retinal edema protecting diabetic rat retina against the oxidative stress induced by ischemia/reperfusion (32). In this study, we confirmed that CaD decreases oxidative and nitrosative stress, because it completely prevented the increase in oxidized carbonyl groups and nitrotyrosine residues in proteins induced by diabetes. Because oxidative stress underlies inflammatory changes responsible for the BRB breakdown, our observations further support the idea that CaD vasoprotective effects might be mainly due to its antioxidant properties.
The activation of p38 MAPK and NF-κB pathways mediates BRB permeability in diabetic retinas (20,21). Also, the inhibition of oxidative stress decreases p38 MAPK and NF-κB activation, and this was correlated with the prevention of early changes in diabetic retinas (20,21,43). In addition, evidences have shown that both p38 MAPK and NF-κB regulate tight junctions. The inhibition of p38 MAPK pathway improves the barrier function in epithelial cells (44) and prevents tumor necrosis factor-α-induced ZO-1 dislocation in bovine corneal endothelial cells (45). Furthermore, tumor necrosis factor-α-mediated NF-κB activation decreases ZO-1 levels and distribution in intestinal epithelial cells (46). In this work, we found that CaD decreased oxidative and nitrosative stress in diabetic retinas, and this was correlated with the inhibition of p38 MAPK and NF-κB activation, as well as with the inhibition of changes in tight junction proteins, thus suggesting that the protective effects of CaD on paracellular permeability appear to be due to the inhibition of oxidative stress and consequently on p38 MAPK and NF-κB activation.
In summary, in this work we shed light into the molecular and cellular mechanisms underlying the protective effect of CaD against retinal vascular leakage induced by diabetes. CaD prevents changes in the content and distribution of tight junction proteins, as well as changes in ICAM-1 and leukocyte adhesion to retinal endothelial cells. These protective effects appear to be linked to its antioxidant effects, which prevent the activation of intracellular signaling pathways and transcription factors, such as p38 MAPK and NF-κB. These data reinforce the use of CaD in the treatment of diabetic retinopathy, particularly in the early stages of the disease.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by OM Pharma, Geneva, Switzerland. J.C.-V. contributed to the work performed; and he has an advisory role with OM Pharma. C.C. contributed to the work performed as head of preclinical and early clinical development at OM Pharma. No other potential conflicts of interest relevant to this article were reported.
E.C.L. and A.F.A. researched data, contributed to discussion, wrote the manuscript, and reviewed/edited the manuscript. J.M., P.V., and J.L. researched data and reviewed/edited the manuscript. C.C., J.B., and J.C.-V. contributed to discussion and reviewed/edited the manuscript.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1. Cunha-Vaz J, Faria de Abreu JR, Campos AJ. Early breakdown of the blood–retinal barrier in diabetes. Br J Ophthalmol 1975;59:649–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 3. Antonetti DA, Barber AJ, Hollinger LA, Wolpert EB, Gardner TW. Vascular endothelial growth factor induces rapid phosphorylation of tight junction proteins occludin and zonula occluden 1. A potential mechanism for vascular permeability in diabetic retinopathy and tumors. J Biol Chem 1999;274:23463–23467 [DOI] [PubMed] [Google Scholar]
- 4. Antonetti DA, Barber AJ, Khin S, Lieth E, Tarbell JM, Gardner TW. Vascular permeability in experimental diabetes is associated with reduced endothelial occludin content: vascular endothelial growth factor decreases occludin in retinal endothelial cells. Penn State Retina Research Group. Diabetes 1998;47:1953–1959 [DOI] [PubMed] [Google Scholar]
- 5. Barber AJ, Antonetti DA. Mapping the blood vessels with paracellular permeability in the retinas of diabetic rats. Invest Ophthalmol Vis Sci 2003;44:5410–5416 [DOI] [PubMed] [Google Scholar]
- 6. Barber AJ, Antonetti DA, Gardner TW. Altered expression of retinal occludin and glial fibrillary acidic protein in experimental diabetes. The Penn State Retina Research Group. Invest Ophthalmol Vis Sci 2000;41:3561–3568 [PubMed] [Google Scholar]
- 7. Harhaj NS, Felinski EA, Wolpert EB, Sundstrom JM, Gardner TW, Antonetti DA. VEGF activation of protein kinase C stimulates occludin phosphorylation and contributes to endothelial permeability. Invest Ophthalmol Vis Sci 2006;47:5106–5115 [DOI] [PubMed] [Google Scholar]
- 8. Klaassen I, Hughes JM, Vogels IM, Schalkwijk CG, Van Noorden CJ, Schlingemann RO. Altered expression of genes related to blood-retina barrier disruption in streptozotocin-induced diabetes. Exp Eye Res 2009;89:4–15 [DOI] [PubMed] [Google Scholar]
- 9. Fanning AS, Mitic LL, Anderson JM. Transmembrane proteins in the tight junction barrier. J Am Soc Nephrol 1999;10:1337–1345 [DOI] [PubMed] [Google Scholar]
- 10. Matter K, Balda MS. Occludin and the functions of tight junctions. Int Rev Cytol 1999;186:117–146 [DOI] [PubMed] [Google Scholar]
- 11. Hirase T, Staddon JM, Saitou M, Ando-Akatsuka Y, Itoh M, Furuse M, Fujimoto K, Tsukita S, Rubin LL. Occludin as a possible determinant of tight junction permeability in endothelial cells. J Cell Sci 1997;110(Pt 14):1603–1613 [DOI] [PubMed] [Google Scholar]
- 12. Turksen K, Troy TC. Barriers built on claudins. J Cell Sci 2004;117:2435–2447 [DOI] [PubMed] [Google Scholar]
- 13. Nitta T, Hata M, Gotoh S, Seo Y, Sasaki H, Hashimoto N, Furuse M, Tsukita S. Size-selective loosening of the blood-brain barrier in claudin-5-deficient mice. J Cell Biol 2003;161:653–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wittchen ES, Haskins J, Stevenson BR. Protein interactions at the tight junction. Actin has multiple binding partners, and ZO-1 forms independent complexes with ZO-2 and ZO-3. J Biol Chem 1999;274:35179–35185 [DOI] [PubMed] [Google Scholar]
- 15. Adamis AP, Berman AJ. Immunological mechanisms in the pathogenesis of diabetic retinopathy. Semin Immunopathol 2008;30:65–84 [DOI] [PubMed] [Google Scholar]
- 16. Kern TS. Contributions of inflammatory processes to the development of the early stages of diabetic retinopathy. Exp Diabetes Res 2007;2007:95103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bucolo C, Ward KW, Mazzon E, Cuzzocrea S, Drago F. Protective effects of a coumarin derivative in diabetic rats. Invest Ophthalmol Vis Sci 2009;50:3846–3852 [DOI] [PubMed] [Google Scholar]
- 18. Leal EC, Manivannan A, Hosoya K, Terasaki T, Cunha-Vaz J, Ambrósio AF, Forrester JV. Inducible nitric oxide synthase isoform is a key mediator of leukostasis and blood-retinal barrier breakdown in diabetic retinopathy. Invest Ophthalmol Vis Sci 2007;48:5257–5265 [DOI] [PubMed] [Google Scholar]
- 19. Miyamoto K, Khosrof S, Bursell SE, Rohan R, Murata T, Clermont AC, Aiello LP, Ogura Y, Adamis AP. Prevention of leukostasis and vascular leakage in streptozotocin-induced diabetic retinopathy via intercellular adhesion molecule-1 inhibition. Proc Natl Acad Sci U S A 1999;96:10836–10841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Joussen AM, Poulaki V, Mitsiades N, Kirchhof B, Koizumi K, Döhmen S, Adamis AP. Nonsteroidal anti-inflammatory drugs prevent early diabetic retinopathy via TNF-alpha suppression. FASEB J 2002;16:438–440 [DOI] [PubMed] [Google Scholar]
- 21. El-Remessy AB, Al-Shabrawey M, Khalifa Y, Tsai NT, Caldwell RB, Liou GI. Neuroprotective and blood-retinal barrier-preserving effects of cannabidiol in experimental diabetes. Am J Pathol 2006;168:235–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Berthet P, Farine JC, Barras JP. Calcium dobesilate: pharmacological profile related to its use in diabetic retinopathy. Int J Clin Pract 1999;53:631–636 [PubMed] [Google Scholar]
- 23. Tejerina T, Ruiz E. Calcium dobesilate: pharmacology and future approaches. Gen Pharmacol 1998;31:357–360 [DOI] [PubMed] [Google Scholar]
- 24. Leite EB, Mota MC, de Abreu JR, Cunha-Vaz JG. Effect of calcium dobesilate on the blood-retinal barrier in early diabetic retinopathy. Int Ophthalmol 1990;14:81–88 [DOI] [PubMed] [Google Scholar]
- 25. Ribeiro ML, Seres AI, Carneiro AM, Stur M, Zourdani A, Caillon P, Cunha-Vaz JG. DX-Retinopathy Study Group Effect of calcium dobesilate on progression of early diabetic retinopathy: a randomised double-blind study. Graefes Arch Clin Exp Ophthalmol 2006;244:1591–1600 [DOI] [PubMed] [Google Scholar]
- 26. Rota R, Chiavaroli C, Garay RP, Hannaert P. Reduction of retinal albumin leakage by the antioxidant calcium dobesilate in streptozotocin-diabetic rats. Eur J Pharmacol 2004;495:217–224 [DOI] [PubMed] [Google Scholar]
- 27. Daubresse JC, Meunier R, Dumont P. A controlled clinical trial of calcium dobesylate in the treatment of diabetic retinopathy. Diabete Metab 1977;3:27–30 [PubMed] [Google Scholar]
- 28. Larsen HW, Sander E, Hoppe R. The value of calcium dobesilate in the treatment of diabetic retinopathy. A controlled clinical trial. Diabetologia 1977;13:105–109 [DOI] [PubMed] [Google Scholar]
- 29. Stamper RL, Smith ME, Aronson SB, Cavender JC, Cleasby GW, Fung WE, Becker B. The effect of calcium dobesilate on nonproliferative diabetic retinopathy: a controlled study. Ophthalmology 1978;85:594–606 [DOI] [PubMed] [Google Scholar]
- 30. Haritoglou C, Gerss J, Sauerland C, Kampik A, Ulbig MW. CALDIRET study group Effect of calcium dobesilate on occurrence of diabetic macular oedema (CALDIRET study): randomised, double-blind, placebo-controlled, multicentre trial. Lancet 2009;373:1364–1371 [DOI] [PubMed] [Google Scholar]
- 31. Brunet J, Farine JC, Garay RP, Hannaert P. In vitro antioxidant properties of calcium dobesilate. Fundam Clin Pharmacol 1998;12:205–212 [DOI] [PubMed] [Google Scholar]
- 32. Szabo ME, Haines D, Garay E, Chiavaroli C, Farine JC, Hannaert P, Berta A, Garay RP. Antioxidant properties of calcium dobesilate in ischemic/reperfused diabetic rat retina. Eur J Pharmacol 2001;428:277–286 [DOI] [PubMed] [Google Scholar]
- 33. Xu Q, Qaum T, Adamis AP. Sensitive blood-retinal barrier breakdown quantitation using Evans blue. Invest Ophthalmol Vis Sci 2001;42:789–794 [PubMed] [Google Scholar]
- 34. Xu H, Manivannan A, Goatman KA, Liversidge J, Sharp PF, Forrester JV, Crane IJ. Improved leukocyte tracking in mouse retinal and choroidal circulation. Exp Eye Res 2002;74:403–410 [DOI] [PubMed] [Google Scholar]
- 35. Abbitt KB, Rainger GE, Nash GB. Effects of fluorescent dyes on selectin and integrin-mediated stages of adhesion and migration of flowing leukocytes. J Immunol Methods 2000;239:109–119 [DOI] [PubMed] [Google Scholar]
- 36. Hosoya K, Tomi M, Ohtsuki S, Takanaga H, Ueda M, Yanai N, Obinata M, Terasaki T. Conditionally immortalized retinal capillary endothelial cell lines (TR-iBRB) expressing differentiated endothelial cell functions derived from a transgenic rat. Exp Eye Res 2001;72:163–172 [DOI] [PubMed] [Google Scholar]
- 37. Müller SL, Portwich M, Schmidt A, Utepbergenov DI, Huber O, Blasig IE, Krause G. The tight junction protein occludin and the adherens junction protein alpha-catenin share a common interaction mechanism with ZO-1. J Biol Chem 2005;280:3747–3756 [DOI] [PubMed] [Google Scholar]
- 38. Joussen AM, Murata T, Tsujikawa A, Kirchhof B, Bursell SE, Adamis AP. Leukocyte-mediated endothelial cell injury and death in the diabetic retina. Am J Pathol 2001;158:147–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Joussen AM, Poulaki V, Le ML, Koizumi K, Esser C, Janicki H, Schraermeyer U, Kociok N, Fauser S, Kirchhof B, Kern TS, Adamis AP. A central role for inflammation in the pathogenesis of diabetic retinopathy. Faseb J 2004;18:1450–1452 [DOI] [PubMed] [Google Scholar]
- 40. Joussen AM, Poulaki V, Qin W, Kirchhof B, Mitsiades N, Wiegand SJ, Rudge J, Yancopoulos GD, Adamis AP. Retinal vascular endothelial growth factor induces intercellular adhesion molecule-1 and endothelial nitric oxide synthase expression and initiates early diabetic retinal leukocyte adhesion in vivo. Am J Pathol 2002;160:501–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Qaum T, Xu Q, Joussen AM, Clemens MW, Qin W, Miyamoto K, Hassessian H, Wiegand SJ, Rudge J, Yancopoulos GD, Adamis AP. VEGF-initiated blood-retinal barrier breakdown in early diabetes. Invest Ophthalmol Vis Sci 2001;42:2408–2413 [PubMed] [Google Scholar]
- 42. El-Remessy AB, Behzadian MA, Abou-Mohamed G, Franklin T, Caldwell RW, Caldwell RB. Experimental diabetes causes breakdown of the blood-retina barrier by a mechanism involving tyrosine nitration and increases in expression of vascular endothelial growth factor and urokinase plasminogen activator receptor. Am J Pathol 2003;162:1995–2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kowluru RA, Koppolu P, Chakrabarti S, Chen S. Diabetes-induced activation of nuclear transcriptional factor in the retina, and its inhibition by antioxidants. Free Radic Res 2003;37:1169–1180 [DOI] [PubMed] [Google Scholar]
- 44. Carrozzino F, Pugnale P, Féraille E, Montesano R. Inhibition of basal p38 or JNK activity enhances epithelial barrier function through differential modulation of claudin expression. Am J Physiol Cell Physiol 2009;297:C775–787 [DOI] [PubMed] [Google Scholar]
- 45. Shivanna M, Rajashekhar G, Srinivas SP. Barrier dysfunction of the corneal endothelium in response to TNF-alpha: role of p38 MAP kinase. Invest Ophthalmol Vis Sci 2010;51:1575–1582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ma TY, Iwamoto GK, Hoa NT, Akotia V, Pedram A, Boivin MA, Said HM. TNF-alpha-induced increase in intestinal epithelial tight junction permeability requires NF-kappa B activation. Am J Physiol Gastrointest Liver Physiol 2004;286:G367–376 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.