Abstract
Gardner's syndrome is an autosomal dominant disease and is a subtype of familial adenomatous polyposis. It is characterized by adenomatous intestinal polyps, multiple osteomas in the skull, maxillae, mandible, and multiple cutaneous and subcutaneous masses (epidermoids and desmoid). Intestinal polyps, if not treated, have 100% chance of becoming malignant. We report a case of a 25-year-old female patient with Gardner's syndrome, with clinical manifestations including impacted supernumerary teeth, odontomes, sebaceous cyst on the scalp, and osteomas. It is important for the general dental practitioners to be aware of the clinical and radiological characteristics of Gardner's syndrome.
Keywords: Familial intestinal polyposis, gardner's syndrome, impacted teeth, osteoma
INTRODUCTION

In 1951, Eldon J. Gardner (1909 – 1989), a college teacher of genetics, first described the syndrome, as a rare autosomal, dominant, inherited disorder with a high degree of penetrance, characterized by a triad of multiple osteomas, colonic polyposis, and mesenchymal tumors of the skin and soft tissues.[1] It is a variant of the familial adenomatous polyposis syndrome, known to be caused by the mutation in the Adenomatous Polyposis Coli (APC) gene located on chromosome 5q21 (band q21 on chromosome 5).[2]
The incidence of Gardner's syndrome in the general population has been estimated as one in 14,025 live births.[3] Dental anomalies including odontoma and multiple unerupted supernumerary and permanent teeth have been reported.[4] Dental anamolies are seen in 30% of patients with Gardner's syndrome.
Presence of osteomas is required to make the diagnosis of Gardner's syndrome. The mandible is the most common location, however, osteomas may occur in the skull, paranasal sinuses, and the long bones.[5] Classic location of osteomas in mandible is the mandibular angle and inferior surface. Osteomas precede the clinical and radiographic evidence of colonic polyposis or Gardner's syndrome, therefore, may be insightful markers for the disease. It is also proposed that radiography of the jaws may serve as a valuable tool for the early detection of carriers of Gardner's syndrome.
The epidermoid cyst is the most common cutaneous finding in Gardner's syndrome and is present in multiple forms in 50 – 60% of the patients and may occur on the face, extremities, and / or the scalp.[6]
Desmoid tumor is benign fibrous proliferation that occurs under the skin predominantly in the abdominal wall. This tumors has high rate of recurrence after excision. It is seen in 8.6% of cases of Gardner syndrome.
Our patient was a 25-year-old female with a history of multiple swellings in the lower jaw that had developed over a period of 11 years. The swelling was not associated with pain, discharge, or numbness. An extraoral examination revealed gross facial asymmetry, because of a diffuse swelling on the left side of the mandible measuring about 3 cm × 4 cm in size, extending from the parasymphysis to the posterior border of the mandible [Figure 1]. Similar swellings, three in number, were present on the inferior aspect on the right side of the mandible. The skin over the swellings appeared normal. On palpation, all the swellings were bony hard in consistency, non-tender, and were fixed to the mandible.
Figure 1.

Extraoral osteomas. A 25-year-old female patient with diffuse bilateral swellings on the lower third of face along the mandibular border.
Intraoral examination revealed a diffuse swelling, obliterating the right buccal vestibule, measuring about 2 cm × 2 cm in size, and extending from the mesial aspect of tooth 46 to the distal aspect of tooth 48 anteroposteriorly. The overlying mucosa was intact, with no ulceration or sinus discharge. On palpation, all the swellings were bony hard in consistency and non-tender. There were clinically missing teeth 21 and 23 (no history of extraction revealed) and over-retained tooth 63. Other dental findings were a carious tooth 47. Patient had a small swelling measuring about 1 cm × 1 cm on the scalp, which was fluctuant and cystic in nature (epidermoid / sebaceous cyst).
The patient did not have any symptoms of rectal bleeding, cramping abdominal pain, weight loss, diarrhea or small bowel or colonic obstruction, and was reluctant to get a colonoscopy done to rule out the presence of polyps in the intestine, colon, and rectum. The clinical and radiographic findings, of osteomas, odontomes, impacted teeth, and sebaceous cyst suggested a diagnosis of Gardner's syndrome.
Our patient's need was aesthetic improvement, for which the osteomas were surgically excised and sent for histopathological examination. The patient was followed up for one year and has remained asymptomatic, with no relapse of the lesions [Figure 2].
Figure 2.

Postoperative radiograph after removal of osteomas, impacted teeth, and implant placement, with respect to tooth 21.
RADIOLOGICAL FEATURES
The patient underwent maxillary and mandibular cross-sectional occlusal radiograph, orthopantomograph (OPG), and posteroanterior radiograph [Figure 3]. The OPG revealed impacted teeth 21 and 23 and homogenous radiopaque masses over the right and left inferior aspect of the mandible, suggestive of osteomas [Figure 4]. Also, multiple small, homogeneous radiopaque masses surrounded by a radiolucent halo could be seen throughout the maxilla and mandible, suggestive of complex odontomes. Diffuse sclerotic masses were present throughout the body of the mandible giving it a mottled appearance. Impacted teeth 21 and 23 and the complex odontomes in the near vicinity were better visualized in the maxillary cross-sectional occlusal radiograph [Figure 5].
Figure 3.

Posteroanterior radiograph shows extra-oral osteomas along the mandible (white arrows).
Figure 4.
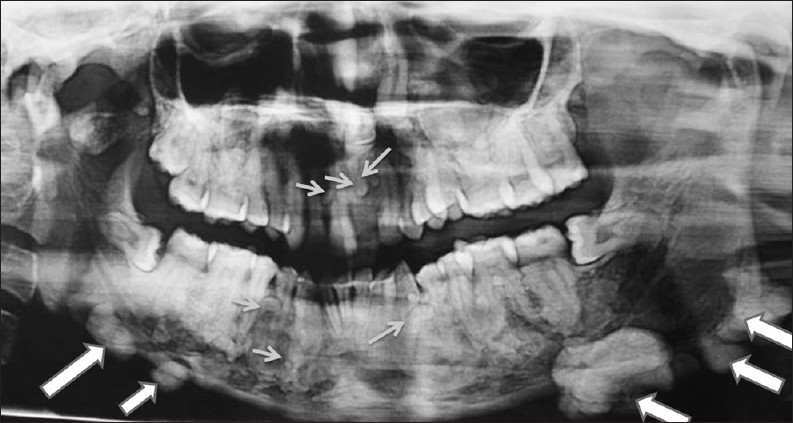
OPG demonstrates impacted teeth 21 and 23, homogenous radiopaque masses over the right and left inferior aspect of the mandible suggestive of osteomas (large arrows). Also multiple small, homogeneous radiopaque masses surrounded by a radiolucent halo could be seen throughout the maxilla and mandible suggestive of complex odontomes (small arrows).Diffuse sclerotic masses are present throughout the body of mandible giving it a mottled appearance
Figure 5.
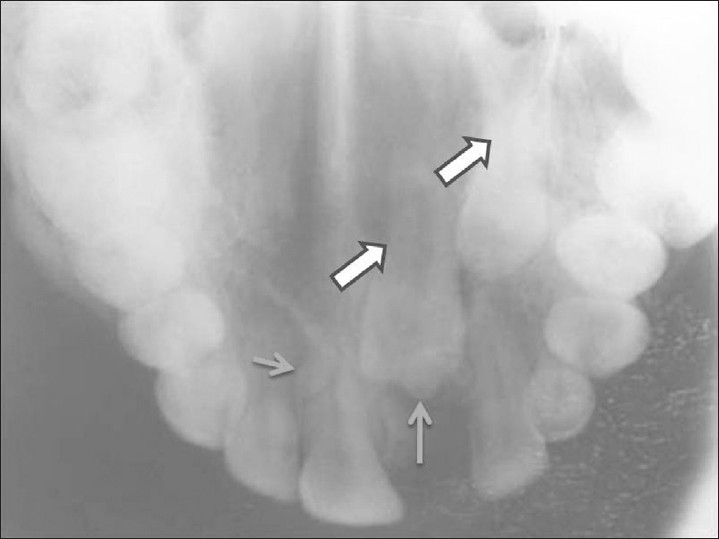
Maxillary occlusal radiograph shows impacted teeth 21, 23 (large arrows) and odontomes (small arrows) in the near vicinity.
PATHOLOGICAL FEATURES
The histopathological report revealed the presence of compact lamellar bone with a haversian canal, lacunae, histiocytes, and reversal and resting lines suggestive of osteoma [Figure 6].
Figure 6.
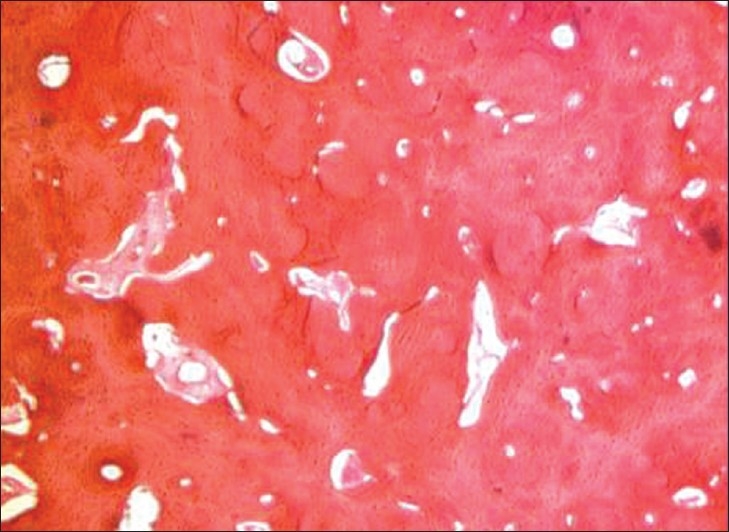
Photomicrograph shows the presence of compact lamellar bone with haversian canal, lacunae, histiocytes and reversal and resting lines suggestive of osteoma. (Hematoxylin-Eosin stain 10×).
DISCUSSION
Gardner's syndrome is a disease that affects multiple systems. It is an autosomal dominant condition with an incidence between 1 in 8300 and 1 in 14,025 live births, affecting both genders equally, with a uniform worldwide distribution.[7] Symptoms are usually present by the end of the second decade of life, but they may present anytime between two months and 70 years. As the clinical and radiological features in the maxillofacial region, such as osteomas, skin cysts, atypical skin pigmentation, and abnormal dental findings or radiographical lesions can precede frequent asymptomatic intestinal polyps for many years, dental practitioners and radiologists should be familiar with the manifestations of this syndrome.
Unlike most patients with Gardner's syndrome who present with gastrointestinal symptoms such as bloody diarrhea and pain in the abdomen, our patient presented with dental and facial cosmetic issues. Our case showed the classical clinical features associated with the syndrome: Multiple osteomas and odontomes, epidermoid cyst, and impacted teeth.
Skeletal abnormalities appear in approximately 90% of the patients with Gardner's syndrome, and osteoma is considered to be the most common.[8] Supernumerary teeth, compound odontomes, and / or impacted teeth are seen in 30% of the patients with this disease.
The gastrointestinal manifestations of Gardner's syndrome include colonic adenomatous polyps (tubular, villous, tubulovillous), gastric and small intestinal adenomatous polyps (12% of the patients), and periampullary carcinomas (2% of the patients).[9] In our patient there were no gastrointestinal symtoms and she had refused colonoscopy.
Patients may also suffer from congenital hypertrophy of the retinal pigment epithelium,[7] although the finding was absent in our case.
Panoramic radiography by the dentist can be useful for early detection of Gardner's syndrome, because the components of this entity, like osteoma, odontoma, supernumerary, and impacted teeth, can be detected. However, panoramic radiography is of limited value in the evaluation, localization, and extension of the tumor mass, considering the superimposition of the bony structures and the two-dimensional image.[10]
The maxillofacial features of the syndrome can appear many years before the intestinal polyposis.[10] Therefore, dental professionals should be familiar with the significance of the syndrome as a pre-cancerous condition. Dental management includes removal of the impacted teeth, cysts of the jaw or face, as well as, resection of osteomas for functional or cosmetic reasons. Tooth extraction can be difficult because of generalized increased alveolar bone density and complete absence of periodontal space caused by hypercementosis.[7]
CONCLUSION
Osteomas of the skull, angle of the mandible and its inferior surface are classic bony features, in addition to intestinal ployps, in patients with Gardner syndrome. A practicing dental surgeon should be aware of this entity in which intestinal polyps have 100% chance of malignant transformation.
ACKNOWLEDGEMENT
The authors would like to thank Dr Zameera Naik for her contribution to this manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/65/92187.
REFERENCES
- 1.Gardner EJ. “A genetic and clinical study of intestinal polyposis, a predisposing factor for carcinoma of the colon and rectum”. Am J Hum Genet. 1951;3:167–76. [PMC free article] [PubMed] [Google Scholar]
- 2.Gu GL, Wang SL, Wei XM, Bai L. Diagnosis and treatment of Gardner's syndrome with gastric polyposis: A case report and review of literature. World J Gastroenterol. 2008;14:2121–3. doi: 10.3748/wjg.14.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lyons LA, Lewis RA, Strong LC, Zuckerbrod S, Ferrell RE. A Genetic study of Gardner syndrome and Congenital Hypertrophy of the Retinal Pigment Epithelium. Am J Hum Genet. 1988;42:290–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Davies AS. Gardner's syndrome: A case report. Br J Oral Surg. 1970;8:51–7. doi: 10.1016/s0007-117x(70)80068-3. [DOI] [PubMed] [Google Scholar]
- 5.Gorlin RJ, Pindborg JJ, Cohen MM. Syndromes of the Head and Neck. 2nd ed. New York: McGraw-Hill; 1976. pp. 324–8. [Google Scholar]
- 6.Ascari-Raccagni A, Baldari U, Righini MG. Cutaneous symptoms of Gardner's syndrome. J Eur Acad Dermatol Venereol. 1999;12:80–1. doi: 10.1111/j.1468-3083.1999.tb00824.x. [DOI] [PubMed] [Google Scholar]
- 7.Kamel SG, Kau CH, Wong ME, Kennedy JW, English JD. The role of Cone beam CT in the evaluation and management of a family with Gardners syndrome. J Craniomaxillofac Surg. 2009;37:461–8. doi: 10.1016/j.jcms.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Lew D, DeWitt A, Hicks RJ, Cavalcanti MG. Osteomas of the condyle associated with Gardner's syndrome causing limited mandibular movement. J Oral Maxillofac Surg. 1999;57:1004–9. doi: 10.1016/s0278-2391(99)90026-5. [DOI] [PubMed] [Google Scholar]
- 9.Fotiadis CV, Tsekouras DK, Antonakis P, Sfiniadakis J, Genetzakis M, Zografos GC. Gardner's syndrome: A case report and review of the literature. World J Gastroenterol. 2005;11:5408–11. doi: 10.3748/wjg.v11.i34.5408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fonseca LC, Kodama NK, Nunes FC, Maciel PH, Fonseca FA, Roitberg M, et al. Radiographic assessment of Gardners syndrome. Dentomaxillofac Radiol. 2007;36:121–4. doi: 10.1259/dmfr/18554322. [DOI] [PubMed] [Google Scholar]


