Abstract
Purpose
To examine daily- and event-level associations of substance use with occurrence of sex and condom nonuse among depressed youth.
Methods
Depressed, sexually active outpatients age 15–22 reported alcohol use, marijuana use, and sex on a personal digital assistant for 2 weeks. If they reported sex, participants indicated partner type and condom use. Data were analyzed for participants who reported both substance use and sex events (N=39) using generalized estimating equations. Daily-level models compared the likelihood of sex and of condom nonuse between days on which participants did or did not use substances. Event-level models examined the likelihood of sex in the 2, 6, and 12 hours following substance use and the likelihood of condom nonuse if substances were used in the preceding 2, 6, and 12 hours.
Results
Participants reported 307 sex events (180 unprotected) and 391 substance use events on 572 days. Substance use was associated with increased odds of sex on the same day, but not after adjusting for weekend. Depressed youth were less likely to have sex within 2 hours following substance use and more likely to have sex within 12 hours after marijuana use. There was no main effect of substance use on condom nonuse; however, there was a significant interaction such that on weekdays, condom nonuse was less likely when substances were used within 6 hours before sex.
Conclusions
The findings from this small, predominantly female sample suggest that contextual factors, not intoxication, influence associations of substance use with sexual behavior in depressed youth.
Keywords: Substance use, sexual intercourse, condom use, unprotected sex, adolescent, young adult, event-level, momentary sampling
Introduction
Substance use has been linked to sexual behavior in adolescents and young adults. Young people who use substances are more likely to have had sexual intercourse (sex) and those who have had sex are more likely to use substances [1, 2]. Similarly, substance use and condom non-use co-occur in youth. Hypothesized reasons for these associations include lifestyle clustering of behaviors [3] and event-specific effects of substances on sexual decision-making [4, 5]. For example, the alcohol myopia model postulates that intoxication decreases ability to attend to distal cues for a behavior (e.g., knowledge about and motivation to reduce risk) and increases focus on proximal cues (e.g., sensory input and physiological arousal associated with a potential partner) [4, 5]. To be plausible, substance use would have to occur close enough to sex for the individual to be intoxicated [6, 7]. However, observations of co-variation in behaviors can be confounded by individual, relationship, and situational characteristics (e.g., personality trait, partner type, or relationship duration) [8].
Diary and timeline follow-back calendar studies have examined substance use and sex on the same day [9], or report of substance use at the time of [10, 11], before [7, 12–14], or proximal to [15] sex. Although some studies have found global associations [16, 17], most within-participant analyses have suggested that unprotected sex does not follow substance use [7, 10, 16, 17]. In college students, drinking before sex was associated with a lower likelihood of condom use when positive mood was increased [14]. However, analyses did not adjust for other potentially confounding contextual information (e.g., both behaviors may be more likely on the weekend, when positive mood is higher [18]).
Another relevant factor is the nature of the sexual partnership [8, 12, 19]. One study of male college students found that drinking preceded unprotected sex only with casual partners [12]. In another study of college students, drinking before sex was not related to condom use overall, but women who drank before sex with a casual partner were more likely to use a condom than women who did not drink [7]. The findings suggest that individuals may follow their usual patterns of behavior regardless of intoxication (i.e., drinking is related to sex with casual partners, with whom condom use is more likely) [10]. At least one event-level study found that women were more likely to have sex with a new acquaintance when the encounter involved alcohol than when it did not [20].
Most event-level studies have examined alcohol [7, 12, 20], but not cannabis or other drugs. One study of 16- to 24-year olds found no association between cannabis use and condom nonuse with a new partner over the previous two years [21]. However, few sexual events were preceded by cannabis use. Further, the long recall period may have biased reporting, especially among individuals who used cannabis heavily [22]. Because cannabis is the most frequently used illicit drug among U.S. youth [23], studies should specifically examine cannabis in relation to sexual behavior.
Although event-level methodology improves investigation of causal associations between substance use and sexual behavior, it is not without limitations. When participants are asked to record substance use in relation to a sexual event, they may alter their behaviors or reporting of their behaviors. Behavioral data may be biased by both recall duration and behavior frequency [24]. Further, most studies do not collect precise information about the timing of behavioral events. Substance use shortly before sex may influence decisions about whether to have sex or use a condom. However, substance use preceding sex by several hours may affect social decision-making (e.g., whether to go to a party). Investigating these relationships requires analyses of event data ordered in time over intervals of varying lengths.
Momentary sampling methods can address many limitations of other methodologies [25]. Individuals use portable electronic devices to report shortly after behaviors, minimizing recall bias and missing data [26]. Reports may be prompted by signal, thereby not relying on the participant to remember to make a report. Participants have multiple opportunities to report the same phenomenon, reducing the likelihood that they will not report it. Participants can report the time of events, allowing them to be ordered and for the time between events to be examined. By assessing multiple events, momentary sampling can obtain a more representative sample of behavior than with recall of one specific event (e.g., last sex). Data on multiple sex events/person allows for within-individual analyses of sex with and without antecedent substance use, thereby controlling for individual characteristics [27]. Momentary sampling permits report of specific event information (e.g., partner type) that may be difficult to recall reliably. Within-participant analyses can then determine how associations vary across these event-specific characteristics, as well as across days [28]. Momentary sampling can assess behaviors without linking them (i.e., without asking whether substances were used before sex [29]), minimizing the possibility that participants change what they are or report doing because they become aware of connections between their behaviors or ascertain study objectives [27].
Event-level associations between substance use and sexual behaviors are of particular interest among depressed youth, who report high levels of both substance- [30] and sex-related risk behavior [31], including substance use before sex [6]. Research elucidating possible causal links between these behaviors may help to explain increased rates of sexually transmitted infections (STIs) in this population [32]. Using momentary sampling, we examined associations between substance use and two sexual behaviors (having sex and not using a condom) in a sample of depressed adolescents and young adults, addressing the following questions:
Substance use and sex
-
1)
Are depressed young people more likely to have sex on a day on which they use substances than on non-substance-using days?
-
2)
Are they more likely to have sex after using substances?
Substance use and condom nonuse
-
3)
When depressed young people have sex, are they more likely to not use a condom on a day on which they use substances than on non-substance-using days?
-
4)
When they have sex, are they more likely to not use a condom after using substances?
We accounted for potential moderating factors (weekend day, partner type), and analyzed alcohol and marijuana separately as well as together.
Method
Participants
Depressed outpatients of two adolescent medicine clinics, a psychiatric clinic, and a young parents’ program of a children’s hospital were recruited if they were 15–22 and reported sex at least once/week and clinically significant depressive symptoms (Beck Depression Inventory-II [33] score ≥ 16). Patients self-referred or were referred by their medical or mental health provider, then completed a screening audio computer-assisted self-interview (ACASI). Institutional review board approval was obtained with a waiver of parental consent for participants under 18. Fifty-four young people enrolled; 52 (96%) collected momentary data (one had technical problems, one did not make any reports). Of these, 39 (75%) reported sex and substance use each at least once during the study, and comprised the analytic sample. One participant’s event data did not have valid times and were excluded from the event-level analyses.
Procedure
Participants collected data for two weeks using a personal digital assistant (PDA). The PDA signaled participants 4–6 times/day at random during their waking hours, except when they anticipated not being able to respond (median number of signals/participant, 68, an average of 4.8 signals/day).1 When signaled, participants answered questions on alcohol and marijuana use and sex events since the previous signal (median signal response rate, 82.1%; median number of reports/day, 3.7). Signal response rate was not associated with participant age, gender, or racial/ethnic group; or signal time or day. Participants were also instructed to make a report following sex or substance use. Event date and time were compared with report time- and date-stamp to identify if an event was reported more than once; if so, the report closest to the event time was analyzed.
Measures
On baseline ACASI, participants reported their age (years), gender, and whether they (females) were or a partner (males) was currently pregnant.
On momentary reports, participants indicated if they had sex, and if so, identified partner type (main, new, other; dichotomized as main vs. non-main) and whether a condom was used (condom nonuse; yes, no). Participants reported the date (today, yesterday, or calendar date) and time (to the nearest 15-minute interval) of sex events. Similarly, participants reported if they had used alcohol or marijuana (substance use) and the date and time of use.
Data Analysis
Analyses were performed using SAS 9.2 (Cary, NC). Generalized estimating equations (GEE) with a binary outcome and a logit link function were used to account for within-participant clustering of observations and assumed a compound symmetric covariance structure. Analyses examined alcohol and marijuana together and separately, and explored interactions of substance use with partner type and weekend (one interaction term at a time). Daily-level analyses examined the co-occurrence of substance use and sex behaviors on the same day, without regard to order and according to date (so behaviors close in time but crossing midnight would not be identified as co-occurring). In contrast, event-level analyses examined the behaviors in order, such that substance use preceded sex, and distanced in time by hours (regardless of date).
Substance use and sex
To examine whether days on which depressed youth used substances were more likely to be days on which they had sex, we created daily summaries of events for each participant and tested for associations within the same calendar day. Models adjusted for age, gender, pregnancy status, and weekend day (Friday or Saturday [34]).
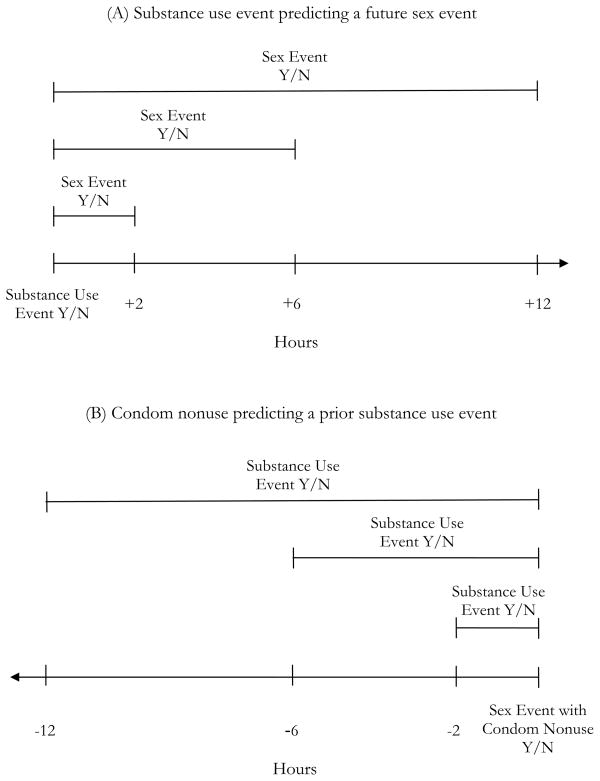
To test associations between substance use and subsequent sex, we created time blocks of 2 hours following each substance use event and compared the odds of a sex event in these blocks to the odds of a sex event in blocks more distant from substance use (Figure 1a). The 2-hour window was consistent with other research [6] inferring the substance’s immediate effects. Similar models examined the likelihood of sex within 6 and 12 hours after a substance use event, more intermediate and distant intervals during which behaviors may occur sequentially owing to individual or contextual factors. The blocks distant from substance use excluded time 2, 6, or 12 hours before substance use (to avoid a reverse association) and varied in length; models adjusted for block duration. Models also adjusted for age, gender, pregnancy status, proportion of reports in a block with a weekend time (3 pm Friday through 11:59 pm Sunday [18]), and proportion of reports in a block made at each of four times of day (12 midnight–5:59 am, 6 am–11:59 am, 12 noon–5:59 pm, 6 pm–11:59 pm).
Figure 1.
Structure of analyses for event-level associations between substance use and sex (A) and between substance use and condom nonuse (B) across 2-, 6-, and 12-hour time intervals.
Substance use and condom nonuse
For days on which sex occurred, we examined associations between using substances and having unprotected sex on the same day. Models adjusted for age, gender, pregnancy, weekend day, and having any sex events with a non-main partner on the day.
To determine whether substance use before sex was associated with condom nonuse, we created windows of 2, 6, and 12 hours before sex events and compared the odds of condom nonuse if substance use had vs. had not occurred (Figure 1b). Each model controlled for age, gender, pregnancy, whether the sex event occurred on a weekend, sex event time of day, and if sex was with a non-main partner.
Results
Descriptive statistics
Participants were severely depressed (median BDI-II score, 30), mostly female (85%) and black (39%) or Hispanic (28%), with a median age of 18. They reported coitarche at a median age of 15, a median of 4 partners in their lifetime, and a median of 3 sex events in the previous week. Nearly one-half (44%) reported multiple partners in the past 3 months, 41% had been treated for an STI, and 67% had used substances before sex. Two male participants had pregnant partners.
Participants reported 307 unique sex events (1–17 events/participant; median, 3.3 events/week/participant). One-half (51%) reported not using a condom with some sex events, 28% did not use a condom with any events, and 21% reported using a condom with each sex. One-third (33%) had sex with a non-main partner at least once. Participants reported 391 unique substance use events; 92% used alcohol (1–17 alcohol events/participant) and 79% used marijuana (1–25 marijuana events/participant).
Participants completed reports on 572 days (96% of days enrolled, on average); 39% of days contained at least one sex event, 38% of which included at least one episode without a condom. Forty-two percent of days contained a report of substance use (22% with alcohol, 27% with marijuana). On 108 days (19%), participants reported both having sex and using substances. Sex, alcohol use, and marijuana use were disproportionately reported on weekend days (33%, 40%, and 34% of events, respectively).
Participants made 2,450 momentary reports. Of the 307 sex events, 59% were unprotected and 17% were with a non-main partner. Of the 391 substance use events, 47% involved alcohol and 63% involved marijuana; 9% included both substances.
Substance use and sex
Daily level
Sex occurred on 45% of days with and 35% of days without substance use (Table 1). In the unadjusted daily-level model, substance use was associated with increased odds of sex on the same day (odds ratio [OR] = 1.44, p = 0.049; Table 2). After controlling for age, gender, pregnancy, and weekend day, this association was no longer significant. The estimate for substance use changed by < 10% when the individual-level covariates were added (β= 0.3677 to β = 0.3431), then by nearly 23% when weekend day was added (to β = 0.2652), suggesting a confounding effect. Similarly, same-day alcohol use was significantly associated with sex in the unadjusted model (OR = 1.50, p = 0.04), but not once the co-variates were included.
Table 1.
Sex on Same Day as and after Substance Use vs. No Substance Use
| Sex | Substance Use | Alcohol Use | Marijuana Use | |||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |
| On same day (a) | 108/241 (45%) | 116/331 (35%) | 61/127 (48%) | 163/445 (37%) | 70/157 (45%) | 154/415 (37%) |
| After (b) | ||||||
| Within 2 h | 18/233 (8%) | 79/244 (32%) | 8/101 (9%) | 52/125 (42%) | 12/149 (8%) | 58/150 (39%) |
| Within 6 h | 49/271 (18%) | 67/182 (37%) | 24/120 (20%) | 49/111 (44%) | 29/174 (17%) | 47/100 (43%) |
| Within 12 h | 92/309 (30%) | 51/114 (45%) | 45/140 (32%) | 39/78 (50%) | 54/197 (27%) | 35/73 (48%) |
Each cell displays the proportion of days with (or without) substance use on which sex occurred.
Each cell displays the proportion of 2-, 6-, or 12-hour blocks of time following substance use (or not following substance use) during which sex occurred.
Table 2.
Daily- and Event-level Associations between Substance Use and Sex
| Daily-level Analyses: Sex on the Same Day as Substance Use* | Event-level Analyses: Sex Occurring After Substance Use** | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | AOR (95% CI) | p | OR (95% CI) | p | AOR (95% CI) | p | ||
| Sex on a substance use day | 1.44 (1.001, 2.08) | 0.049 | 1.30 (0.92, 1.84) | 0.13 | |||||
| Sex on an alcohol use day | 1.50 (1.01, 2.23) | 0.04 | 1.26 (0.85, 1.90) | 0.25 | |||||
| Sex on a marijuana use day | 1.39 (0.90, 2.14) | 0.13 | 1.36 (0.89, 2.09) | 0.16 | |||||
| Substance use event | |||||||||
| Sex within 2 h after substance use | 0.65 (0.30, 1.41) | 0.27 | 0.44 (0.19, 0.99) | 0.048 | |||||
| Sex within 6 h after substance use | 1.30 (0.62, 2.76) | 0.49 | 1.13 (0.48, 2.67) | 0.78 | |||||
| Sex within 12 h after substance use | 1.62 (0.76, 3.49) | 0.21 | 1.70 (0.72, 3.98) | 0.23 | |||||
| Alcohol use event | |||||||||
| Sex within 2 h after alcohol use | 0.66 (0.21, 2.08) | 0.48 | 0.59 (0.17, 2.01) | 0.40 | |||||
| Sex within 6 h after alcohol use | 1.42 (0.47, 4.30) | 0.53 | 0.51 (0.17, 1.56) | 0.24 | |||||
| Sex within 12 h after alcohol use | 2.08 (0.97, 4.47) | 0.06 | 1.96 (0.84, 4.62) | 0.12 | |||||
| Marijuana use event | |||||||||
| Sex within 2 h after marijuana use | 0.79 (0.30, 2.09) | 0.64 | 0.62 (0.23, 1.67) | 0.34 | |||||
| Sex within 6 h after marijuana use | 1.81 (0.71, 4.59) | 0.21 | 2.36 (0.84, 6.66) | 0.10 | |||||
| Sex within 12 h after marijuana use | 3.46 (1.30, 9.22) | 0.01 | 5.11 (1.60, 16.35) | 0.006 | |||||
OR = odd ratio; AOR = adjusted odds ratio; CI = confidence interval.
Models compare the odds of having sex on a substance use day with the odds of having sex on a day without substance use. Adjusted models control for age, gender, pregnancy, weekend day, and sex event with a non-main partner.
Models compare the odds of sex occurring within 2, 6, or 12 hours after substance use with the odds of sex occurring in blocks of time more distant from substance use. Adjusted models control for age, gender, pregnancy, substance use event on a weekend, substance use event time of day, sex event with a non-main partner, and duration of time blocks.
Event level
With increasing block duration, sex was more likely following substance use (unadjusted percentages: 8% of 2-hour blocks, 18% of 6-hour blocks, and 30% of 12-hour blocks; Table 1). However, for the same block duration, the proportion of blocks during which sex occurred was consistently lower following substance use than at other times (32% – 45%). Similar patterns were seen for alcohol and marijuana.
In adjusted event-level analyses, depressed youth were less likely to have sex within 2 hours following substance use, compared to other times (Table 2; adjusted OR [AOR] = 0.44, p = 0.048). Sex was not more or less likely to occur in the 6 or 12 hours following substance use. While none of the adjusted alcohol models was significant, the adjusted odds of sex within 12 hours after marijuana use were more than 5 times the odds of sex at other times (p = 0.006). None of the models exploring interactions with weekend was significant (all ps > 0.28).
Substance use and condom nonuse
Daily level
Condom nonuse was reported on 44% of sex days with and 32% of sex days without substance use (Table 3). Daily-level GEE models showed that participants were not more likely to report condom nonuse on days with vs. without substance use (Table 4). Similarly, condom nonuse was not associated with either alcohol or marijuana use on the same day. Interactions with weekend day and partner type were not significant (all ps > 0.13).
Table 3.
Condom Nonuse on Same Day as and Preceded by Substance Use
| Substance Use | Alcohol Use | Marijuana Use | ||||
|---|---|---|---|---|---|---|
| Condom Nonuse | Yes | No | Yes | No | Yes | No |
| On same day (a) | 47/108 (44%) | 37/116 (32%) | 26/61 (43%) | 58/163 (36%) | 31/70 (44%) | 53/154 (34%) |
| Preceded by (b) | ||||||
| Within 2 h | 20/44 (45%) | 155/247 (63%) | 8/20 (40%) | 167/271 (62%) | 13/28 (46%) | 163/263 (62%) |
| Within 6 h | 35/73 (48%) | 140/218 (64%) | 18/35 (51%) | 157/256 (61%) | 21/45 (47%) | 154/246 (63%) |
| Within 12 h | 50/97 (52%) | 125/194 (64%) | 27/52 (52%) | 148/239 (62%) | 36/63 (57%) | 143/228 (63%) |
Each cell displays, for days on which sex occurred, the proportion of days with (or without) substance use on which condom nonuse occurred.
Each cell displays the proportion of sex events with (or without) substance use in preceding 2, 6, or 12 hours that were unprotected.
Table 4.
Daily- and Event-level Associations between Substance Use and Condom Nonuse
| Daily-level Analyses: Condom Nonuse on the Same Day as Substance Use* | Event-level Analyses: Condom Nonuse After Substance Use** | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | AOR (95% CI) | p | OR (95% CI) | p | AOR (95% CI) | p | ||
| Condom nonuse on a substance use day | 0.90 (0.66, 1.23) | 0.52 | 0.83 (0.55, 1.25) | 0.37 | |||||
| Condom nonuse on an alcohol use day | 1.12 (0.74, 1.70) | 0.60 | 1.00 (0.58, 1.74) | 0.99 | |||||
| Condom nonuse on a marijuana use day | 0.83 (0.61, 1.14) | 0.24 | 0.83 (0.55, 1.24) | 0.36 | |||||
| Substance use event | |||||||||
| Condom nonuse within 2 h after substance use | 0.65 (0.33, 1.30) | 0.23 | 0.58 (0.29, 1.17) | 0.13 | |||||
| Condom nonuse within 6 h after substance use | 0.67 (0.43, 1.07) | 0.09 | 0.66 (0.37, 1.18) | 0.16 | |||||
| Condom nonuse within 12 h after substance use | 0.94 (0.66, 1.32) | 0.71 | 0.83 (0.52, 1.33) | 0.43 | |||||
| Alcohol use event | |||||||||
| Condom nonuse within 2 h after alcohol use | 0.62 (0.24, 1.63) | 0.33 | 0.60 (0.24, 1.50) | 0.27 | |||||
| Condom nonuse within 6 h after alcohol use | 0.76 (0.46, 1.25) | 0.28 | 0.81 (0.45, 1.43) | 0.46 | |||||
| Condom nonuse within 12 h after alcohol use | 1.01 (0.61, 1.69) | 0.96 | 0.91 (0.49, 1.68) | 0.76 | |||||
| Marijuana use event | |||||||||
| Condom nonuse within 2 h after marijuana use | 0.63 (0.28, 1.45) | 0.28 | 0.58 (0.19, 1.72) | 0.32 | |||||
| Condom nonuse within 6 h after marijuana use | 0.71 (0.36, 1.39) | 0.32 | 0.71 (0.31, 1.66) | 0.43 | |||||
| Condom nonuse within 12 h after marijuana use | 0.90 (0.56, 1.44) | 0.66 | 0.83 (0.44, 1.56) | 0.55 | |||||
OR = odd ratio; AOR = adjusted odds ratio; CI = confidence interval.
Models compare the odds of condom nonuse if sex occurred on a substance use day with the odds of condom nonuse if sex occurred on a day without substance use. Adjusted models control for age, gender, pregnancy, sex event with a nonmain partner, and weekend day.
Models compare the odds of condom nonuse within 2, 6, or 12 hours after substance use with the odds of condom nonuse within 2, 6, or 12 hours after no substance use. Adjusted models control for age, gender, pregnancy, sex event on a weekend day, time of day of sex event, sex event with a nonmain partner, and duration of time blocks.
Event level
Approximately one-half (45%–52%) of sex events preceded by substance use were unprotected, whereas almost two-thirds (63%–64%) of sex events without antecedent substance use were unprotected (unadjusted percentages; Table 3). None of the main-effects models showed an association between substance use before sex and condom nonuse (Table 4). However, the interaction between substance use within 6 hours before sex and weekend was significant. On weekdays, the odds of not using a condom when substances were used within the previous 6 hours were 0.45 times the odds when substances were not used (p = 0.037); there was no difference in condom nonuse according to substance use on the weekend (AOR = 1.29, p = 0.45). Interactions between substance use and partner type were not significant (all ps > 0.10).
Discussion
This study supports the view that in depressed young people substance use is linked to sexual behavior in a contextually-dependent manner, but not owing to a causal relationship. Sex and substance use were likely to co-occur within a day, but the association was no longer significant after accounting for weekend. As in previous research with adolescents [18, 34, 35], study youth were more likely both to have sex and to use substances on the weekend, when out of school or work and engaged in leisure activities.
When we considered timing of sex in relation to substance use, sex was less, not more likely to occur within 2 hours of substance use, contrary to intoxication-based theories [4, 36]. Study youth were in predominantly main partnerships and may have preferentially had sex when not intoxicated. Additionally, depressed individuals may use substances following certain affective states (e.g., high positive and/or negative affect [37]) and have sex after others (e.g., low positive affect [38]).
In other research [6], high-risk young couples with at least one depressed member were more likely than nondepressed couples to report using alcohol or marijuana before sex when recalling their behaviors over 60 days. Studies that compare behaviors between people may detect differences in individual characteristics (e.g., psychological symptoms or dispositional make-up), whereas studies that compare behaviors between situations, within participants, may detect differences in environment, relationships, and intoxication that can better inform theories about causality [8]. Future research into psychological and social contexts of substance use (e.g., using when more vs. less depressed, using alone vs. with an intimate partner vs. with others) would aid in understanding the associations with sexual behavior, as will more research on the partners [6].
In contrast to the findings for the 2-hour window, sex was more likely within 12 hours after marijuana use. The association strengthened once time of day and weekend were included, supporting to the concept of behavioral patterns being embedded in a socioenvironmental context. This may be especially true for marijuana, which is used across a wider range of times and situations than alcohol [35]. It is less plausible that intoxication from marijuana directly increases the likelihood of sex within 12 hours of use; serum concentrations of cannabinoids decrease substantially by 6 hours after smoking marijuana [39]. Participants may have used marijuana over several hours, but varied in how they reported event time, limiting precision of the time window. We did not examine amount used or self-perceived intoxication, which may influence sexual decision-making and behavior [15].
Consistent with most previous diary and event-level research [10, 19, 21], in general we did not observe an association between substance use and condom nonuse either on the same day or when the events were temporally ordered. However, depressed youth were less likely to have unprotected sex if they had used substances within the past 6 hours on a weekday. There may be differences in nature of substance use and/or sex (independent of partner type, which was in the models) according to when in the week the behaviors occur. Depressed youth may use less substance during the week vs. the weekend, impairing less their ability to engage in protected sex. Depending on the day of the week, they may use substances for different reasons, in different social settings, and with different people in ways that can influence the likelihood of not using a condom. Similarly, after using substances, they may have sex under different conditions on weekdays vs. weekend (e.g., weekday sex may be more likely at home where condoms are more readily available). On the weekend, positive mood is higher [18], which has been associated with condom nonuse following alcohol use [14].
We did not find evidence for a relationship between substance use and condom nonuse with a casual or new partner, in contrast to some event-level studies [12, 20]. In our sample, relatively few sex events occurred outside of a main partnership, so we may have not had the power to detect small or medium effects. Further, the small sample (especially of males) did not permit examination of potential differences by gender [6] or other individual-level characteristics. Additionally, the findings may be influenced by selection bias.
This study improved on previous event-level research by locating substance use and sexual events in time and analyzing links between events over varying time intervals to better assess the plausibility of intoxication hypotheses. Future research should determine dose and duration of substance use. This study also evaluated alcohol and marijuana events separately, consistent with research indicating substance-related differences in the temporal and social context of use [35]. Using computer-based reporting, collecting data in near-real time, and assessing substance use and sexual events independently minimized recall and responding biases [26, 27, 40]. As with most behavioral research, this study was limited by the validity and reliability of self-report. Additionally, the findings for heterosexually active youth may not generalize to those in same-sex partnerships.
Disentangling the causal, co-varying, and sequential relationships between substance use and sexual behavior in depressed youth has implications for interventions to reduce risk in this already-vulnerable population. Our research suggests that it is important to acknowledge differential patterns of risk according to contextual factors and help these young people to consider event-specific conditions in developing individualized strategies for reducing risk. Messages that focus solely on reducing unsafe sex as a result of intoxication will fail to recognize how the likelihood of sex and condom use may be higher or lower after using substances, depending on whether use occurs on the weekend and what substance is used.
Acknowledgments
We gratefully acknowledge Henry A. Feldman, PhD for his guidance on data analysis, Lisa E. Sunner, MPH for her assistance in data management, the clinical staff at the recruitment sites for their efforts in participant enrollment and data collection, and the young people who contributed data for the purposes of this research.
This study was funded by grant R21MH72533 (Shrier) from the National Institute of Mental Health, National Institutes of Health and a grant (Shrier) from the Aerosmith Endowment Fund for Prevention and Treatment of AIDS and HIV Infections, Children’s Hospital Boston.
Footnotes
The PDA was programmed to emit one signal at random within each 3-hour block during each participant’s self-identified waking hours, no closer than 30 minutes apart. Therefore, a participant who was awake from 7 am to 10 pm would be signaled five times, a participant who was awake from 9 am to 2 am would be signaled six times, and a participant who was awake from 9 am to 9 pm would be signaled four times. Additionally, the PDA was programmed not to emit a signal at times when participants indicated that they would be unable to respond (e.g., on Sunday from 10 am to 11 am while at church).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lydia A. Shrier, Division of Adolescent/Young Adult Medicine, Children’s Hospital Boston, and Department of Pediatrics, Harvard Medical School, Boston, Massachusetts.
Courtney Walls, Clinical Research Program, Children’s Hospital Boston, Boston, Massachusetts.
Christopher Lops, Division of Adolescent/Young Adult Medicine, Children’s Hospital Boston, Boston, Massachusetts.
Ashley D. Kendall, Division of Adolescent/Young Adult Medicine, Children’s Hospital Boston, Boston, Massachusetts.
Emily A. Blood, Clinical Research Program, Children’s Hospital Boston, and Department of Pediatrics, Harvard Medical School, Boston, Massachusetts.
References
- 1.Santelli JS, Robin L, Brener ND, et al. Timing of alcohol and other drug use and sexual risk behaviors among unmarried adolescents and young adults. Fam Plann Perspect. 2001;33:200–205. [PubMed] [Google Scholar]
- 2.Tapert SF, Aarons GA, Sedlar GR, et al. Adolescent substance use and sexual risk-taking behavior. J Adolesc Health. 2001;28:181–189. doi: 10.1016/s1054-139x(00)00169-5. [DOI] [PubMed] [Google Scholar]
- 3.Jessor R, Jessor S. Problem Behavior and Psychosocial Development: A Longitudinal Study of Youth. New York: Academic; 1977. [Google Scholar]
- 4.Steele CM, Josephs RA. Alcohol myopia. Its prized and dangerous effects. Am Psychol. 1990;45:921–933. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- 5.Ebel-Lam AP, MacDonald TK, Zanna MP, et al. An experimental investigation of the interactive effects of alcohol and sexual arousal on intentions to have unprotected sex. Basic Appl Soc Psych. 2009;31:226–233. [Google Scholar]
- 6.Shrier LA, Aneja P, Rice PA, et al. Depression and STI risk within young, Chlamydia-infected, heterosexual dyads. J Adolesc Health. 2009;45:63–69. doi: 10.1016/j.jadohealth.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Leigh BC, Vanslyke JG, Hoppe MJ, et al. Drinking and condom use: results from an event-based daily diary. AIDS Behav. 2008;12:104–112. doi: 10.1007/s10461-007-9216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Halpern-Felsher BL, Millstein SG, Ellen JM. Relationship of alcohol use and risky sexual behavior: a review and analysis of findings. J Adolesc Health. 1996;19:331–336. doi: 10.1016/S1054-139X(96)00024-9. [DOI] [PubMed] [Google Scholar]
- 9.Hensel DJ, Fortenberry JD, Orr DP. Variations in coital and noncoital sexual repertoire among adolescent women. J Adolesc Health. 2008;42:170–176. doi: 10.1016/j.jadohealth.2007.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fortenberry JD, Orr DP, Katz BP, et al. Sex under the influence. A diary self-report study of substance use and sexual behavior among adolescent women. Sex Transm Dis. 1997;24:313–319. doi: 10.1097/00007435-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Bryan A, Rocheleau CA, Robbins RN, et al. Condom use among high-risk adolescents: testing the influence of alcohol use on the relationship of cognitive correlates of behavior. Health Psychol. 2005;24:133–142. doi: 10.1037/0278-6133.24.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.LaBrie J, Earleywine M, Schiffman J, et al. Effects of alcohol, expectancies, and partner type on condom use in college males: event-level analyses. J Sex Res. 2005;42:259–266. doi: 10.1080/00224490509552280. [DOI] [PubMed] [Google Scholar]
- 13.Bailey SL, Gao W, Clark DB. Diary study of substance use and unsafe sex among adolescents with substance use disorders. J Adolesc Health. 2006;38:297, e213–220. doi: 10.1016/j.jadohealth.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 14.Schroder KE, Johnson CJ, Wiebe JS. An event-level analysis of condom use as a function of mood, alcohol use, and safer sex negotiations. Arch Sex Behav. 2009;38:283–289. doi: 10.1007/s10508-007-9278-9. [DOI] [PubMed] [Google Scholar]
- 15.Kiene SM, Barta WD, Tennen H, et al. Alcohol, helping young adults to have unprotected sex with casual partners: findings from a daily diary study of alcohol use and sexual behavior. J Adolesc Health. 2009;44:73–80. doi: 10.1016/j.jadohealth.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leigh BC. Alcohol consumption and sexual activity as reported with a diary technique. J Abnorm Psychol. 1993;102:490–493. doi: 10.1037//0021-843x.102.3.490. [DOI] [PubMed] [Google Scholar]
- 17.Weinhardt LS, Carey MP, Carey KB, et al. The relation of alcohol use to HIV-risk sexual behavior among adults with a severe and persistent mental illness. J Consult Clin Psychol. 2001;69:77–84. doi: 10.1037//0022-006x.69.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larson R, Richards M. Waiting for the weekend: Friday and Saturday night as the emotional climax of the week. New Dir Child Adolesc Dev. 1998 Winter;:37–51. [PubMed] [Google Scholar]
- 19.Leigh BC. Alcohol and condom use: a meta-analysis of event-level studies. Sex Transm Dis. 2002;29:476–482. doi: 10.1097/00007435-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Testa M, Collins RL. Alcohol and risky sexual behavior: Event-based analyses among a sample of high-risk women. Psychol Addict Behav. 1997;11:190–201. [Google Scholar]
- 21.Brodbeck J, Matter M, Moggi F. Association between cannabis use and sexual risk behavior among young heterosexual adults. AIDS Behav. 2006;10:599–605. doi: 10.1007/s10461-006-9103-9. [DOI] [PubMed] [Google Scholar]
- 22.Deahl M. Cannabis and memory loss. Brit J Addict. 1991;86:249–252. doi: 10.1111/j.1360-0443.1991.tb01776.x. [DOI] [PubMed] [Google Scholar]
- 23.Office of Applied Studies. Technical Appendices and Selected Data Tables. II. Rockville, MD: SAMSHA; 2002. National Household Survey on Drug Abuse. Report No.: NHSDA Series H-18. DHHS Pub. No. (SMA) 02-3759. [Google Scholar]
- 24.Jaccard J, McDonald R, Wan CK, et al. Recalling sexual partners: the accuracy of self-reports. J Health Psychol. 2004;9:699–712. doi: 10.1177/1359105304045354. [DOI] [PubMed] [Google Scholar]
- 25.Shiffman S. Real-Time Self-Report of Momentary States in the Natural Environment: Computerized Ecological Momentary Assessment. Mahwah, NJ: Lawrence Erlbaum; 2000. [Google Scholar]
- 26.Stone AA, Shiffman S. Capturing momentary, self-report data: A proposal for reporting guidelines. Ann Behav Med. 2002;24:236–243. doi: 10.1207/S15324796ABM2403_09. [DOI] [PubMed] [Google Scholar]
- 27.Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res. 2000;11:125–157. [PMC free article] [PubMed] [Google Scholar]
- 28.Kiene SM, Tennen H, Armeli S. Today I’ll use a condom, but who knows about tomorrow: a daily process study of variability in predictors of condom use. Health Psychol. 2008;27:463–472. doi: 10.1037/0278-6133.27.4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bryan A, Ray LA, Cooper ML. Alcohol use and protective sexual behaviors among high-risk adolescents. J Stud Alcohol Drugs. 2007;68:327–335. doi: 10.15288/jsad.2007.68.327. [DOI] [PubMed] [Google Scholar]
- 30.Rao U, Daley SE, Hammen C. Relationship between depression and substance use disorders in adolescent women during the transition to adulthood. J Am Acad Child Adolesc Psychiatry. 2000;39:215–222. doi: 10.1097/00004583-200002000-00022. [DOI] [PubMed] [Google Scholar]
- 31.Ramrakha S, Caspi A, Dickson N, et al. Psychiatric disorders and risky sexual behaviour in young adulthood: cross sectional study in birth cohort. Brit Med J. 2000;321:263–266. doi: 10.1136/bmj.321.7256.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shrier LA, Harris SK, Beardslee WR. Temporal associations between depressive symptoms and self-reported sexually transmitted disease among adolescents. Arch Pediatr Adolesc Med. 2002;156:599–606. doi: 10.1001/archpedi.156.6.599. [DOI] [PubMed] [Google Scholar]
- 33.Beck A, Steer R, Brown G. BDI-II Manual. San Antonio: The Psychological Corporation, Harcourt Brace & Company; 1996. [Google Scholar]
- 34.Fortenberry JD, Orr DP, Zimet GD, et al. Weekly and seasonal variation in sexual behaviors among adolescent women with sexually transmitted diseases. J Adolesc Health. 1997;20:420–425. doi: 10.1016/S1054-139X(96)00275-3. [DOI] [PubMed] [Google Scholar]
- 35.Larson R, Csikszentmihalyi M, Freeman M. Alcohol and marijuana use in adolescents’ daily lives: a random sample of experiences. Int J Addict. 1984;19:367–381. doi: 10.3109/10826088409057188. [DOI] [PubMed] [Google Scholar]
- 36.Apostolopoulos Y, Sonmez S, Yu CH. HIV-risk behaviours of American spring break vacationers: a case of situational disinhibition? Int J STD AIDS. 2002;13:733–743. doi: 10.1258/095646202320753673. [DOI] [PubMed] [Google Scholar]
- 37.Armeli S, Tennen H, Affleck G, et al. Does affect mediate the association between daily events and alcohol use? J Stud Alcohol. 2000;61:862–871. doi: 10.15288/jsa.2000.61.862. [DOI] [PubMed] [Google Scholar]
- 38.Shrier LA, Feldman HA, Black SK, et al. Momentary affective states preceding sexual intercourse in depressed adolescents and young adults. Arch Sex Behav. doi: 10.1007/s10508-011-9787-4. Under review. [DOI] [PubMed] [Google Scholar]
- 39.Kauert GF, Ramaekers JG, Schneider E, et al. Pharmacokinetic properties of delta9-tetrahydrocannabinol in serum and oral fluid. J Anal Toxicol. 2007;31:288–293. doi: 10.1093/jat/31.5.288. [DOI] [PubMed] [Google Scholar]
- 40.Turner CF, Ku L, Rogers SM, et al. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]