Abstract
Purpose
To assess the long-term impact of HIV-prevention interventions delivered to youth before sexual initiation and the effects of interventions delivered in non-study settings.
Methods
A five-group comparison of HIV knowledge, and condom-use skills, self-efficacy, intentions and practice among 1997 grade 10 youth attending one of the eight government high schools in Nassau, The Bahamas. Group 1 received an HIV-prevention intervention, Focus on youth in the Caribbean (FOYC), in Grade 6 as part of a randomized trial; Group 2 received FOYC as part of the regular school curriculum but outside of the trial; Group 3 received the control condition as part of the trial; Group 4 received the control condition as part of the school curriculum but outside of the trial; and, Group 5 (Naïve Controls) were not enrolled in a school receiving FOYC or the control and did not participate in the trial.
Results
FOYC youth compared to control youth and Naive Controls had higher HIV knowledge, condom-use skills and self-efficacy four years later. By subgroups, Group 1 demonstrated higher HIV/AIDS knowledge than all groups except Group 2, higher condom skills than all groups, and higher condom self-efficacy than Naïve Controls. Youth in Group 2 demonstrated higher HIV knowledge than youth in Groups 3 to 5. Behavioral effects were not found.
Conclusions
FOYC delivered to grade 6 students continued to have protective effects four years later. Positive effects are present among youth who received FOYC as part of the school curriculum but were not enrolled in the trial.
Keywords: HIV Prevention, pre-adolescents, long-term follow-up, testing effect
INTRODUCTION
Delivering effective HIV prevention education to adolescents prior to their involvement in risky sex is an accepted HIV reduction strategy 1, 2. However, the long-term impact of messages delivered to preteen youth prior to sexual initiation remains uncertain 3, 4. Unanswered are several questions of public health importance. Will messages heard by youth at the onset of adolescence when abstract reasoning is not fully developed, when they have not completed puberty, and/or when they have had limited experience with sexual arousal be understood? Will messages heard under such circumstances be remembered and influence attitudes and behavior later in adolescence? 3,5-7 A small number of intervention studies with follow-up periods beyond two years conducted among pre- and early-adolescents have been published; while selected enduring effects have been reported in some studies, evidence is limited in this important research area 4,7-8.
An expectation in the field of intervention research is that some of the interventions found to be effective will be implemented in expanded settings 9. Consistent with this expectation is the presumption that the intervention effects observed in the trial setting reflect what would be expected in the broader community; an intervention found in a trial setting to have a moderate effect size would be expected to have an equivalent impact in a similar, non-experimental setting. However, there are challenges to this presumption. Conducting multiple assessments, which are necessary to determine program impact over time, may enhance apparent intervention effects10. Enhancements that were possible in a classroom setting in the context of an intervention evaluation may have greatly contributed to the success of the school-based curriculum (i.e., follow-up phone calls to the parents to remind them about aspects of the intervention). Future implementers seeking to reduce costs and/or logistical complications would not know what aspects of the intervention were critical to the success thereof, raising significant questions about fidelity of intervention delivery in subsequent iterations of the intervention11, 12. A related uncertainty is whether intervention responses of youth who agree to participate in a randomized trial of an intervention can be generalized to a wider population. Specifically, are the results from youth who voluntarily enrolled in a trial applicable to youth who were exposed to the intervention not by choice (e.g., did not enroll in a program) but in other more generalized conditions (e.g., part of the school curriculum)?13
Through the intersection of two longitudinal studies conducted among youth residing in Nassau, The Bahamas, we are able to evaluate the long-term impact of HIV reduction efforts delivered to preteen youth and explore the equivalence of responses obtained from youth who participated in a randomized trial of the HIV reduction efforts compared to those from youth who were exposed to the intervention in the classroom but not enrolled in the trial.
METHODS
Setting
With 3.3% of adults infected, The Bahamas has the second highest annual incidence of HIV/AIDS in the Caribbean; over half of infections occur among individuals 15 years to 34 years old, who represent < 20% of the population14. In response, the Bahamian Ministry of Health (MOH) and Ministry of Education (MOE) have partnered to develop a school-based approach to HIV prevention efforts. These efforts, the first targeting grade 6 students and the second grade 10 students, were designed to be assessed by randomized, controlled trials, as described below.
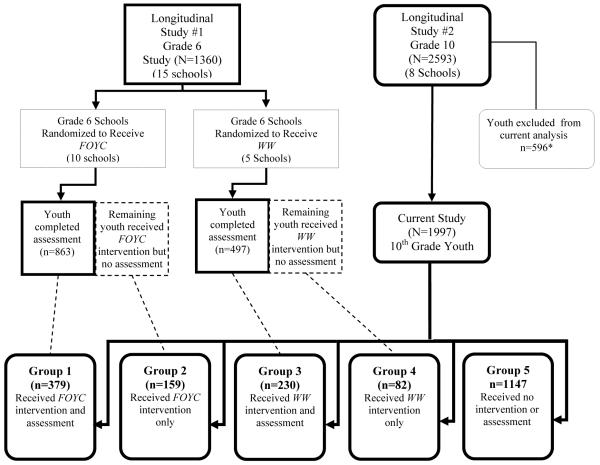
Longitudinal Study#1, grade 6 intervention evaluation (see Figure 1)
Figure 1.
Flowchart of the Study Design and Intersection of Longitudinal Studies #1 and #2
*Youth with uncertain exposure status to FOYC or WW as they were in a FOYC or WW school the year after the intervention was delivered to that school; thus some teachers may have continued to teach some or all of the curricula
Focus on Youth in the Caribbean (FOYC), a 10-session program plus two booster sessions (delivered in grades 7 and 8) and a brief one session parent intervention, was evaluated through a randomized, controlled trial among grade 6 students. Based on a social cognitive model, Protection Motivation Theory 15, FOYC is highly interactive and includes discussions, risk avoidance strategies, communication and negotiation strategies and skills, HIV-related knowledge, and condom-use skills as well as games and exercises to reinforce main messages, and a fictional family story to contextualize decision-making16. The control condition for adolescents was a ten-session ecological intervention, “The Wondrous Wetlands” (WW) and a brief one session parent intervention. (FOYC, WW, the FOYC boosters and the parent ancillary interventions are described in detail in references 4, 16, 17.) FOYC was evaluated through a randomized trial conducted among grade 6 youth from 15 of the 26 government elementary schools located on the island of New Providence, The Bahamas. Neither FOYC nor WW was offered at the remaining 11 schools; the 15 participating school had been selected on the basis of geographic distribution and the level of interest and willingness of the administrators to accept randomization and include either the WW or FOYC into the grade 6 curriculum. Parents and youth in the 15 participating schools were presented the option to enroll in the evaluation; it was explained that all students would receive the curriculum but only assenting/consenting youth-parent dyads would participate in the evaluation. Approximately two-thirds of the students in grade 6 in the participating schools returned assent/consent forms before the desired sample size was reached and enrollment was terminated. Subsequently, enrolled students completed baseline measures, after which randomization was conducted at the level of the school. The FOYC curriculum was delivered to all of the students attending grade 6 in the 10 schools randomized to FOYC, (and the WW curriculum was delivered to all students in the five schools randomized to WW) regardless of whether a student was or was not enrolled in the evaluation of the interventions. Parents of youth enrolled in the study (but not parents of non-enrolled youth) received a brief parent intervention (focusing on parental monitoring in five schools and career-planning in the remaining five schools); in addition, youth enrolled in the evaluation who attended one of the FOYC schools (but not youth in these schools who were not enrolled in the trial) received a brief (one hour) booster session in grade 7 and grade 8. The Bahamian Youth Health Risk Behavioral Inventory (BYHRBI)16, 18, a questionnaire assessing HIV knowledge and condom-use skills, self-efficacy, intentions and self-reported behaviors was administered to youth enrolled in the study (but not to non-enrolled youth) at baseline and at five follow-up assessments (6, 12, 18, 24 and 36 months post intervention).
FOYC was demonstrated through the randomized controlled study to be effective in increasing HIV knowledge and condom-use skills, self-efficacy for condom-use, and intentions to use condoms at some or all of the five follow-up assessments conducted from 6 through 36 months post-intervention 4, 16, 17. Self-reported condom-use was significantly increased at 36 months post-intervention among the subset of FOYC youth whose parents had been randomized to receive the parental monitoring intervention 4, 19.
Longitudinal Study #2, grade 10 (see Figure 1)
A randomized, controlled evaluation of an HIV-prevention intervention targeting older adolescents is being conducted among youth attending grade 10 in all eight of the government high schools in New Providence, The Bahamas. The youth intervention is an age-appropriate form of FOYC; several of the exercises and games were changed to reflect the older age of the participants (e.g., in exercises presenting scenarios, the ages of the participants were changed as were the types of activities in which they were engaged). The control condition is the current standard Bahamian Health and Family Life Curriculum. Because this longitudinal assessment is ongoing and only data obtained at baseline (prior to receipt of the study curricula) are utilized in the present analyses, the intervention and control curricula are not described here.
Among the grade 10 students enrolled in Longitudinal Study #2 (approximately 60% of all grade 10 students), the 1997 students whose data are used in the analyses described below had one of five types of exposures to FOYC in grade 6. Youth in Group 1 received FOYC in grade 6 and were part of the Longitudinal Study #1; thus they received multiple exposures to the questionnaire (at baseline and the five follow-up assessments), received a booster session in grades 7 and 8; and, their parents received a brief intervention. Youth in Group 2 received FOYC as part of the regular school curriculum, but were not part of Longitudinal Study #1 and thus were not tested and received no boosters, and their parents did not receive an intervention. Youth in Group 3 received WW and were part of Longitudinal Study #1 (and thus were tested repeatedly and their parents received a brief intervention) while youth in Group 4 received WW as part of the school curriculum but were not part of Longitudinal Study #1 (and thus were not tested). Youth in Group 5 (“Naïve Controls”) were not enrolled in a school receiving either FOYC or WW and thus did not receive either intervention or testing and were not part of Longitudinal Study #1.
Human Subjects Protection
Grade 6 youth participating in Longitudinal Study #1 and their parents provided written consent and assent as did grade 10 youth participating in Longitudinal Study #2 and their parents. All parents and grade 10 youth participating in Longitudinal Study #2 were asked as part of the consenting process for permission to link data in the grade 10 study to data from the grade 6 study if they had been enrolled in that study. Therefore, for students participating in both studies, data are available from grade 6 and grade 10. For students participating only in Longitudinal Study #2, only their grade 10 data are available. However, because the grade 10 questionnaire asks them to identify the elementary school they attended in grade 6, and we know which schools delivered FOYC, delivered WW or did not deliver either to all of their grade 6 students, we know whether or not each individual youth was exposed to FOYC, to WW, or, to neither. The study protocols and consenting procedures were approved both by the Human Research Protection Boards of Wayne State University and the Princess Margaret Hospital, Ministry of Health, The Bahamas.
Data Sources and Variables
Data used in these analyses were derived from responses to the study questionnaire (i.e., the BYHRBI) at baseline and 36 months follow-up of Longitudinal Study # 1 (“grade 6 study”) and from the baseline of Longitudinal Study #2 (“grade 10 study”). The BYHRBI variables used in these analyses have been described in detail in previous publications4; 18. An 18- item scale including true (e.g. “Anybody can get AIDS”) and false (“What you eat can give you AIDS”) statements was used to assess level of knowledge regarding HIV/AIDS. Correct responses were scored 1 and incorrect 0, resulting in a mean score of 1-18 for each participant based on the number of correct answers. Condom-use skills were assessed using the Condom-use Skills Checklist, a validated scale developed for use when direct observation of actual condom-use would be difficult20 . The scale includes seven correct steps (e.g., Put the condom on the erect penis”) and seven incorrect steps (e.g.,” Put the condom on anytime before you ejaculate”); correct responses were scored “1” and incorrect “0”. Six items (for example “I could put a condom on correctly” and “I could ask for condoms in a store”) were used to assess condom-use self-efficacy; agreement was measured through a five-point Likert scale (1=strongly disagree to 5=strongly agree). Intention to have sex in the next sex months and intention to use a condom if a youth were to have sex were assessed by self-reported likelihood (1=very unlikely to 5=very likely) according to two items. For each of these categories, a mean score was derived using individuals’ responses to the items, with higher scores indicating higher levels of condom-use skills, self-efficacy and behavioral intentions respectively. Adolescents were asked if they had engaged in sexual intercourse in the last six months (one item), and if so, how consistent was their condom usage (never, sometimes, always) (one item).
Statistical Analysis
To ascertain whether youth who had been in Longitudinal Study #1 and enrolled in Longitudinal Study # 2 were comparable with those Longitudinal Study #1 participants who did not enroll in Longitudinal Study #2, we compared basic demographic and relevant characteristics between the two study populations using data from Longitudinal Study #1 assessed at baseline and 36 months, the year prior to the start of Longitudinal Study #2. Student t-test was used to assess continuous variables while chi-square test was used to assess categorical variables.
The longitudinal impact of receipt of FOYC was first assessed by comparing through a three groups comparison the students who received FOYC (Groups 1 and 2) with the WW controls (Groups 3 and 4) and the Naïve Controls (Group 5). To further assess impact of FOYC alone considering repeated exposures to the questionnaire, comparison was made among the five subgroups. A significantly greater effect for Group 1 than for Group 2 was used as evidence supporting the existence of enhanced program effect from repeated testing (as well the intervention enhancements described above). Significant differences between Group 1 and Group 3 and between Group 2 and Group 4 were used as evidence supporting FOYC program effect without the influences of repeated assessment and intervention enhancements. Results from bivariate comparison were verified using the mixed modeling (for continuous variables) and the generalized linear mixed modeling methods to include covariates (e.g., age and gender) as well as to adjust design effect from cluster sampling by schools21. The multivariate analysis was conducted using the SAS procedures PROC MIXED (for mixed effect modeling) and PROC GLIMMIX (for generalized linear mixed modeling). For continuous variables (e.g., HIV/AIDS knowledge and condom-use self-efficacy), Bonferroni corrections were used for pair-wise comparisons. Statistical analyses were conducted using the software SAS v. 9.2 (SAS Institute Inc, Cary, NC).
RESULTS
Table 1 presents the data for the full cohort of youth enrolled in Longitudinal Study #1 and the subset of youth enrolled in both Longitudinal Study #1 and Longitudinal Study #2. As shown in the first four columns of Table 1, the groups were comparable at baseline with respect to all characteristics, with the following exceptions: 1) among WW youth, more males participated only in Longitudinal Study #1 compared to those who participated in both Longitudinal Study #1 and Longitudinal Study #2 (p< .05); 2) WW youth who participated only in Longitudinal Study #1 exhibited higher condom-use skills (p< .05), higher intention to have sex and higher intention to use a condom (p<0.05 for both); and, 3) FOYC youth in Longitudinal Study #1 only exhibited higher condom-use self-efficacy (P<.05). As shown in the next four columns, there were no significant differences at the 36 month follow-up with one exception: WW youth participating only in Longitudinal Study #1 exhibited higher knowledge (p<.05). Thus the subset of youth enrolled in Longitudinal Studies #1 and #2, appear to be generally representative of all youth enrolled in Longitudinal Study #1.
Table 1.
Baseline and 36 month characteristics of youth who enrolled in Longitudinal Studies #1 (Grade 6) and #2 (Grade 10) compared to youth only enrolled in Longitudinal Study #1 by intervention status
| Baseline |
36 Months |
|||||||
|---|---|---|---|---|---|---|---|---|
| Intervention (FOYC) |
Control (WW) |
Intervention (FOYC) |
Control (WW) |
|||||
| In Longitudinal Study # 1 only |
In both Longitudinal Studies # 1 and #2 |
In Longitudinal Study # 1 only |
In both Longitudinal Studies # 1 and #2 |
In Longitudinal Study # 1 only |
In both Longitudinal Studies # 1 and #2 |
In Longitudinal Study # 1 only |
In both Longitudinal Studies # 1 and #2 |
|
|
Sample size, n
Gender |
483 | 379 | 266 | 230 | 348 | 357 | 191 | 211 |
| Males (%) | 232 (48.0) | 179 (48.0) | 137 (51.5)* | 91 (39.6) | 167 (48.0) | 166 (46.5) | 93 (48.7) | 83 (39.3) |
| Age in years (SD) | 10.4 (0.7) | 10.5 (0.8) | 10.4 (0.6) | 10.4 (0.7) | 13.6 (0.8) | 13.6 (0.7) | 13.5 (0.6) | 13.5 (0.6) |
| Knowledge/Skills (SD) | ||||||||
| HIV/AIDS Knowledge | 0.68 (0.13) | 0.68 (0.14) | 0.68 (0.15) | 0.67 (0.15) | 0.90 (0.13) | 0.91 (0.11) | 0.83 (0.15)* | 0.86 (0.13) |
| Condom-Use Skills | 0.55 (0.13) | 0.56 (0.13) | 0.57 (0.15)* | 0.53 (0.13) | 0.66 (0.15) | 0.66 (0.15) | 0.58 (0.14) | 0.56 (0.15) |
| Condom-Use Self-Efficacy | 2.5 (1.2)* | 2.3 (1.2) | 2.3 (1.2) | 2.4 (1.7) | 3.9 (0.9) | 3.7 (0.9) | 3.6 (1.0) | 3.4 (1.0) |
| Sexual Behaviors | ||||||||
| Intention to have sex (SD) | 1.8 (1.2) | 1.8 (1.2) | 1.6 (1.0)* | 1.8 (1.1) | 2.1 (1.5) | 2.3 (1.5) | 2.2 (1.5) | 1.9 (1.4) |
| Intention to use condom (SD) | 3.1 (1.7) | 2.9 (1.7) | 2.9 (1.7)* | 2.6 (1.5) | 4.3 (1.4) | 4.4 (1.2) | 4.1 (1.5) | 4.1 (1.5) |
| Had sex in the last 6 months (%) | 7 (1.5) | 6 (1.6) | 2 (0.8) | 0 (0.0) | 43 (12.4) | 45 (12.3) | 20 (10.5) | 13 (6.2) |
| Condom-use among those who have had sex in the last 6 months (%) |
1 (14.3) | 0 (0.0) | 2 (100.0) | NA | 23 (53.5) | 32 (71.1) | 12 (60.0) | 9 (69.23) |
p < .05;
p < .01
HIV Knowledge and the condom skills checklist were scored 1=correct/0=incorrect; Condom-use self-efficacy scored on a 5-point Likert scale (1= Strongly disagree to 5 = Strongly agree); and Intentions were scored on a 5-point Likertscale (from 1= Very unlikely to 5 = Very likely)
As shown in Table 2, overall the differences in gender composition across all five subgroups were statistically not significantly different (p>0.05); however, in an examination across the three main comparison groups (FOYC, WW and Naïve Controls), significantly more males were present in the FOYC group than in other two groups (p<0.01). A pairwise comparison indicated significantly more males than females in Group 1 (p<0.01), Group 2 (p<0.05), and Group 4 (p<0.05). Therefore, gender was included as a covariate in all comparison analyses for program effect evaluation.
Table 2.
Demographic and means scores of selected measures for ‘Focus on Youth in the Caribbean’ (FOYC), ‘Wondrous Wetlands’ (WW), and Naïve Control students in grade 10 by intervention condition1,2and subgroups3
| Items and Constructs4 | Intervention (FOYC) |
Control (WW) |
Naïve Control |
||||
|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | FOYC Subtotal |
Group 3 | Group 4 | WW Subtotal |
Group 5 | |
|
Sample size, n
Gender |
379 | 159 | 538 | 230 | 82 | 312 | 1147 |
| Males (%) | 178(47.0) | 76(47.8) | 255(47.5) | 89(38.7) | 41(50.0) | 131(41.3) | 476(41.5) |
| Age in years (SD) | 14.5(0.7) | 14.7(0.8) | 14.5(0.7) | 14.4(0.6) | 14.5(0.7) | 14.4(0.6) | 14.5(0.7) |
| Knowledge/Skills (SD) | |||||||
| HIV/AIDS Knowledge | 0.76(0.13) | 0.75(0.14) | 0.76(0.13) | 0.72(0.14) | 0.69(0.14) | 0.71(0.14) 1 | 0.73(0.13) 2 |
| Condom-Use Skills | 0.72(0.14) | 0.66(0.13) | 0.70(0.14) | 0.65(0.14) | 0.65(0.14) | 0.65(0.14) 1 | 0.64(0.13) 2 |
| Condom-Use Self-Efficacy | 3.87(1.08) | 3.66(1.23) | 3.81(1.13) | 3.61(1.00) | 3.70(1.00) | 3.64(1.00) | 3.56(1.10) 2 |
| Sexual Behaviors | |||||||
| Intention to have sex (SD) | 2.49(1.58) | 2.38(1.57) | 2.46(1.58) | 2.20(1.42) | 2.79(1.76) | 2.35(1.53) | 2.31(1.51) |
| Intention to use condom (SD) | 4.27(1.35) | 4.35(1.30) | 4.30(1.34) | 4.14(1.42) | 4.34(1.28) | 4.20(1.39) | 4.21(1.45) |
| Had sex in the last 6 months (%) |
59(15.6) | 19(12.0) | 78(14.7) | 29(12.6) | 15(18.3) | 45(14.2) | 152(13.3) |
| Condom-use among those who have had sex in the last 6 |
40(67.8) | 15(79.0) | 55(70.5) | 20(69.0) | 7(46.7) | 27(61.4) | 104(68.4) |
Group 1: FOYC + enrolled in Longitudinal Study #1; Group 2: FOYC, not enrolled in Longitudinal Study #1; Group 3: WW + enrolled in Longitudinal Study #1; Group 4: WW, not enrolled in Longitudinal Study #1; Group 5: No intervention, not enrolled in Longitudinal Study #1.
Note: Gender and age were used as covariates for all significance testing
Significant differences between FOYC and WW (all p < .01)
Significant differences between FOYC and Naïve Control (all p < .01)
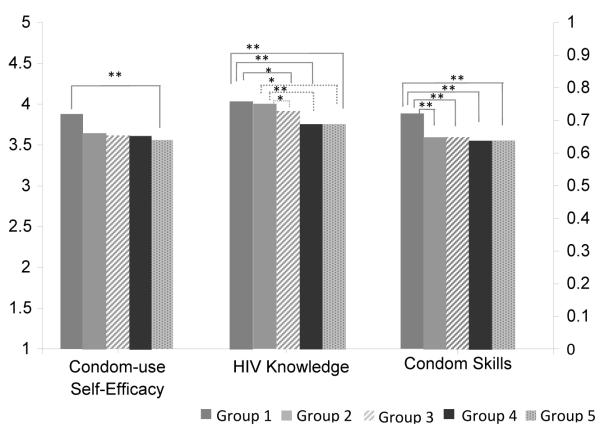
See Figure 2 for significance testing between subgroups
HIV Knowledge and the condom skills checklist were scored 1=correct/0=incorrect; Condom-use self-efficacy scored on a 5-point Likert scale (1 = o, I could not 2 = Probably no, 3 =Don’t know, 4 = Maybe I could, 5 = Yes, I could); and Intentions were scored on a 5-point Likert scale (1 = No, 2= Probably not, 3 = Don’t know, 4 = Maybe, 5 = Yes)
Results from the three group comparison (FOYC, including both Groups 1 and 2; WW, including both Groups 3 and 4; and Naïve Controls, Group 5) indicate that receipt of FOYC significantly increased HIV/AIDS knowledge and condom-use skills compared to both the WW controls and the Naïve Controls. Receipt of FOYC increased condom-use self-efficacy compared to Naïve Controls. No significant differences were observed in intention to have sex ,intention to use a condom, or sexual behaviors.
Figure 2 displays the results from the five group comparison analysis (after controlling for age and gender and the design effect using the mixed modeling method) for the three outcomes in which there were significant differences found between one or more of the groups. Four years after receiving the intervention, youth in Group 1 had significantly higher HIV/AIDS knowledge than youth in Group 3, youth in Group 4 and youth in Group 5 (the Naive Controls). Youth in Group 1 also exhibited significantly greater condom-use skills than youth in all other groups, including youth in Group 2. Group 1 youth scored higher on condom-use self-efficacy compared to Group 5 youth. In addition, youth in Group 2 demonstrated higher knowledge compared all groups of “control” youth (e.g., Groups 3, 4 and 5). HIV knowledge and self-efficacy did not differ between students in Group 1 and Group 2.
Figure 2.
Group comparison showing effect four years post intervention according to grade 6 exposure to FOYC and participation in intervention trial (n=1997)
Note: Gender and age were used as covariates in mixed effect modeling analysis for significance testing.
*p < .05; **p < .01.
Legend: Group 1 consisted of youth who received FOYC and were enrolled in Longitudinal Study #1; Group 2 received FOYC but were not enrolled in Longitudinal Study #1; Group 3 received the control condition WW and were enrolled in Longitudinal Study #1; Group 4 received the control condition WW but were not enrolled in Longitudinal Study # 1; and Group 5 consisted of youth who were not exposed to either FOYC or WW , e.g. were “Naïve Controls” .
DISCUSSION
In these analyses, we assessed the effect of FOYC four years post-intervention, taking advantage of the overlap of subjects in two trials. In addition to assessing sustained program effect, the application of the five group design permitted this study to assess program effect for youth who received FOYC but did not participate in the original trial. Findings of these analyses indicate that an HIV-prevention intervention delivered to pre-adolescent youth in grade 6 had enduring effects on HIV knowledge, condom-use skills and self-efficacy four years later. The results demonstrate that the combination of repeated testing, boosters and a parent intervention were associated with a stronger intervention effect four years later than receipt of FOYC alone. The results also demonstrate that sustained effects are evident with regard to HIV/AIDS knowledge for youth who received FOYC as part of the school curriculum but were not enrolled in Longitudinal Study #1.
Four years post-intervention, neither condom-use intention nor self-reported condom-use was higher among youth exposed to FOYC. In Longitudinal Study #1, condom-use had only been higher at the 36-month follow-up and only among the subset of youth whose parents had been randomly assigned to receive a parental monitoring intervention 4, 19; thus, this absence of a behavioral effect was not unexpected. Condom-use intentions had been significantly higher among youth assigned to FOYC in Longitudinal Study #1, in the 6, 24 and 36 month follow-up assessments 4, 16, 17 and so we had anticipated that at least among Group 1 youth, it might still be significantly higher. The facts that condom-skills and knowledge remain significantly higher indicate a persisting intervention effect. However, the finding that the more meaningful outcomes of condom-use intention and condom-use are not significantly higher suggests the need for an additional intervention focusing more intensely on factors leading to increased intention and use, such as Motivational Interviewing 22.
Potential limitations
First, these data were obtained based on self-report by the youth; however, while the youth may misreport prior involvement in risk and protective behaviors and perceived self-efficacy, knowledge and condom-skills are less subject to such manipulation.
Second, the grade 6 youth in Group 2 (youth attending schools receiving FOYC but not enrolled in the study) did not receive the questionnaire prior to intervention delivery, did not receive the booster sessions in grade 7 or grade 8 and their parents did not receive a parent booster intervention. Thus the differences between Group 1 and Group 2 may result from one or more of these four factors. The five-group design used for this analysis is closely related to the Solomon four-group design that was proposed to address the possible impact on behavior change of completing a questionnaire in intervention studies..23 Typically, the lack of availability of subjects without a pre-test limits the use of this design in intervention research24, 25. While the design employed in the current study was consistent with a Solomon design in that it did permit assessment of youth who were exposed to the intervention but not the questionnaire, as well as those who completed the questionnaire but did not receive FOYC, and those who received neither, it did differ from a Solomon design in that the groups of enrolled and unenrolled youth were not determined through randomization, potentially compromising the comparability of the two groups at baseline. Second, youth who were enrolled in the evaluation and randomized to receive FOYC received intervention enhancements, while youth who were not enrolled in the evaluation did not receive the enhancements.
Third, while these data provide evidence that the enrolled and non-enrolled grade 6 youth both responded to FOYC, the sample allowing us to make this assessment consists of youth who chose to enroll in Longitudinal Study #2. It remains possible that youth who were not enrolled in either Longitudinal Study #1 or #2 (approximately one third of all grade 10 students in New Providence) may not have responded in a similar fashion to FOYC. Further, the observation that at 36 months post-intervention the self-reported condom-use rate was lower among the subset of youth who were only in Longitudinal Study #1 compared to those who enrolled in both studies does suggest a possible selection bias, although these numbers were very low and there were no other indices of risk differences between the two groups.
In conclusion, these findings suggest that some aspects (knowledge and skills) of a successful intervention delivered to pre-adolescents in grade 6 may endure over four years. The findings that youth who were not enrolled in the evaluation but were exposed to the curriculum in the classroom experienced positive effects from the intervention provide some support for the effectiveness of the intervention in a “real life” setting. Future work assessing fidelity of implementation and its relationship to intervention outcomes will be needed.
SUMMARY STATEMENT.
A randomized, controlled trial demonstrated that an HIV prevention intervention delivered to pre-adolescent youth continues to increase protective knowledge, skills, and self-efficacy four years later. Effects regarding knowledge were present among youth who were not enrolled in the trial but received the intervention as part of the school curriculum.
Acknowledgments
Grateful Acknowledgements We thank the National Institute of Mental Health (1 R01 MH069229 and 2 R01 MH069229), the Bahamian Ministry of Education, and the students, parents, teachers, principals and guidance counselors who made this research possible.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.DiClemente RJ, Salazar LF, Crosby RA. A review of STD/HIV preventive interventions for adolescents sustaining effects using an ecological approach. J. Pediatric Psychol. 2007;32:888–906. doi: 10.1093/jpepsy/jsm056. [DOI] [PubMed] [Google Scholar]
- 2.Monarch R, Mahy M. Young people the center of the HIV epidemic. World Health Organ Tech Rep Ser. 2006;938:15–41. [PubMed] [Google Scholar]
- 3.Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet. 2008;372:669–84. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen X, Stanton B, Gomez P, Lunn S, Deveaux L, Brathwaite N, Li X, Marshall S, Cottrell L, Harris C. Effects on condom-use of an HIV prevention programme 36 months postintervention: a cluster randomized controlled trial among Bahamian youth. International Journal of STD & AIDS. 2010;21:622–630. doi: 10.1258/ijsa.2010.010039. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirby D, Obasi A, Laris BA. The effectiveness of sex education and HIV education interventions in schools in developing countries. World Health Organ Tech Rep Ser. 2006;938:103–50. discussion 317-41. [PubMed] [Google Scholar]
- 6.Pedlow MA, Teal C, Carey M. Developmentally-Appropriate Sexual Risk Reduction Interventions for Adolescents: Rationale, Review of Interventions, and Recommendations for Research and Practice. Ann Behav Med. 2004;27(3):172–184. doi: 10.1207/s15324796abm2703_5. NIH Public Access Author Manuscript published. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marlow RM, Kershaw T, Sipsma H, Rosenberg R, Deveaux J. HIV Preventive Interventions for Adolescents: A Look Back and Ahead. Current Medicine Group LLC, Current HIV/AIDS Reports. 2007;4:173–180. doi: 10.1007/s11904-007-0025-6. [DOI] [PubMed] [Google Scholar]
- 8.Doyle AM, Ross DA, Maganja K, Baisley K, Masesa C, Andreasent A, Plummer ML, Obasi Al, Weiss HA, Kapiga S, Watson-Jones D, Changalucha J, Hayes RJ, MEMA kwa Vijana Trial Study Group Long-term biological and behavioral impact of an adolescent sexual health intervention in Tanzania: follow-up survey of the community-based MEMA kwa Vijana Trial. PLoS Med. 2010;7(6):e1000288. doi: 10.1371/journal.pmed.1000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rotherman-Borus MJ, Swendeman D, Chovnick G. The Past, Present, and Future of HIV Prevention: Integrating Behavioral, Biomedical, and Structural Intervention Strategies for the Next Generation of HIV Prevention. Annu Rev Clin Psychol. 2009;5:143–167. doi: 10.1146/annurev.clinpsy.032408.153530. NIH Public Access Published in final edited form as. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huck S, Sandler HM. A note on the Solomon 4-group design: Appropriate statistical analyses. Journal of Experimental Education. 1973;42:54–55. [Google Scholar]
- 11.Stanton B, Kaljee L, Lunn S, Deveaux L, Li X, Chen X, Naar-King S, Harris C, Mathur A, Kamat D. Implementation of effective health innovations and pediatricians, Clinical Pediatrics. (In press) [DOI] [PMC free article] [PubMed]
- 12.Fixsen DL, Naoom SF, Blasé KA, Friedman RM, Wallace F. Implementation Research: A synthesis of the literature. Louis dl la Parte Florida Mental health Institute; Tampa, Florida: 2005. Publication #231. [Google Scholar]
- 13.Rosenthal R, Rosnow RL. The volunteer subject. John Wiley; New York: 1975. [Google Scholar]
- 14.Ministry of Health HIV/AIDS Center . HIV/AIDS. Ministry of Health; Nassau, The Bahamas: 2008. [Google Scholar]
- 15.Rogers RW. Cognitive and physiological processes in fear appeals and attitude change: a revised theory of protection motivation. In: Caaioppi T, Petty RE, editors. Social Psychology. Guilford Press; New York, NY: 1983. pp. 153–176. [Google Scholar]
- 16.Deveaux L, Stanton B, Lunn S, et al. Reduction in human immunodeficiency virus risk among youth in developing countries. Arch Ped and Adolesc Med. 2007;161:1130–9. doi: 10.1001/archpedi.161.12.1130. [DOI] [PubMed] [Google Scholar]
- 17.Gong J, Stanton B, Lunn S, Deveaux L, Li X, Brathwaite NV Marshall, Cottrell L, Harris C, Chen X. Effects through 24 months of an HIV/AIDS prevention intervention program based on protection motivation theory among preadolescents in the Bahamas. Pediatrics. 2009;123:917–28. doi: 10.1542/peds.2008-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stanton B, Li X, Black M, Feigelman S, Ricardo I, Galbraith J, Kaljee L, Nesbit R. Development of a culturally, theoretically and developmentally based survey instrument for assessing risk behaviors among African-American early adolescents living in urban low-income neighborhoods. AIDS Edu Prev. 1995;7:160–77. [PubMed] [Google Scholar]
- 19.Deveaux LC, Lunn S, Bain RM, Gomez P, Kelly T, Brathwaite N, Russell-Rolle G, Li X, Stanton B. Focus on youth in the Caribbean: Beyond the numbers. J International Assoc Physicians in AIDS Care. doi: 10.1177/1545109710397367. Published online 23 March 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stanton B, Deveaux L, Lunn S, Yu S, Braithwaite N, Li X, Cottrell L, Harris C, Clemens R, Marshall S. The condom-use skills checklist (CUSC): a proxy for assessing condom-use knowledge and skills when direct observation is not possible. Journal of Health, Population and Nutrition. 2009;27:406–413. doi: 10.3329/jhpn.v27i3.3383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singer J. Using Proc Mixed to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1978;24(4):325–355. [Google Scholar]
- 22.Naar-King S, Suarez M. Motivational interviewing with adolescents and young adults. Guilford Press; New York: 2011. [Google Scholar]
- 23.Solomon RL. An extension of control group design. Psychological Bulleting. 1949;46:137–150. doi: 10.1037/h0062958. [DOI] [PubMed] [Google Scholar]
- 24.Campbell D, Stanley J. Experimental and quazi-experimental designs for research. Rand McNally; Chicago: 1963. [Google Scholar]
- 25.Walton-Braver MC, Braver SL. Statistical Treatment of the Solomon Four-Group Design: A Meta-Analytic Approach. American Psychological Association, Inc.; Washington, D.C.: 1988. [Google Scholar]