Abstract
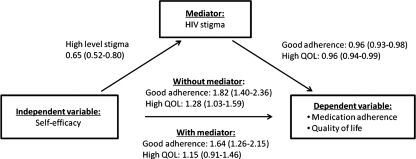
Although the relationship between self-efficacy and health-related behaviors is well known, limited data are available describing the association between self-efficacy and HIV stigma. Specifically, it is not known if the relationship between self-efficacy and health outcomes is mediated by HIV stigma. This study aimed to test these relationships. Data were collected from 202 HIV/AIDS patients in China using questionnaires measuring self-efficacy for disease management, self-reported 7 day medication adherence, perceived HIV/AIDS stigma and quality of life. The total mean score for self-efficacy was 6.73 (range, 2.78–10.0), and the total mean score for HIV stigma was 102.24 (range, 57.0–148.0). Seventy-four percent (150/202) of subjects reported missing no medication doses during past 7 days, and 73% (148/202) subjects reported a quality of life score over 60. There was a moderate level of association between self-efficacy and HIV stigma (Pearson r=-0.43, p=0.000). High self-efficacy predicted better medication adherence (odds ratio [OR]=1.82, 95% confidence interval [CI]=1.40–2.36) and better quality of life (OR=1.28, 95% CI=1.03–1.60) after controlling for demographic and HIV related characteristics. HIV stigma partially mediated the relationship between self-efficacy and medication adherence (OR=1.64, 95% CI=1.26-2.15; Sobel test result Z=1.975, p=0.048). HIV stigma totally mediated the relationship between self-efficacy and quality of life (OR=1.15, 95% CI=0.91–1.46; Sobel test result Z=2.362, p=0.018). The results suggest that, although self-efficacy is an important predictor for medication adherence and quality of life, HIV stigma as a mediator should not be neglected. Health care providers should also evaluate HIV stigma conditions when seeking to improve self-efficacy through interventions.
Introduction
Antiretroviral treatment (ART) has showed great efficacy in viral suppression, immune restoration, mortality reduction, and quality of life enhancement, thereby transforming HIV/AIDS from a fatal condition into a chronic disease.1,2 In China, the national free ART program began in 2003 and was scaled up quickly nationwide.3 Recently, a second line of antiretroviral (ARV) drugs has become available in most area of China. However, to get the optimal benefit of such treatment, patients need to maintain excellent adherence to the regimen. Unfortunately, nonadherence is common among HIV-positive individuals as it is among those with many illnesses. Evidence from Western countries suggests that suboptimal ART adherence occurs among 20% to 40% of patients.4–6 Two recent studies in China showed around 20% suboptimal adherence.7,8 Poor ART adherence leads to rebound of HIV viral load, development of drug-resistant strains of HIV, potentially reducing quality of life.4,9
Factors associated with medication adherence and quality of life have been explored in the past. Among these factors, self-efficacy is both an important predictor for adherence and an influencing factor on quality of life.10,11 Self-efficacy is an important determinant of health behavior, associated with positive quality of life among patients living with chronic illnesses.12,13
The construct of self-efficacy is derived from Bandura's social-cognitive theory, which considers that individuals' perceptions of their own capabilities play a key role in changing their behaviors, motivations and experiences.14 Thus, self-efficacy is generally defined as an individual's confidence in his or her ability to do a specific task or achieve certain outcomes.15 Since self-efficacy is content-specific, the scales measuring self-efficacy in one illness can not be used in another illness. A number instruments measure self-efficacy in the context of HIV/AIDS, including measures of self-efficacy to reduce high HIV risk behaviors,16,17 to disclose HIV status to sexual partner,18,19 to cope with HIV/AIDS,20,21 to improve medication adherence,11 and to manage the chronic disease by oneself.22
A number of reports have revealed close relationships between self-efficacy and specific behaviors. High perceptions of self-efficacy are positively related to reduction in HIV risk behaviors,23 condom use,24 and negotiation for condom use.25 Similarly, adherence self-efficacy predicts adherence behavior over and above any other cognitive processes.26,27 However, there is little evidence that explores the association between disease management self-efficacy and health-related outcomes. It is hypothesized that high sense of disease management self-efficacy leads to better medication adherence and improved quality of life.
HIV-related stigma is another important factor affecting ART adherence and quality of life. HIV stigma is a social process,28 and it is culturally sensitive.28 Thus the content and expression of perceived stigma, enacted stigma and internalized stigma vary across the globe.28,29 Therefore, tools to measure HIV stigma must be culturally sensitive. Accumulating evidence suggests a negative association between HIV stigma and ART adherence,30,31 and a significantly negative impact of stigma upon quality of life for HIV/AIDS patients.32
As discussed above, a body of data supports the hypothesized relationships between pairs of the study variables. However, these variables as a group have not been examined, nor been examined in the Chinese specific context. Our hypothesized model is based on Bandura's social–cognitive theory and Goffman's stigma concept.33 Goffman asserts that stigma reduces the bearer “from a whole and usual person to a tainted, discounted one,” and that this is a social process. During this process, self-efficacy for disease management, such as managing mood and fatigue, communicating with health providers and looking for social support could be affected by internalized stigma and experienced stigma. Thus, based on the theory and empirical findings reviewed above, we hypothesized that: (1) there is a negative relationship between HIV stigma and disease management self-efficacy; (2) good disease management self-efficacy predicts good medication adherence and high quality of life without considering HIV stigma; (3) HIV stigma mediates the relationships between self-efficacy and medication adherence and between self-efficacy and quality of life.
Methods
Study design
This was a cross-sectional descriptive study conducted in Hunan Province, south central China between March and June 2009. Data were collected from 202 HIV/AIDS patients, using structured interviewer-administered questionnaires.
Participants and setting
The target population was HIV/AIDS patients participating in the national free ART program. People were eligible for this study if they met the following criteria: (1) a confirmed diagnosis of HIV infection; (2) age 18 years or older; (3) had received ART for at least 1 month prior to the interview and were continuing their ART at study commencement; and (4) mentally competent to answer questions. The majority of patients in Hunan acquired HIV through injection drug use (31%) or heterosexual contact (52%).
Three HIV/AIDS treatment sites were randomly selected among the 6 HIV/AIDS treatment sites in Hunan Province. The three sites were located in Hengyang, Chenzhou, and Shimen. In Hunan, the free ART program started in 2004 and by October 2008, 1149 patients had received free ART treatment, and 896 patients continued on treatment (Hunan CDC internal statistics).
The treatment sites followed Chinese national standards for ART management, including providing the ART combination therapy (two nucleoside reverse transcriptase inhibitors [NRTIs] plus one non-nucleoside reverse transcriptase inhibitor [NNRTI]). First-line ARV drugs available in the treatment sites included three NRTIs (zidovudine, stavudine, and lamifudine) and two NNRTIs (nevirapine and efavirenz). There were no second-line ARV drugs available at the time of data collection.
Measurement
Demographic information collected included age, gender, place of residence (rural or urban), marital status, educational background, occupation, yearly family income, and items related to HIV status including the length of time since HIV diagnosis, presumed route of HIV infection, recent CD4 counts, and illicit drug use history.
The self-efficacy for HIV disease management questionnaire was used to measure self-efficacy, which has been tested to have good reliability and construct validity.22 There are a total of 34 items within 6 domains, namely managing mood, managing medications, managing symptoms, managing fatigue, communication with health care providers, and getting support. Participants were asked how confident they felt about their ability to perform each specific behavior/goal on a 10-point Likert scale (1=not sure at all, 10=totally sure). The higher the total score, the better self-efficacy they have.
HIV/AIDS related stigma was measured using a culturally sensitive Chinese scale, which was developed by our research group.34 This scale has 34 items with 5 domains (disclosure concerns, public rejection, family stigma, internalized stigma and health care providers' discrimination). Subjects were asked to rate the extent to which they agreed that their personal experiences were mirrored in each statement. Points were assigned as follows: 1 for strongly disagree, 2 for disagree, 3 for unsure/no such experiences, 4 for agree, and 5 for strongly agree. A higher score indicates a stronger sense of feeling stigmatized. The Cronbach α of the scale was 0.90, content validity CVI was 0.88, and the psychometric evaluation results were acceptable.34
Adherence was measured using a translation of the adherence questionnaire from the Community Programs for Clinical Research on AIDS (CPCRA) Antiretroviral Medication Self-Report.35 Patients were asked how many doses had been missed during last seven days. The adherence questionnaire was validated in our previous studies.7
Quality of life was measured using a Chinese scale developed among HIV/AIDS patients in China.36 This is a 41-item scale with 10 factors. Patients were asked to rate how often the statements happened to them during past four weeks on a 5-point Likert scale. The total score was then transformed into a standard 100 point scale, 60 points or greater is indicative of good quality of life. The internal consistency reliability ranged from 0.7 to 0.9.
Data collection
This study was approved by Institutional Review Committee in School of Nursing Central South University. Data were collected when patients came to HIV/AIDS treatment sites to get medications refilled or undergo laboratory testing. Researchers explained the purpose and procedures for the study, and also informed subjects that they had the right to decline to participate. Potential participants were assured that their responses would be kept confidential and that they could withdraw from the study at any time. After obtaining informed consent, the investigator and two research assistants conducted structured face-to-face interviews in a private clinic room. The interviewers were trained to avoid showing judgmental attitudes regarding the subject's medication taking or drug using behaviors. The subject's primary health care provider did not take part in the interview in order to minimize response bias. After the interview, each subject received 20 Renminbi ($3) as compensation for their time.
Data analysis
We first examined the frequencies and distributions of all independent and the two dependent variables (medication adherence and quality of life). We then constructed two separate multiple logistic regression models to estimate the associations between dependent variables and self-efficacy, controlling for demographic and disease-related characteristics. Finally, we examined whether HIV stigma mediated the relationship between self-efficacy and medication adherence and quality of life. Specifically, we first explored the association between self-efficacy and stigma. Next, we examined the association between stigma and each of the dependent variables. If these two associations were significant, then the possibility of mediation existed. In the final step, we examined the extent to which the association between self-efficacy and dependent variables was attenuated by adding stigma to the model using multivariate model analysis. Additionally, the Sobel test was conducted to examine the significance of the mediator effect by using the following formula37:
 |
All the analyses were conducted using SPSS 13.0 (SPSS Inc., Chicago, IL).
Results
Demographic and HIV-related characteristics
Two hundred two participants completed the questionnaires, and another two participants stopped the interviews. The average age of the sample was 39 years with a range of 21 to 78. Most of the participants were of Han ethnicity, and without a religious background. More HIV-positive injection drug users than sexually HIV-infected patients agreed to participate in the study, with the result that 54% of subjects were infected through injecting drug use, 42% through sexual contact, and 4% through improper blood collection practices. The average time since HIV diagnosis was 22 months (range, 1–289; median, 18.5), and 15 months since beginning ART (range, 1–56; median, 12). Other characteristics are shown in Table 1.
Table 1.
Demographic and HIV-Related Characteristics (n=202)
| Characteristics | n (%) |
|---|---|
| Age (years old) | |
| 18∼ | 70 (34.7) |
| 36∼ | 112 (55.4) |
| ≥50 | 20 (9.9) |
| Gender | |
| Male | 144 (71.3) |
| Female | 58 (28.7) |
| Race | |
| Han nation | 196 (97.0) |
| Minorities | 6 (3.0) |
| Marriage | |
| Married/having stable sexual partner | 103 (51.0) |
| Single/divorced/widowed | 99 (49.0) |
| Education background | |
| Illiteracy | 4 (2.0) |
| Primary school | 26 (12.9) |
| Middle school | 107 (53.0) |
| High school/Vocational school | 57 (28.2) |
| College or above | 8 (4.0) |
| Family income per year (RMB) | |
| <5000 | 81 (40.1) |
| 5000∼ | 105 (52.0) |
| ≥20000 | 16 (7.9) |
| Religious background | |
| None | 186 (92.1) |
| Yes | 16 (7.9) |
| Years since HIV diagnosis (yrs) | |
| <1 | 74 (36.6) |
| 1∼ | 92 (45.5) |
| ≥3 | 36 (17.8) |
| Use drug in last 3 months | |
| No | 168 (83.2) |
| Yes | 34 (16.8) |
| CD4 counts ≥200 | |
| No | 94 (46.5) |
| Yes | 108 (53.5) |
Description of self-efficacy, HIV stigma, medication adherence, and quality of life
The total mean score on the self-efficacy scale was 6.73±1.61 (range, 2.78–10.4). The total mean score on the HIV stigma scale was 102.24±16.74 (range, 57.0–148.0). The mean subscale scores of the both scales are shown in Table 2 and Table 3. During past seven days, 150 (74.3%) patients reported 100% adherence, 25 (12.4%) patients missed 1 dose, 20 (9.9%) patients missed 2 doses, 4 (2.0%) patients missed 3 doses, 2 (1%) patients missed 4 doses, and 1 (0.5%) patient missed 14 doses. The total mean score for quality of life was 68.02±12.97 (range, 23.66–96.39). During past 4 weeks, 148 (73.3%) subjects reported score≥60 on the quality of life scale.
Table 2.
Description of Disease Management Self-Efficacy (n=202)
| Items | Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|---|
| Managing mood | 9 | 1.00 | 10.00 | 6.08 | 2.10 |
| Managing medication | 7 | 2.57 | 10.00 | 8.80 | 1.43 |
| Managing symptoms | 5 | 1.00 | 10.00 | 6.16 | 2.27 |
| Communicating with the health care provider | 4 | 1.00 | 10.00 | 7.66 | 2.38 |
| Getting support | 5 | 1.00 | 10.00 | 5.12 | 2.14 |
| Managing fatigue | 4 | 1.25 | 10.00 | 6.65 | 2.55 |
| Total | 34 | 2.78 | 10.00 | 6.73 | 1.61 |
Possible range of each subscale score is 1–10.
SD, standard deviation.
Table 3.
Description of HIV-Related Stigma (n=202)
| Items | Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|---|
| Disclosure concern (score range, 6–30) | 6 | 9 | 30 | 22.98 | 4.88 |
| Public rejection (score range, 6–30) | 6 | 6 | 30 | 18.61 | 4.27 |
| Family stigma (score range, 10–50) | 10 | 10 | 45 | 22.68 | 6.66 |
| Internalized stigma (score range, 6–50) | 10 | 10 | 49 | 32.00 | 7.90 |
| Health care providers' discrimination (score range, 2–10) | 2 | 2 | 10 | 5.97 | 1.80 |
| Total (score range, 34–170) | 34 | 57 | 148 | 102.24 | 16.74 |
SD, standard deviation.
Association between self-efficacy and two dependent variables
Table 4 and Table 5 present the logistic regression models. Patients who perceived a better sense of self-efficacy for disease management reported better medication adherence (OR=1.82, 95% CI=1.40–2.36) and better quality of life (OR=1.28, 95% CI=1.03–1.60) after controlling for demographic and HIV related characteristics.
Table 4.
Mediation Effect of Stigma on Relationship Between Self-Efficacy and Adherence Analyzed by Logistic Regression and Sobel Test
| Regression model | Independent variable | Dependent variable | β | SE | OR (95% CI) |
|---|---|---|---|---|---|
| 1. | Self-efficacy | Adherence | 0.597a | 0.133 | 1.82 (1.34–2.36) |
| 2. | Self-efficacy | Stigma | −0.431a | 0.107 | 0.65 (0.52–0.80) |
| 3. | Stigma | Adherence | −0.034a | 0.015 | 0.96 (0.93–0.98) |
| 4. | Self-efficacy stigma | Adherence | 0.497a | 0.137 | 1.64 (1.26–2.15) |
Sobel test: Z=1.975, p=0.048 (two tails).
p<0.01.
Models controlled for the following variables: age, gender, marriage education, family income, years since HIV diagnosis, drug use in last 3 months, and CD4 counts.
SE, standard error; OR, odds ratio; CI, confidence interval.
Table 5.
Mediation Effect of Stigma on Relationship Between Self-Efficacy and Quality of Life Analyzed by Logistic Regression and Sobel Test
| Regression model | Independent variable | Dependent variable | β | SE | OR (95% CI) |
|---|---|---|---|---|---|
| 1. | Self-efficacy | QOL | 0.244a | 0.111 | 1.28 (1.03–1.59) |
| 2. | Self-efficacy | Stigma | −0.431a | 0.107 | 0.65 (0.52–0.80) |
| 3. | Stigma | QOL | 0.035a | 0.012 | 0.96 (0.94–0.99) |
| 4. | Self-efficacy Stigma | QOL | 0.138 | 0.121 | 1.15 (0.91–1.46) |
Sobel test: Z=2.362, p=0.018 (two tails).
p<0.001.
Models controlled for the following variables: age, gender, marriage education, family income, years since HIV diagnosis, drug use in last 3 months, and CD4 counts.
SE, standard error; OR, odds ratio; CI, confidence interval; QOL, quality of life.
Mediating role of HIV stigma
To examine HIV stigma as a mediator of the relationship between self-efficacy and medication adherence and quality of life, we tested the mediation model presented in Figure 1. The bivariate analysis indicated a moderate relationship between self-efficacy and HIV stigma (Pearson r=−0.43, p=0.000). Logistic regression models showed that HIV stigma was associated with both medication adherence (OR=0.96, 95% CI=0.93–0.98) and quality of life (OR=0.96, 95% CI=0.94–0.99), and also associated with self-efficacy (OR=0.65, 95% CI=0.52–0.80), controlling for covariates. Therefore, conditions for the mediation hypothesis were met.
FIG. 1.
Mediation model of HIV stigma mediating the prediction between self-efficacy and medication adherence and self-efficacy and quality of life.
When HIV stigma was added to the model predicting good medication adherence, better sense of self-efficacy remained significantly associated with good medication adherence (OR=1.64, 95% CI=1.26-2.15), although the Sobel test showed nearly statistically significant result with Z=1.975, p=0.048. So the relationship between self-efficacy and medication adherence was partially mediated. When HIV stigma was added to the model predicting high quality of life, the relationship between self-efficacy and quality of life was no longer statistically significant (OR=1.15, 95% CI=0.91–1.46). The Sobel test confirmed the results, with Z=2.362, p=0.018 (Tables 4 and 5).
Discussion
The level of self-efficacy in this sample of people living with HIV/AIDS in Hunan Province was lower than that reported by others.22 The subscales of managing mood, communicating with health care provider, and getting support, managing fatigue were especially lower. This may reflect Chinese cultural characteristics. China has a family-oriented culture, so that patients mostly turn to the family for support; they rarely are motivated to look for social support beyond the family.38 Second, social workers and psychiatrists are generally not on staff in AIDS clinics in China, so there is little support to help patients manage mood problems. Third, doctors have a relatively high social status, and are a respected authority in the patients' eyes. When a patient visits his or her doctor, they tend not to question doctors' orders. Furthermore, our study showed HIV/AIDS patients reported experiencing discrimination from health care providers (with mean score of 5.97), which are consistent with findings of previous studies in China.39,40 These help to explain the low mean score (7.66) of communicating with health care provider in our study, which is far lower than 9.05 in Shively's study.22
The self-reported medication adherence in this study (About 87% of the sample reported>90% adherence) is a little bit higher than our former study (80% of the sample reported>90% adherence)7 in the almost same population by using the same measurement 3 years later. This might reflect the impact of the multiple research programs and nationwide HIV/AIDS prevention and treatment programs carried out recent years.
In this group, high self-efficacy for disease management was a predictor for good medication adherence after controlling for demographic and HIV related characteristics. This result is similar to other studies.26,27 Importantly, this relationship was partially mediated by HIV stigma. High disease management self-efficacy was also a predictor for improved quality of life, but this predictive relationship was significantly mediated by HIV stigma. The main reason is that self-efficacy was affected by HIV stigma, which has been confirmed by the results. Another explanation might be that the level of HIV stigma among this population is high, consistent with earlier study.41
This study is limited by the lack of measures of potentially important covariates such as social inequality, social support, and mental status. Path analysis or structural equation modeling might be an appropriate next step when considering all these covariates in a larger sample, which should be better represent the characteristics of the total HIV/AIDS patients in Hunan Province or in China.
Nevertheless, the results indicate the importance of assessing self-efficacy for adherence and providing appropriate support when prescribing ARVs. The China CARE free ARV program requires assessment of and education about self-efficacy on three occasions prior to initiation of ART. But this requirement is not rigidly followed in our experiences when collecting data in CARE clinics.
Additionally, the role of stigma must be addressed. Interventions aimed to improve self-efficacy should combine stigma-reduction measures during the preparation period before beginning ART, so as to achieve optimal medication adherence and quality of life. Our findings suggest that, health care providers should also pay attention to patients' psychological needs, and encourage patients to communicate with health care providers. Communication skills training program for Chinese health care providers may be an emerging issue in China, which deserves further study.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Murphy E. Collier ALK. Highly active antiretroviral therapy decreases mortality and morbidity in patients with advanced HIV disease. Ann Intern Med. 2001;135:17–26. doi: 10.7326/0003-4819-135-1-200107030-00005. [DOI] [PubMed] [Google Scholar]
- 2.Rathbun RC. Lockhart SM., JR. Current HIV treatment guidelines—An overview. Curr Pharm Design. 2006;12:1045–1063. doi: 10.2174/138161206776055840. [DOI] [PubMed] [Google Scholar]
- 3.Zhang F. Haberer JE. Wang Y. Zhao Y. The Chinese free antiretroviral treatment program: Challenges and responses. AIDS. 2007;21:143–148. doi: 10.1097/01.aids.0000304710.10036.2b. [DOI] [PubMed] [Google Scholar]
- 4.Chesney M. Ickovics J. Chambers D, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG Adherence Instruments. AIDS Care. 2000;12:255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 5.Aloisi M. Arici C. Balzano R, et al. Behavioral correlates of adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31:145–148. doi: 10.1097/00126334-200212153-00012. [DOI] [PubMed] [Google Scholar]
- 6.Sayles JN. Wong MD. Kinsler JJ. Martins D. Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24:1101–1108. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang H. He G. Li X, et al. Self-reported adherence to antiretroviral treatment among HIV-infected people in central China. AIDS Patient Care STDs. 2008;22:72–80. doi: 10.1089/apc.2007.0047. [DOI] [PubMed] [Google Scholar]
- 8.Wang X. Wu Z. Factors associated with adherence to antiretroviral therapy among HIV/AIDS patients in rural China. AIDS. 2007;21:149–155. doi: 10.1097/01.aids.0000304711.87164.99. [DOI] [PubMed] [Google Scholar]
- 9.Garder E. Sharma S. Peng G, et al. Differential adherence to combination antiretroviral therapy is associated with virological failure with resistance. AIDS. 2008;22:75–82. doi: 10.1097/QAD.0b013e3282f366ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Evangelos CK. Self-efficacy, social support and well-being: The mediating role of optimism. Person Indiv Diff. 2006;40:1281–1290. [Google Scholar]
- 11.Gifford AL. Bormann J. Shively MJ. Wright BC. Richman DD. Predictors of self-reported adherence and plasma HIV concentrations in patients on multidrug antitroviral regimens. J Acquir Immune Defic Syndr. 2000;23:386–395. doi: 10.1097/00126334-200004150-00005. [DOI] [PubMed] [Google Scholar]
- 12.Lavoie KL. Bouchard A. Joseph M. Campbell TS. Favreau H. Bacon SL. Association of asthma self-efficacy to asthma control and quality of life. Ann Behav Med. 2008;36:100–106. doi: 10.1007/s12160-008-9053-8. [DOI] [PubMed] [Google Scholar]
- 13.Motl RW. McAuley E. Doerksen S. Hu L. Morris KS. Preliminary evidence that self-efficacy predicts physical activity in multiple sclerosis. Int J Rehabil Res. 2009;32:260–263. doi: 10.1097/mrr.0b013e328325a5ed. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 15.Bandura A. Social cognitive theory and exercise of control over HIV infection. In: DiClemente R, editor; Peterson J, editor. Preventing AIDS: Theories, Methods, and Behavioral Interventions. New York: Plenum; 1994. pp. 25–60. [Google Scholar]
- 16.Brafford LJ. Beck KH. Development and validation of a condom self-efficacy scale for college students. J AM Coll Health. 1991;39:219–224. doi: 10.1080/07448481.1991.9936238. [DOI] [PubMed] [Google Scholar]
- 17.Bowleg L. Belgrave FZ. Reisen CA. Gender roles, power strategies, and precautionary sexual self-efficacy: Implications for Black and Latina women's HIV/AIDS preventive behaviors. Sex Roles. 2000;42:613–635. [Google Scholar]
- 18.Kalichman SC. Rompa D. DiFonzo K, et al. Initial development of scales to assess self-efficacy for disclosing HIV status and negotiating safer sex in HIV-positive persons. AIDS Behav. 2001;5:291–296. [Google Scholar]
- 19.Parsons JT. Rosof E. Mustanski B. Medication adherence mediate the relationship between adherence self-efficacy and biological assessments of HIV health aming thouse with alcohol use disorders. AIDS Behav. 2008;12:95–103. doi: 10.1007/s10461-007-9241-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharts-Hopko NC. Regan-Kubinski MJ. Lincoln PS. Heverly M. Peoblem-focused coping in HIV-infected mothers in relation to self-efficacy, uncertainty, social support, and psychological distress. Image J Nurs Sch. 1996;28:107–111. doi: 10.1111/j.1547-5069.1996.tb01201.x. [DOI] [PubMed] [Google Scholar]
- 21.Kraaij V. Garnefski N. Schroevers MJ. van der Veek SMC. Witlox R. Maes S. Cognitive coping, goal self-efficacy and personal growth in HIV-infected men who has sex with men. Patient Educ Couns. 2008;72:301–304. doi: 10.1016/j.pec.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 22.Shively M. Smith TL. Bormann J. Gifford AL. Evaluating self-efficacy for HIV disease management skills. AIDS Behav. 2002;6:371–379. [Google Scholar]
- 23.Kang SY. Deren S. Andia J. Colon HM. Robles R. Effects of changes in perceived self-efficacy on HIV risk behaviors over time. Addict Behav. 2004;29:567–574. doi: 10.1016/j.addbeh.2003.08.026. [DOI] [PubMed] [Google Scholar]
- 24.Burns MJ. Dillon FR. AIDS health locus of control, self-efficacy for safer sexual health practices, and future time orientation as predictors of condom use in African American college students. J Black Psychol. 2005;31:172–188. [Google Scholar]
- 25.Lam AG. Barnhart JE. It takes two: The role of partner ethnicity and age characteristics on condom negotiation of heterosexual Chinese and Filipina American college women. AIDS Educ Prev. 2006;18:68–80. doi: 10.1521/aeap.2006.18.1.68. [DOI] [PubMed] [Google Scholar]
- 26.Parsons JT. Rosof EJ. Mustanski B. Patient related factors predicting HIV medication adherence among men and women with alcohol problems. J Health Psychol. 2007;12:357–370. doi: 10.1177/1359105307074298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deschamps AE. De Graeve V. van Wijngaerden E, et al. Prevalence and correlates of non-adherence to antiretroviral therapy in a population of HIV patients using Medication Event Monitoring System. AIDS Patient Care STDs. 2004;18:644–657. doi: 10.1089/apc.2004.18.644. [DOI] [PubMed] [Google Scholar]
- 28.Parker R. Aggleton P. HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Soc Sci Med. 2003;57:13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 29.Ogden J. Nyblade L. Common at its core: HIV-related stigma across contexts: International Center for Research on Women (ICRW) 2005.
- 30.Rintamaki LS. Davis TC. Skripkauskas S. Bennett CL. Wolf MS. Social stigma concerns and HIV medication adherence. AIDS Patient Care STDs. 2006;20:359–368. doi: 10.1089/apc.2006.20.359. [DOI] [PubMed] [Google Scholar]
- 31.Vanable PA. Carey MP. Blair DC. Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS Behav. 2006;10:473–482. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holzemer WL. Human S. Arudo J, et al. Exploring HIV stigma and quality of life for persons living with HIV infection. J Assoc Nurses AIDS Care. 2009;20:161–168. doi: 10.1016/j.jana.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 33.Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, NJ: Prentice-Hall, Inc.; 1963. [Google Scholar]
- 34.Li X. He G. Wang H. Huang L. Liu L. Development and Evaluation of HIV/AIDS-related Stigma and Discrimination Scale. Chin J Nurs. 2010;45:496–499. [Google Scholar]
- 35.Mannheimer SB. Matts J. Telzak E, et al. Quality of life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS Care. 2005;17:10–22. doi: 10.1080/09540120412331305098. [DOI] [PubMed] [Google Scholar]
- 36.Meng Y. The development and assessment on an instrument regarding quality of life for patients living with HIV/AIDS in China[dissertation] Chengdu, Sichuan University. 2007. [PubMed]
- 37.Sobel M. E. Direct and indirect effects in linear structural equation models. In: Long JS, editor. Common Problems/Proper Ssolutions. Beverly Hills, CA: Sage; 1988. pp. 46–64. [Google Scholar]
- 38.Li L. Wu Z. Wu S. Jia M. Lieber E. Lu Y. Impacts of HIV/AIDS stigma on family identity and interactions in China. Fam Syst Health. 2008;26:431–442. doi: 10.1037/1091-7527.26.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cai G. Moji K. Honda S, et al. Inequality and unwillingness to care for people living with HIV/AIDs: A survey of medical professionals in southeast China. AIDS Patient Care STDs. 2007;21:593–601. doi: 10.1089/apc.2006.0162. [DOI] [PubMed] [Google Scholar]
- 40.Zhang SR. Yan H. Li XH, et al. The personal experiences of HIV/AIDS patients in rural areas of western China. AIDS Patient Care STDs. 2010;24:447–453. doi: 10.1089/apc.2009.0347. [DOI] [PubMed] [Google Scholar]
- 41.Li X. Wang H. Williams AB. He G. Stigma reported by people living with HIV in south central China. J Assoc Nurses AIDS Care. 2009;20:22–30. doi: 10.1016/j.jana.2008.09.007. [DOI] [PubMed] [Google Scholar]