Abstract
Background
Psychiatric treatment for children and adolescents with clinically significant aggression is common and often involves the use of antipsychotic medications. Increasingly, pediatricians are initiating or managing such treatments despite limited evidence on optimal diagnostic, psychosocial, and medication approaches for pediatric aggression.
Aims
The objective of this study was to gather clinicians' and researchers' expertise concerning the treatment of maladaptive aggression, using expert consensus survey methods to aid the development of guidelines for pediatricians and psychiatrists on the outpatient treatment of maladaptive aggression in youth (T-MAY).
Methods
Forty-six experts (psychiatrists, pediatricians, and researchers) with >10 years of clinical and/or research experience in the treatment of pediatric aggression completed a 27-item survey (>400 treatment alternatives) about optimal diagnostic, psychosocial, and medication treatments. Data were analyzed using descriptive statistics and confidence intervals.
Results
Expert consensus methodology clearly differentiated optimal versus nonoptimal treatment strategies for maladaptive aggression. In contrast to current practice trends, results indicated that experts support the use of psychosocial interventions and parent education and training before the use of medication for maladaptive aggression at every stage of medication treatment, from diagnosis to maintenance to medication discontinuation.
Conclusion
Overall findings indicate that evidence-informed strategies for outpatient treatment of pediatric maladaptive aggression, guided by systematically derived expert opinions, are attainable. In light of the gap between the research literature and clinical practice, expert consensus opinion supports specific practices for optimal outpatient management in children and adolescents with severe and persistent behavioral difficulties.
Introduction
Psychotropic medications, especially second-generation antipsychotics (SGAs), are often prescribed to children and adolescents with clinically significant aggression and other co-morbid psychiatric conditions (Pappadopulos et al. 2003; Schur et al. 2003; Patel et al. 2005b; RUPP Autism Network 2005; Jensen et al. 2007a; Olfson et al. 2010). Epidemiologic data suggest that nearly one third or greater of antipsychotic prescriptions are associated with visits to nonmental health providers such as pediatricians and nurse practitioners (Cooper et al. 2004). Although pediatricians are often the first to identify and possibly treat disruptive behavior problems, the development of treatment guidelines for pediatric aggression in primary care and psychiatry outpatient settings has been largely neglected.
Although several reviews have examined the role of antipsychotics in the treatment of inpatient aggression and related co-morbid conditions (Schur et al. 2003; Pappadopulos 2006; Findling et al. 2008), significant gaps exist in the availability of published randomized, controlled evidence regarding the efficacy, safety, and long-term use of SGAs in pediatric outpatient populations (Findling et al. 2004; Reyes et al. 2006; Findling et al. 2009; Patel et al. 2005a; Ratzoni et al. 2002), which would provide data applicable to primary care and outpatient psychiatry treatment providers. The lack of consensus on “best practice” approaches in the identification, assessment, and management of clinically significant pediatric aggression may be at the source of high treatment variability—including inappropriate or overprescribing—that may lead to poor outcomes often seen in this population (Jensen et al. 2007b).
In an effort to fill the gaps in the existing literature in terms of accurate assessment, psychosocial interventions, and short- and long-term psychopharmacology, the present study employs a systematic survey used for gathering of expert consensus opinion to provide an effective, data-informed way to identify practices thought to achieve the best outcomes for children and adolescents with clinically significant aggression with a specific focus on the types of cases that could be effectively managed in primary care and psychiatric outpatient settings.
The results of the expert consensus survey reported here were used to inform the development of treatment recommendations for monitoring and managing clinically significant aggression in pediatric primary care and outpatient psychiatry settings (see the Treatment of Maladaptive Aggression in Youth [T-MAY] articles; Pediatrics, in press). These survey data were systematically gathered prior to the consensus conference, as a part of an initiative of the Rutgers Center for Education and Research on Mental Health Therapeutics (CERTs-Mental Health). The survey was believed to be an essential step in guideline development, because members of the T-MAY Steering Committee (SC) recognized that the extant clinical trials literature was sparse and that, in many areas, data concerning optimal medication practices might not be available for many years, if ever. In an effort to consider the risk–benefit ratios of various current clinical practices, SC members (see Appendix) concluded that the final T-MAY consensus recommendations should not remain silent about critical clinical management issues where children's safety and health might be at stake. As a result, the questions developed for the survey were intended to address the apparent wide variation in practices among outpatient prescribers as to what constitutes appropriate prescribing behaviors, focusing particularly in areas where no or insufficient controlled clinical trial data were available.
The resulting survey posed many important clinical questions to survey respondents (who later were conference attendees), to efficiently consolidate expert opinion on common clinical challenges that are not directly answered in clinical trials or the existing literature. Thus, the ultimate goal of the survey was to generate data that might identify outpatient prescribers' optimal decision-making processes, by examining a range of management options that might be suggested in an expert consultation and in reviewing the range of options, to offer clinicians much needed practical guidance on the specific steps for optimal assessment and management of pediatric aggression.
Methods
Study procedures
Phase 1
We conducted interviews with members of the SC, consisting of an expert panel of clinicians and policy makers including child and adolescent psychiatrists, pediatricians, psychologists, and mental health service administrators in the public and private sectors in the states of New York, California, and Texas (see Appendix). Participants were asked to generate key concerns and decision points related to the effective assessment, treatment, and monitoring of aggression in school-age pediatric outpatient populations (∼6–18 years). Responses were used to draft the survey questions and responses.
Phase 2
Using PsycINFO and Medline, we conducted selective literature reviews of the child and adolescent literature on the treatment of aggression, including controlled trials, open-label studies, and case reports across psychosocial and medication treatment (T-MAY CERTs Guidelines for Primary Care and Mental Health Providers, I and II, Knapp et al., in press; Scotto Rosato et al., in revision). Additionally, published articles on the treatment challenges of aggressive youth and their families were also examined to elaborate on policy and service-related issues. These findings also informed the development of the consensus survey.
Phase 3: Survey construction
Drawing upon the information from the first two phases, the SC constructed a consensus survey. The survey was organized to correspond to the different phases of clinical treatment in primary care and psychiatric outpatient settings. These included assessment and diagnosis, psychosocial interventions, medication initiation and treatment management. The survey had 27 items with over 400 treatment options (adapted from Pappadopulos et al. 2003). Survey questions presented clinicians with vignettes depicting various assessment situations and treatment challenges commonly encountered in the treatment of youth with clinically significant aggression.
Phase 4: Survey tool completion
Forty-six of 55 (83.6%) research and clinical experts (i.e., psychiatrists, pediatricians, and psychologists) with significant experience in treating psychiatric disorders in children and adolescents completed the mailed survey on optimal assessment, treatment, and management of clinical aggression in children and adolescent. Data collection was completed in 2007.
Phase 5: Consensus recommendations development
Subjects then participated in a 2-day consensus conference on the development of expert consensus treatment guidelines on the treatment of outpatient pediatric aggression. The survey results were presented at this meeting to generate discussion and formulate an initial draft of the treatment guidelines. Information derived from the survey, consensus conference discussions, and subsequent meetings were incorporated into the final T-MAY recommendations (Knapp et al. and Scotto Rosato et al., in press).
Respondents
The forty-six experts (72% male and 85% MDs) completed the consensus survey on outpatient management of aggressive behavior. The majority of these subjects (94%) participated in the follow-up expert consensus conference that took place in 2007 in Dallas, Texas. Thirty-eight of the 46 had prescribing privileges at the time of the survey, and 8 of these individuals also participated in the development of the survey.
Data analysis
On the expert consensus survey, experts rated possible treatment alternatives on a 9-point Likert scale (Brook et al. 1986; Khan et al. 1997) that contained the following anchor points and descriptors: 9=extremely appropriate: this is your first strategy of choice, or standard of practice; 7–8=usually appropriate: a first-line strategy you would often use; 4–6=equivocal: a second-line strategy you would sometimes use (e.g., depending upon patient/family preference, or if a first-line strategy is ineffective, unavailable, or unsuitable); 2–3=usually inappropriate: a strategy you would rarely use; 1=extremely inappropriate: a strategy you would never use; DK=don't know: use only for items you cannot score because of insufficient knowledge. Survey data were first analyzed by calculating the mean ( ), standard deviation (SD), and confidence interval (CI) for each item. The CI is a statistically calculated range, which indicates a 95% chance that the mean score would fall within that range if the survey were repeated with a similar group of experts. Graphically, the CI is displayed as horizontal bars within a particular rating category. We designated a rating of first, second, or third line for each treatment, based on the category into which the 95% CI of its mean score fell. First-line strategies were those for which the mean response was at or above 6.5 when survey responses were statistically aggregated, indicating that experts felt these strategies were appropriate as the initial treatment for a given situation. A “strategy of choice,” “standard of practice,” or “treatment of choice” (TOC) is an especially strong first-line recommendation that is rated “9” by at least half of the survey participants. The mean response and CI for second-line strategies fell between 3.5 and 6.49, indicating potential choices for patients who fail to tolerate or respond to first-line strategies. They may also be selected as an initial treatment if first-line options are unsuitable for a particular patient. Third-line strategies (CI below 3.5) are typically inappropriate, even contraindicated, or used only when more favorable options have been ineffective.
), standard deviation (SD), and confidence interval (CI) for each item. The CI is a statistically calculated range, which indicates a 95% chance that the mean score would fall within that range if the survey were repeated with a similar group of experts. Graphically, the CI is displayed as horizontal bars within a particular rating category. We designated a rating of first, second, or third line for each treatment, based on the category into which the 95% CI of its mean score fell. First-line strategies were those for which the mean response was at or above 6.5 when survey responses were statistically aggregated, indicating that experts felt these strategies were appropriate as the initial treatment for a given situation. A “strategy of choice,” “standard of practice,” or “treatment of choice” (TOC) is an especially strong first-line recommendation that is rated “9” by at least half of the survey participants. The mean response and CI for second-line strategies fell between 3.5 and 6.49, indicating potential choices for patients who fail to tolerate or respond to first-line strategies. They may also be selected as an initial treatment if first-line options are unsuitable for a particular patient. Third-line strategies (CI below 3.5) are typically inappropriate, even contraindicated, or used only when more favorable options have been ineffective.
Results
Survey
Here, we report the findings for critical issues in the areas of assessment/diagnosis, family engagement and early treatment, psychosocial treatment, and pharmacological management for school-age children aged 6–18 years. For each of these four areas, we present one to two of the questions and all response options for each question in a figure format, the same format in which all findings were reviewed by attendees at the Phase 5 consensus conference, described earlier. Other key findings from these four areas are summarized later in text format. (In view of space limitations, figures and survey results for all 27 questions are available from the corresponding author upon request.) Please note that each of the 27 survey questions required multiple response options, of which none was mutually exclusive. Thus, for any question, respondents might indicate that multiple approaches were strategies of choice, or inappropriate, etc. Therefore, any conclusions about preferences for particular approaches must be considered in the context of all other response options for the particular stem question.
Initial assessment and diagnosis
Necessary assessments
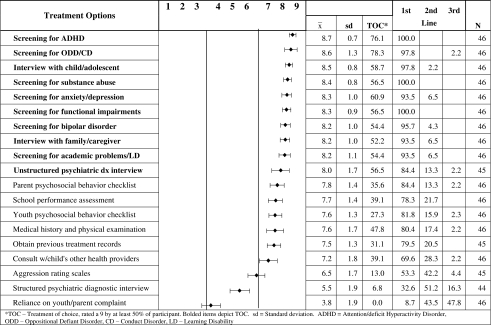
In the area of assessment and diagnoses, Figure 1 illustrates the expert ratings on a comprehensive list of clinical procedures that could be used during the initial evaluation of a child with clinically significant maladaptive aggression. Experts strongly endorsed several methods as part of a general evaluation for a child/adolescent who presents with aggression accompanied by other emotional-behavioral problems, including screening for attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD)/conduct disorder, substance abuse, learning disability, depression, and bipolar disorder, all TOC (i.e., selected as a “9” by >50% of respondents). As seen in Figure 1, multiple other areas were considered “first-line” strategies, whereas use of a structured diagnostic interview was a second-line option and sole reliance on either parent or youth complaints was generally considered inappropriate ( =3.8).
=3.8).
FIG. 1.
Appropriateness of each method as part of a general evaluation for a child/adolescent with aggression accompanied by other emotional-behavioral problems.
Other items that are not usually collected in the clinical evaluation but considered a first-line option by survey responders included the evaluation of parental and child treatment preferences and readiness and parenting skill (i.e., especially the use of harsh and inconsistent punishment and adequacy of child supervision and monitoring) ( range: 8.3 − 8.8). Also important was the consideration of parental burden (
range: 8.3 − 8.8). Also important was the consideration of parental burden ( =7.8, SD 1.3) and psychopathology (
=7.8, SD 1.3) and psychopathology ( =7.8, SD 1.3) as well as the child's quality of life (
=7.8, SD 1.3) as well as the child's quality of life ( =7.8, SD 1.2).
=7.8, SD 1.2).
Use of rating scales
When respondents were given the option of endorsing specific standardized rating scales for the purpose of evaluating and monitoring maladaptive aggression, none of the specific measures was endorsed as a strategy of choice. Except for the clinician-completed Overt Aggression Scale ( =7.3, SD 1.5), all measures considered for use as a first-line approach were more general rating scales such the Connors Teacher and Parent Rating Scale (
=7.3, SD 1.5), all measures considered for use as a first-line approach were more general rating scales such the Connors Teacher and Parent Rating Scale ( =7.6, SD 1.4), Child Behavior Checklist (
=7.6, SD 1.4), Child Behavior Checklist ( =7.4, SD 1.4), and the Clinical Global Impressions Scale (
=7.4, SD 1.4), and the Clinical Global Impressions Scale ( =7.0, SD 1.8). Finally, knowledge about specific scales was quite variable, with many respondents either adding scales to the question or noting that they had never heard of some of the scales.
=7.0, SD 1.8). Finally, knowledge about specific scales was quite variable, with many respondents either adding scales to the question or noting that they had never heard of some of the scales.
Family engagement
Engaging the family in assessment and treatment planning
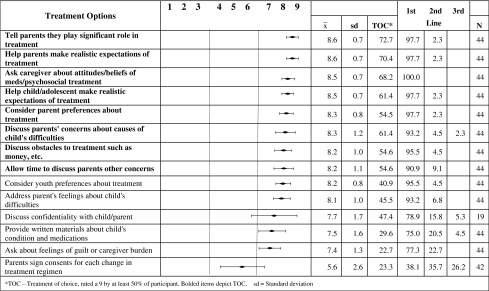
As seen in Figure 2, given the query of how best to enhance parental and child/adolescent engagement in the treatment process, experts endorsed multiple strategies of choice, including telling parents they play a significant role in treatment, helping parents set realistic treatment expectations, discussing family attitudes and beliefs about medication and therapy, considering parent/family preferences, and discussing treatment obstacles. First-line practices related to confidentiality and providing written materials, whereas having parents sign consent before each change to the treatment regimen was the lowest-rated item in the group.
FIG. 2.
Appropriateness of each method for enhancing parental and child/adolescent engagement in the treatment process.
Psychosocial interventions
Optimal psychosocial interventions
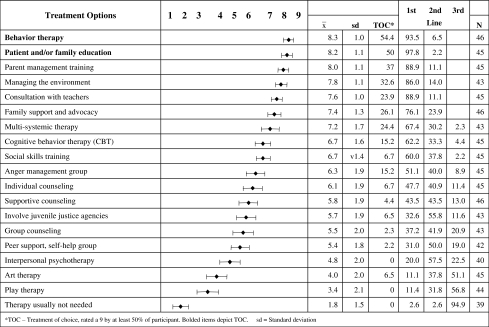
Despite an exhaustive list of possible psychosocial interventions for the treatment of maladaptive aggression, only two items received a strategy of choice rating: behavior therapy and patient/family education (Fig. 3). Some first-line approaches focused on managing the environment, consulting with teachers, and multisystemic therapy. Second-line approaches included individual modalities such as cognitive behavior therapy, supportive therapy, as well as group approaches such as social skills training and anger management. Art therapy and play therapy were seen as third-line choices, and proceeding with treatment without therapy was rated as a nonviable alternative (e.g., CI below 3.5).
FIG. 3.
Rating of how appropriate and essential these psychosocial treatments are for youth with maladaptive aggression.
Pharmacotherapy
Initiation of antipsychotic treatment
Several items were scored as TOC indications for the initiation of antipsychotic medication treatment after unsuccessful behavioral intervention, including attacks others causing serious injury, inflicts major injury on self or suicide attempt, bangs head, cuts, bruises or burns self, and impulsively threatens violent injury (x range: 8.7 − 8.8; see supplemental tables available from the corresponding author).
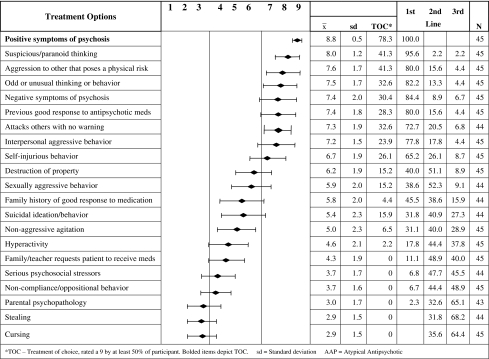
In terms of reasons to initiate antipsychotic pharmacotherapy, clinicians felt that presence of psychotic symptoms was a standard of practice reason (78.3%) for the initiation of antipsychotic medication. Other symptoms of psychosis such as suspicious thinking, odd or unusual behavior, and negative symptoms were also highly rated as first-line reasons for antipsychotic use. In terms of aggressive behavior, serious risk of physical aggression to others or attacks without warning were considered appropriate first-line reasons to initiate antipsychotic treatment when behavioral and environmental interventions have failed. In contrast, relatively minor conduct problems such as stealing and cursing were not viewed as valid reasons to initiate antipsychotic treatment (see Fig. 4).
FIG. 4.
Rating of whether specific clinical symptoms warrant use of an AAP. AAP=atypical antipsychotic.
Selection of medication
According to expert respondents, the strategies of choice representing the standard of care for both mild and moderate to severe aggression were similar; therefore, the means are not presented here (please contact the corresponding author for the complete survey findings). The strategies of choice included establishing the presence of co-occurring symptoms/diagnoses, providing parents with behavior management strategies, and ensuring that the youth and family receive mental healthcare. Simply monitoring symptoms at the next scheduled appointment, starting pharmacotherapy, and making a referral to a crisis/emergency service were deemed second-line considerations (scores 4–6). Not providing for follow-up treatment was considered contraindicated (scores 1–3).
Several questions probed about specific medication selections. For example, in cases where stimulant treatment is ineffective in managing a child with severe aggression and ADHD, experts endorsed atypical antipsychotics ( =7.7, SD 1.5) and mood stabilizers/anticonvulsants (
=7.7, SD 1.5) and mood stabilizers/anticonvulsants ( =6.8, SD 1.6) as first-line approaches. Also, given the scenario that a child/adolescent is not responding to an adequate trial of medication, experts endorsed all but one item as strategies of choice before making any changes to the medication regimen, including ensuring an adequate dose (
=6.8, SD 1.6) as first-line approaches. Also, given the scenario that a child/adolescent is not responding to an adequate trial of medication, experts endorsed all but one item as strategies of choice before making any changes to the medication regimen, including ensuring an adequate dose ( =8.9, SD 0.4) and duration (
=8.9, SD 0.4) and duration ( =8.9, SD 0.4), assessing for compliance problems (
=8.9, SD 0.4), assessing for compliance problems ( =8.9, SD 0.3), and assessing side effects (
=8.9, SD 0.3), and assessing side effects ( =8.5, SD 0.8) and drug interactions (
=8.5, SD 0.8) and drug interactions ( =8.4, SD 0.1), among others.
=8.4, SD 0.1), among others.
Experts supported the use of stimulants ( =6.6, SD 2.3) as a first-line treatment for patients with ODD and conduct problems who continue to present with maladaptive disruptive psychopathology despite an adequate trial of behavior therapy and parent management training. Further, on a different question, experts rated risperidone (
=6.6, SD 2.3) as a first-line treatment for patients with ODD and conduct problems who continue to present with maladaptive disruptive psychopathology despite an adequate trial of behavior therapy and parent management training. Further, on a different question, experts rated risperidone ( =7.9, SD 0.9), lithium (
=7.9, SD 0.9), lithium ( =7.3, SD 1.1), and divalproex/valproic acid (
=7.3, SD 1.1), and divalproex/valproic acid ( =7.2, SD 1.1) as first-line treatment considerations, with regard to the best combination of effectiveness, tolerability, and safety in the treatment of aggressive/disruptive behavior in youth. In contrast, gabapentin (
=7.2, SD 1.1) as first-line treatment considerations, with regard to the best combination of effectiveness, tolerability, and safety in the treatment of aggressive/disruptive behavior in youth. In contrast, gabapentin ( =2.9, SD 1.5) was not recommended based on the same criteria. All other medications were endorsed as second-line options.
=2.9, SD 1.5) was not recommended based on the same criteria. All other medications were endorsed as second-line options.
Polypharmacy
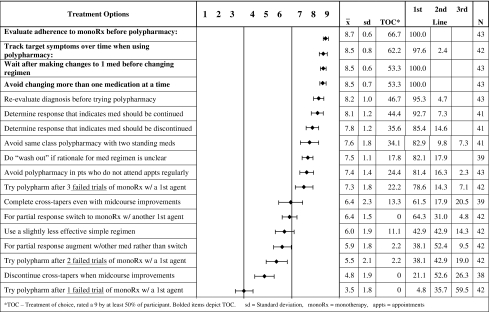
Figure 5 illustrates a single question and 20 response options for potential guiding principles on the use of polypharmacy in children and adolescents with clinically significant aggression. As seen in Figure 5, over 50% of respondents considered the following four option strategies of choice that should be employed when initiating polypharmacy: evaluate adherence, track target symptoms to ensure benefits, wait after making changes to one medicine, and avoid changing more than one medication at a time. These options were statistically distinct from the final four second-line options, indicating that experts did not fully support these treatment approaches to polypharmacy: switch rather than augment for a partial response, try polypharmacy after two failed trials of monotherapy, discontinue cross tapers in the event of midcourse improvements, and try polypharmacy after one failed trial of monotherapy. Most subjects (59.5%) viewed the use of polypharmacy after one failed trial of monotherapy as the least favorable treatment option.
FIG. 5.
Appropriateness of strategies as “guiding principles” on the use of polypharmacy in children and adolescents.
Medication discontinuation considerations
All response options were considered either a strategy of choice or first-line considerations as reasons to continue (i.e., to not discontinue) medications for aggression in youth ( =7.9). Some of these included the concern of relapse during previous discontinuation (
=7.9). Some of these included the concern of relapse during previous discontinuation ( =8.5, SD 0.8), history of very severe symptoms (
=8.5, SD 0.8), history of very severe symptoms ( =8.1, SD 1), and/or self-injurious behavior (
=8.1, SD 1), and/or self-injurious behavior ( =7.7, SD 1.1). In contrast, reasons to discontinue medications under the same clinical circumstances focused on the risk for long-term side effects (
=7.7, SD 1.1). In contrast, reasons to discontinue medications under the same clinical circumstances focused on the risk for long-term side effects ( =7.5, SD 1.1) and benign (
=7.5, SD 1.1) and benign ( =7.1, SD 1.1) or provoked aggression (
=7.1, SD 1.1) or provoked aggression ( =7.5, SD 1.5) in the past. Stopping medications because the child wants to stop and take control of his/her aggression without medication (
=7.5, SD 1.5) in the past. Stopping medications because the child wants to stop and take control of his/her aggression without medication ( =5.7, SD 2.0) was rated as a second-line option.
=5.7, SD 2.0) was rated as a second-line option.
Experts rated the following factors as the most important and sufficient clinical justification for attempting to reduce or discontinue one or more medications: child is on three or more antipsychotic medications ( =8.8, SD 0.5), symptoms could be due to side effect or drug interactions (
=8.8, SD 0.5), symptoms could be due to side effect or drug interactions ( =8.8, SD 0.5), or child is taking six (
=8.8, SD 0.5), or child is taking six ( =8.8, SD 0.8), five (
=8.8, SD 0.8), five ( =8.6, SD 0.9), or four (
=8.6, SD 0.9), or four ( =8.3, SD 1.1) psychotropic medications with no evidence of substantial benefit.
=8.3, SD 1.1) psychotropic medications with no evidence of substantial benefit.
For those patients demonstrating no response to an atypical antipsychotic and where a medication switch might be needed, experts endorsed switching to another atypical antipsychotic ( =7.7, SD 1.2) or anticonvulsant/mood stabilizer (
=7.7, SD 1.2) or anticonvulsant/mood stabilizer ( =7.9, SD 0.8) as a first-line approach. For a partial response to an atypical antipsychotic for aggressive or destructive behavior, experts endorsed adding a mood stabilizer (
=7.9, SD 0.8) as a first-line approach. For a partial response to an atypical antipsychotic for aggressive or destructive behavior, experts endorsed adding a mood stabilizer ( =7.8, SD 1.1) as a first-line approach. All other medication classes were either second line or below. For conceptually similar questions, experts supported switching to an atypical agent (
=7.8, SD 1.1) as a first-line approach. All other medication classes were either second line or below. For conceptually similar questions, experts supported switching to an atypical agent ( =8.2, SD 0.8) or another mood stabilizer (
=8.2, SD 0.8) or another mood stabilizer ( =7.1, SD 1.5) as a first-line treatment when a patient has shown no response to a trial of a mood stabilizer. Further, experts felt that the addition of an atypical antipsychotic (
=7.1, SD 1.5) as a first-line treatment when a patient has shown no response to a trial of a mood stabilizer. Further, experts felt that the addition of an atypical antipsychotic ( =7.9, SD 1.3) for a partial response to a mood stabilizer was a first-line treatment.
=7.9, SD 1.3) for a partial response to a mood stabilizer was a first-line treatment.
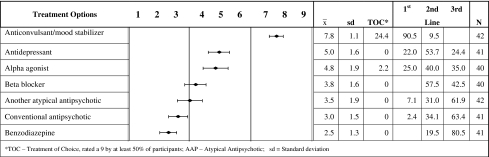
Partial response considerations
As seen in Figure 6, for patients displaying a partial response to an atypical antipsychotic for aggressive-destructive behavior, clinicians regarded the addition of a mood stabilizer as a first-line treatment approach, whereas the addition of another atypical was considered a second-line approach. Strategies such as the addition of conventional agents and benzodiazepines were not recommended. Overall, clinicians did not recommend within class polypharmacy.
FIG. 6.
Assume a patient has had only a partial response to an AAP for aggressive-destructive behavior. Rate the appropriateness of adding any of the listed medications.
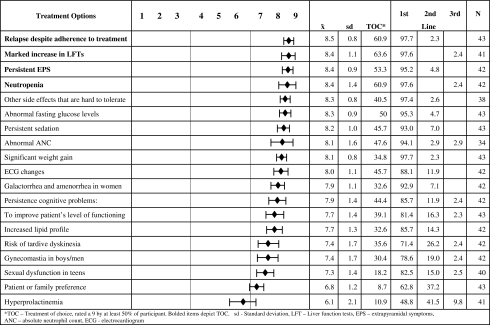
Considerations warranting a medication switch
In terms of clinical situations that might warrant a medication switch, four items were rated as treatments of choice (Fig. 7): relapse despite adherence ( =8.5, SD 0.8), marked increase in liver function test (LFTs) (
=8.5, SD 0.8), marked increase in liver function test (LFTs) ( =8.4, SD 1.1), persistent extrapyramidal symptoms (EPSs) (
=8.4, SD 1.1), persistent extrapyramidal symptoms (EPSs) ( =8.4, SD 0.9), and neutropenia (
=8.4, SD 0.9), and neutropenia ( =8.4, SD 1.4). All remaining items were in the realm of first-line treatment options firmly for warranting an antipsychotic medication switch. Items such as gynecomastia in boys/men (
=8.4, SD 1.4). All remaining items were in the realm of first-line treatment options firmly for warranting an antipsychotic medication switch. Items such as gynecomastia in boys/men ( =7.4, SD 1.7), sexual dysfunction in teens (
=7.4, SD 1.7), sexual dysfunction in teens ( =7.3, SD 1.4), patient or family preference ((
=7.3, SD 1.4), patient or family preference (( =6.8, SD 1.2), and especially, isolated hyperprolactinemia (
=6.8, SD 1.2), and especially, isolated hyperprolactinemia ( =6.1, SD 2.1) were less important indications.
=6.1, SD 2.1) were less important indications.
FIG. 7.
Rate the appropriateness of each factor as a reason for switching a child/adolescent from one antipsychotic to another. Assume an optimal therapeutic dose and the patient has been taking the agent as prescribed.
Discussion
In the last 10 years, outpatient psychotropic prescribing to pediatric populations in the United States has ballooned, with the greatest increase seen in the use of atypical antipsychotics for off-label uses, such as the management of persistent aggressive behavior in children and adolescents (Martin and Leslie 2003; Cooper et al. 2004; Olfson et al. 2006). At the same time, the use of psychosocial and psychological interventions has declined, raising significant concerns about the current overreliance on pharmacotherapy in the treatment of children and adolescents (Mojtabai and Olfson 2008). In light of the gap between the research literature and clinical practice, the current survey findings suggest that expert consensus opinion can provide an alternative perspective and support the development of best practice guidelines for optimal outpatient management in children and adolescents with severe and persistent behavioral difficulties. The usefulness of expert consensus in developing treatment strategies for children and adolescents has been demonstrated in other psychiatry initiatives, such as Guidelines for Adolescent Depression in Primary Care (Cheung et al. 2007) and Treatment Recommendations for the Use of Antipsychotics for Aggressive Youth (Pappadopulos et al. 2003). High degrees of consensus among survey responders suggest that there is general agreement on optimal treatment strategies for pediatric aggression.
In contrast to current practice trends, the results of this survey show that experts strongly support the use of evidence-based psychosocial interventions (e.g., behavior therapy and parent management training vs. play therapy and art therapy) and parent education and training before the use of medication for maladaptive aggression—at every stage of medication treatment from diagnosis to maintenance to medication discontinuation. The fact that the primary or coutilization of psychosocial interventions is not consistently followed in clinical practice (Crystal et al. 2009) can be due to a number of reasons, including lack of (quickly) available therapy appointments, scarcity of resources, urgency/severity of the problem, paucity of therapists using evidence-based psychotherapy methods, desire for a “quick fix,” and refusal to engage in nonpharmacologic treatments. Further, much of what was endorsed by experts appears to be consistent with the literature. For example, with regard to the use of polypharmacy for aggression, survey responders agreed that monotherapy is preferable to polypharmacy for most conditions, except for bipolar symptoms such as severe mood lability. These findings suggest that a systematic model for outpatient treatment of pediatric maladaptive aggression that is informed by the systematically derived expert opinion and the literature is attainable.
These survey findings provide consistent evidence of expert endorsement of strategies that emphasize the importance of behavioral interventions and talking to families about their treatment preferences. However, in routine clinical practice, such behavioral interventions are not often used (Mojtabai and Olfson 2008; Crystal et al. 2009), suggesting that they should be done more regularly and systematically.
Although clinicians endorsed the use of rating scales to assess target symptoms, experts supported the use of more general measures of child psychopathology such as the Child Behavior Checklist (CBCL), which may reflect familiarity rather than the usefulness of a more specific measure. Further, this finding may also reflect clinicians' needs to balance convenience and time constraints with the narrowness of any particular measure. Also of interest was that clinicians did not strongly endorse the use of measures of functioning or quality of life, even though this is the ultimate focus of treatment. Experts seem focused on the more immediate treatment issues and symptoms as opposed to the long-term impact on functioning and quality of life.
Experts also strongly endorsed intervention strategies to help build the therapeutic relationship. Such approaches can be easily taken for granted and cannot be replaced by treatment consent procedures that were not highly rated. Education and the use of written materials were strongly endorsed, although it is unclear how often patients and families actually receive handouts. Experts seemed aware of the constraints in busy practice settings and concentrated on interventions that would not be too time consuming or otherwise unrealistic because of excessive burdens on clinicians.
The use of psychosocial interventions at every phase of treatment was strongly endorsed by clinicians and never considered inappropriate. Yet, Mojtabai and Olfson (2008) have shown that the use of psychosocial interventions has been significantly curtailed in child and adolescent psychiatric care. Although behavior therapy was rated highly and is strongly supported by the literature (Scotto Rosato et al., submitted), environmental interventions and parent education were more strongly supported than group interventions for the child, such as anger management and social skills training.
In terms of pharmacological interventions, experts supported the use of medication for patients with high risk for interpersonal harm or psychosis. Additionally, ratings of other items indicate that, generally, expert opinion does not support the use of medications for difficult children to address symptoms that are limited to minor aggression, such as persistent cursing, mild temper outbursts, or stealing. Expert ratings did support pharmacological interventions that focus on the underlying symptoms or primary diagnosis rather than chasing symptoms. The importance of evaluating and treating co-morbid symptoms was also strongly endorsed.
Experts endorsed the use of atypical antipsychotics and mood stabilizers as first-line strategies for treating clinically significant aggression. Interestingly, levels of expert support for use of atypical antipsychotics and use of mood stabilizers were similar. Unfortunately, however, to date, studies are lacking that could provide support for choosing one class of agents over another. Moreover, comparative effectiveness evidence is missing, which would provide information about the relative efficacy and safety of different agents, even within each medication class. When medication treatments were not working, experts strongly supported the assessment of patient compliance before changing the medication regimen. They noted the importance of only changing one medication at a time to fully realize the benefits or costs of any particular agent in the regimen. The use of within class polypharmacy was viewed with some degree of skepticism.
It is interesting that experts supported the use of a stimulant in cases of failed behavior therapy for conduct disorder. Although the initial use of stimulants in youth with behavioral problems and ADHD has been strongly endorsed before (Pliszka et al. 2006), there appeared to be emerging consensus that stimulants may be appropriate even in the absence of clear-cut ADHD symptoms, most likely because they would offer the quickest response with the least potential for dangerous or unexpected side effects. This finding remains an important area for future investigation. Finally, experts were cautious about discontinuing successful pharmacotherapy in light of a history of persistent symptoms or relapse during discontinuation. Although doctors emphasized the importance of preventing another relapse during adherence with a given medication, life-threatening side effects such as neutropenia and a marked increase in LFTs were also justifications for change. It is important to note that fasting glucose abnormalities and significant weight gain were also first-line reasons to switch medications along with persistent sedation, abnormal ANC (absolute neutrophil count), and ECG (electrocardiogram) changes. Respondents rated gynecomastia in boys/men and sexual dysfunction in teens relatively less important within the context of the treatment options presented in the question on switching. Such items may not be as critical to clinicians who are trying to manage very serious and at times dangerous aggressive symptoms; however, these very items may be critical to child and adolescent adherence with their antipsychotic treatment regimen. In contrast, consistent with current recommendations for the monitoring and management of antipsychotic-treated youth (Correll 2008), isolated prolactin elevations had the lowest justification for switching antipsychotics.
Conclusions
Overall findings indicate that evidence-informed strategies for outpatient treatment of pediatric maladaptive aggression, guided by systematically derived expert opinions, are attainable. In light of the gap between the research literature and clinical practice, expert consensus opinion supports specific practices for optimal outpatient management in children and adolescents with severe and persistent behavioral difficulties.
A shortcoming of the survey was that it did not attempt to identify the minimal professional competencies required to manage youth with dangerous behavioral dyscontrol or those who require complex medication regimens. Therefore, primary care doctors who elect to treat children with behavioral problems involving aggression should consider based on the severity, treatment nonresponse, negative functional impact, and dangerousness, whether a referral to a child psychiatrist or a more restrictive treatment setting is needed. In rural settings or locations where child psychiatrists are in short supply, a professional consultation may be very helpful.
By way of caution, expert opinion may be informative, but does not substitute clinical trial evidence. Although we aimed to include experts representing as broad and diverse a range of expertise, experience, and professional backgrounds as possible, the selection of the experts was not based on systematic sampling procedures and may not capture the full range of expert opinion. As noted in the Disclosures section, some of the authors have received significant support from pharmaceutical manufacturers, although none was an industry employee at the time the work was conducted (the first author is currently employed by Pfizer). We also did not attempt to restrict the expert survey respondents to individuals who had not received industry support.
Clinical Significance
Although expert opinion does not substitute for empirical evidence, expert consensus provides added insight into clinical practices and treatment nuances that may never be addressed in controlled studies. Practicing clinicians are encouraged to use such data in light of their own clinical judgment as well as of the available and emerging knowledge from the literature. As the treatment of youth with clinically relevant aggression is an important and evolving area in child and adolescent psychiatry, addressing the needs of these youth will continue to be a challenging issue for clinicians, regulators, stakeholders, and policy makers, and it will be important to inform practice with insights both from the evolving evidence base and from experts' assessment of the available evidence.
Appendix: Treatment of Maladaptive Aggression in Youth Steering Committee Members
Peter S. Jensen, M.D., Chair
Stephen Crystal, Ph.D.
Elizabeth Pappadopulos, Ph.D.
Alanna Chait, B.S.
Nancy Scotto Rosato, Ph.D.
Lynn Crismon, Pharm D.
Robert Findling, M.D.
Penelope Knapp, M.D.
Mark Olfson, M.D.
David Woodlock, M.S.
Sherrie Bendele, B.S.
Christoph U. Correll, M.D.
Tobias Gerhard, Ph.D.
Karen Hart, B.S.
Cindy Hopkins
Danielle Laraque, M.D.
Laurel K. Leslie, M.D., M.P.H.
Judith A. Lucas, Ed.D., A.P.N.
Nancy Parker
Mark Wolraich, M.D.
John Lochman, Ph.D., ABPP
Disclaimer
Views expressed in this article are those of the authors and do not necessarily reflect positions of the Agency for Healthcare Research and Quality.
Disclosures
Dr. Pappadopulos is currently employed by Pfizer and has a part-time research position at Zucker Hillside Hospital. She also receives grant support from the NIMH. Dr. Scotto Rosato is currently employed by the New Jersey Department of Health and Senior Services and has no other competing interests. Dr. Correll has been a consultant to or has received honoraria from AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Janssen, Otsuka, Pfizer, Supernus, and Vanda and has served on the speaker's bureau of AstraZeneca, Bristol-Myers Squibb/Otsuka, and Pfizer. Dr. Findling receives or has received research support, acted as a consultant and/or served on the speaker's bureau for Abbott, Addrenex, AstraZeneca, Biovail, Bristol-Myers Squibb, Forest, GlaxoSmithKline, Johnson & Johnson, KemPharm Lilly, Lundbeck, Neuropharm, Novartis, Organon, Otsuka, Pfizer, Sanofi-Aventis, Sepracore, Shire, Solvay, Supernus Pharmaceuticals, Validus, and Wyeth. Dr. Lucas receives research support from The Retirement Research Foundation, has received research support from the RWJ Foundation, and has no other competing interests. Dr. Crystal receives support from the Agency for Healthcare Policy and Research and the National Institute of Mental Health and has no competing interests. Dr. Jensen has received training and/or research funds from the Lowenstein Foundation, the Klingenstein Third Generation Foundation, Annie E. Casey Foundation, Casey Family Programs, Magellan, and Value Options, participates in speakers' bureaus for the Neuroscience Education Institute, and consults with Best Practice, Inc., Janssen-Ortho, and Shire.
References
- Brook RH. Chasin MR. Fink A. Solomon DH. Kosecoff J. Park RE. A method for the detailed assessment of the appropriateness of medical technologies. Int J Technol Assess Health Care. 1986;2:53–63. doi: 10.1017/s0266462300002774. [DOI] [PubMed] [Google Scholar]
- Cheung AH. Zuckerbrot RA. Jensen PS. Ghalib K. Laraque D. Stein RKE. Guidelines for adolescent depression in primary care (GLAD-PC):II. Treatment and ongoing management. Pediatrics. 2007;120:e1313–e1326. doi: 10.1542/peds.2006-1395. [DOI] [PubMed] [Google Scholar]
- Cooper WO. Hickson GB. Fuchs C. Arbogast PG. Ray WA. New users of antipsychotic medications among children enrolled in TennCare. Arch Pediatr Adolesc Med. 2004;158:753–759. doi: 10.1001/archpedi.158.8.753. [DOI] [PubMed] [Google Scholar]
- Correll CU. Antipsychotic use in children and adolescents: Minimizing adverse effects to maximize outcomes. J Am Acad Child Adolesc Psychiatry. 2008;47:9–20. doi: 10.1097/chi.0b013e31815b5cb1. [DOI] [PubMed] [Google Scholar]
- Crystal S. Olfson M. Huang C. Pincus H. Gerhard T. Broadened use of atypical antipsychotics: Safety, effectiveness, and policy challenges. Health Aff (Millwood) 2009;28:770–781. doi: 10.1377/hlthaff.28.5.w770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findling RL. Aman MG. Eerdekens M. Derivan A. Lyons B. Long-term, open-label study of risperidone in children with severe disruptive behaviors and below-average IQ. Am J Psychiatry. 2004;161:677–684. doi: 10.1176/appi.ajp.161.4.677. [DOI] [PubMed] [Google Scholar]
- Findling RL. Kusumakar V. Daneman D. Moshang T. De Smedt D. Binder C. Prolactin levels during long-term risperidone treatment in children and adolescents. J Clin Psychiatry. 2003;64:1362–1369. doi: 10.4088/jcp.v64n1113. [DOI] [PubMed] [Google Scholar]
- Findling RL. Robb A. Nyilas M. Forbes RA. Jin N. Ivanova S. Marcus R. McQuade RD. Iwamoto T. Carson WH. A multiple-center, randomized, double-blind, placebo-controlled study of oral aripiprazole for treatment of adolescents with schizophrenia. Am J Psychiatry. 2008;165:1432–1441. doi: 10.1176/appi.ajp.2008.07061035. [DOI] [PubMed] [Google Scholar]
- Findling RL. Kauffman R. Sallee FR. Salazar DE. Sahasrabudhe V. Kollia G. Kornhauser DM. Vachharajani N. Assuncao-Talbott S. Mallikaarjun S. Iwamoto T. McQuade RD. Boulton DW. Blumer J. An open-label study of aripiprazole: Pharmacokinetics, tolerability, and effectiveness in children and adolescents with conduct disorder. J Child Adolesc Psychopharmacol. 2009;19:431–439. doi: 10.1089/cap.2008.0111. [DOI] [PubMed] [Google Scholar]
- Jensen P. Builtelaar J. Pandina G. Binder R. Reyes M. Management of psychiatric disorders in children and adolescents with atypical antipsychotics. Eur J Child Adolesc Psychiatry. 2007a;16:104–120. doi: 10.1007/s00787-006-0580-1. [DOI] [PubMed] [Google Scholar]
- Jensen PS. Youngstrom E. Steiner H. Findling RL. Meyer RE. Malone RP. Carlson GA. Coccaro EF. Aman MG. Blair J. Dougherty D. Ferris C. Flynn L. Green E. Hoagwood K. Hutchinson J. Laughren T. Leve LD. Novins DK. Vitiello B. Consensus report: Impulsive aggression as a symptom across diagnostic categories in child psychiatry: Implications for medication studies. J Am Acad Child Adolesc Psychiatry. 2007b;46:309–322. doi: 10.1097/chi.0b013e31802f1454. [DOI] [PubMed] [Google Scholar]
- Khan DA. Docherry JP. Carpenter D. Frances A. Consensus methods in practice guidelines development: A review and description of a new method. Psychopharmacol Bull. 1997;33:631–639. [PubMed] [Google Scholar]
- Martin A. Leslie D. Psychiatric inpatient, outpatient, and medication utilization and costs among privately insured youths, 1997–2000. Am J Psychiatry. 2003;160:757–764. doi: 10.1176/appi.ajp.160.4.757. [DOI] [PubMed] [Google Scholar]
- Mojtabai R. Olfson M. National trends in psychotherapy by office-based psychiatrists. Arch Gen Psychiatry. 2008;65:962–970. doi: 10.1001/archpsyc.65.8.962. [DOI] [PubMed] [Google Scholar]
- Olfson M. Blanco C. Liu L. Moerno C. Laje G. National trends in outpatient treatment of children and adolescents with antipsychotic drugs. Arch Gen Psychiatry. 2006;63:679–685. doi: 10.1001/archpsyc.63.6.679. [DOI] [PubMed] [Google Scholar]
- Olfson M. Crystal S. Huang C. Gerhard T. Trends in antipsychotic drug use by very young, privately insured children. J Am Acad Child Adolesc Psychiatry. 2010;49:13–23. doi: 10.1097/00004583-201001000-00005. [DOI] [PubMed] [Google Scholar]
- Pappadopulos E. MacIntyre JC., II Crismon ML. Findling RL. Malone RP. Derivan A. Schooler A. Sikich L. Greenhill LL. Schur SB. Felton C. Kranzler H. Rube D. Sverd J. Finnerty M. Ketner S. Siennick SE. Jensen PS. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY): Part Two. J Am Acad Child Adolesc Psychiatry. 2003;42:145–161. doi: 10.1097/00004583-200302000-00008. [DOI] [PubMed] [Google Scholar]
- Pappadopulos E. Woolston S. Chait A. Perkins M. Connor DF. Jensen PS. Pharmacotherapy of aggression in children and adolescents: Efficacy and effect size. J Can Acad Child Adolesc Psychiatry. 2006;15:27–39. [PMC free article] [PubMed] [Google Scholar]
- Patel NC. Crismon ML. Hoagwood K. Jensen PS. Unanswered questions regarding antipsychotic use in children and adolescents. J Child Adolesc Psychopharmacol. 2005a;15:270–284. doi: 10.1089/cap.2005.15.270. [DOI] [PubMed] [Google Scholar]
- Patel NC. Crismon ML. Hoagwood K. Johnsrud MT. Rascati KL. Wilson JP. Jensen PS. Trends in the use of atypical and typical antipsychotics in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2005b;44:548–556. doi: 10.1097/01.chi.0000157543.74509.c8. [DOI] [PubMed] [Google Scholar]
- Pliszka SR. Crismon ML. Hughes CW. Conners CK. Emslie GJ. Jensen PS. McCracken JT. Swanson JM. Lopez M. Texas Consensus Conference Panel on Pharmacotherapy of Childhood Attention Deficit Hyperactivity Disorder: The Texas Children's Medication Algorithm Project: A revision of the algorithm for medication treatment of childhood attention deficit hyperactivity disorder (ADHD) J Am Acad Child Adolesc Psychiatry. 2006;45:520–526. doi: 10.1097/01.chi.0000215326.51175.eb. [DOI] [PubMed] [Google Scholar]
- Ratzoni G. Gothelf D. Brand-Gothelf A. Reidman J. Kikinzon L. Gal G, et al. Weight gain associated with olanzapine and risperidone in adolescent patients: A comparative prospective study. J Am Acad Child Adolesc Psychiatry. 2002;41:337–343. doi: 10.1097/00004583-200203000-00014. [DOI] [PubMed] [Google Scholar]
- Reyes et al. A randomized, double-blind, placebo-controlled study of risperidone maintenance treatment in children and adolescents with disruptive behavior disorders. Am J Psychiatry. 2006;163:402–410. doi: 10.1176/appi.ajp.163.3.402. [DOI] [PubMed] [Google Scholar]
- RUPP Autism Network: Risperidone treatment of autistic disorder: Longer-term benefits and blinded discontinuation after 6 months. Am J Psychiatry. 2005;162:1361–1369. doi: 10.1176/appi.ajp.162.7.1361. [DOI] [PubMed] [Google Scholar]
- Schur SB. Sikich L. Findling RL. Malone RP. Crismon ML. Derivan A. MacIntyre JC., II Pappadopulos E. Greenhill LL. Schooler N. Van Order K. Jensen PS. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY) Part One: A review. J Am Acad Child Adolesc Psychiatry. 2003;42:132–144. doi: 10.1097/00004583-200302000-00007. [DOI] [PubMed] [Google Scholar]