Abstract
Background and Objectives:
Methicillin resistant Staphylococcus aureus (MRSA) is a major nosocomial pathogen causing significant morbidity and mortality. The aim of this study was to evaluate in vitro activities of different antibiotics against methicillin resistant Staphylococcus aureus.
Materials and Method:
The study was conducted over a period of one year (January 2009 – December 2009) in the Department of Microbiology, Army Medical College, the National University of Sciences and Technology, Pakistan. One hundred and thirty-nine Methicillin resistant Staphylococcus aureus isolated from the clinical specimens at Rawalpindi Military Hospital were subjected to in vitro susceptibility against various antimicrobials using Kirby Bauer disc diffusion technique.
Results:
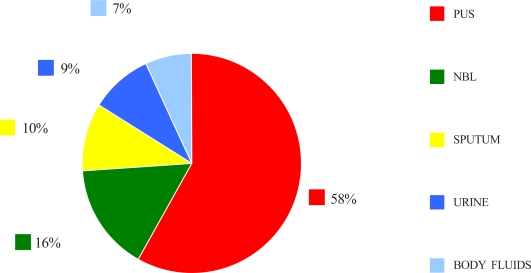
All the isolated MRSA organisms were uniformly susceptible to vancomycin, linezolid and tigecycline. Other drugs which were found to be effective were chloramphenicol, and rifampacin. Most of the MRSA were isolated from pus samples.
Conclusion:
Vancomycin, tigecycline and linezolid were effective against methicillin resistant strains of S.aureus. This study suggests that chloramphenicol and rifampacin also have good in vitro efficacy for methicillin resistant S. aureus infections. Oral dosing option for linezolid, chloramphenicol and rifampacin can allow earlier discharge of hospitalized patients and thus reduce health care expenses as well as help reduce the chances of vancomycin resistant strains emergence.
Keywords: Staphylococcus aureus, MRSA, Vancomycin, Susceptibility pattern, Military Hospital
INTRODUCTION
The genus Staphylococcus includes pathogenic organisms in which Staphylococcus aureus is the most important. It has overcome most of the therapeutic agents that have been developed against it in the recent years (1). The introduction of beta-lactamase resistant semi-synthetic penicillins in the early 1960's provided temporary relief which ended with the emergence of Methicillin (oxacillin) Resistant Staphylococcus aureus (MRSA), discovered shortly after methicillin became available for clinical use (2).
Many of these MRSA isolates are becoming multidrug resistant and are susceptible only to glycopeptide antibiotics such as vancomycin. Low level resistance even to vancomycin is emerging at present (1). Prolonged hospital stays, indiscriminate use of antibiotics, lack of awareness, and receipt of antibiotics before coming to the hospital are some of the possible predisposing factors of MRSA emergence. The knowledge of MRSA prevalence and the current antimicrobial profile is necessary in selection of appropriate empirical treatment of these infections. Control of MRSA in hospitals is essential. This can be achieved by proper implementation of hospital infection control measures and regular surveillance activity. Therefore, we planned this study to determine the current antimicrobial profile of MRSA isolates from our hospital so as to formulate an appropriate as well as cost effective empirical therapy.
MATETIALS AND METHODS
The study was conducted over a one-year (January 2009–December 2009) period at the Department of Microbiology, Army Medical College, National University of Sciences and Technology, Pakistan. All Staphylococcus aureus isolates encountered in routine clinical specimens received from clinical wards of Military Hospital Rawalpindi were identified morphologically and biochemically by standard laboratory procedures including tube coagulase test and DNase test using DNase agar (Oxoid Ltd, Basingstoke, Hampshire, England). MRSA screening was performed on Mueller-Hinton agar using 6 µg oxacillin and 30 µg cefoxitin discs as per Clinical and Laboratory Standards Institute (CLSI) guidelines (3). Susceptibility to antimicrobial agents was determined by the modified Kirby Bauer disc diffusion method using following antimicrobial discs: vancomycin (30 µg), linezolid (30 µg), teicoplanin (30µg), tigecycline (30 µg), tetracycline (30 µg), minocycline (30 µg), quinopristin/dalfopristin (15 µg), Fluoroquinolones (ciprofloxacin, levofloxacin, ofloxacin and moxifloxacin 5 µg), chloramphenicol (30 µg), rifampicin (5 µg), fusidic acid (10 µg), macrolides (erythromycin and clindamycin 15 µg) as per CLSI guidelines (3).
RESULTS
A total of 139 MRSA were isolated during the study period. All of the isolated MRSA were found to be susceptible to vancomycin, linezolid and quinopristin/ dalfoprisitin. One hundred and thirty isolates (94%) were susceptible to teicoplanin and minocycline, whereas 93% of isolates were sensitive to chloramphenicol and 91% were sensitive to tigecycline. Only 38 and 22% of the isolates were susceptible to fluoroquinolones and macrolides respectively (Table 1). Majority of MRSA were isolated from pus samples followed by nasobronchial lavages samples (Fig. 1).
Table 1.
Susceptibility pattern of MRSA against various antibiotics.
| Antibiotic | Sensitive | Resistant | % sensitive |
|---|---|---|---|
| Vancomycin | 139 | 0 | 100 |
| Linezolid | 139 | 0 | 100 |
| Quinopristin/Dalfopristin | 139 | 0 | 100 |
| Teicoplanin | 130 | 9 | 94 |
| Minocycline | 130 | 9 | 94 |
| Chloramphenicol | 129 | 10 | 93 |
| Tigecycline | 127 | 12 | 91 |
| Trimethoprim/sulphamethoxazole | 94 | 45 | 67 |
| Fusidic acid | 91 | 48 | 65 |
| Tetracycline | 89 | 50 | 64 |
| Rifampicin | 86 | 53 | 62 |
| Doxycycline | 57 | 82 | 41 |
| Fluoroquinolones | 53 | 86 | 38 |
| Macrolides | 31 | 108 | 22 |
Fig. 1.
Percentage of MRSA isolated from various specimens.
DISCUSSION
A study conducted at the Armed Forces Institute of Pathology Rawalpindi in 2003–2004 indicated that there was no reduced susceptibility of vancomycin against studied MRSA isolates as indicated in our study. However, VISA strains were detected in 4% of isolates in Lahore in 2004 (4, 5). The incidence of VISA in the regional countries has been documented as 3.3% (Srinagar, Kashmir, 2003), 6% (India, 2007) and 7.5% (Iran, 2008) (6–8).
The results of our study are in accordance with a study carried out at Aga Khan University in 2009 which showed variable susceptibility pattern with high resistance rates to tetracycline (82%), clindamycin (79%), cotrimoxazole (59%), and rifampicin (50%). Resistance to chloramphenicol (10%) and fusidic acid (9%) was low (9). A study carried out at Lahore in 2009 showed that only 4% of MRSA isolates were sensitive to fluoroquinoles, whereas 38% of isolates were found to be sensitive in our study (10).
In our study 100% of the isolates were sensitive to linezolid which is complemented by a 2009 study carried out in Iran. In that study, tigecycline was also found to be 100% which is similar to the results of another study in Iran (11).
Vancomycin and linezolid are highly effective against MRSA. Chloramphenicol and Minocycline also have good in vitro efficacy. Tigecycline, though effective, enhances health care costs enormously.
Effective antimicrobial activity as well as cost effectiveness should be considered in drugs prescribed for MRSA infections. Oral dosing options for linezolid and chloramphenicol can allow earlier discharge of hospitalized patients and minimize the chances of VRSA emergence. Good hospital infection control measures prove to be the main stay against these infections because antibiotics can never be an effective alternative to good medical practice
ACKNOWLEDGEMENT
This was supported by National University of Sciences and Technology, Clinical Pathology Lab, Microbiology, Army Medical College Rawalpindi, Pakistan.
REFERENCES
- 1.Rajaduraipandi K, Mani KR, Panneerselvam K, Mani M, Bhaskar M, Manikandan P. Prevalence and antimicrobial susceptibility pattern of methicillin resistant Staphylococcus aureus: A multicentre study. Indian J Med Microbiol. 2006;24:34–38. doi: 10.4103/0255-0857.19892. [DOI] [PubMed] [Google Scholar]
- 2.Hafeez R, Chughtai AS, Aslam M. Prevalence and antimicrobial susceptibility of methicillin resistant Staphylococcus aureus (MRSA) Int J Pathol. 2004;2:10–15. [Google Scholar]
- 3.National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing-19th informational supplement; 2009. M100-S19. NCCLS, Wayne, PA, USA. [Google Scholar]
- 4.Mehmood A, Butt T, Usman M. A study on MRSA isolates to detect reduced susceptibility to vancomycin: A preliminary report. Infect Dis J. 2007;16:102–104. [Google Scholar]
- 5.Bukhari MH, Iqbal A, Khatoon N, Iqbal N, Naeem S, Qureshi G R, et al. A laboratory study of susceptibility of methicillin resistant Staphylococcus aureus (MRSA) Pak J Med Sci. 2004;20:229–33. [Google Scholar]
- 6.Assadullah S, Kakru DK, Thoker MA, Bhat FA, Hussain N, Shah A. Emergence of low level vancomycin resistance in MRSA. Indian J Med Microbiol. 2003;21:196–198. [PubMed] [Google Scholar]
- 7.Sonavane A, Mathur M. Screening for vancomycin intermediate-resistant Staphylococcus aureus among clinical isolates of MRSA. Indian J Med Microbiol. 2007;25:79–80. doi: 10.4103/0255-0857.31078. [DOI] [PubMed] [Google Scholar]
- 8.Mehdinejad M, Sheikh AF, Jolodar A. Study of methicillin resistance in Staphylococcus aureus and species of coagulase negative Staphylococci isolated from various clinical specimens. Pak J Med Sci. 2008;24:719–24. [Google Scholar]
- 9.Idrees F, Jabeen K, Khan MS, Zafar A. Antimicrobial resistance profile of methicillin resistant staphylococcal aureus from skin and soft tissue isolates. J Pak Med Assoc. 2009;59:266–269. [PubMed] [Google Scholar]
- 10.Hannan A, Absar M, Usman M, Naeem T, Saleem S, Arshad M. In vitro activity of linezolid against clinical isolates of methicillin resistant Staphylococcus . J Ayub Med Coll Abbottabad. 2009;21:106–109. [PubMed] [Google Scholar]
- 11.Fatholahzadeh B, Emaneini M, Gilbert G, Udo E, Aligholi M, Modarressi MH, et al. Staphylococcal cassette chromosome mec (SCCmec) analysis and antimicrobial susceptibility patterns of methicillin-resistant Staphylococcus aureus (MRSA) isolates in Tehran, Iran. Microb Drug Resist. 2008;14:217–220. doi: 10.1089/mdr.2008.0822. [DOI] [PubMed] [Google Scholar]