Abstract
Background
Leishmaniasis is endemic in Iran. Different species of Leishmania (L.) parasites are causative agents of this disease. Correct identification of Leishmania species is important for clinical studies, prevention, and control of the diseases. Mix up of Leishmania isolates is possible in the laboratory, so there is need for verification of species for isolates of uncertain identity. Different methods may be used for this purpose including isoenzyme electrophoresis and molecular methods. The isoenzyme electrophoresis, due to its drawbacks, is feasible only in specialized laboratories while molecular methods may be more feasible. The aim of this research was to study the application of the internal transcribed spacer 1 (ITS1) sequencing method, in comparison to isoenzyme electrophoresis method, for verification of Leishmania species.
Methods
Six Leishmania isolates were received from different research institutions in Iran. The species of these isolates were known by donating institution according to their isoenzyme profile. The species of these isolates were re-identified in Pasteur Institute of Iran by PCR amplification of ITS1 followed by sequencing and comparison of these sequences with Leishmania sequences in GenBank. Isoenzyme electrophoresis was performed for confirmation of the results of ITS1.
Results
ITS1 sequence showed that some isolates were mixed up or contaminated with Crithidia. Isoenzyme electrophoresis confirmed the results of ITS1 sequences.
Conclusion
ITS1 sequencing is relatively more feasible than the traditional isoenzyme electrophoresis method and is suggested for verification of Leishmania species.
Keywords: Leishmania, Crithidia, Internal transcribed spacer (ITS), Isoenzyme electrophoresis
Introduction
The leishmaniases are a spectrum of diseases of humans and other mammals that are endemic in 88 countries with an estimated yearly incidence of l–1.5 million cases of cutaneous leishmaniasis and 500000 cases of visceral leishmaniasis (1). Cutaneous and visceral leishmaniases are endemic in Iran (2, 3). Different species of Leishmania (L.) parasites are causative agent of these diseases in Iran (4–6). Leishmania species differ from each other from many aspects including clinical presentation of the disease, their vectors and reservoirs, and their epidemiological criteria. Hence, identification of Leishmania species is important in Leishmania studies including clinical research, evaluation of vaccines and drugs, epidemiology, prevention and control of the diseases (7).
Different methods are used for species identification of Leishmania parasites including: use of monoclonal antibodies (6), study of isoenzyme (8), and molecular methods (9). Not all clinical and experimental laboratories have sufficient facilities necessary for identification of Leishmania parasites at species level. Laboratories lacking such facilities usually use Leishmania species that have already been identified by other laboratories. Hence, exchange of Leishmania parasites with identified species between different laboratories takes place usually. It is possible that Leishmania isolates are mixed up or they are contaminated with non-Leishmania trypanosomatids (e.g. Crithidia) in laboratory. Mixing up or contamination of Leishmania isolates in one laboratory and exchange of this parasite between laboratories can lead to incorrect data and conclusions. This pitfall can be prevented by verification of Leishmania isolates of uncertain identity. The gold standard for species identification is still isoenzyme electrophoresis (10). However, only specialized laboratories have sufficient facilities and expertise to perform this method. The internal transcribed spacer 1 (ITS1) sequencing is an alternative method for species identification that does not have many technical drawbacks of the isoenzyme electrophoresis.
The aim of this study was to evaluate the relative feasibility of ITS1 sequencing, in comparison to isoenzyme electrophoresis for verification of Leishmania species.
Material and Methods
Parasite
Six Leishmania isolates were received as gifts from different research laboratories (see Table 1). The species of these isolates were assumed to be known based on isoenzyme profile provided by the donating laboratories. The isolates were stored in liquid nitrogen and were recovered for the present study by thawing and culturing them in NNN media (11). Logarithmic parasites were harvested and washed by phosphate buffer saline (PBS) two times and were stored in aliquots of 100×106 parasites (for DNA extraction) and 1×109 parasites (for isoenzyme electrophoresis) in −70°C.
Table 1.
Leishmania isolates studied in the present study
| Isolate No. | International code | Assumed species according to the donating institutions | Real species as identified in the present study |
|---|---|---|---|
| 1 | MHOM/IR/75/ER | L. majora | L. major |
| 2 | MHOM/IR/05/SHZ5 | L. infantum | C. fasciculata |
| 3 | MCAN/IR/97/LON 49 | L. infantum | L. tropica |
| 4 | Not available | L. infantum | C. fasciculata |
| 5 | MHOM/IR/04/IPI-UN10 | L. infantum | L. infantum |
| 6 | MHOM/AF/88/KK27 | L. tropica | L. tropica |
Abbreviations used: L.; Leishmania, C.; Crithidia.
Amplification of ITS1 and RFLP analysis
Genomic DNA was extracted by LiCl extraction (12). The ITS1 region was amplified using DNA extracted from parasite and ITS1 specific primers LITSR and L5.8S and analyzed by restriction fragment length polymorphism (RFLP) analysis using the restriction endonuclease HaeIII (13).
Sequencing of ITS1
PCR amplification of genomic DNA from each of the isolates No. 1, 2, 4, and 5 resulted in a sharp single band in agarose gel electrophoresis. These PCR products were directly sent for sequencing (Macrogene, Seoul, Korea). Each PCR product was sequenced at least twice by ITS1 specific primers: once by the forward primer (LITSR) and once by the reverse primer (L5.8S). Nucleotide in each position was considered correct if the two sequencing results (which were sequenced in opposite directions) confirmed each other. The ITS1 sequences of isolates No. 3 and 6 were determined through a T/A cloning approach. This approach was done because PCR amplification of these isolates did not resulted in a single sharp band in electrophoresis; hence direct sequencing of PCR products were not sufficiently informative and conclusive. The T/A cloning was performed by using InsTA cloning kit (Fermentas, Burlington, Canada) according to the manufacturer instructions. Briefly, ITS1 fragment was amplified through PCR by ITS1 specific primers. The product of ITS1-PCR was run in agarose gel electrophoresis. The band that was compatible to ITS1 molecular weight (about 300 base pairs) was excised and extracted from agarose gel by Silica Bead DNA Gel Extraction kit (Fermentas Co.). Gel extracted DNA fragment was inserted into pTZ57R plasmid by ligase enzyme. The insert containing plasmid was transformed into DH5α strain of Escherichia coli bacteria. The transformed bacteria were cultured overnight and plasmids were purified by a plasmid purification kit (Bioneer Co.) according to the manufacturer instruction. This kit purifies the plasmids by the modified alkaline lysis method. The purified plasmids were sequenced by plasmid specific forward and reverse primers.
Isoenzyme electrophoresis
The isoenzyme study was performed using discontinuous polyacrylamide gel electrophoresis (PAGE) as described earlier (14). Each Leishmania strain was tested for the activity of at least four enzyme systems out of the following enzymes: glucose phosphate isomerase (GPI), malate dehydrogenase (MDH), nucleoside hydrolase (NH), malic enzyme (ME), super oxide dismutase (SOD) and phosphoglucomutase (PGM). Performance of this technique, due to fund limitation, was restricted to the isolates whose species were revealed to be different from the assumed species (i.e. declared by the donating institution) and for the only true L. infantum isolate studied in the present study.
Results
RFLP
RFLP patterns of isolate No.1 was compatible with L. major. RFLP pattern for isolates No 2 and 4 were suggestive of other trypanosomatids such as Crithidia species (e.g. C. fasciulata with GenBank accession number Y00055.1). RFLP patterns for isolates 3, 5 and 6 were compatible with the reported RFLP pattern for L. tropica or L. infantum (data not shown).
ITS1 sequencing
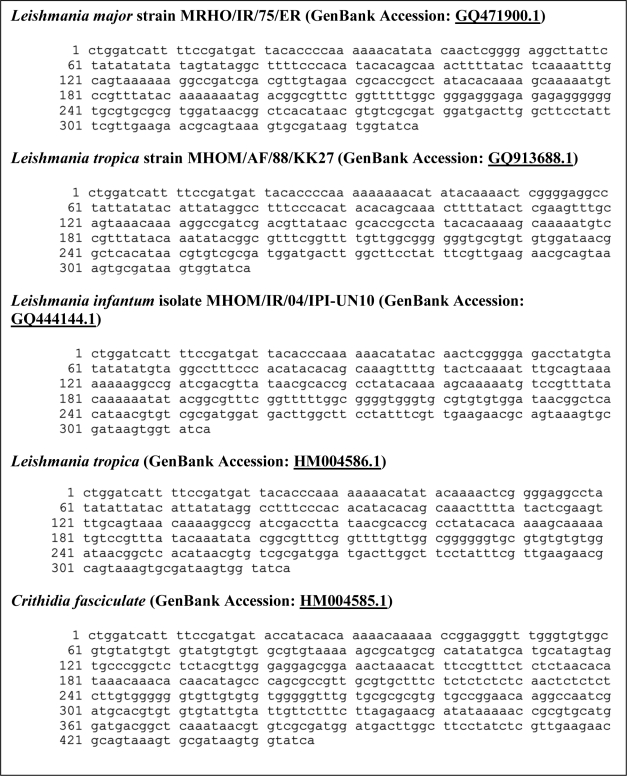
The ITS1 of the Leishmania isolates studied in the present report (six isolates) were sequenced and deposited in GenBank (Fig. 1). Comparison of the ITS1 sequences of the six isolates with other Leishmania species in GenBank (http://www.ncbi.nlm.nih.gov/sites/entrez?db=nucleotide) revealed the following results: isolate 1 was 99% and 100% identical to L. major Friedlin strain and L. major MRHO/IR/75/ER strain respectively (GenBank accession numbers CP000079.1 and EF653269.1 respectively), isolate 2 and 4 (these two isolates showed complete identical ITS1 sequences) have 96% identity to C. fasciculata(accession number Y00055.1), isolate 3 had 100% identity with many L. tropica strains e.g. L. tropica with GenBank accession number FJ948456.1, isolate 5 was 100% identical to L. infantum MCAN/ES/98/LLM-877 strain (GenBank accession number: AM502245.1), and isolate 6 was 99% identity to L. tropica MHOM/SU/60/OD strain (accession number EU326226.1). It was concluded that isolate 1, 2, 3, 4, 5 and 6 were L. major, C. fasciculata, L. tropica, C. fasciculata, L. infantum, and L. tropica respectively (as are shown in Table 1). It is noteworthy that ITS1 sequences of the two Crithidia isolates were completely identical. This ITS1 sequence (accession number HM004585.1) has 11 different nucleotides in comparison to its closest match in GenBank (C. fasciculata accession number Y00055.1).
Fig. 1.
ITS1 containing sequences of Leishmania species studied in this study
Species identification by isoenzyme electrophoresis
The isolate No. 3 was revealed L. tropica according to ITS1 sequence while it was stated to be L. infantum by the donating institution. Isoenzyme electrophoresis, as the gold standard for species identification, was performed for resolving this discrepancy. Characterization of isolate No. 3, using 4 enzyme systems (GPI, MDH, NH, and PGM), with reference strains indicated that its isoenzyme profile in all 4 enzyme systems is compatible with L. tropica MHOM/IR/72/NADIM3 strain. The isolate No. 5 was revealed L. infantum according to ITS1 sequence and according to data of the donating institution. The isoenzyme electrophoresis was performed for confirmation of species of this isolate. Isoenzyme profile of this isolate was compatible with L. infantum MHOM/TN/80/IPT1 strain using 4 enzyme systems (MDH, GPI, ME, and SOD). Isoenzyme electrophoresis was not done for Crithidia isolates (isolates No. 2 and 4) due to fund restriction and with respect to their lack of clinical relevancy. It is noteworthy that blastocrithidia form of Crithidia was seen in microscopical examination of Geimsa stained slides of the Crithidia isolate (isolate No. 2) whereas no promastigote form of Leishmania was observed in the slides. In addition, intravenous injection of this isolate into golden hamster did not resulted in parasite growth after 6 months.
Discussion
Feasibility of ITS1 sequencing method
Species verification is necessary for isolates of uncertain identity. Isoenzyme electrophoresis is still the gold standard for this purpose (10). This technique has many limitations: it is demanding, laborious, time consuming, requires bulk cultivation of parasites and only specialized laboratories has the expertise to perform this method (10, 15). Molecular methods are increasingly becoming more popular for identification of Leishmania species (10). Amplification of ITS1 by PCR followed by restriction analysis of the amplification product or sequencing is a molecular method that has proved to be useful for species identification of Leishmania isolates (10, 15–20). Advantages of ITS1 sequencing, in comparison to isoenzyme electrophoresis, include: 1) ITS1 sequencing does not need mass cultivation of parasite. The amount of parasite needed for this technique is reported to be as little as 0.2 parasites that can be retrieved through microscopic glass slides used for routine diagnosis of the disease in clinics or filter paper that can be used in remote areas like villages (15). This advantage is especially critical for laboratories lacking cell culture facilities. 2) ITS1 sequencing does not need use of reference Leishmania strains, because this method uses the reliable database of reference strains (e.g. GenBank) for the comparison. This advantage is especially important for laboratories with no access to reference strains or no facilities for their storage. These two advantages of this method show the relative ease of performance of ITS1 sequencing in comparison to the traditional isoenzyme electrophoresis. Our data confirms the relative feasibility of the ITS1 sequencing method in comparison to isoenzyme electrophoresis method.
Pitfall of mixing up or contamination of isolates
Our findings show the possibility of mixing up of Leishmania isolates or contamination with other trypanosomatids (e.g. Crithidia) in the laboratory. Therefore, verification of Leishmania species identity is vital for Leishmania researches especially research involving different species of Leishmania. We studied ITS1 for confirmation of species of 6 Leishmania isolates currently in use in different research laboratories in Iran. The results of ITS1 sequence revealed that species of some isolates were not the assumed species (See Table 1). Isoenzyme electrophoresis confirmed the results of ITS1 sequencing for isolates No. 3 (L. tropica) and No. 5 (L. infantum). So ITS1 sequence and isoenzyme profile show compatible results. Two isolates (No. 2 and 4) were labeled L. infantum while they were C. fasciculata. These two Crithidia isolates have identical ITS1 sequences. This ITS1 sequence (accession number HM004585.1) is novel and has not been already reported. These Crithidia species were stated to be isolated from visceral leishmaniasis patients. Crithidia microorganisms are reported to infect exclusively invertebrates and predominantly insects (21) and we found no report for pathogenicity of this trypanosomatid in humans. The real sources of the Crithidia isolates studied in the present study remain to be identified. The Crithidia has been reported as a contaminant in another study of different Leishmania isolates (22).
Use of ITS1 sequence for species verification
Verification of Leishmania species is needed for isolates of uncertain identity. However, species verification by isoenzyme electrophoresis method is not feasible in many laboratories due to its limitation as discussed above. An important application of our findings is use of ITS1 sequence for verification of Leishmania species. As we know this is the first study to apply ITS1 sequencing for verification of species identity of Leishmania parasites. A shortcoming of our study is the limited number of isolates studied which was due to limitations in fund and manpower. We propose further studies with larger number of isolates for solid conclusion.
In conclusion, our results documented the possibility of mixing up or contamination of Leishmania isolates in the laboratory and confirm the relative feasibility of the ITS1 sequencing in comparison to the isoenzyme electrophoresis for species verification. It is suggested that ITS1 sequencing method, with regard to its high specificity and relative ease of performance, can be used for verification of species of Leishmania isolates of uncertain identity.
Acknowledgement
Helpful advice of Dr Gabriele Schönian (Institute of Microbiology and Hygiene, Charité Universitätsmedizin, Berlin, Germany) for species identification and generous advice and help of Dr Anis Jafari (Molecolar Biology Department, Pasteur Institute of Iran) for molecular methods are highly appreciated. This research received financial supports from Pasteur Institute of Iran (Research Project No. 314). The authors declare that they have no conflicts of interest.
References
- 1.Desjeux P. The increase in risk factors for leishmaniasis worldwide. Trans R Soc Trop Med Hyg. 2001;95(3):239–243. doi: 10.1016/s0035-9203(01)90223-8. [DOI] [PubMed] [Google Scholar]
- 2.Edrissian GH, Nadim A, Alborzi AV, Ardehali S. Visceral leishmaniasis: the Iranian experiences. Arch Iran Med. 1999;1(1):6–22. [Google Scholar]
- 3.Dowlati Y. Cutaneous leishmaniasis: clinical aspect. Clin Dermatol. 1996;14(5):425–431. doi: 10.1016/0738-081x(96)00058-2. [DOI] [PubMed] [Google Scholar]
- 4.Fazaeli A, Fouladi B, Sharifi I. Emergence of cutaneous leishmaniasis in a border area at south-east of Iran: an epidemiological survey. J Vector Born Dis. 2009;46(1):36–42. [PubMed] [Google Scholar]
- 5.Razmjou S, Hejazy H, Motazedian MH, Baghaei M, Emamy M, Kalantary M. A new focus of zoonotic cutaneous leishmaniasis in Shiraz, Iran. Trans R Soc Trop Med Hyg. 2009;103(7):727–730. doi: 10.1016/j.trstmh.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Ardehali S, Moattari A, Hatam GR, Hosseini SMH, Sharifi I. Characterization of Leishmania isolated in Iran: 1. Serotyping with species specific monoclonal antibodies. Acta Tropica. 2000;75(3):301–307. doi: 10.1016/s0001-706x(00)00064-4. [DOI] [PubMed] [Google Scholar]
- 7.Mohebali M. Taxonomy of Leishmania parasites. In: Nadim A, Javadian E, Mohebali M, Momeni AZ, editors. Leishmania parasite and leishmanioses. 3rd ed. Tehran, Iran: Iran University Press; 2008. p. 24. [Google Scholar]
- 8.Evans D. Handbook on isolation, characterization and cryopreservation of Leishmania. Geneva: World Health Organization; 1989. [Google Scholar]
- 9.Reithinger R, Dujardin JC. Molecular diagnosis of leishmaniasis: current status and future applications. J Clin Microbiol. 2007;45(1):21–5. doi: 10.1128/JCM.02029-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schönian G, Mauricio I, Gramiccia M, Cañavate C, Boelaert M, Dujardin JC. Leishmaniases in the Mediterranean in the era of molecular epidemiology. Trends Parasitol. 2008;24(3):135–42. doi: 10.1016/j.pt.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Mahmoudzadeh-Niknam H. Induction of partial protection against Leishmania major in BALB/c mice by Leishmania tropica . Scand J Lab Anim Sci. 2004;31(4):201–207. [Google Scholar]
- 12.Medina-Acosta E, Cross GA. Rapid isolation of DNA from trypanosomatid protozoa using a simple ‘mini-prep’ procedure. Mol Biochem Parasitol. 1993;59(2):327–329. doi: 10.1016/0166-6851(93)90231-l. [DOI] [PubMed] [Google Scholar]
- 13.el Tai NO, Osman OF, el Fari M, Presber W, Schönian G. Genetic heterogeneity of ribosomal internal transcribed spacer in clinical samples of Leishmania donovani spotted on filter paper as revealed by single-strand conformation polymorphisms and sequencing. Trans R Soc Trop Med Hyg. 2000;94(5):575–9. doi: 10.1016/s0035-9203(00)90093-2. [DOI] [PubMed] [Google Scholar]
- 14.Hatam GR, Hosseini SM, Ardehali S. Isoenzyme studies in characterization of Leishmania isolated in Iran. Iran J Med Sci. 1999;24(1&2):8–13. [Google Scholar]
- 15.Schönian G, Nasereddin A, Dinse N, et al. PCR diagnosis and characterization of Leishmania in local and imported clinical samples. Diagn Microbiol Infect Dis. 2003;47(1):349–58. doi: 10.1016/s0732-8893(03)00093-2. [DOI] [PubMed] [Google Scholar]
- 16.Nasereddin A, Bensoussan-Hermano E, Schonian G, Baneth G, Jaffe CL. Molecular Diagnosis of Old World Cutaneous Leishmaniasis and Species Identification by Use of a Reverse Line Blot Hybridization Assay. J Clin Microbiol. 2008;46(9):2848–2855. doi: 10.1128/JCM.00951-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bensoussan E, Nasereddin A, Jonas F, Schnur LF, Jaffe CL. Comparison of PCR assays for diagnosis of cutaneous leishmaniasis. J Clin Microbiol. 2006;44(4):1435–9. doi: 10.1128/JCM.44.4.1435-1439.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar R, Bumb RA, Ansari NA, Mehta RD, Salorta P. Cutaneous leishmaniasis caused by Leishmania tropica in Bikaner, India: parasite identification and characterization using molecular and immunologic tools. Am J Trop Med Hyg. 2007;76(5):896–901. [PubMed] [Google Scholar]
- 19.Strauss-Ayali D, Jaffe CL, Burshtain O, Gonen L, Baneth G. Polymerase chain reaction using noninvasively obtained samples, for the detection of Leishmania infantum DNA in dogs. J Infect Dis. 2004;189(9):1729–33. doi: 10.1086/383281. [DOI] [PubMed] [Google Scholar]
- 20.Marfurt J, Nasereddin A, Niederwieser I, Jaffe CL, Beck HP, Felger I. Identification and Differentiation of Leishmania Species in Clinical Samples by PCR Amplification of the mini exon sequence and subsequent restriction fragment length polymorphism analysis. J Clin Microbiol. 2003;41(7):3147–53. doi: 10.1128/JCM.41.7.3147-3153.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wallace FG. Biology of the Kinetoplastida of arthropods. In: Lumsden WHR, Evans DA, editors. Biology of Kinetoplastida. London: Academic Press; 1979. pp. 213–35. [Google Scholar]
- 22.Tashakori M, Ajdary S, Kariminia A, Mahboudi F, Alimohammadian MH. Characterization of Leishmania species and L. major strains in different endemic areas of cutaneous leishmaniasis in Iran. Iran Biomed J. 2003;7(2):43–50. [Google Scholar]