Abstract
Time of ingestion of hypertension medications can affect circadian patterns of BP, but whether this translates into an effect on clinical outcomes is unknown. Here, in an open-label trial, we randomly assigned 661 patients with CKD either to take all prescribed hypertension medications upon awakening or to take at least one of them at bedtime. We measured 48-hour ambulatory BP at baseline and 3 months after any adjustment in treatment or, at the least, annually. After a median follow-up of 5.4 years, patients who took at least one BP-lowering medication at bedtime had an adjusted risk for total cardiovascular events (a composite of death, myocardial infarction, angina pectoris, revascularization, heart failure, arterial occlusion of lower extremities, occlusion of the retinal artery, and stroke) that was approximately one-third that of patients who took all medications upon awakening (adjusted HR 0.31; 95% CI 0.21 to 0.46; P < 0.001). Bedtime dosing demonstrated a similar significant reduction in risk for a composite outcome of cardiovascular death, myocardial infarction, and stroke (adjusted HR 0.28; 95% CI 0.13 to 0.61; P < 0.001). Furthermore, patients on bedtime treatment had a significantly lower mean sleep-time BP and a greater proportion demonstrated control of their ambulatory BP (56% versus 45%, P = 0.003). Each 5-mmHg decrease in mean sleep-time systolic BP was associated with a 14% reduction in the risk for cardiovascular events during follow-up (P < 0.001). In conclusion, among patients with CKD and hypertension, taking at least one antihypertensive medication at bedtime improves control of BP and reduces the risk for cardiovascular events.
A number of published prospective trials reviewed elsewhere1 have reported clinically meaningful morning-evening, treatment-time differences in BP-lowering efficacy, duration of action, safety profile, and/or effects on the circadian BP pattern for different classes of hypertension medications. For instance, a once-daily evening, in comparison to morning, ingestion schedule of angiotensin receptor blockers and angiotensin-converting enzyme inhibitors results in greater therapeutic effect on sleep-time BP and a significant increase in the sleep-time relative BP decline toward more of a dipping pattern, independent of the terminal half-life of each individual medication.2 Moreover, independent trials have documented that ingesting at least one BP-lowering medication at bedtime, compared with treatment with all medications upon awakening, is associated with increased BP control, significant lowering of sleep-time BP, decrease in the prevalence of nondipping, and reduction of urinary protein excretion.3,4
The impact of bedtime chronotherapy on sleep-time BP regulation might be of clinical importance. This perspective is based on the growing number of studies, all based on ambulatory BP monitoring (ABPM), that have consistently shown that the sleep-time BP mean is a better predictor of cardiovascular disease (CVD) events than the daytime or 24-hour BP means,5–9 a relevant finding also documented for patients with chronic kidney disease (CKD).10,11 A limitation of all of these previous studies on the prognostic value of sleep-time BP is their reliance on a single baseline ABPM profile from each participant at the time of inclusion, without accounting for changes in the BP pattern or level during the years of follow-up. Thus, the potential reduction in CVD risk associated with specifically reducing sleep-time BP is still a matter of debate.11,12
Nocturnal hypertension is not only frequent, but also highly predominant, in patients with CKD.13 Thus, evaluating the potential influence of timed hypertension treatment on sleep-time BP regulation and CVD risk in CKD seems particularly relevant. Accordingly, we prospectively investigated in hypertensive patients with CKD whether bedtime treatment with ≥1 hypertension medications exerts better BP control and CVD risk reduction than treatment with all medications ingested upon waking.14
RESULTS
Demographic Characteristics, Laboratory Variables, and Ambulatory BP
Among the 661 participants in the study, 332 were randomized to ingest all their hypertension medications upon awakening and 329 to ingest ≥1 medications at bedtime. At baseline, the two treatment-time groups were comparable for the prevalence of type 2 diabetes, obstructive sleep apnea, metabolic syndrome, and obesity, plus all anthropometric variables and clinical laboratory test values (Table 1). The clinic BP and ambulatory BP values and prevalence of nondipping at baseline were also comparable between groups (Table 1). The percentage of participants with estimated GFR <60 ml/min per 1.73 m2, albuminuria (albumin excretion ≥30 mg/24-hour urine), or both, was similar in both groups. At the final evaluation, there were no differences in the classes and number of hypertension medications used for therapy between the two treatment groups, except from a slightly lower use of diuretics in patients treated at bedtime (Table 2). The percentage of subjects treated with statins or low-dose aspirin were also similar in both treatment-time groups (Table 2). During follow-up, eGFR was unchanged in participants treated at bedtime (decrease of 0.4 ml/min per 1.73 m2, P = 0.551) and slightly reduced in patients ingesting all medications on awakening (decrease of 2.3 ml/min per 1.73 m2, P = 0.003; P = 0.043 between treatment-time groups). Bedtime treatment was also associated with a greater percent reduction of albumin excretion from baseline (26.9% versus 15.6% in patients on morning treatment, P = 0.018) and reduction in absolute values (median 20.0 and interquartile range, 2.2, 63.2 mg/24-hour urine (P < 0.001 from baseline) versus 4.6 and −1.9, 38.2 mg/24-hour urine (P = 0.012 from baseline) with bedtime and awakening treatment, respectively). A reduction in albumin excretion of >10 mg/24-hour urine during follow-up was documented in 61% of patients treated at bedtime and 39% of those ingesting all medications upon awakening.
Table 1.
Baseline characteristics of patients investigated according to treatment time (either all hypertension medications upon awakening or ≥1 medication at bedtime)
| Variablea | Awakening | Bedtime | P between groups |
|---|---|---|---|
| Demographic characteristics | |||
| Patients (n) | 332 | 329 | |
| eGFR <60 ml/min per 1.73 m2 and albuminuria (n) | 43 | 45 | |
| eGFR ml/min per 1.73 m2 <60 without albuminuria (n) | 120 | 115 | |
| eGFR ml/min per 1.73 m2 >60 and albuminuria (n) | 169 | 169 | |
| Proteinuriab | 13.6 (45) | 15.5 (51) | 0.477 |
| Gender (men)b | 62.9 (209) | 56.8 (187) | 0.109 |
| Diabetesb | 32.8 (109) | 33.7 (111) | 0.805 |
| Obstructive sleep apneab | 14.7 (49) | 12.5 (41) | 0.389 |
| Metabolic syndrome | 72.3 (240) | 70.2 (231) | 0.218 |
| Cigarette smokingb | 16.0 (53) | 14.3 (47) | 0.547 |
| Obesityb | 53.6 (178) | 50.8 (167) | 0.463 |
| Previous CVD eventsb | 6.9 (23) | 7.3 (24) | 0.854 |
| Duration of known hypertension (year) | 6.8 ± 8.3 | 7.1 ± 8.1 | 0.452 |
| Anthropometric variables and office BP | |||
| Age (year) | 60.3 ± 13.6 | 58.5 ± 13.2 | 0.619 |
| Height (cm) | 161.6 ± 9.0 | 161.8 ± 9.7 | 0.736 |
| Weight (kg) | 81.1 ± 16.4 | 80.4 ± 16.3 | 0.589 |
| BMI | 30.9 ± 5.2 | 30.6 ± 5.1 | 0.398 |
| Waist (cm) | 100.6 ± 13.2 | 99.2 ± 11.9 | 0.162 |
| Clinic SBP (mmHg)c | 157.8 ± 23.4 | 158.5 ± 21.4 | 0.658 |
| Clinic DBP (mmHg)c | 87.0 ± 13.5 | 88.8 ± 12.7 | 0.298 |
| Clinical laboratory test values | |||
| Glucose (mg/dl) | 120.3 ± 44.3 | 120.0 ± 45.7 | 0.938 |
| Creatinine (mg/dl) | 1.19 ± 0.40 | 1.15 ± 0.33 | 0.146 |
| Uric acid (mg/dl) | 6.5 ± 2.0 | 6.4 ± 1.7 | 0.173 |
| Total cholesterol (mg/dl) | 210.4 ± 44.5 | 212.0 ± 41.8 | 0.627 |
| Triglycerides (mg/dl) | 132.6 ± 69.5 | 126.1 ± 75.5 | 0.259 |
| HDL-cholesterol (mg/dl) | 44.8 ± 14.3 | 45.6 ± 14.6 | 0.475 |
| LDL-cholesterol (mg/dl) | 139.8 ± 36.0 | 140.6 ± 34.9 | 0.757 |
| Hemoglobin (g/dl) | 14.2 ± 1.9 | 14.1 ± 1.5 | 0.519 |
| Erythrocyte sedimentation rate (mm) | 18.6 ± 18.2 | 17.7 ± 15.7 | 0.453 |
| eGFR (ml/min per 1.73 m2) | 65.8 ± 22.2 | 66.6 ± 21.0 | 0.784 |
| Albumin, mg/24-hour urined | 64.8 (32.1 to 187.8) | 59.2 (31.8 to 210.1) | 0.285 |
| Ambulatory BP | |||
| Awake SBP mean (mmHg) | 137.7 ± 18.4 | 137.4 ± 16.2 | 0.846 |
| Asleep SBP mean (mmHg) | 129.0 ± 20.8 | 128.7 ± 18.5 | 0.871 |
| 48-hour SBP mean (mmHg) | 134.9 ± 18.5 | 134.6 ± 16.0 | 0.836 |
| Sleep-time relative SBP decline (%) | 6.2 ± 8.5 | 6.2 ± 9.1 | 0.950 |
| Awake DBP mean (mmHg) | 80.3 ± 13.0 | 82.5 ± 12.6 | 0.558 |
| Asleep DBP mean (mmHg) | 71.2 ± 12.3 | 73.0 ± 11.3 | 0.128 |
| 48-hour DBP mean (mmHg) | 77.4 ± 12.4 | 79.4 ± 11.7 | 0.342 |
| Sleep-time relative DBP decline (%) | 11.1 ± 9.5 | 11.1 ± 8.9 | 0.942 |
| Nondipper (%) | 67.8 | 65.1 | 0.458 |
a Values are shown as mean ± SD. eGFR, estimated GFR (ml/min per 1.73 m2) using the MDRD-4 equation.15 Albuminuria, urinary albumin excretion ≥30 mg/24-hour urine. Proteinuria, urinary albumin excretion ≥300 mg/24-hour urine. Metabolic syndrome: National Cholesterol Education Program Adult Treatment Panel III (ATP-III) revised definition.16 Obesity, body mass index (BMI) ≥30, calculated as weight in kilograms divided by height in meters squared (kg/m2). The sleep-time relative BP decline, an index of BP dipping, is defined as the percent decline in mean BP during night-time sleep relative to the mean BP during daytime activity and was calculated as follows: [(awake BP mean − asleep BP mean)/awake BP mean] × 100. Nondipper, patients with sleep-time relative SBP decline <10%, using data sampled by ABPM for 48 consecutive hours.
b Values are percentages with number of subjects in parentheses.
c Values correspond to the average of six conventional BP measurements obtained for each subject at the clinic before starting 48-hour ABPM.
d Values are medians with interquartile range in parentheses.
Table 2.
Final characteristics of patients investigated according to treatment time (either all hypertension medications upon awakening or ≥1 medication at bedtime)
| Variablea | Awakening (n = 332) | Bedtime (n = 329) | P between groups |
|---|---|---|---|
| Hypertension treatment | |||
| Number of medications | 2.3 ± 1.1 | 2.2 ± 1.5 | 0.544 |
| 1 medication (%) | 31.9 | 37.7 | 0.119 |
| 2 medications (%) | 19.0 | 13.7 | 0.066 |
| ≥3 medications (%) | 49.1 | 48.6 | 0.902 |
| ARB (%) | 55.4 | 58.7 | 0.481 |
| ACEI (%) | 21.7 | 17.0 | 0.130 |
| CCB (%) | 48.2 | 52.3 | 0.285 |
| α-blocker (%) | 25.6 | 27.4 | 0.633 |
| ß-blocker (%) | 19.9 | 21.3 | 0.692 |
| Diuretic (%) | 59.6 | 49.5 | 0.010 |
| Other medications | |||
| Statins (%) | 32.5 | 30.4 | 0.554 |
| Low-dose aspirinb (%) | 15.7 | 15.2 | 0.869 |
| Clinic and ambulatory BP | |||
| Clinic SBP (mmHg)c | 146.8 ± 24.6 | 146.7 ± 21.1 | 0.953 |
| Clinic DBP (mmHg)c | 80.5 ± 14.8 | 82.2 ± 13.4 | 0.112 |
| Awake SBP mean (mmHg) | 128.3 ± 17.7 | 129.3 ± 15.2 | 0.419 |
| Asleep SBP mean (mmHg) | 122.6 ± 21.3 | 116.7 ± 16.8 | <0.001 |
| 48-hour SBP mean (mmHg) | 126.5 ± 17.8 | 125.4 ± 15.0 | 0.384 |
| Sleep-time relative SBP decline (%) | 4.4 ± 9.8 | 9.7 ± 7.7 | <0.001 |
| Awake DBP mean (mmHg) | 73.4 ± 11.8 | 76.8 ± 11.9 | <0.001 |
| Asleep DBP mean (mmHg) | 66.3 ± 12.0 | 65.2 ± 10.5 | 0.205 |
| 48-hour DBP mean (mmHg) | 71.1 ± 11.4 | 73.1 ± 11.1 | 0.024 |
| Sleep-time relative DBP decline (%) | 9.3 ± 11.4 | 14.7 ± 8.8 | <0.001 |
| Nondipper (%) | 71.1 | 41.0 | <0.001 |
| Controlled ambulatory BP (%) | 45.2 | 56.5 | 0.003 |
| Controlled awake BP (%) | 67.2 | 64.1 | 0.411 |
| Controlled asleep BP (%) | 54.8 | 67.2 | <0.001 |
a Values are shown as mean ± SD; n is number of patients. The sleep-time relative BP decline, an index of BP dipping, is defined as the percent decline in mean BP during nocturnal sleep relative to the mean BP during daytime activity and is calculated as follows: [(awake BP mean − asleep BP mean)/awake BP mean] × 100. Nondipper, patients with sleep time relative to SBP decline <10%, using data sampled ABPM for 48 consecutive hours. ARB, angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; CCB, calcium channel blocker.
b Aspirin dosage was 100 mg/d.
c Values correspond to the average of six conventional BP measurements obtained for each subject at the clinic before starting 48-hour ABPM.
The data of the last evaluation revealed differences between the two treatment-time groups that were significant after correction for multiple testing. The group of patients ingesting ≥1 medication at bedtime showed significantly lower asleep, but not awake, systolic BP (SBP) mean than the group of subjects ingesting all their medications upon awakening (P < 0.001; Table 2). The sleep-time relative decline of both SBP and diastolic BP (DBP) was significantly greater among participants ingesting ≥1 medication at bedtime; accordingly, the proportion of patients in this treatment-time group with a nondipper BP profile (sleep-time SBP decline <10%) was significantly lower than that in the upon-awakening treatment-time group, 41.0% (95% confidence interval [CI] 35.7% to 46.3%) versus 71.1% (66.2% to 76.0%; P < 0.001) between groups. Finally, the proportion of patients with controlled BP, with reference to established ABPM criteria for both awake and asleep BP mean, was significantly greater among participants ingesting ≥1 medication at bedtime than in those ingesting all medications upon awakening (56.5% [51.2% to 61.9%] versus 45.2% [39.8% to 50.5%]; P = 0.003; Table 2). This difference in ambulatory BP control was mainly due to improved sleep-time BP control in patients treated at bedtime. Thus, whereas the percentage of patients with controlled awake BP mean was similar for both treatment-time groups (P = 0.411), asleep BP mean was controlled in a significantly larger percentage of patients treated at bedtime (67.2% [62.1% to 72.2%] versus 54.8% [49.5% to 60.2%]; P < 0.001, Table 2).
CVD Risk According to Time-of-Day of Hypertension Treatment
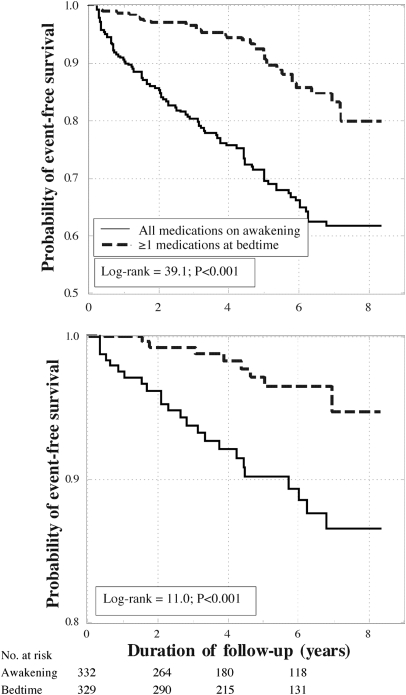
During the median follow-up period of 5.4 years (range 0.5 to 8.4 years), we documented 139 events (21 deaths, 21 myocardial infarctions, 21 angina pectoris, 16 coronary revascularizations, 6 cerebrovascular events, 35 heart failures, eight cases of aortoiliac occlusive disease, and 11 thrombotic occlusions of the retinal artery; Table 3). Figure 1 presents, for total (top) and major (bottom) events, the Kaplan-Meier survival curves for the patients of the two treatment-time groups; a highly significant difference was detected in event-free survival (log-rank 39.1 and 11.0 for total and major events, respectively; P < 0.001). Table 3 provides further information on the distribution of the CVD events in both treatment-time groups.
Table 3.
Event rates for primary and secondary end points according to treatment time (either all hypertension medications upon awakening or ≥1 medication at bedtime)
| Variablea | Awakeningb (n = 332) | Bedtimeb (n = 329) | P between groupsc |
|---|---|---|---|
| Primary end points | |||
| Total events | 57.9 (48.6 to 67.1); 104 | 19.8 (13.6 to 26.0); 35 | <0.001 |
| Major events | 14.5 (9.1 to 19.8); 26 | 5.1 (1.8 to 8.4); 9 | <0.001 |
| Secondary end points | |||
| Total death | 7.8 (3.8 to 11.8); 14 | 4.0 (1.0 to 6.8); 7 | 0.056 |
| Cardiovascular death | 3.9 (1.0 to 6.8); 7 | 1.1 (0.0 to 2.7); 2 | 0.059 |
| Other cause | 3.9 (1.0 to 6.8); 7 | 2.8 (0.4 to 5.3); 5 | 0.758 |
| Cardiovascular events | 26.1 (19.2 to 33.1); 47 | 6.2 (2.6 to 9.8); 11 | <0.001 |
| Myocardial infarction | 8.9 (4.7 to 13.2); 16 | 2.8 (0.4 to 5.3); 5 | 0.005 |
| Angina pectoris | 10.0 (5.5 to 1.45); 18 | 1.7 (0.1 to 3.6); 3 | <0.001 |
| Revascularization | 7.2 (3.4 to 11.1); 13 | 1.7 (0.1 to 3.6); 3 | 0.004 |
| Cerebrovascular events | 2.2 (0.3 to 4.4); 4 | 1.1 (0.0 to 2.7); 2 | 0.310 |
| Heart failure | 15.0 (9.6 to 20.5); 27 | 4.5 (1.4 to 7.6); 8 | <0.001 |
| Other events | 6.7 (3.0 to 10.4); 12 | 0.0 (1.0 to 6.8); 7 | 0.119 |
a Total events include the following: death (from all causes), cardiovascular events (myocardial infarction, angina pectoris, and coronary revascularization), cerebrovascular events (stroke and transient ischemic attack), heart failure, and other events (acute arterial occlusion of lower extremities and thrombotic occlusion of the retinal artery). Major events include the following: cardiovascular deaths, myocardial infarction, ischemic stroke, and hemorrhagic stroke.
b Event rates (with 95% CIs in parentheses, followed by the actual number of events) are expressed as the number/1000 patient-years, i.e., a ratio of the observed number of events to the total number of patient-years of exposure.
c Comparison of event rates between treatment time groups was done by the Mantel log-rank test.
Figure 1.
Kaplan-Meier survival curves as a function of time-of-day of hypertension treatment, i.e., for patients with CKD ingesting either all their BP-lowering medications upon awakening or ≥1 medication at bedtime, for total CVD events (top) and major CVD events (cardiovascular deaths, myocardial infarction, ischemic stroke, and hemorrhagic stroke; bottom).
Figure 2 shows the hazard ratios (hazards ratio [HR], with 95% CI) of CVD events estimated by the Cox proportional-hazard model for the participants of the respective treatment-time groups. Adjustments were applied for sex, age, and diabetes in all comparisons, because these influential factors, among all of the demographic and laboratory variables shown in Table 1, were consistently significant in all tested Cox regression models. Patients ingesting ≥1 BP-lowering medication at bedtime evidenced a significantly lower HR of total events than participants ingesting all of their medications upon awakening (0.31 [0.21 to 0.46]; P < 0.001). Particularly relevant is the difference between the two treatment-time groups in the adjusted HR of major CVD events (0.28 [0.13 to 0.61]; P < 0.001). Despite the relatively limited sample size for analysis of individual secondary end points, results document significant reductions in the HR of myocardial infarction, angina pectoris, coronary revascularization, and heart failure with bedtime treatment (Figure 2). The incidence of stroke was rather small in both treatment-time groups.
Figure 2.
Hazard ratios (with 95% confidence intervals) of CVD events (adjusted by age, sex, and diabetes) as a function of time-of-day of hypertension treatment, i.e., for patients with CKD ingesting either all their BP-lowering medication upon awakening or ≥1 medication at bedtime. Total events include the following: death (from all causes), cardiovascular events (myocardial infarction, angina pectoris, and coronary revascularization), cerebrovascular events (stroke and transient ischemic attack), heart failure, acute arterial occlusion of lower extremities, and thrombotic occlusion of the retinal artery. Major events include: cardiovascular deaths, myocardial infarction, ischemic stroke, and hemorrhagic stroke.
Changes in Clinic and Ambulatory BP during Follow-Up as Predictors of Event-Free Survival
The results shown in Table 2 indicate that those patients randomized to ingest ≥1 medication at bedtime experienced significantly better sleep-time BP control. Most important, only 14.4% (95% CI 8.6% to 20.2%) of the subjects who experienced a CVD event had their sleep-time BP properly controlled (<120/70 for SBP/DBP17), whereas 83.5% (95% CI 77.3% to 89.6%) of the event-subjects had a nondipper BP profile. Accordingly, we further evaluated the influence on CVD risk of changes in ambulatory BP during follow-up. Cox regression analyses (using the change in BP during follow-up as a time-dependent covariate, and adjusted for sex, age, diabetes, number of hypertension medications used for treatment, and baseline BP) revealed that the progressive decrease in asleep SBP mean during follow-up was most significantly associated with event-free survival (HR 0.86 [0.77 to 0.96], P < 0.001, for every 5-mmHg decrease in asleep SBP mean), whereas the decrease in awake SBP mean was not (0.95 [0.87 to 1.04], P = 0.247). The reduction of albumin excretion during follow-up was not a significant predictor of survival (P = 0.172) in a Cox model also including changes in asleep SBP mean from baseline.
The top panel in Figure 3 shows, for the studied population divided in five classes of equal size (quintiles), the significant relationship between progressively lower achieved asleep SBP mean and reduced risk of CVD events. Adjusted HR was significantly higher (P always <0.014) in the three middle quintiles compared with the first class and in the last quintile compared with any other class. There was a progressive reduction from 60% to 32% in the percentage of patients treated at bedtime across the quintiles, indicating the association between bedtime treatment, enhanced sleep-time BP reduction, and decreased CVD risk. Figure 3 (bottom), on the contrary, shows a J-shaped relationship between achieved clinic SBP and CVD risk; the adjusted HR was lowest in the second quintile (achieved clinical SBP 131 to 142 mmHg) and then progressively increased in the other classes (P = 0.021 between the second and the last quintile). The percentage of patients treated with ≥1 hypertension medication at bedtime was lower (43%) in the first than in the second quintile (58%; P = 0.018).
Figure 3.
Hazard ratio of CVD events (adjusted by age, sex, diabetes, and number of hypertension medications used for treatment) as a function of achieved asleep SBP mean (top) and achieved daytime-determined clinic SBP (bottom) at the time of the last ABPM evaluation. The studied population was divided into five classes of equal size (quintiles).
DISCUSSION
This study prospectively investigated in hypertensive patients with CKD the hypothesis that bedtime treatment with ≥1 hypertension medication exerts better BP control and CVD risk reduction than morning-only dosing. The results document, first, greater ambulatory BP control in patients ingesting ≥1 hypertension medication at bedtime than in those ingesting all their medications upon awakening. The main differences between groups in terms of BP control were achievement in patients treated at bedtime of (1) significantly lower asleep BP mean and (2) greater sleep-time relative BP decline, without loss of awake BP-lowering efficacy (Table 2). These treatment-time-dependent effects on sleep-time BP control were strongly associated with lower risk of CVD events. Indeed, the progressive reduction in the asleep BP mean from baseline was the most significant predictor of event-free survival. Moreover, lack of sleep-time BP control with reference to established ABPM criteria17 and a nondipper BP pattern were the most prevalent factors among event-patients. As documented in a series of prospective controlled trials reviewed elsewhere.1,2 and also as corroborated in the long-term evaluation provided here, treatment at bedtime is the most cost-effective and simplest strategy of successfully achieving the therapeutic goals of adequate asleep BP reduction and preserving or re-establishing the normal 24-hour BP dipping pattern. One could thus conclude that the increased event-free survival associated with bedtime-treatment with ≥1 BP-lowering medication, compared with upon-waking ingestion of all medications, is somehow linked to better achievement of these novel hypertension therapeutic goals.
Apart from the prognostic value of ABPM-derived asleep BP mean, international guidelines also recognize albuminuria as a marker of target organ damage and CVD risk.17 We previously demonstrated that urinary albumin excretion was significantly reduced after bedtime, but not morning, treatment with valsartan.18 This reduction was independent of changes in 24-hour BP with treatment, but significantly correlated with the decrease in asleep BP mean and increase in sleep-time relative BP decline, both therapeutic targets being better achieved with bedtime than morning ingestion of valsartan.18 Another recent small study3 reported similar findings, namely significant reduction of asleep BP mean and decreased urinary albumin excretion, after shifting one BP-lowering medication from morning to evening in 32 uncontrolled nondipper patients with CKD. In the trial reported here, albumin was greatly reduced in patients ingesting ≥1 hypertension medication at bedtime than in those ingesting all medications upon awakening. However, change in albumin during follow-up was not a significant predictor of outcome when the reduction in asleep BP mean was included as a confounding variable in the Cox survival analysis.
Therapeutic intervention in hypertension consists of adequate control of BP, the goal being to reduce/avert CVD morbidity and mortality. BP control has been mainly defined so far on the unique basis of lowering BP level (mainly if not exclusively determined conventionally at the clinic), without paying attention to potential alterations in the circadian BP pattern due to treatment.19,20 Some studies found that too high a reduction in clinic BP might be associated with increased CVD risk, whereas moderate reduction in BP would decrease the risk. Thus, it has been suggested that CVD outcomes have a J-shaped relationship to BP, decreasing as BP was lowered and rising again as BP decreased further.19–22 This concept has generated a widely open discussion and concern, leading to recommendations to lower BP only to a certain level (140/90 mmHg for clinic SBP/DBP), even in patients at high risk such as those with diabetes19 or CKD.20
We also found a J-shaped association in the relation of CVD risk with achieved clinic BP (Figure 3, bottom), but not with achieved asleep BP mean (Figure 3, top), as risk decreased with progressive diminished asleep BP. Moreover, the amount of the asleep BP reduction during follow-up was associated with increased number of patients treated at bedtime, whereas greater clinic BP reduction (first quintile in Figure 3, bottom) was associated with over-treatment in the morning. It has being previously shown that increasing number of hypertension medications administered in the morning may lead to more intensive clinic BP reduction, but also to an increased prevalence of nondipping as a consequence of the greater reduction in awake than asleep BP.4 We thus conclude that the actual controversy on the possible J-shaped relation with CVD risk, described so far only for clinic BP determined in patients, including those with CKD, presumably treated in the morning,19–22 might not apply (when avoiding nocturnal hypotension) to asleep BP, a most significant predictor of CVD morbidity and mortality that can be cost-effectively modified by properly timed treatment,1,2 as also documented here in patients with CKD.
Our study has some potential limitations. First, compared with other larger multicenter clinical trials on hypertensive patients entailing only clinic BP measurement during follow-up, the sample size of our ABPM-based, single-center study might seem a limitation. However, the number of patients participating in our study was considerably greater than that of most other published trials on the prognostic value of ABPM in patients with CKD10,11 and was sufficient according to the statistical significance of the reported results. Second, the sample size of the trial is limited to derive definitive conclusions from the comparison between classes of medications on the benefits, in terms of CVD risk reduction, of bedtime treatment. Finally, the use of a prospective, randomized, open-label, blinded end point (PROBE) design might also be considered a limitation. However, the PROBE design was specifically developed for the conduct of long-term morbidity and mortality trials. Nonetheless, the design of our study also incorporates several strengths. Although all previous trials on the prognostic value of ABPM relied on a single baseline profile from each participant, our study is the first to provide results that are based on systematic periodic multiple evaluations by ABPM throughout the median 5.4 years of follow-up. This so-far unique approach allowed first-time determination of the influence on CVD risk of specific changes during follow-up in ambulatory BP. Further strengths of our study are the use of (1) 48-hour, instead of the most common 24-hour ABPM sampling, to increase the reproducibility of the BP findings;23 and (2) wrist actigraphy to precisely and individually determine the beginning and end of the activity and sleep spans for each subject to enable accurate calculation of the awake and asleep BP means, sleep-time relative BP decline, and type of dipping pattern.
In conclusion, our findings document that, in hypertensive patients with CKD, a bedtime schedule with ≥1 BP-lowering medication, in comparison to a schedule in which all such medications are ingested upon awakening, not only significantly and cost-effectively improves BP control, but it significantly reduces CVD risk. Our results also document that reducing the asleep BP mean, while avoiding nocturnal hypotension, a novel therapeutic target requiring proper patient evaluation by ABPM, significantly decreases CVD morbidity and mortality in patients with CKD.
CONCISE METHODS
Inclusion and Exclusion Criteria
The sample represents a population of hypertensive patients of both sex, ≥18 years of age, and with CKD, defined as either eGFR <60 ml/min per 1.73 m2, albuminuria (urinary albumin excretion ≥30 mg/24-hour urine) or both, in at least two occasions ≥3 months apart.24 Exclusion criteria were pregnancy, history of drug or alcohol abuse, night- or shift-work employment, AIDS, type 1 diabetes, secondary hypertension, CVD disorders (unstable angina pectoris, heart failure, life-threatening arrhythmia, atrial fibrillation, kidney failure, and grade III–IV retinopathy), intolerance to ABPM measurement, and inability to communicate and comply with all of the study requirements. This prospective single-center study (registered at www.clinicaltrials.gov, NCT00295542) was approved by the state Ethics Committee of Clinical Research. All subjects gave written informed consent.
Subjects and Diagnostic Criteria
For the specific hypothesis tested here (influence of time of hypertension treatment on cardiovascular risk in CKD), between 2000 and 2007 we assessed 695 patients with CKD fulfilling the inclusion/exclusion criteria. Among these, 661 (396 men/265 women, 59.2 ± 13.5 [mean ± SD] years of age) provided all required information for the study. A total of 34 patients evaluated by ABPM for potential inclusion were not randomized because of their lack of consent for additional ABPM evaluations. Diagnosis of hypertension was based on accepted ABPM criteria: an awake BP mean ≥135/85 mmHg for SBP/DBP or an asleep BP mean ≥120/70 mmHg.17
Study Design
This was a PROBE trial. Participants were randomized to ingest all their prescribed BP-lowering medications upon awakening or ≥1 of them at bedtime.12,14 Randomization of participants to treatment time (awakening or bedtime) was done separately for each allowed individual hypertension medication (the angiotensin-receptor blockers valsartan, telmisartan, and olmesartan; the angiotensin-converting enzyme inhibitors ramipril and spirapril; and the calcium channel blockers amlodipine and nifedipine gastrointestinal therapeutic system). This ensured that the proportion of patients treated with each medication was similar across the morning and bedtime treatment arms of the study. The protocol did not allow dividing any prescribed medication in two or more doses. Thus, patients randomized to the bedtime-treatment group were never ingesting in the morning any of the medications ingested at bedtime.
Blood samples were obtained between 0800 and 0900, after overnight fasting, the same week when each 48-hour ABPM session was initiated. The subjects collected their urine during the first 24-hour of ABPM for determination of albumin excretion in 24-hour urine. Just before commencing ABPM, six clinic BP measurements were obtained with a validated automatic oscillometric device (HEM-705IT, Omron Health Care Inc., Vernon Hills, Illinois) after the subject had rested in a seated position for ≥10 minutes.
ABPM Assessment
At inclusion, as well as at each scheduled visit for ABPM during follow-up (see below), the SBP and DBP of each patient were automatically measured every 20 minutes between 0700 and 2300 and every 30 minutes during the night for 48 consecutive hours with a calibrated SpaceLabs 90207 ABPM monitor (SpaceLabs Inc., Issaquah, Washington). BP series were considered invalid for analysis if ≥30% of the measurements were missing, if data were lacking for an interval of >2 hours, if data were obtained while patients had an irregular rest-activity schedule during the 2 days of monitoring, or if the nighttime sleep period was <6 or >12 hours during ABPM.
Actigraphy
All patients wore an actigraph (Mini-Motion-Logger, Ambulatory Monitoring Inc., Ardsley, New York) on the dominant wrist to monitor physical activity every minute during ABPM. The actigraphy data, combined with patient diaries, were used to define the commencement and termination of the daytime awake and nocturnal asleep spans so the respective BP means for each subject could be accurately determined.
Follow-Up
The same evaluation procedure described above, including conventional clinic BP measurement, 48-hour ABPM and wrist activity monitoring, was scheduled annually, or more frequently (after 3 months of any change in treatment) if the therapeutic scheme was modified to improve ambulatory BP control. Investigators blinded to the timed-treatment scheme of each participant (excluding those performing clinic evaluation at each visit to the hospital, clinic, and ambulatory BP measurement, and/or statistical analyses) reviewed at least annually the complete clinical records of all enrolled patients to assess CVD morbidity and mortality. Registered events included the following: death from all causes, myocardial infarction, angina pectoris, coronary revascularization, heart failure, acute arterial occlusion of lower extremities, thrombotic occlusion of the retinal artery, hemorrhagic stroke, ischemic stroke, and transient ischemic attack.
Statistical Methods
The primary outcomes study end point was total CVD morbidity and mortality, which included all of the events listed above. We also used as an additional end point major CVD events, i.e., a composite of CVD deaths, myocardial infarction, and stroke. Demographic and clinical characteristics were compared on an intention-to-treat basis among groups of participants randomized to the two treatment-time groups by two-sided t test (continuous variables) or nonparametric chi-squared test (proportions). The Cox proportional-hazard model was used to estimate HR, with 95% CI, for events associated with time of treatment, with adjustment for significant confounding variables. Event rates for CVD events during follow-up were also expressed as the number/1000 patient-years, i.e., ratio of the observed number of events to the total number of patient-years of exposure. Survival curves were generated using the Kaplan-Meier product-limit method and compared by the Mantel log-rank test.
DISCLOSURES
None.
Supplementary Material
Acknowledgments
This independent investigator-promoted research was supported by unrestricted grants from Ministerio de Ciencia e Innovación (SAF2006-6254-FEDER; SAF2009-7028-FEDER); Consellería de Presidencia, Relacións Institucionais e Administración Pública, Secretaría Xeral de Investigación e Desenvolvemento, Xunta de Galicia (PGIDIT03-PXIB-32201PR); Consellería de Economía e Industria, Dirección Xeral de Investigación e Desenvolvemento, Xunta de Galicia (INCITE07-PXI-322003ES; INCITE08-E1R-322063ES; INCITE09-E2R-322099ES; 09CSA018322PR); and Vicerrectorado de Investigación, University of Vigo.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Chronotherapy in Hypertension: A Pill at Night Makes Things Right?,” on pages 2152–2155.
Supplemental information for this article is available online at http://www.jasn.org/.
REFERENCES
- 1. Smolensky MH, Hermida RC, Ayala DE, Tiseo R, Portaluppi F: Administration-time-dependent effect of blood pressure-lowering medications: Basis for the chronotherapy of hypertension. Blood Press Monit 15: 173–180, 2010 [DOI] [PubMed] [Google Scholar]
- 2. Hermida RC, Ayala DE, Fernández JR, Portaluppi F, Fabbian F, Smolensky MH: Circadian rhythms in blood pressure regulation and optimization of hypertension treatment with ACE inhibitor and ARB medications. Am J Hypertens 24: 383–391, 2011 [DOI] [PubMed] [Google Scholar]
- 3. Minutolo R, Gabbai FB, Borrelli S, Scigliano R, Trucillo P, Baldanza D, Laurino S, Mascia S, Conte G, De Nicola L: Changing the timing of antihypertensive therapy to reduce nocturnal blood pressure in CKD: An 8-week uncontrolled trial. Am J Kidney Dis 50: 908–917, 2007 [DOI] [PubMed] [Google Scholar]
- 4. Hermida RC, Ayala DE, Fernández JR, Calvo C: Chronotherapy improves blood pressure control and reverts the nondipper pattern in patients with resistant hypertension. Hypertension 51: 69–76, 2008 [DOI] [PubMed] [Google Scholar]
- 5. Kikuya M, Ohkubo T, Asayama K, Metoki H, Obara T, Saito S, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y: Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality. The Ohasama Study. Hypertension 45: 240–245, 2005 [DOI] [PubMed] [Google Scholar]
- 6. Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M: Predictors of all-cause mortality in clinical ambulatory monitoring. Unique aspects of blood pressure during sleep. Hypertension 49: 1235–1241, 2007 [DOI] [PubMed] [Google Scholar]
- 7. Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Kuznetsova T, Torp-Pedersen CH, Lind L, Ibsen H, Imai Y, Wang J, Sandoya E, O'Brien E, Staessen JA: Prognostic accuracy of day versus night ambulatory blood pressure: A cohort study. Lancet 370: 1219–1229, 2007 [DOI] [PubMed] [Google Scholar]
- 8. Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA: Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 51: 55–61, 2008 [DOI] [PubMed] [Google Scholar]
- 9. Fan HQ, Li Y, Thijs L, Hansen TW, Boggia J, Kikuya M, Björklund-Bodegard K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Ibsen H, O'Brien E, Wang J, Staessen JA: Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J Hypertens 28: 2036–2045, 2010 [DOI] [PubMed] [Google Scholar]
- 10. Agarwal R, Andersen MJ: Prognostic importance of ambulatory blood pressure recordings in patients with chronic kidney disease. Kidney Int 69: 1175–1180, 2006 [DOI] [PubMed] [Google Scholar]
- 11. Agarwal R, Peixoto AJ, Santos SFF, Zoccali C: Out-of-office blood pressure monitoring in chronic kidney disease. Blood Press Monit 14: 2–11, 2009 [DOI] [PubMed] [Google Scholar]
- 12. Hermida RC, Ayala DE, Mojón A, Fernández JR: Influence of circadian time of hypertension treatment on cardiovascular risk: Results of the MAPEC study. Chronobiol Int 27: 1629–1651, 2010 [DOI] [PubMed] [Google Scholar]
- 13. Pogue V, Rahman M, Lipkowitz M, Toto R, Miller E, Faulkner M, Rostand S, Hiremath L, Sika M, Kendrick C, Hu B, Greene T, Appel L, Phillips RA: African American Study of Kidney Disease and Hypertension Collaborative Research Group. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension 53: 20–27, 2009 [DOI] [PubMed] [Google Scholar]
- 14. Hermida RC: Ambulatory blood pressure monitoring in the prediction of cardiovascular events and effects of chronotherapy: Rationale and design of the MAPEC study. Chronobiol Int 24: 749–775, 2007 [DOI] [PubMed] [Google Scholar]
- 15. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. for the Modification of Diet in Renal Disease Study Group: A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med 130: 461–470, 1999 [DOI] [PubMed] [Google Scholar]
- 16. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Frauss RM, Savage PJ, Smith SC, Spertus JA, Costa F: Diagnosis and management of the metabolic syndrome. An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112: 2735–2752, 2005 [DOI] [PubMed] [Google Scholar]
- 17. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker HAJ, Zanchetti A: 2007 guidelines for the management of arterial hypertension. The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 25: 1105–1187, 2007 [DOI] [PubMed] [Google Scholar]
- 18. Hermida RC, Calvo C, Ayala DE, López JE: Decrease in urinary albumin excretion associated to the normalization of nocturnal blood pressure in hypertensive subjects. Hypertension 46: 960–968, 2005 [DOI] [PubMed] [Google Scholar]
- 19. Cushman WC, Evans GW, Byington RP, Goff DC, Jr., Grimm RH, Jr., Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F. ACCORD Study Group: Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 362: 1575–1585, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Appel LJ, Wright JT, Jr., Greene T, Agodoa LY, Astor BC, Bakris GL, Cleveland WH, Charleston J, Contreras G, Faulkner ML, Gabbai FB, Gassman JJ, Hebert LA, Jamerson KA, Kopple JD, Kusek JW, Lash JP, Lea JP, Lewis JB, Lipkowitz MS, Massry SG, Miller ER, Norris K, Phillips RA, Pogue VA, Randall OS, Rostand SG, Smogorzewski MJ, Toto RD, Wang X; AASK Collaborative Research Group: Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med 363: 918–929, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vokó Z, Bots ML, Hofman A, Koudstaal PJ, Witteman JCM, Breteler MMB: J-shaped relation between blood pressure and stroke in treated hypertensives. Hypertension 34: 1181–1185, 1999 [DOI] [PubMed] [Google Scholar]
- 22. Okumura K, Ohya Y, Maehara A, Wakugami K, Iseki K, Takishita S: Effects of blood pressure levels on case fatality after acute stroke. J Hypertens 23: 1217–1223, 2005 [DOI] [PubMed] [Google Scholar]
- 23. Hermida RC, Calvo C, Ayala DE, Fernández JR, Ruilope LM, López JE: Evaluation of the extent and duration of the “ABPM effect” in hypertensive patients. J Am Coll Cardiol 40: 710–717, 2002 [DOI] [PubMed] [Google Scholar]
- 24. National Kidney Foundation K/DOQI clinical practice guidelines on chronic kidney disease: Evaluation, classification and stratification. Am J Kidney Dis 39(2 Suppl 1): S1–S266, 2002 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.