Abstract
Purpose
This study examined responses of persons with aphasia (PWAs) to a general question about their speech. The goal was to describe their evaluative responses as positive, negative, or neutral/mixed and determine if responses differed, based on time post-onset, aphasia severity, and aphasia type.
Methods
71 participants from the AphasiaBank project were included. As part of a larger protocol, investigators asked, “How do you think your speech is these days?” Responses were videotaped and transcribed using CLAN. Two authors coded the evaluative responses and categorized themes in the elaborative content provided by the participants.
Results
Positive responses accounted for 59% of all responses, followed by neutral/mixed (18%), and negative (17%). Participants also mentioned specific speech problems (35%), improvement (31%), and therapy (8%) in their responses. Time post-onset and aphasia type were not significantly associated with nature of response. Aphasia severity was significantly associated with nature of response, with higher AQ scores in the positive group and vice versa.
Conclusions
The responses are discussed in the context of self-image and self-expression in PWA and social models in aphasia therapy. Results are also compared with those of others with chronic disabilities and research on resilience, positive affect, and optimism.
The increasing focus on discourse in aphasiology research attests to the fact that connected speech samples across a variety of contexts reveal important information about the aphasic speaker’s linguistic and cognitive abilities, personal and social insights related to identity, adjustment to aphasia, and interactional skills (Hinckley, 2006; Shadden & Hagstrom, 2007; Simmons-Mackie & Damico, 2009). To date, discourse samples used in aphasia research have included both monologic recounts of significant events in the person’s life and dialogues about everyday activities and interests. Examples of such monologues include recounts of: 1) frightening events (Behrns, Wengelin, Broberg, & Hartelius, 2009; Olness, Matteson, & Stewart, 2010; Ulatowska & Olness, 2001; Ulatowska & Olness, 2003); 2) positive events such as a wedding or holiday (Armstrong, 2001); and 3) illness, particularly related to stroke stories (Armstrong & Ulatowska, 2007; Hinckley, 2006; Ulatowska, Olness, Keebler, & Tillery, 2006). Dialogic interactions have covered a variety of topics and occur in contexts such as aphasia groups or private homes (Beeke, Wilkinson, & Maxim, 2009; Oeschlager & Thorne, 1999; Simmons-Mackie & Damico, 2009). Nonetheless, by far the majority of work in aphasic discourse (in both research and clinical practice) tends to look at discourse involving picture descriptions, story retell, and procedural discourse. These all involve third-person-focused language dealing with almost anything but the life experiences of persons with aphasia (PWAs), topics familiar or interesting to them, or their (possibly emotionally tinged) attitudes.
Interest in including relevant personal experience in clinical and research discourse sampling methods parallels the emergence of social models for aphasia, which have gained traction in aphasia assessment and treatment in the last 10 years (Byng & Duchan, 2005; Elman, 2005; Simmons-Mackie, et al., 2007). Stemming from such models, there has been increasing advocacy to empower PWAs to play a role in the management of their own disorders and to equalize the social relations involved in service delivery. Empowerment includes altering the interactions between clinician/investigator and client/participant by asking genuine, information-seeking questions of PWAs regarding their speech, their strokes, and their recoveries. In this way, parity in clinical conversations can be restored.
Several researchers (e.g., Hagstrom, 2004; Holland, 2007; Pound, Parr, Lindsay, & Woolf, 2000; Shadden, Hagstrom, & Koski, 2008) have investigated the telling of personal stroke narratives in aphasia therapy situations and have discussed the benefits of such narratives. All agree that narratives present people with aphasia (similar to other individuals suffering from a chronic illness) with an opportunity to talk about their problems and, thereby, help to reestablish a more positive sense of self and diminish what Shadden (2005) called “identity theft”. The role of the speech-language pathologist in this context is that of an active listener, “co-constructing clinical interactions in such a way as to create authentic relationships aimed at effecting relevant change” (Simmons-Mackie & Damico, 2010, p. 52).
Talking about one’s own speech and language is a notion related to the healing power of personal narrative (Hinckley, 2006; Shadden & Hagstrom, 2007). Reporting on scripts developed by aphasic speakers or used in script training (Cherney, Halper, Holland, & Cole, 2008; Youmans, Holland, Munoz, & Bourgeois, 2005; Youmans, Youmans, & Hancock, 2010), Holland, Halper, and Cherney (2010) described the content of 28 self-determined monologues written and subsequently learned by persons with chronic aphasia. Nineteen (68%) of these monologues were stories about some aspect of the speaker’s life and 12 (43%) were specifically about their strokes. These scripts were affirmative and optimistic, supporting the notion that, despite aphasia, many persons with chronic aphasia have NOT lost (or perhaps have reestablished) their sense of identity over time.
This issue, in turn, relates to the importance of helping an aphasic individual either to capitalize on or to develop some resilience, defined here simply asthe ability to bounce back from aphasia. Evidence from aphasic narratives (Hinckley, 2006) and from clinical encounters (Holland, 2010) indicates that resilience matters. This should not be surprising when one considers the rich literature relating to the palliative, if not curative effects ofresilience, optimism, and positive affect in other illnesses (Edward & Warelow, 2005; Pressman & Cohen, 2005; Rasmussen, Scheier, & Greenhouse, 2009). It is likely that resilience, optimism, and identity issues change over time for PWAs, altering their attitudes toward a variety of activities and opportunities, including aphasia treatment. Although neither Holland (2010) nor Hinckley (2006) specifically analyzed the effects of aphasia severity or type, Hinckley did emphasize that readjustment after aphasia takes many years.
Code and Hermann (2003) reviewed a number of factors in aphasia as they relate to emotional and psychosocial status and made a strong case for better therapeutic outcomes in people with positive mood states. Regarding time post-onset, they explained that depression is not uncommon in PWAs, citing statistics of 16% at 12 months and 29% at two to three years following stroke. Additionally, they described how site of lesion, specifically left hemisphere frontal damage, is associated with higher frequency and severity of depression in the acute period, but cognitive and physical impairment becomes almost as important as time post-onset increases. A recent study by Hilari et al. (2010) further explored the relationship of different variables to psychological distress in the first six months after stroke. At three months post-onset, aphasia was significantly associated with psychological distress, but aphasia was not a predictor of distress at any time. They reported a complex interaction between physical, linguistic, and social variables over time.
The correspondence between site of lesion and type of aphasia would suggest the likelihood of a relationship between type of aphasia and emotional status as well. It is also intuitive to expect that participants who have marked production difficulties along with acute awareness of their deficits because of relatively good comprehension and monitoring (e.g., Broca and Conduction) would experience ongoing frustration that would produce negative affect. In fact, Robinson and Benson (1981) found depression to be common (almost 50%) in a group of inpatients with chronic aphasia, and reported greater frequency and severity in patients with nonfluent aphasias compared to those with fluent or global aphasias. They used two self-rating scales and two rating scales completed by professionals. Fromm, Holland, and Swindell (1984) found depression in almost half (48%) of a group of left hemisphere stroke patients with aphasia during the first year post-onset using a self-report inventory administered by examiners. A significant correlation was found between severity of aphasia and depression; type of aphasia revealed no significant correlation. Several studies have shown that aphasia severity also has an effect on Quality of Life or QOL (Bose, McHugh, Schollenberger, & Buchanan, 2009; Cruice, Worrall, Hickson, & Murison, 2003; Hilari, Wiggins, Roy, Byng, & Smith, 2003; Hilari & Byng, 2009). Though the current study is more narrowly focused on direct communication to elicit personal evaluations about speech in a group of non-hospitalized people with chronic aphasia, these findings on depression and QOL suggest that time post-onset, severity, and aphasia type may play important roles in emotional valence.
Recent work exploring the language of attitudes, feelings, and opinions suggests that evaluative language, a crucial part of expression of identity, may be relatively well retained in aphasia (Armstrong, 2001; Armstrong & Ulatowska, 2007; Ferguson, Worrall, Davidson, Hersh, & Sherratt, 2010; Olness, Matteson, & Stewart, 2010; Ulatowska, Olness, Keebler, & Tillery, 2006). Evaluations occur on a continuum of valence from negative to positive, and can involve different types of meanings including personal affect (e.g., I hated my time in the hospital, I loved seeing my family), judgment (e.g., my speech was bad, it’s now excellent), and appreciation (e.g., the bed was uncomfortable, the stay was too long) (for full overview, see Martin & White, 2005). Armstrong and Ulatowska (2007) analyzed stroke stories produced by participants with mild to moderately severe aphasia and examined a number of evaluative devices (the use of repetition for emphasis, direct speech, metaphoric language, and the use of emotive words and phrases). Results showed that participants were able to use evaluative language to express their attitudes and feelings in spite of their incomplete utterances and impaired syntax and semantics. Additionally, studies focusing specifically on verbal pragmatics, for example, have found that speakers with left hemisphere damage and aphasia varying both in type (nonfluent, fluent, mixed) and severity (mild, mild-moderate, moderate, moderate-severe) produce more elaborate discourse when discussing emotional vs. non-emotional topics (Bloom, Borod, Obler, & Koff, 1990; Bloom, Borod, Obler, & Gerstman, 1993; Borod et al., 2000). Hence, from both identity and language performance perspectives, it may in fact be therapeutic to include personal and evaluative topics and tasks in assessment and treatment contexts.
Few studies have explored personal and evaluative discourse in large groups of PWAs and systematically evaluated the effects of time post-onset, aphasia severity, or aphasia type. As part of AphasiaBank, a project designed to create a shared database of multi-media interactions for the study of communication in aphasia, a protocol was developed to elicit various types of discourse, some of which is essentially evaluative in nature.1 The first free speech probe in the protocol is, “How do you think your speech is these days?” Based on its open-ended nature, this opening question achieved several goals. First, it starts off the interaction by valuing the participant’s opinion on this meaningful and relevant topic. Second, it allows PWAs the opportunity to give their own assessment of their communication skills in any way they can. Third, it creates a shared perspective for the investigator and the participant as they move through the rest of the tasks. Analysis of data from this interaction can provide some indication of PWA’s ability to use evaluative language to express opinions and attitudes; it can allow us to judge the positive/negative nature or ‘valence’ of their feelings about their speech at a particular time post-onset. In addition, by looking at the further elaborations that PWAs provide, we can derive further detail regarding their approaches and attitudes toward recovery from and adaptation to aphasia.
In describing ways for physicians to solicit patients’ concerns, Robinson (2006) explains that, “in mundane conversation, as well as in physician-patient visits, the question How are you feeling? “performs the action of soliciting an evaluation of a particular, recipient-owned, currently experienced condition that is known about by the speaker and typically related to physical health” (p. 33). Hence, the similar elicitation technique used in AphasiaBank resonates with everyday clinical practice and provides a question aimed at eliciting evaluative discourse.
Emotions and attitudes are conveyed in numerous non-verbal and paralinguistic ways, as well as through direct linguistic output (Camras, Holland, & Patterson, 1993; Pittam & Scherer, 1993). Facial expression, body language, gestures, stress patterns and intonation, loudness, speech rate, sighs, and laughs all convey important meanings. The multi-media aspect of the AphasiaBank project allows for analysis of verbal and nonverbal aspects of participants’ responses. However, while the nonverbal and paralinguistic aspects of the interactions elicited in this study were examined in terms of the way they supported the verbal expression of participants, this initial study focuses primarily on the verbal meanings conveyed, leaving the more detail analysis of these other aspects to future studies. The complexity of the verbal aspects alone involved in evaluative meanings has been acknowledged (Hunston & Thompson, 2003; Martin & White, 2005). Thus, the goal was to conduct a preliminary study with data from a large number and wide range of participants to explore the effects of clinical variables on emotional expression. Specifically, the following questions will be addressed:
What is the valence (positive, negative, neutral/mixed) of the participants’ evaluative responses as expressed primarily through their verbal behaviors?
Is the valence of their evaluative responses associated with time post-onset, severity of aphasia, or type of aphasia?
What additional elaborations do participants include when answering this simple question?
Method
This descriptive study was conducted on one segment of a larger dataset from the AphasiaBank project. Participants, materials, and procedures from the larger project are presented and followed by an explanation of the coding and statistical analyses specific to this investigation.
AphasiaBank: Participants
The data presented here comprise the responses made by the first 71 PWAs entered into the AphasiaBank database who met the following selection criteria: 1) aphasia resulting from stroke, verified through neuroimaging and/or a clear medical diagnosis; 2) auditory and visual abilities adequate for testing; and 3) English spoken as the primary language. Co-existing apraxia and dysarthria werenot exclusionary criteria, but participants with dementia or with comorbidities associated with serious cognitive consequences were excluded. The AphasiaBank project received the required IRB approval. All participants (and/or their representatives) signed consent forms for the testing and data collection and gave approval for the data to be available for research and teaching purposes. Participants ranged in age from 35.9–90.7 years (mean = 64.5) and came from eight different test sites in the United States. The sample included 27 females and 44 males. Fifty-eight were right handed; six were left-handed; two were ambidextrous; and the handedness of the other five was unavailable. Education ranged from 12–25 years (mean = 15.9) and time post onset ranged from 0.5–39.2 years (mean = 7.4). Side of lesion was left hemisphere in 58 cases, right hemisphere in 3 cases, and unavailable in 10 cases. WAB Aphasia Quotients (AQs) ranged from 20.3–97.6 points (mean = 68.7). Table 1 provides a list of aphasia types based on WAB AQ subtest scores.
Table 1.
WAB Data
| Aphasia Types | Frequency |
|---|---|
| Anomic | 21 |
| Broca | 16 |
| Conduction | 13 |
| Global | 2 |
| Transcortical Motor | 5 |
| Transcortical Sensory | 1 |
| Wernicke | 7 |
| not aphasic (scored above cutoff) | 5 |
| unavailable | 1 |
AphasiaBank: Materials and Procedures
All AphasiaBank testing sessions were conducted by a licensed speech-language pathologist (SLP) or by an SLP graduate student. In most cases, the investigator did not know the participant prior to the session. Testing typically took place in a room at a clinic or an aphasia center, with the investigator and the participant seated together at a table. Often a third person was in the room to monitor the video recording. In two cases, testing took place in the participant’s home.
The AphasiaBank research protocol begins with the investigator saying, “I am going to be asking you to do some talking.” This comment is immediately followed by the first prompt, “How do you think your speech is these days?” The prompt is delivered in a natural, conversational manner. The investigator does minimal verbal prompting, but is an attentive, active listener, providing extensive nonverbal encouragers as well as plenty of time for the participant to give as complete a response as he/she desires. This approach allows the PWA to respond in a spontaneous, open-ended fashion and to determine what constitutes an adequate answer to the question. The goal of the investigator is to create an atmosphere that encourages the participant to provide complete responses, rather than short, interrogation-style answers. Using this simple, but uniform, technique allowed for the collection of a large number of comparable samples from different sites, by different investigators, and with different participants.
The opening prompt is followed by prompts for personal narratives, picture descriptions, story telling, and procedural discourse. Finally, a few short formal assessments of naming and repetition are completed. Aphasia Quotients from the Western Aphasia Battery Revised (WAB) (Kertesz, 2007) are available for all participants.
All AphasiaBank test sessions are videotaped. Trained research assistants transcribe the discourse sections using the CHAT transcription format of the CLAN program (MacWhinney, 2000). 2 Following the guidelines set by Berndt, Wayland, Rochon, Saffran, & Schwartz, (2000), utterances are segmented based on the following hierarchy of indices: syntax, intonation, pause, semantics. Two SLPs, with aphasia experience and transcription training, checked the accuracy of each transcription and the two reached forced choice agreement on all features of the transcription.
Evaluative Response Coding
For this study, responses to the first free speech question (How do you think your speech is these days?) were extracted from each transcript. CHAT transcripts include all spoken output as well as gesture coding (e.g., thumbs up, head shake) and paralinguistic events (e.g., sighs, laughs). These responses were reviewed to determine the overall evaluative response by assigning each to one of these three categories: positive, negative, or neutral/mixed. In cases where the words did not indicate a clearly positive (e.g., great), negative (e.g., terrible), or neutral/mixed (e.g., fair, good and bad) response, the investigators played the videos to listen to the intonation and see the nonverbal cues (e.g., facial expressions, hand gestures, body language). For example, if a participant said that his speech is “seventy percent”, it would be difficult to code that response as positive or negative from the words alone. If he said it with a smile, a thumbs-up sign, and/or a sense of pride and satisfaction, it was coded as a positive assessment. If he said it with a headshake, a thumb down sign, a discouraging tone of voice, and/or a frown, it was tallied as negative. If he said it with a shrug and flat intonation, it was coded neutral. Two of the authors, both native speakers of English, used these guidelines and native speaker intuition to independently code the evaluative response. Inter-rater coding agreement was 97%.
Responses were also examined for further elaborative content. One member of the research team identified three themes frequently included by respondents, and a second researcher independently corroborated those findings. Then two other members of the research team independently categorized these responses into one of the three response types. Inter-rater agreement was 99% for this categorization of the elaborative comments.
Statistical Analysis
Descriptive statistics (measures of central tendency and measurement variability for interval data; tallies of frequency of occurrence for categorical data) were used in conjunction with planned inferential statistics. In particular, a two-tailed Welch’s t-test (no assumption of equal population variances) was used to analyze differences between the positive and negative response groups in time post-onset and aphasia severity. Pearson’s Chi-square test, the standard analysis for categorical data, was used to analyze the association between aphasia type (as categorized by WAB) and evaluative response category (positive, negative, or neutral/mixed).
Results
In response to the prompt, the average number of utterances, including incomplete ones, was 4.63 (range = 1–26, SD = 4.28). The average number of words used in the responses (excluding word repetitions, fillers, and revisions) was 23.23 (range = 1–162, SD = 27.17).
Evaluative response
Responses were grouped into three categories, which accounted for 94% of all responses. The remaining 6% were removed from the main categorical analysis because they were uninterpretable, incoherent utterances often with neologisms and paraphasias (e.g., “It, it usually depends upon how long I, how long I get, I get grags. I get, I get, I just have to make my one tek in the teks. One, one a teks. But that, that, that’s about it.”) The three main categories as well as their corresponding percentages, definitions, and examples are given below.
Positive responses (59%) were those in which the verbal and nonverbal communication indicated a favorable assessment.
Negative responses (17%) were those in which the verbal and nonverbal communication reflected an unfavorable assessment.
Neutral/mixed responses (18%) indicated a noncommittal, average, or mixed assessment.
Positive responses mentioned improvement, getting better, and words like fine, good, pretty good, really good, great, normal, and excellent. Negative responses described not being able to talk and having trouble. They included words like awful, terrible, not good, not well, and none. Neutral/mixed responses were characterized by words such as average and fair. This category also had elements of mixed positive and negative assessments, indicating that sometimes speech is good but sometimes it is not.
Table 2 includes examples of responses from each of these categories. Paraphasias and neologisms appear in italics. Although gestures and paralinguistic behaviors are indicated in these transcription excerpts, a cautionary note is offered for reading the response examples without the benefit of actually seeing and hearing the facial expressions, gestures, body language, and vocal intonation that characterized the responses. All extra-linguistic phenomena were taken into consideration by the coders at the time of coding (native English speakers using native speaker intuition), even though these phenomena are not fully represented in the transcripts.
Table 2.
Examples of Responses from Participants by Valence Rating
| Rating | Participant response |
|---|---|
| Positive | Really good from the uh oh stroke. |
| Talking better now. | |
| Well it’s better than it used to bid. | |
| It’s little bit begger. | |
| Improving, improving. I uh cofidlitly improving a lot better. | |
| Well excellent because I have had aphasia. | |
| Seventy, eighty percent. | |
| Now pretty darn good. | |
| Good. I’m great (gestures: thumbs up). | |
| I think it’s normal. | |
| (gestures: counts) one, two, three, four, five, six, seven, eight, nine, ninety percent. | |
| Well, better but no cigar. | |
| Fine. | |
| Uh, uh, uh, well, uh, uh, uh, uh, uh, uh, uh, uh, uh, uh I could &uh I could talk, you know. | |
| Negative | Not good. I’m not good at this. |
| I can’t talk. | |
| Not so well. | |
| No. | |
| Oh it’s awful. | |
| It is terrible. It’s just terrible. It was, because I can’t, uh it was, I was, I … Oh Jesus. I, I’m so dadut and then boom. Buh, buh, buh, buh, buh, buh. None, none, none, none, none. | |
| I think it’s pretty awful then. I mean it used to be pretty good but now I have trouble doing some of this. | |
| Neutral/Mixed | Uh, fair. |
| Sometime words yes, no (gestures: fair). | |
| Not bad. I don’t know how good it is but it’s not bad. | |
| Just not too good but improving. | |
| Uh well I would say is below average. In fact sub sub below average (laughs). But when you, you uh uh if you compare my speech versus another, another patient, is on par. | |
| Average. You know, I get most of it but I have a, I, most of it’s all pretty well tire also. | |
| It varies. Um I’m usually good in the morning and in the afternoon. By that time I get um not uh sloppy. Not sloppy but I’m tired. And that determines how I do. |
Associations Among Variables
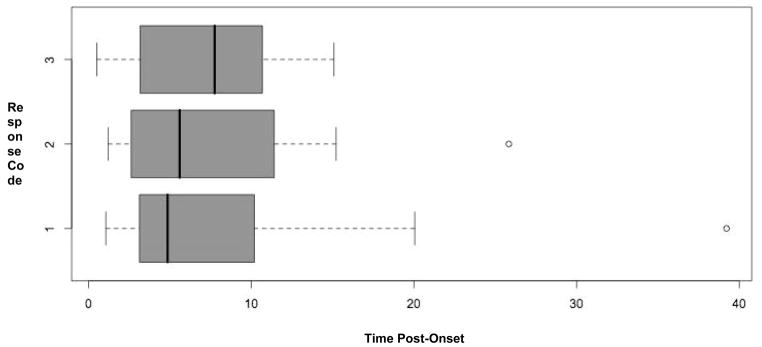
Box plots (Tukey, 1977), shown in Figure 1, were constructed to examine the relationship between time post-onset and category of evaluative response: positive (1) versus negative (2) versus neutral/mixed (3). The dark black vertical lines inside the boxes indicate the median time post-onset for each of the response categories, the outside edges of the boxes indicate the first and third quartiles, and the vertical lines on either end of the dashed lines indicate the lower and upper extreme non-outlier values of time post-onset. The open circles indicate outlier values because they are more than 1.5 times the inter-quartile range (difference between the first and third quartiles). The positive (1), negative (2), and neutral/mixed (3) response distributions can clearly be seen as overlapping, so no further statistical analyses were conducted on the time post-onset variable.
Figure 1.
Boxplots of time post-onset (in years) for positive (code 1, n=42) vs. negative (code 2, n=12) vs. neutral/mixed (code 3, n=13) response valence.
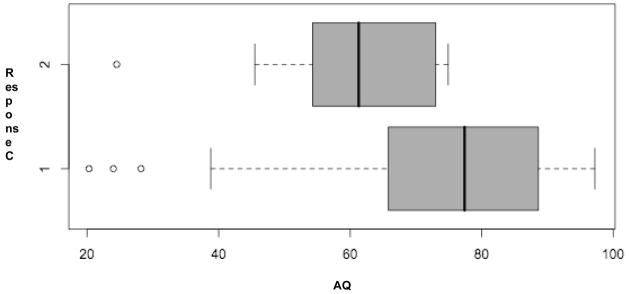
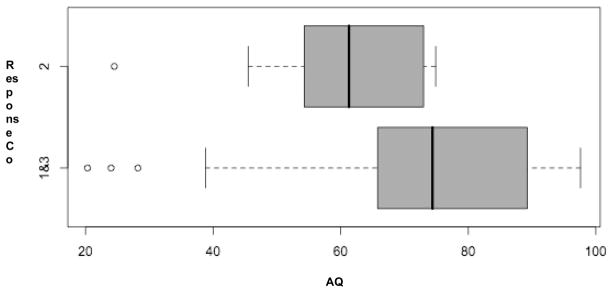
Box plots were also constructed to examine the relationship between the WAB Aphasia Quotient (AQ), as a measure of aphasia severity, and positive (1) versus negative (2) responses. Figure 2 shows the box plots, which suggest a difference in category of evaluative response as a function of severity. The positive response group is shifted higher on the x-axis, indicating higher AQ scores (lower aphasia severity). As the figure shows, the median score for the positive response group is higher on the AQ scale than the upper extreme value for the negative response group. It is also apparent that the distribution for the positive response group is negatively skewed, indicating more positive responses in the higher AQ range. In contrast, the negative response distribution is positively skewed, indicating more negative responses in the lower AQ range. A Welch Two Sample two-tailed t-test showed that the difference between these two distributions was significant, t(24.83) = 2.55, p = .017. This significant difference was maintained when neutral/mixed responses were added to the positive group, thereby creating a “not negative” response group to compare with the negative response group, t(20.79) = 2.84, p = .010. Figure 3 shows the box plots for this comparison, which is similar to the previous one.
Figure 2.
Boxplots of WAB AQ for positive (code 1, n=42) vs. negative (code 2, n=12) response valence.
Figure 3.
Boxplot of WAB AQ for positive and neutral/mixed (codes 1&3, n=55) vs. negative (code 2, n=12) response valence.
To examine the relationship between evaluative response category (positive, negative, neutral/mixed) and type of aphasia, Pearson’s Chi-square test was used. For type of aphasia, the groups were Anomic, Broca, Conduction, and Wernicke. The sample sizes for other types of aphasia were too small (5 or less) to permit their inclusion in the chi-square analysis. Results showed no significant relationship, Χ2(6) = 9.68, p = .138, between response content and aphasia type.
Specific Content
In addition to giving general qualitative assessments (e.g., good, bad, fair), many participants spontaneously elaborated about their speech with content that could be classified into these three topic areas: specific speech problems (n=25), improvement (n=22), and therapy (n=6).
Specific problems included any mention of examples of their speech problems, such as getting stuck and having words spinning around in the head, speaking slowly, not rushing, not being able to talk at all, and needing to work on reading.
Improvement included any mention of positive change over time. For instance, participants mentioned getting better, improving, and being clearer.
Therapy included any mention of any kind of treatment or outside help. These utterances included speech therapy, group therapy, acupuncture treatment, and the internet.
Examples of responses from each of these categories appear in Table 3.
Table 3.
Examples of Specific Elaborated Content by Content Category
| Category | Participant response |
|---|---|
| Specific speech problems | If I don’t rush what I’m trying to say I could get my words across pretty well. |
| It’s, it’s good but it’s very slow. It’s (gestures: no) not, not, not when I talk fast but when I talk slow I understand better. | |
| Sometimes I do get like stuck when I’m like trying to say something and it doesn’t come out. Like I have words that are (gestures: spin) spinning around in my head. And I’m (gestures: pick) like trying to pick out which one I should say first. | |
| But I can’t (points: mouth), it, I, you know takes me quite a long time with aphasia. | |
| I got a long ways to go for reading. But that’s one of the most important thing for me is, is to read. | |
| I remember I couldn’t talk at all. Thirty one days of saying _____, my name. And now talk too too much. | |
| Improvement | My speech is fine. Um slowly it’s improving. |
| Not bad. Much better than a year ago. | |
| Better and better and better and better. | |
| Getting better. Getting better. | |
| Much better. During the stroke, well after the stroke, I couldn’t talk at all. So, it’s much better. Much better. | |
| A little bit clearer in the words. | |
| Better. Little bit better. | |
| Compared to what? I’ll compare it to a year ago. I think it’s a little bit better. Compared to when I first had my stroke it’s A- number-one (laughs). Because when I first had my stroke I couldn’t speak. | |
| Therapy | I go to school for speech (gestures: four) two, three, four years. |
| And I got into a group of people from, uh people who were helling me with um uh speaking. | |
| Uh, entapucture. Saturday, each Saturday. Uh needles, needles. | |
| The (points: here) I like. One, two (gestures: two) days is (points: here). And the internet (points: computer). I one (points: self). One two (points: up). I one uh a big one (gestures: big). |
Discussion
When asked about their speech, 59% of the PWAs gave distinctly positive answers. Another 18% of the answers were categorized as neutral/mixed. Only 17% of the participants gave negative responses to the question. The favorable spin may seem surprising in light of the chronic language impairments that most of these individuals experience. It does, however, correspond to the affirmative and optimistic descriptions of aphasic narratives and monologic scripts (Cherney, Halper, Holland, &Cole, 2008; Hinckley, 2006). While the reasons for the optimism can be explored further, the simple fact of its existence is noteworthy as well as potentially beneficial for the participants and useful for clinicians.
Time post-onset and type of aphasia were not significantly related to positive versus negative responses. However, aphasia severity (as measured by WAB AQ) was significantly related, with higher AQ scores in the positive response group and lower AQ scores in the group with negative responses. Even when the neutral/mixed responses were combined with the positive response group to create a “not negative” response group to compare with the negative response group, the difference was still significant.
These results suggest that these PWAs are responding in what appears to be a realistic way to their situations. Those whose language is more impaired are, in fact, saying more negative things about their speech, and vice versa. In a review of positive affect and health, Pressman and Cohen (2005) described this type of relationship, namely that positive affect declines with increases in disease severity. The fact that type of aphasia was equally distributed across the positive and negative response groups suggests that the specific pattern of impairment and corresponding brain lesions had no effect on the individual’s expressed opinion of his/her speech. That being said, not all types of aphasia were included in this analysis as the sample sizes were too small for Transcortical Sensory, Transcortical Motor, Global aphasia, and not-aphasic-by-WAB (scored above the AQ cutoff but considered themselves aphasic). Results on the time post-onset variable may have been different if the study had been done using a longitudinal design or if participants had incurred their strokes more recently or were less well served professionally. The average time post-onset in this study was over seven years, so this was predominantly a group of people who had been living with aphasia for a while, having been involved in speech-language therapy and stroke groups to varying extents.
The large percentage of positive responses may be due to a number of factors. One possible explanation is that, in general, people are naturally inclined toward optimism rather than pessimism. Similarly, it could be that PWAs who participate in research projects are a self-selected group with a more positive attitude. (To the authors’ knowledge this factor has not been well studied in the research literature.) Not only did individuals in this study agree to participate in a study that involved sharing their language problems with researchers and students in a very direct (though identity-protected) way, the majority of them (73%) participate in aphasia centers and programs designed to implement Life Participation Approaches to living with chronic aphasia (Chapey et al., 2000). The predominant attitudes expressed in this investigation reflect those that such centers and programs foster and support.
One might imagine that these positive responses may simply be a case of phatic communication, much like when people say good or fine in response to standard how are you queries. However, the responses we obtained to this probe typically involved multiple utterances that went beyond the requirements of a minimal phatic response. Of course, even these extended responses to this question could be viewed as constrained by further discourse expectations. For example, Button and Casey (1985) characterized the responses to How are you questions as “itemized news inquiries”. Such responses may minimize negative evaluations. More generally, there is a preference (Pomerantz, 1984) for positive responses to questions over negative responses. It is possible that this preference is further amplified within the context of institutional discourse. However, the analyses of doctor-patient communication presented by Heritage and Clayman (2010) suggest that these communications are typically fairly frank and direct, because it is not in the patient’s interest to misrepresent his medical and emotional status.
The actual shape of the probe we used was designed to minimize superficial or phatic responses to the question. In this regard, Robinson (2006) contrasts the How are you? question with the How are you feeling? question and explains that the former asks for a person’s current and general state of being, whereas the latter requests an evaluation of the “state of a particular and ongoing health condition” (p.39). The former question is more likely to produce a response like “Okay”. In the current study, the prompt of How do you think your speech is these days? led a majority of the subjects to elaborate upon their responses, however briefly. Also, it is worth emphasizing that this question was not posed casually. The investigator poses it in a serious, deliberate manner to initiate the AphasiaBank protocol. This can be verified directly by playing back interactions directly over the web using the interactive browser facility at http://talkbank.org.
Finally, the possibility exists that there is good cause for optimism, given the fact that, in most cases, participants have improved since they first had their strokes. Improvement was specifically mentioned in many of the positive responses. Along these same lines, Riis et al. (2005) found that healthy people tend to underestimate the self-reported well-being of people with chronic disabilities. In studying patients with chronic kidney disease on hemodialysis, the authors found that patients adapt to their conditions and report positive average moods that do not differ significantly from those of healthy controls. The authors conclude that, in coping with hardship, patients may focus more on positive experience as an important part of their adaptation process. Similarly, Cruice, Worrall, Hickson, and Murison (2009) compared quality of life assessments from 30 people with aphasia to the assessments provided by their spouses and children, concluding that significant others rated their partners’ global and health-related quality of life much lower than their aphasic partners rated themselves. While the current study does not purport to be a measure of quality of life, the positive responses by people with aphasia to a question about their speech status fit with the generally more positive ratings given by aphasic participants in these quality of life studies.
Cranfill and Wright (2010) examined quality of life measures with the goal of determining which domains are important to persons with aphasia. The authors found that severity of physical functioning was rated as more important to the persons with aphasia than was communication functioning. Furthermore, the ratings from significant others and SLPs were significantly correlated with each other but not with those of the PWAs. The message continues to be that proxies and PWAs do not necessarily agree on the importance of health-related quality of life domains, thereby emphasizing the importance of initiating and continuing these topics of communication with PWAs themselves.
The comments from PWAs in the current study indicate substantial self-awareness about their speech. Just over a third mentioned some specific attributes that characterize their speech production and just under a third mentioned improvement over time. These comments about the need to speak more slowly or speech being better earlier in the day, for example, suggest self-awareness and self-regulation, curiosity about their own symptoms, and creativity, also thought to be positive strengths that affect well-being. A smaller number of participants mentioned specific techniques being employed for therapeutic purposes. Taken together, these themes bear striking similarity to metaphors used to described aphasia rehabilitation in a recent study by Ferguson et al. (2010). PWAs used the metaphoric concepts of product, body, journey, and battle most frequently; family members and SLPs used journey most frequently. The changes over time were a common theme for all parties involved in the experience of aphasia. The authors encourage the consideration of metaphor to compare and contrast perspectives between PWAs, their family members, and SLPs for purposes of treatment and counseling.
The fact that participants in this study responded positively concerning their speech would seem to bode well for the participants. For example, Seligman and Peterson (2003) note that, “Psychologists have discovered that there are human strengths that act as buffers against mental illness: courage, future-mindedness, optimism, the capacity for flow, and insight to name several” (p. 314). There is reason to believe that these same strengths play a role in recovery from a number of diseases and disorders as well (Fitzgerald, Tennen, Affleck, & Pransky, 1993; Pressman & Cohen, 2005), and stroke and aphasia should be no exception. Using meta-analytic techniques, Rasmussen et al. (2009) demonstrated that optimism is a significant predictor of physical health and that subjective measures, including self-reports, produced significantly higher effect sizes than did objective measures. Also interesting and relevant was the fact that the effect sizes were not significantly different for patient populations versus healthy populations, though they were larger in the studies using patient populations.
In a short report on coping in psychiatric-mental health illness, Edward and Warelow (2005) explain that both genetic factors and learned protective behaviors can contribute to a person’s resilience when facing adversity. They stress that knowing about resilient behaviors may improve clinical practice and affect outcomes. Therapy that includes support and education, and specifically a focus on resilient behaviors can especially help in aphasia where communication skills are involved. Clinicians are being urged to help patients renegotiate their identities (Shadden, 2005). Allowing for identification and recognition of other factors of resilience such as humor, flexibility, intellectual competence, self-reliance, persistence, and hopefulness may help aphasic individuals strengthen their sense of self in the altered context of their post-stroke lives.
This study does not claim to provide in-depth analysis of the acknowledged deep-seated identity and adjustment issues facing people with aphasia, nor a detailed linguistic examination of evaluative language. However, it presents an interesting new approach to this issue, because the raw data from this study are now openly available over the web to the research community. To facilitate direct examinations, we have inserted our coding for each response into each transcript on the @G: Speech line where the prompt was given. Using this transparent and open data window, we can join with other researchers in conducting further analyses of the detailed gestural and into national features accompanying these verbal descriptions. Moreover, as we can add further data to this openly available source from a wider array of participants and use additional prompts, that could elicit more information about the details of physical and social adaptation to aphasia. It may also be possible eventually to include data collected from non-institutional contexts.
Although data collected in this interview format remain bound to the institutional context, it is important to remember that this is the context in which PWAs encounter therapy and treatment. To the degree that these attitudes can shape treatment outcomes, it is important to better understand how PWAs evaluate their own therapy and recovery. By making these data directly available through AphasiaBank, we can add further reliability and replicability to the investigation of these relations.
Acknowledgments
This project is funded by NIH_NIDCD grant R01-DC008524 (2007–2012).
A visiting Fellowship provided by Edith Cowan University, Western Australia, to Audrey Holland resulted in Beth Armstrong’s collaboration in this work.
Footnotes
Another article in this special issue by MacWhinney, Fromm, Forbes, and Holland, discusses the entire AphasiaBank protocol in more detail and explains how to use computerized transcription and language analysis programs to study phonological, lexical, morphosyntactic, and gestural aspects of the database.
The movies, transcripts, and protocols are available to AphasiaBank members on the AphasiaBank website at http://talkbank.org/AphasiaBank. To apply for membership in AphasiaBank, please consult the instructions on that page.
Contributor Information
Davida Fromm, Carnegie Mellon University, Pittsburgh, PA, USA.
Audrey Holland, University of Arizona, Tucson, AZ, USA.
Elizabeth Armstrong, Edith Cowan University, Joondalup, Western Australia.
Margaret Forbes, Carnegie Mellon University, Pittsburgh, PA, USA.
Brian MacWhinney, Carnegie Mellon University, Pittsburgh, PA, USA.
Amy Risko, Carnegie Mellon University, Pittsburgh, PA, USA.
Nicole Mattison, Carnegie Mellon University, Pittsburgh, PA, USA.
References
- Armstrong E. Connecting lexical patterns of verb usage with discourse meanings in aphasia. Aphasiology. 2001;15:1029–1046. [Google Scholar]
- Armstrong E, Ulatowska HK. Making stories: Evaluative language and the aphasia experience. Aphasiology. 2007;21(6):763–774. [Google Scholar]
- Beeke S, Wilkinson R, Maxim J. Prosody as a compensatory strategy in the conversations of people with agrammatism. Clinical Linguistics & Phonetics. 2009;23(2):133–155. doi: 10.1080/02699200802602985. [DOI] [PubMed] [Google Scholar]
- Behrns I, Wengelin A, Broberg M, Hartelius L. A comparison between written and spoken narratives in aphasia. Clinical Linguistics & Phonetics. 2009;23(7):507–528. doi: 10.1080/02699200902916129. [DOI] [PubMed] [Google Scholar]
- Berndt R, Wayland S, Rochon E, Saffran E, Schwartz M. Quantitative production analysis: A training manual for the analysis of aphasic sentence production. Hove, UK: Psychology Press; 2000. [Google Scholar]
- Bloom R, Borod J, Obler L, Gerstman L. Suppression and facilitation of pragmatic performance: Effects of emotional content on discourse following right and left brain damage. Journal of speech and Hearing Research. 1993;36:1227–1235. [PubMed] [Google Scholar]
- Bloom R, Borod J, Obler L, Koff E. A preliminary characterization of lexical emotional expression in right and left brain-damaged patients. International Journal of Neuroscience. 1990;55:71–80. doi: 10.3109/00207459008985952. [DOI] [PubMed] [Google Scholar]
- Borod J, Pick L, Andelman F, Obler L, Welkowitz J, Rorie K, Bloom R, Campbell AL, Tweedy J, Sliwinski M. Verbal pragmatics following unilateral stroke: Emotional content and valence. Neuropsychology. 2000;14(1):112–124. doi: 10.1037//0894-4105.14.1.112. [DOI] [PubMed] [Google Scholar]
- Bose A, McHugh T, Schollenberger H, Buchanan L. Measuring quality of life in aphasia: Results from two scales. Aphasiology. 2009;23(7–8):797–808. [Google Scholar]
- Button G, Casey N. Topic nomination and topic pursuit. Human Studies. 1985;8:3–55. [Google Scholar]
- Byng S, Duchan J. Social model philosophies and principles: Their applications to therapies for aphasia. Aphasiology. 2005;19:906–922. [Google Scholar]
- Camras LA, Holland EA, Patterson MJ. Facial expression. In: Lewis M, Haviland JM, editors. Handbook of emotions. New York: The Guilford Press; 1993. pp. 199–208. [Google Scholar]
- Chapey R, Duchan J, Elman R, Garcia L, Kagan A, Lyon J, Simmons-Mackie N. Life participation approach to aphasia. In: Chapey R, editor. Language intervention strategies in aphasia and related neurogenic communication disorders. 4. Baltimore: Lippincott, Williams & Wilkins; 2000. pp. 235–245. [Google Scholar]
- Cherney LR, Halper AS, Holland AL, Cole R. Computerized script training for aphasia: Preliminary results. American Journal of Speech-Language Pathology. 2008;17:19–34. doi: 10.1044/1058-0360(2008/003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Code C, Hermann M. The relevance of emotional and psychosocial factors in aphasia to rehabilitation. Neuropscyhological Rehabilitation: An International Journal. 2003;13:109–132. doi: 10.1080/09602010244000291. [DOI] [PubMed] [Google Scholar]
- Cranfill TB, Wright HH. Importance of health-related quality of life for persons with aphasia, their significant others, and SLPs: Who do we ask? Aphasiology. 2010;24:957–968. [Google Scholar]
- Cruice M, Worrall L, Hickson L, Murison R. Finding a focus for quality of life with aphasia. Social and emotional health, and psychological well-being. Aphasiology. 2003;17(4):333–353. [Google Scholar]
- Cruice M, Worrall L, Hickson L, Murison R. Measuring quality of life: Comparing family members’ and friends’ ratings with those of their aphasic partners. Aphasiology. 2009;19:111–129. [Google Scholar]
- Edward K, Warelow P. Resilience: When coping is emotionally intelligent. Journal of the American Psychiatric Nurses Association. 2005;11:101–102. [Google Scholar]
- Elman R. Social and life participation approaches to aphasia intervention. In: LaPointe L, editor. Aphasia and related neurogenic language disorders. 3. New York: Thieme Medical Publishers; 2005. pp. 39–50. [Google Scholar]
- Ferguson A, Worrall L, Davidson B, Hersh D, Sherratt S. Describing the experience of aphasia rehabilitation through metaphor. Aphasiology. 2010;24(6–8):685–696. [Google Scholar]
- Fitzgerald T, Tennen H, Affleck G, Pransky G. The relative importance of dispositional optimism and control appraisals in quality of life after coronary bypass surgery. Journal of Behavioral Medicine. 1993;16:25–43. doi: 10.1007/BF00844753. [DOI] [PubMed] [Google Scholar]
- Fromm D, Holland AL, Swindell CS. Clinical Aphasiology Conference Proceedings. Minneapolis: BRK Publishers; 1984. Depression following left hemisphere stroke [Abstract] [Google Scholar]
- Hagstrom F. Including identity in clinical practices. Topics in Language Disorders. 2004;24(3):225–238. [Google Scholar]
- Heritage J, Clayman S. Talk in action: Interactions, identities, and institutions. New York: Wiley; 2010. [Google Scholar]
- Hilari K, Byng S. Health-related quality of life in people with severe aphasia. International Journal of Language and Communication Disorders. 2009;44(2):193–205. doi: 10.1080/13682820802008820. [DOI] [PubMed] [Google Scholar]
- Hilari K, Wiggins RD, Roy P, Byng S, Smith SC. Predictors of health-related quality of life (HRQL) in people with chronic aphasia. Aphasiology. 2003;(17):365–381. [Google Scholar]
- Hilari K, Northcott S, Roy P, Marshall J, Wiggins R, Chataway J. Psychological distress after stroke and aphasia: The first six months. Clinical Rehabilitation. 2010;24:181–190. doi: 10.1177/0269215509346090. [DOI] [PubMed] [Google Scholar]
- Hinckley J. Finding messages in bottles: Successful living with aphasia as revealed by personal narrative. Topics in Stroke Rehabilitation. 2006;13:63–67. doi: 10.1310/FLJ3-04DQ-MG8W-89EU. [DOI] [PubMed] [Google Scholar]
- Holland A. Counseling in communication disorders: A wellness perspective. San Diego, CA: Plural Publishing; 2007. [Google Scholar]
- Holland A. Lessons from a Clinical Life. Topics in Stroke Rehabilitation. 2010;17:13–19. doi: 10.1310/tsr1701-13. [DOI] [PubMed] [Google Scholar]
- Holland A, Halper A, Cherney L. Tell me your story: Analysis of script topics selected by persons with aphasia. American Journal of Speech-Language Pathology. 2010;19:198–203. doi: 10.1044/1058-0360(2010/09-0095). [DOI] [PubMed] [Google Scholar]
- Hunston S, Thompson G, editors. Evaluation in text: Authorial stance and the construction of discourse. Oxford: Oxford University Press; 2003. [Google Scholar]
- Kertesz A. Western Aphasia Battery Revised. San Antonio, TX: PsychCorp; 2007. [Google Scholar]
- MacWhinney B. The CHILDES Project: Tools for analyzing talk. 3. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- Martin JR, White PRR. The language of evaluation: Appraisal in English. Houdsmills, Basingstoke, Hampshire: Palgrave Macmillan; 2005. [Google Scholar]
- Oelschlaeger ML, Thorne JC. Application of the correct information unit analysis to the naturally occurring conversation of a person with aphasia. Journal of Speech, Language, and Hearing Research. 1999;42:636–648. doi: 10.1044/jslhr.4203.636. [DOI] [PubMed] [Google Scholar]
- Olness G, Matteson SE, Stewart CT. “Let me tell you the point”: How speakers assign prominence to information in narratives. Aphasiology. 2010;24(6–8):697–708. [Google Scholar]
- Pittam J, Scherer KR. Vocal expression and communication of emotion. In: Lewis M, Haviland JM, editors. Handbook of emotions. New York: The Guilford Press; 1993. pp. 185–197. [Google Scholar]
- Pomerantz AM. Agreeing and disagreeing with assessment: Some features of preferred/dispreferred turn shapes. In: Atkinson JM, Heritage J, editors. Structure of Social Action: Studies in Conversation Analysis. Cambridge: Cambridge University Press; 1984. [Google Scholar]
- Pound C, Parr S, Lindsay J, Woolf C. Beyond aphasia: Therapies for living with communication disability. Bicester, Oxon: Speechmark; 2000. [Google Scholar]
- Pressman S, Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: A meta-analytic review. Annals of Behavioral Medicine. 2009;37:239–256. doi: 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riis J, Lowenstein G, Baron J, Jepson C, Fagerlin A, Ubel PA. Ignorance of hedonic adaptation to hemodialysis: A study using ecological momentary assessment. Journal of Experimental Psychology: General. 2005;134:3–9. doi: 10.1037/0096-3445.134.1.3. [DOI] [PubMed] [Google Scholar]
- Robinson J. Soliciting patients’ presenting concerns. In: Heritage J, Maynard D, editors. Communication in medical care. Interaction between primary care physicians and patients. Studies in Interactional Sociolinguistics (20) Cambridge: Cambridge University Press; 2006. pp. 22–47. [Google Scholar]
- Robinson RG, Benson DF. Depression in aphasic patients: Frequency, severity, and clinical-pathological correlations. Brain and Language. 1981;14:282–291. doi: 10.1016/0093-934x(81)90080-8. [DOI] [PubMed] [Google Scholar]
- Seligman M, Peterson C. Positive Clinical Psychology. In: Aspinwall L, Staudinger U, editors. Fundamental questions and future directions for a positive psychology. Washington DC: American Psychological Association; 2003. [Google Scholar]
- Shadden BB. Aphasia as identity theft. Aphasiology. 2005;19:211–224. [Google Scholar]
- Shadden BB, Hagstrom F. The role of narrative in the life participation approach to aphasia. Topics in Language Disorders. 2007;27(4):324–338. [Google Scholar]
- Shadden B, Hagstrom F, Koski PR. Neurogenic communication disorders: Life stories and the narrative self. San Diego: Plural Publishing. Psychology Press; 2008. [Google Scholar]
- Simmons-Mackie N, Damico J. Engagement in group therapy for aphasia. Seminars in Speech & Language. 2009;30:18–26. doi: 10.1055/s-0028-1104531. [DOI] [PubMed] [Google Scholar]
- Simmons-Mackie N, Damico J. Exploring clinical interactionin speech-language therapy: Narrative, discourse and relationships. In: Fourie R, editor. Therapeutic processes for communication disorders: A guide for clinicians and students. London: 2010. [Google Scholar]
- Simmons-Mackie N, Kagan A, Christie D, Huiuibregtas M, McEwan S, Williams J. Communicative access and decision making for people with aphasia: Implementing sustainable healthcare systems change. Aphasiology. 2007;21(1):39–66. [Google Scholar]
- Tukey JW. Exploratory data analysis. Reading, MA: Addison-Wesley; 1977. [Google Scholar]
- Ulatowska HK, Olness G. Dialectal variants of verbs in narratives of African Americans with aphasia: Some methodological considerations. In: Paradis M, editor. Manifestations of aphasia symptoms in different languages. Amsterdam: Pergamon; 2001. pp. 9–26. [Google Scholar]
- Ulatowska H, Olness G. On the nature of direct speech in narratives of African Americans with aphasia. Brain and Language. 2003;87:69–70. [Google Scholar]
- Ulatowska H, Olness G, Keebler M, Tillery J. Evaluation in stroke narratives: A study in aphasia. Brain & Language. 2006;99 (1–2):61–2. [Google Scholar]
- Youmans G, Holland A, Munoz M, Bourgeois M. Script training and automaticity in two individuals with aphasia. Aphasiology. 2005;19:435–450. [Google Scholar]
- Youmans G, Youmans S, Hancock A. Script training treatment for adults with apraxia of speech. American Journal of Speech Language Pathology. 2010 August; doi: 10.1044/1058-0360(2010/09-0085). (online edition) [DOI] [PubMed] [Google Scholar]