Abstract
Syphilitic aortic aneurysm is a rare occurrence in the antibiotic era, making the diagnose assumption even more infrequent. Nonetheless, this pathology can appear and should be suspected in patients with aortic aneurysm. We report a case of a 57-year old patient who presents with neurosyphilis and, in the following study, a large ascending aorta aneurysm is identified. The authors discuss the diagnostic challenge, the epidemiologic concerns, surgical indication and treatment and subsequent follow-up.
Keywords: Syphilitic, Aortic, Aneurysm
INTRODUCTION
The incidence of late manifestations of syphilis have declined almost to a rare entity since the era of antibiotics. Before the discovery of penicillin, tertiary syphilis infection was the most common cause of thoracic aortic aneurysm, resulting in 5–10% of cardiovascular deaths [1, 2].
The primary lesion of cardiovascular syphilis is aortitis, an inflammatory response to the invasion of the aortic wall by the Treponema pallidum that evolves to obliterative endarteritis of the vasa vasorum and results in necrosis of the elastic fibres and connective tissue in the aortic media. The resulting weakening of the aortic wall will progress into the late vascular manifestations of syphilis [3]. Syphilitic aortitis is reported in 70–80% of untreated cases after the primary infection, and in 10% of these patients, significant cardiovascular complications will occur, such as aortic aneurysm, aortic regurgitation and coronary ostia stenosis [1]. The ascending aorta is the segment most commonly affected (50%), followed by the arch (35%) and the descending aorta (15%) [3]. The rich lymphatic arrangement in the ascending aorta that may predispose greater mesoaortitis is believed to be the cause for larger involvement of this segment [3].
Cardiovascular syphilis is a late form of syphilis, which usually manifests in the 4th–5th decade of life, typically 5–40 years after the primary infection. It may become symptomatic with thoracic pain or symptoms of compression of the surrounding structures, but can enlarge asymptomatically until incidental finding in a chest X-ray or a catastrophic and often fatal aneurysmal rupture [1, 2]. Without surgical treatment, the mortality rate at 1 year can reach 80% due to the high rate of rupture of these aneurysms [4]. The authors report a currently rare case of syphilitic ascending aorta aneurysm.
CASE REPORT
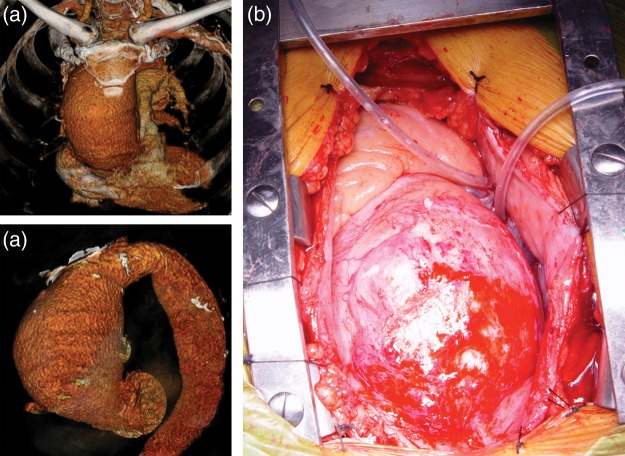
A 57-year old patient, without previous medical events of note, presented at the emergency department with sudden neurologic symptoms, namely left appendicular dysmetria and ataxic gait. The cerebral computer tomography (CT) revealed a small left ischaemic cerebellar stroke and the patient was admitted for further investigation and rehabilitation physiotherapy. The patient had a known history of poorly controlled hypertension, dyslipidaemia, tobacco abuse and ethylism. The haemogram, blood chemistry and coagulation tests were unremarkable and the viral markers tested negative for human immunodeficiency virus (HIV) 1 and 2, hepatitis B and C. The echocardiogram conducted to evaluate potential embolic source revealed a significant ascending aorta ectasia with normal aortic root diameter and moderate left ventricular hypertrophy, with good biventricular systolic function without aortic regurgitation, intracavitary mass or interatrial communication. The CT angiogram confirmed the presence of a giant fusiform ascending aortic aneurysm measuring 82 mm of maximum diameter extending nearly to the origin of the brachiocephalic artery with normal diameter across the descending thoracic and abdominal aorta and no flow-limiting obstruction or significant atherosclerotic disease of the supra-aortic arteries (Fig. 1). The patient tested positive for treponemal pallidum particle agglutination (TPHA) on blood and positive for venereal disease research laboratory (VDRL) test on blood (titre 1/64) and cerebrospinal fluid.
Figure 1:
(a) CT reconstruction images of the ascending aorta aneurysm; (b) intraprocedural photograph of the aneurysm.
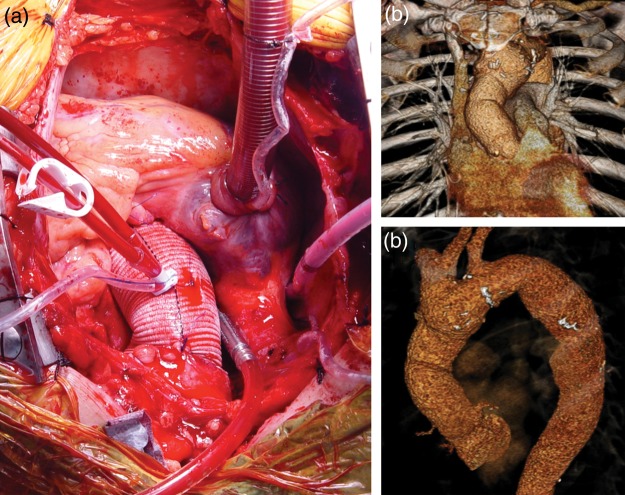
In this clinical scenario, the patient was diagnosed with tertiary syphilis with neurologic and cardiovascular involvement and was treated with penicillin and probenecid. The patient recovered completely from the neurologic deficits within 1 week. The cardiovascular involvement was limited to the ascending aorta, with no flow-limiting disease in the coronary angiogram. The patient denied any previous cardiovascular clinical manifestation or compression-related symptom such as dysphagia, dyspnoea or superior member oedema. Although admitting past history of risky sexual behaviour, the patient had no recollection of any primary lesions or symptoms related to secondary syphilis. The size and aetiology of the aneurysm indicated surgical treatment and surgery was programmed as soon as possible. The surgical procedure was planned as usual for large ascending aorta aneurysms, and cardiopulmonary bypass (CBP) was established with peripheral femoral artery access for arterial cannulation and central two-stage (cavoatrial) access for venous cannulation (Fig. 1). The patient was cooled to 28°C and the ascending aorta was cross-clamped just proximal to the origin of the brachiocephalic artery. The heart was protected with intermittent retrograde blood cardioplegia and the ascending aorta was replaced with a 34 mm polyester vascular graft (Hemashield platinum woven double velour vascular graft, Maquet Cardiovascular LLC, Wayne, USA) without the need for cardiocirculatory arrest (Fig. 2). Weaning from CBP was straightforward and haemostasis was uncomplicated. The postoperative course was uneventful and the patient was discharged on the 6th postoperative day. Histological examination of the aneurysmal wall revealed the presence of mesoaortitis with marked reduction in the musculo-elastic medial tissue and significant lymphocytic infiltration with reasonable amount of plasmocytes in relation to the vasa vasorum, compatible with the morphologic findings in histological involvement of syphilis. On postoperative follow-up evaluation at 1 and 2 months, the patient was well and asymptomatic. Chest CT showed neither pseudoaneurysms nor other anastomotic site-related complications (Fig. 2).
Figure 2:
(a) Intraprocedural photograph of the corrected aneurysm with the vascular graft; (b) postoperative CT reconstruction images of the ascending aorta.
DISCUSSION
Cardiovascular syphilitic infection has nearly disappeared in developed countries, although it remains a differential diagnosis in developing nations. Recent epidemiologic reports show an increase in reported cases related to the HIV infection [5, 6]. The rarity of this aetiology makes the diagnosis difficult, mainly because syphilis testing is not routinely used. In late syphilis, non-treponemal tests like VDRL test and rapid plasma reagin test are less sensitive (71–73%), when compared with treponema-specific tests such as TPHA, micro-haemagglutination test, flourescent treponemal antibody absorption test (94–96%) [7, 8]. According to Kuramochi et al. [9], serologic proved syphilis is necessary to make the diagnosis of syphilitic aortitis, the histologic findings of mesoaortitis by itself is not diagnostic. In the presence of an aortic aneurysm, particularly in younger patients, syphilitic serological testing is advised [8]. CT angiogram is the best imaging study to define the size and anatomy of the aneurysm, but in the setting of an aneurysm, the echocardiogram and coronary angiogram are mandatory to exclude aortic regurgitation and coronary flow-limiting lesions [1, 2]. The definitive treatment of aortic aneurysm is surgical repair, which involves resection of the dilated portion of the aorta and replacing it with a synthetic vascular graft [1]. The simultaneous presence of aortic regurgitation or significant coronary disease should be surgically treated at the same time [1]. Surgery and specific antibiotic treatment does not exclude future manifestations of the disease, even after erradication of the Treponema pallidum, which makes permanent follow-up needed [1, 10].
Conflict of interest: none declared.
REFERENCES
- 1.Duncan JM, Cooley DA. Surgical considerations in aortitis. Part III: syphilitic and other forms of aortitis. Tex Heart Inst J. 1983;10:337–41. [PMC free article] [PubMed] [Google Scholar]
- 2.Jackman JD, Radolf JD. Cardiovascular syphilis. Am J Med. 1989;87:425–33. doi: 10.1016/s0002-9343(89)80826-5. [DOI] [PubMed] [Google Scholar]
- 3.Heggtveit HA. Syphilitic aortitis: a clinicopathologic autopsy study of 100 cases, 1950 to 1960. Circulation. 1964;24:346–55. doi: 10.1161/01.cir.29.3.346. [DOI] [PubMed] [Google Scholar]
- 4.Revest M, Decaux O, Frouget T, Cazalets C, Cador B, Jégo P, et al. Syphilitic aortitis. Experience of an internal medicine unit. Rev Med Intern. 2006;27:16–20. doi: 10.1016/j.revmed.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 5.Ntsekhe M, Hakim J. Impact of HIV infection in cardio vascular diseases in Africa. Circulation. 2005;112:3602–7. doi: 10.1161/CIRCULATIONAHA.105.549220. [DOI] [PubMed] [Google Scholar]
- 6.Restrepo CS, Diethelm L, Lemos JA, Velásquez E, Ovella TA, Martinez S, et al. Cardiovascular complications of HIV infection. Radiographics. 2006;26:213–31. doi: 10.1148/rg.261055058. [DOI] [PubMed] [Google Scholar]
- 7.Larsen SA, Steiner BM, Rudolph AH. Laboratory diagnosis and interpretation of tests for syphilis. Clin Microbiol Rev. 1995;8:1–21. doi: 10.1128/cmr.8.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tichonova L, Borisenko K, Ward H, Meheus A, Gromyko A, Renton A. Epidemics of syphilis in the Russian Federation: trends, origins and priority of control. Lancet. 1997;350:210–3. doi: 10.1016/S0140-6736(97)01382-2. [DOI] [PubMed] [Google Scholar]
- 9.Kuramochi S, Sugiura H, Kishida Y. Pathology of inflammatory aortic aneurysma: discussion on their diferencial diagnosis. Myakkan-gaku. 1996;36:261–5. [Google Scholar]
- 10.Salas Millán J, Martínez Calzón JL, González de Vega N, Castillo Castro JL. Cardiovascular syphilis: a case report. Rev Esp Cardiol. 2000;53:1656–8. doi: 10.1016/s0300-8932(00)75293-6. [DOI] [PubMed] [Google Scholar]