Abstract
OBJECTIVES: It is generally accepted that in adult type 1 diabetes patients (T1D) continuous subcutaneous insulin infusion (CSII) via a personal pump is more effective than the multiple daily injections (MDI) model. However, it is not clear whether all age groups of adult T1D patients may equally benefit from CSII therapy. We aimed to compare the glycemic control and use of selected pump tools in T1D subjects using CSII over the age of 50 (50+ T1D) with patients younger than 50 years of age. METHODS: The last available insulin pump/blood glucose meter downloads and last available HbA1c levels of 124 adult T1D subjects using CSII were reviewed. We divided our cohort into two subgroups: 50+ T1D patients (n = 13) and younger patients (n = 111). RESULTS: There were no differences in glycemic control achieved with CSII treatment in 50+ T1D patients vs. younger subjects. HbA1c levels were 7.01 ± 0.67% and 7.34 ± 1.24% (p = 0.46), and the mean glycemia based on glucometer downloads was 141.8 ± 17.7 mg/dl and 150.8 ± 35.7 mg/dl (p = 0.69), respectively. Also, there were no differences with respect to the use of important personal pump options and tools. CONCLUSION: In conclusion, insulin pump therapy appears to be effective and safe in T1D patients regardless of age.
Keywords: type 1 diabetes, insulin pump, glycemic control, HbA1c, dual-wave bolus, bolus wizard, monitoring
Abbreviations: 50+ T1D - T1D subjects using CSII over the age of 50; <50 T1D - T1D subjects using CSII below the age of 50; BMI - body mass index; CSII - continuous subcutaneous insulin infusion; DCCT - Diabetes Control and Complications Trial; HbA1c - glycated hemoglobin; IU - international unit; MDI - multiple daily injections; T1D - type 1 diabetes
Introduction
The Diabetes Control and Complications Trial (DCCT) showed that intensive insulin therapy in type 1 diabetes (T1D) combined with structured self-monitoring of blood glucose can delay the onset and slow down the progression of microvascular complications of diabetes compared to the conventional therapy of manually administered daily insulin injections [1, 2]. Insulin therapy may be implemented either with continuous subcutaneous insulin infusion (CSII) via a personal pump or multiple daily injections (MDI) model. The currently available data suggest that in adults with T1D, CSII is more effective than MDI in optimizing glycemic control [1, 3-5]. However, there is insufficient evidence regarding adverse events, mortality, and morbidity [6]. Personal insulin pump therapy dates back to the late 1970s [7, 8]. Contemporary insulin pumps offer programming of multiple basal insulin infusion rates, profiling of boluses, suspension or temporary rate program of insulin delivery, and additional features enabling calculation of the insulin doses for the carbohydrate content of meals and for the correction of glycemic levels outside of target ranges [9]. These options were shown to improve the efficacy of pump use [10-12].
Given these improvements, it remains unclear whether all age groups of adult T1D patients benefit equally from modern insulin pump therapy. In particular, the effectiveness of this new technology-based therapy in elderly patients may be of concern. It was shown that CSII may be equally effective as MDI in optimizing metabolic control in older individuals with T2D [13]. However, there is a shortage of data addressing this issue in T1D, only two small studies examine this topic. The first, a retrospective analysis of five older patients with T1D, showed a profound decrease in HbA1c levels and a significant decrease in the frequency of severe hypoglycemic episodes after the switch from MDI to CSII [14]. Also in this analysis, CSII treatment initiation resulted in better outcomes in patients older than 50 years of age compared to those younger than 20 years [15]. In our cross-sectional study, we aim to compare glycemic control and use of selected pump tools in T1D patients using CSII over the age of 50 (50+ T1D) with that in patients younger than 50 years of age (<50 T1D).
Patients and methods
All subjects whose records were collected for the purpose of this study were patients of the Department of Metabolic Diseases, University Hospital in Krakow, and were residents of southern Poland. The patients were seen at the outpatient clinic on a regular basis (every 3-4 months). Individuals with CSII treatment of less than 3 months duration were excluded from the analysis. The last available insulin pump and blood glucose meter downloads and HbA1c levels of 124 adult T1D subjects on CSII treatment were recorded. For insulin pumps, we analyzed records from the last 4-6 weeks, while for glucometers, the whole memory content (200-300 records depending on glucometer type) was included.
We divided the subjects into two subgroups: 50+ T1D patients (n = 13) and patients below the age of 50 years (<50 T1D) (n = 111). The groups were similar with respect to gender (% of male/female patients: 38/62 (n = 5/8) and 30/70 (n = 33/78), p = 0.52) and BMI (24.05 ± 2.62 kg/m2 vs. 21.35 ± 2.72 kg/m2, p = 0.28) for older and younger patients, respectively. The clinical characteristics of the study groups are provided in Table 1. All patients in the <50 T1D group and all but one in the 50+ T1D group used rapid acting insulin analogs. One patient in the 50+ T1D group, a 75-year old woman, was treated with regular short-acting human insulin. Clinical data were collected from patients regarding:
Table 1. Clinical characteristics of patients and use of insulin pump tools and options in the study groups.
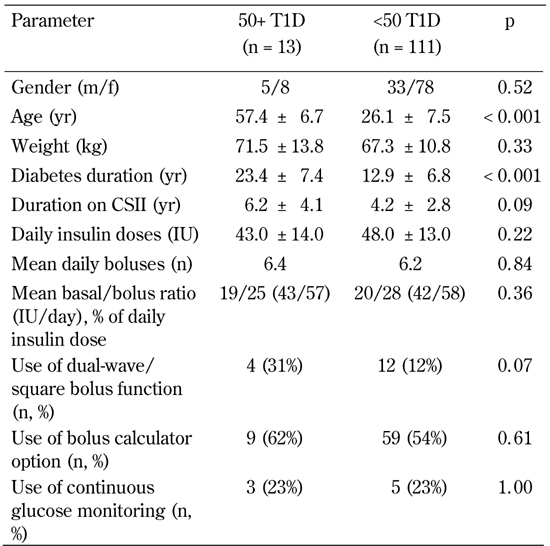
Legend: Data are mean ± SD. 50+ T1D: patients using CSII over 50 years of age. <50 T1D: patients using CSII below 50 years of age. CSII: continuous subcutaneous insulin infusion. IU: international unit. T1D: type 1 diabetes.
- carbohydrate counting,
- active adjustment of basal/bolus insulin delivery,
- severe hypoglycemic episodes that required either the assistance of another person or medical assistance, and
- diabetic ketoacidosis.
Summary statistics, including means and standard deviations for continuous data, and frequencies and proportions for categorical data, were used to describe the study group characteristics. An unpaired t-test was used for comparisons between the two groups when data were normally distributed; otherwise, nonparametric analysis was applied (Mann-Whitney U-test). For categorical variables we used chi-squared test or Fisher’s exact test where appropriate. A p-value of <0.05 was considered significant. The analyses were conducted by the use of Statistica, version 9.0 (Statsoft, Poland).
Results
There were no differences in glycemic control achieved with CSII treatment in 50+ T1D patients vs. younger subjects: the HbA1c levels were 7.01 ± 0.67% and 7.34 ± 1.24% (p = 0.46). The groups did not differ with respect to the number of daily blood glucose measurements (5.3 vs. 5.9, for older and younger patients, respectively, p = 0.74). Mean glycemia based on glucometer downloads was 141.8 ± 17.7 mg/dl (50+ T1D) and 150.8 ± 35.7 mg/dl (<50 T1D, p = 0.69), respectively.
There were no episodes of severe, assistance-requiring hypoglycemic episodes in the 50+ T1D group during the last year, while the <50 T1D patients had nine such episodes (frequency of 8.1/100 patients/year). None of the 50+ T1D subjects required hospitalization due to glycemic decompensation, but there were four hospitalizations in the <50 T1D group (frequency of 3.6/100 patients/year). For both features, however, the differences were not statistically significant (p = 0.59 and p = 1.0 for severe hypoglycemia and metabolic decompensation, respectively).
Interestingly, there were no differences with respect to:
- The use of important personal pump options and tools such as daily number of boluses and basal/bolus ratio.
- The percentage of usage of dual-wave/square bolus function and Bolus Wizard option.
- The percentage of patients using continuous glucose monitoring (Table 1).
T1D patients under the age of 50 required more insulin per kilogram (0.73 IU/kg vs. 0.55 IU/kg for younger and older individuals, respectively, p = 0.0007). While all of the <50 T1D patients declared carbohydrate counting and active adjustment of basal/bolus insulin delivery, 2 out of 13 individuals in the 50+ T1D group chose to stay on relatively steady insulin doses following predictable meals and physical activity.
Discussion and conclusions
In this study, we found that outcomes of CSII treatment in T1D subjects over 50 years of age in comparison to younger patients are equally effective and safe. Furthermore, both groups were equally willing to use modern pump technology.
The age limit used to stratify the study group was chosen arbitrarily and corresponded to an earlier report performed in T1D subjects in whom CSII had just been initiated [15]. Our older cohort included mostly subjects from the sixth and seventh decade of live, so it is not representative for T1D patients of very advanced age. We should point out that our project is merely a clinical observation. Specifically, T1D subjects were clinically selected for pump treatment, and CSII was not implemented in patients with a decline in cognitive function, vision impairment, or other age-related contraindications for this pump therapy. In general, 50+ T1D subjects were supposed to fulfill the same generally recognized criteria for CSII initiation as younger patients [12, 16-18].
Interestingly, there were no significant differences in basal/bolus ratios between younger and older individuals. This finding suggests that insulin delivery profiles do not differ considerably between patients of different age groups. Previous reports addressing this issue and showing significant age-related differences in insulin patterns examined much younger populations [19].
The only clinical difference between the groups analyzed was a significantly higher insulin dose per kilo in the <50 T1D group. This outcome may be surprising given expected age-related impairments in insulin sensitivity [20] and the lower rate of physical activity among older individuals [21]. One potential explanation could be a higher carbohydrate intake among younger individuals. However, data is lacking to support this hypothesis. Finally, CSII therapy appears to be safe in 50+ T1D patients since, during the last year of observation, no episodes of hypoglycemia or severe glycemic decompensation that required medical assistance were recorded [22].
Our study has some limitations. The number of patients in the two groups is unbalanced. The sample size represents the proportion of subjects from both age groups seen at our outpatient clinic. The overrepresentation of younger individuals may be, at least to some degree, a result of the reimbursement system, with no lack of support regarding purchase of the pump or disposables for individuals over 26 years of age.
It should also be noted that the duration of CSII treatment was not fully matched between the patient groups. Older individuals were treated with CSII on average for 6.2 years vs. 4.2 years in younger subjects. This tendency, although not statistically significant, may mean that the study outcomes could have been influenced by differences in the patients' experience with CSII treatment. Furthermore, the study was a cross-sectional study; we did not analyze certain factors that may be important for safety considerations of CSII treatment in older populations, including the safety of the initiation process (e.g. number of hypoglycemic episodes) which needs to be clarified in future analysis. Finally, the current study was based on clinical observation, while prospective randomized trials are required to fully define the effectiveness and safety of insulin pump therapy in older populations.
In conclusion, results from this study indicate that the effectiveness and safety of insulin pump therapy is largely equivalent in younger and elderly T1D patients. Basal/bolus ratios in CSII treated patients were not significantly different between younger and older adult diabetic individuals. Patients over 50 years of age were willing to use advanced personal insulin pump options and tools such as dual-wave/square bolus, Bolus Wizard, and continuous glucose monitoring just as frequently as younger T1D individuals.
Disclosures: Tomasz Klupa received payments for lectures from Medtronic. Katarzyna Cyganek received travel grants from Medtronic and Willcare.
Acknowledgments
The authors are grateful to Ms. Anna Lipowska and Sebastian Borys for their editorial help in the preparation of this manuscript.
References
- 1.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 2.Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes. N Engl J Med. 2011 doi: 10.1056/NEJMoa1111732. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pickup J, Keen H. Continuous subcutaneous insulin infusion at 25 years: evidence base for the expanding use of insulin pump therapy in type 1 diabetes. Diabetes Care. 2002;25(3):593–598. doi: 10.2337/diacare.25.3.593. [DOI] [PubMed] [Google Scholar]
- 4.Hoogma RP, Hammond PJ, Gomis R, Kerr D, Bruttomesso D, Bouter KP, Wiefels KJ, de la Calle H, Schweitzer DH, Pfohl M. et al. 5-Nations Study Group. Comparison of the effects of continuous subcutaneous insulin infusion (CSII) and NPH-based multiple daily insulin injections (MDI) on glycaemic control and quality of life: results of the 5-nations trial. Diabet Med. 2006;23(2):141–147. doi: 10.1111/j.1464-5491.2005.01738.x. [DOI] [PubMed] [Google Scholar]
- 5.Bruttomesso D, Costa S, Baritussio A. Continuous subcutaneous insulin infusion (CSII) 30 years later: still the best option for insulin therapy. Diabetes Metab Res Rev. 2009;25(2):99–111. doi: 10.1002/dmrr.931. [DOI] [PubMed] [Google Scholar]
- 6.Misso ML, Egberts KJ, Page M, O'Connor D, Shaw J. Continuous subcutaneous insulin infusion (CSII) versus multiple insulin injections for type 1 diabetes mellitus. Cochrane Database Syst Rev. 2010;1:CD005103. doi: 10.1002/14651858.CD005103.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pickup JC, Keen H, Parsons JA, Alberti KG. Continuous subcutaneous insulin infusion: an approach to achieving normoglycemia. BMJ. 1978;1(6107):204–207. doi: 10.1136/bmj.1.6107.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tamborlane WV, Sherwin RS, Genel M, Felig P. Reduction to normal of plasma glucose in juvenile diabetes by subcutaneous administration of insulin with a portable infusion pump. N Engl J Med. 1979;300(11):573–578. doi: 10.1056/NEJM197903153001101. [DOI] [PubMed] [Google Scholar]
- 9.Wolpert H, Block J. Hands-on demonstration and discussion of new pump software/hardware. Diabetes Technol Ther. 2005;7(5):840–844. doi: 10.1089/dia.2005.7.840. [DOI] [PubMed] [Google Scholar]
- 10.Klupa T, Benbenek-Klupa T, Malecki M, Szalecki M, Sieradzki J. Clinical usefulness of a bolus calculator in maintaining normoglycaemia in active professional patients with type 1 diabetes treated with continuous subcutaneous insulin infusion. J Int Med Res. 2008;36(5):1112–1116. doi: 10.1177/147323000803600531. [DOI] [PubMed] [Google Scholar]
- 11.Shashaj B, Busetto E, Sulli N. Benefits of a bolus calculator in pre- and postprandial glycaemic control and meal flexibility of paediatric patients using continuous subcutaneous insulin infusion (CSII) Diabet Med. 2008;25(9):1036–1042. doi: 10.1111/j.1464-5491.2008.02549.x. [DOI] [PubMed] [Google Scholar]
- 12.Cukierman-Yaffe T, Konvalina N, Cohen O. Key elements for successful intensive insulin pump therapy in individuals with type 1 diabetes. Diabetes Res Clin Pract. 2011;92(1):69–73. doi: 10.1016/j.diabres.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Herman WH, IIag LL, Johnson SL, Martin CL, Sinding J, Al Harthi A, Plunkett CD, LaPorte FB, Burke R, Brown MB. et al. A clinical trial of continuous subcutaneous insulin infusion versus multiple daily injections in older adults with type 2 diabetes. Diabetes Care. 2005;28(8):1568–1573. doi: 10.2337/diacare.28.7.1568. [DOI] [PubMed] [Google Scholar]
- 14.Rizvi AA, Petry R, Arnold MB, Chakraborty M. Beneficial effects of continuous subcutaneous insulin infusion in older patients with long-standing type 1 diabetes. Endocr Pract. 2001;7(5):364–369. doi: 10.4158/EP.7.5.364. [DOI] [PubMed] [Google Scholar]
- 15.Lepore G, Dodesini AR, Nosari I, Trevisan R. Age and A1C are important clinical predictors of continuous subcutaneous insulin infusion efficacy in type 1 diabetic patients. Diabetes Care. 2005;28(7):1834–1835. doi: 10.2337/diacare.28.7.1834. [DOI] [PubMed] [Google Scholar]
- 16.Hanaire H, Lassmann-Vague V, Jeandidier N, Renard E, Tubiana-Rufi N, Vambergue A, Raccah D, Pinget M, Guerci B. Treatment of diabetes mellitus using an external insulin pump: the state of the art. Diabetes Metab. 2008;34(4):401–423. doi: 10.1016/S1262-3636(08)73972-7. [DOI] [PubMed] [Google Scholar]
- 17.Pickup J, Keen H. Continuous subcutaneous insulin infusion at 25 years: evidence base for the expanding use of insulin pump therapy in type 1 diabetes. Diabetes Care. 2002;25(3):593–598. doi: 10.2337/diacare.25.3.593. [DOI] [PubMed] [Google Scholar]
- 18.Bode BW, Tamborlane WV, Davidson PC. Insulin pump therapy in the 21st century. Strategies for successful use in adults, adolescents, and children with diabetes. Postgrad Med. 2002;111(5):69–77. doi: 10.3810/pgm.2002.05.1200. [DOI] [PubMed] [Google Scholar]
- 19.Bachran R, Beyer P, Klinkert C, Heidtmann B, Rosenbauer J, Holl RW. for the German/Austrian DPV Initiative, the German Pediatric CSII Working Group and the BMBF Competence Network Diabetes. Basal rates and circadian profiles in continuous subcutaneous insulin infusion (CSII) differ for preschool children, prepubertal children, adolescents and young adults. Pediatr Diabetes. 2011 doi: 10.1111/j.1399-5448.2011.00777.x. In press. [DOI] [PubMed] [Google Scholar]
- 20.Ferrannini E, Natali A, Capaldo B, Lehtovirta M, Jacob S, Yki-Järvinen H. Insulin resistance, hyperinsulinemia, and blood pressure: role of age and obesity. European Group for the Study of Insulin Resistance (EGIR) Hypertension. 1997;30(5):1144–1149. doi: 10.1161/01.hyp.30.5.1144. [DOI] [PubMed] [Google Scholar]
- 21.Brown DR, Yore MM, Ham SA, Macera CA. Physical activity among adults > or =50 yr with and without disabilities, BRFSS 2001. Med Sci Sports Exerc. 2005;37(4):620–629. doi: 10.1249/01.mss.0000158189.17546.ed. [DOI] [PubMed] [Google Scholar]
- 22.Klupa T, Matejko B, Cyganek K, Katra B, Galicka-Latała D, Grzanka M, Malecki MT. Insulin pump therapy may be equally effective in elderly an young type 1 diabetes patients. Diabetologia. 2011;54(Suppl 1):P976. doi: 10.1900/RDS.2011.8.254. [DOI] [PMC free article] [PubMed] [Google Scholar]


